Abstract
Background/objectives
To evaluate perioperative safety and outcome of parenchyma-preserving pancreatectomy and risk factors of metastasis and recurrence for patients with solid pseudopapillary neoplasm (SPN).
Methods
Demographic data, operative and pathological parameter, follow-up data of patients with SPN undergoing their first operation were collected in our single center from May 2016 to October 2021 and compared between regular pancreatectomy group and parenchyma-preserving surgery group. Risk factors for metastasis and recurrence were investigated.
Results
A total of 194 patients were included, 154 of whom were female and the average age of all patients was 33 years old. Most patients were asymptomatic, with the most common complaint being abdominal pain or discomfort. Of them, 62 patients underwent parenchyma-preserving pancreatectomy including middle segment pancreatectomy and enucleation, and 132 patients underwent regular pancreatectomy including pancreaticoduodenectomy, distal pancreatectomy and total pancreatectomy. Patients in the parenchyma-preserving surgery group had a shorter duration of operation, less intraoperative bleeding, and decreased risk of combined organ removal and blood transfusion, with no statistical significance yet. The two groups exhibited a similar incidence of postoperative complications including grade B and C pancreatic fistula, delayed gastric emptying, postoperative pancreatic hemorrhage, and other complications, as well as radiological intervention, relaparotomy and the length of postoperative hospital stay. There were no perioperative deaths. All the patients, except 18 of those who discontinued follow-up, were alive with a median follow-up time of 31 months. Three patients in the regular pancreatectomy group were observed to have liver metastasis, and no metastasis was observed in the parenchyma-preserving surgery group. Significant risk factors for tumor metastasis and recurrence were tumor size, angioinvasion, and nerve infiltration.
Conclusions
Parenchyma-preserving surgery did not significantly increase the frequency of perioperative complications or recurrence and might be preferable if comprehensive conditions allow.
Similar content being viewed by others
Introduction
Solid pseudopapillary neoplasm (SPN) or solid pseudopapillary tumor (SPT) of pancreas was described by an authoritative pathologist, Virginia Kneeland Frantz, in 1959 [1] and was officially renamed by the World Health Organization (WHO) in 1996. SPN is a relatively rare type of pancreas tumor, accounting for 1–2% of pancreatic neoplasms [2]. It predominantly occurs in adolescent and young adult females and is, thus, called daughter disease [3, 4]. There are no specific symptoms of SPN. With the accumulation of cases and experience from single center studies with small sample size, the knowledge of SPN has improved gradually than before and remains worthy of study. SPN is considered as a low-grade malignant tumor with an indolent growing pattern. Operation is the preferred treatment currently, and its purpose is the removal of the primary lesion in the pancreas and metastatic lesion, without routine lymphadenectomy [5,6,7]. With a certain potential for recurrence and metastatic dissemination, the recurrence rate is reported at 2.6–3.5% according to a meta-analysis [3, 8]. The prognosis of SPN patients is extremely favorable if followed by complete resection [7]. Patients with recurrence and metastasis may survive for a long time following reoperation. If perioperative safety and efficacy are warranted, surgical methods that preserve pancreatic parenchyma and function might be prioritized. Additionally, although SPN with surrounding tissue invasion, perineural invasion, vascular invasion on microscopic pathology exhibits malignant biological behaviors, no agreement has been achieved on the effect of these characteristics on the recurrence and metastasis. Identification of risk factors would aid in the follow-up of high-risk patients.
In this study, we retrospectively collected and analyzed the clinicopathological data of recent patients with SPN classified into regular pancreatectomy group and parenchyma-preserving surgery group in our center, compared the perioperative safety and outcomes between patients of the two groups, and investigated risk factors for metastasis and recurrence to improve SPN cognition and benefit patients.
Methods
Patient population
All patients with SPN undergoing their first operation were screened at pancreas center, the First Affiliated Hospital with Nanjing Medical University from May 2016 to October 2021. All cases were confirmed by pathological examination including hematoxylin and eosin stain and immunohistochemistry. Patients undergoing pancreaticoduodenectomy (PD), distal pancreatectomy (DP), and total pancreatectomy (TP) constituted the regular pancreatectomy group, and those undergoing middle segment pancreatectomy (MSP) and enucleation constituted the parenchyma-preserving surgery group. Other surgical procedures were not performed and collected. The consent form was collected at the time of admission. The study was complied with the Declaration of Helsinki and approved by the Ethics Committee of the First Affiliated Hospital with Nanjing Medical University.
Surgical procedures
The surgical procedure included PD (classic Whipple procedure or pylorus-preserving pancreaticoduodenectomy, PPPD) with modified one-layer duct-to-mucosa pancreaticojejunostomy [9], DP (with splenectomy, the Warshaw technique, or the Kimura technique), total pancreatectomy, MSP, and enucleation and was established by preoperative diagnosis, individual surgeon preference, and intraoperative discretion depending on tumor location and size.
Data collection
Demographic data including sex, age, chief complaint, diabetes, history of smoking and drinking, preoperative carbohydrate antigen (CA) 19–9, preoperative carcinoembryonic antigen (CEA), pathological parameters including tumor size (the largest diameter), margin status, Ki-67 index, number of lymph node metastasis, number of detected lymph nodes, angioinvasion, and nerve infiltration, operative parameters including surgical procedure, operation duration, combined organ resection, blood transfusion, and estimated blood loss, and preoperative computed tomography (CT) scans were retrospectively collected from electronic medical records in our hospital. Surgical complications, including postoperative pancreatic fistula (POPF), delayed gastric emptying (DGE), and postoperative hemorrhage (POPH), were assessed and graded based on criteria established by the International Study Group of Pancreatic Surgery [10,11,12].
Follow-up
Following discharge, regular follow-up of patients was performed. Follow-up data, including exocrine and endocrine function of pancreas, survival status, and the presence or absence of recurrence and metastasis, were gathered from the hospital records or through regular phone interviews with patients. Endocrine dysfunction included new-onset diabetes or deterioration of preoperative diabetes. Exocrine pancreatic insufficiency was measured in terms of enzyme supplementation or steatorrhea. The last follow-up was in January 2022.
Statistical analysis
Categorical variables were represented as frequency. Continuous variables were expressed as means ± SD or median (interquartile range). The Student t test was used to compare continuous parameters between the two groups. The chi-squared test and Fisher's exact test were used to compare the categorical parameters. Logistic regression analysis was performed to screen the risk factors of metastasis. P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 26.0 software.
Results
Safety and efficacy of parenchyma-preserving procedure
From May 2016 to October 2021, a total of 194 patients undergoing their primary surgery at our center were included in this study. There were 154 females and 40 males, with an average age of 33 years. Abdominal pain or discomfort was the main complaint of patients, and more than half were admitted after a physical examination that revealed a pancreatic tumor (Table 1).
The patients were divided into two groups based on the degree of parenchymal preservation in the operation: regular pancreatectomy group including PD or PPPD (19%), DP with the spleen (25%), Kimura technique (15%), or Warshaw technique (9%), and TP (< 1%) and the parenchyma-preserving surgery group including MSP (24%) and enucleation (8%). There was no significant difference in gender, age, main complaint, general condition, and the level of preoperative CA 19–9 and CEA between the two groups (Table 1).
Patients in the regular pancreatectomy group had larger tumor size than that in the parenchyma-preserving surgery group (5.66 ± 3.14 versus 3.73 ± 2.16 cm). More lymph nodes were easily detected in surgical specimens in regular pancreatectomy group (7.15 versus 1.91). However, there was no significant difference in other pathological parameters such as number of lymph node metastasis, Ki-67 index, angioinvasion or nerve infiltration between the two groups (Table 1).
To evaluate the safety of parenchyma-preserving surgery, we compared surgical parameters and the incidence of postoperative complications. Patients in the parenchyma-preserving surgery group had a shorter operation duration (181 min versus 196 min), less intraoperative bleeding (120 mL versus 160 mL), and a lower risk of combined organ removal (0% versus 4.5%) and blood transfusion (1.6% versus 5.3%) than those in the regular pancreatectomy group. However, these values were not statistically significant. In terms of postoperative complications, the incidence of grade B or grade C pancreatic fistula, DGE, and POPF were statistically identical between the two groups, and there was no significant difference in the incidence of other complications, such as biliary fistula, chylous leakage, or incision infection, as well as radiological intervention and the length of postoperative hospital stay. Two patients in each group underwent a second operation. The perioperative mortality rate was zero in both groups. However, there were three readmissions and four readmissions in two groups respectively. Postoperative metastasis was not observed in the parenchyma-preserving surgery group. Furthermore, the incidence of exocrine pancreatic insufficiency and endocrine dysfunction were significantly lower in the parenchyma-preserving surgery group than that in the regular pancreatectomy group (Table 2).
Demographics and clinicopathologic features subgrouped by age
Considering the difference in the incidence of SPN in patients of different ages, we compared the demographics and clinicopathological features of the patients divided into three groups based on age. As indicated in Table 3, there was no difference in the distribution of symptoms, sex, and preoperative CA 19–9 and CEA, whereas there was a difference in the distribution of diabetes, which was consistent with age. The composition ratios of surgical procedure in each group are slightly different. There was no significant difference in the lymph node metastasis, angioinvasion, nerve infiltration, and postoperative metastasis of the groups. However, Ki-67 revealed a statistically significant difference.
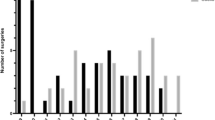
General and misdiagnosed image features
One hundred eleven abdominal CT scans were available and reviewed at our hospital (Table 4). Execpt for a case that could not be evaluated by CT scan, there were 40 cases of mass in the head of the pancreas, 13 in the neck of the pancreas, and 57 in the body and tail of the pancreas. Based on the proportion of cystic and solid components (Fig. 1), SPN on the scan displayed pure cystic (n = 3), mostly cystic (n = 9), cystic and solid or mixed density (n = 81), mostly solid (n = 11), or pure solid components (n = 6). Calcification was present in different site of tumor. About two-thirds of cases were radiographically typical and had high diagnostic values. The rest of the images were not typical, and the diagnosis of SPN was not a priority, which requires the expertise of experienced specialists. The scan might be misdiagnosed as pancreatic ductal adenocarcinoma (PDAC), pancreatic neuroendocrine tumor (PNET), or mucinous cystic neoplasm (MCN) when SPN displayed pure solid or pure cystic components (Fig. 2A–D). In addition, SPN could showed extremely large size and contacted with several organs, which is indistinguishable in the organ origin of the tumor radiographically (Fig. 2E).
Atypical and easily misdiagnosed SPN images. A A 33-year-old-female, low density lesion in pancreatic head with fuzzy boundary, like PDAC. B A 45-year-old-female, small solid lesion in body of pancreas, like neuroendocrine tumor. C A 19-year-old-female, pure cystic lesion with septa inside, like mucinous cystic neoplasms. D A 49-year-old-female, several calcifications around the lesion, like chronic pancreatitis. E A 14-year-old female, huge mass with portal vein contour irregularity
Risk factors for recurrence and metastasis
Follow-up data for 176 patients were available, and 18 patients were lost to follow-up. All the surviving patients had a median follow-up duration of 31 months (3 − 69 months). Three female patients presented with liver metastasis at 6, 12, and 39 months, respectively, following the initial operation. These patients underwent radiofrequency ablation, and one of them had a simultaneous liver resection with relapse. Clinicopathological risk factors for metastasis were investigated. Significant risk factors for tumor recurrence and metastasis were tumor size, angioinvasion, and nerve infiltration (Table 5).
Discussion
Solid pseudopapillary neoplasm of the pancreas is a rare pancreatic tumor accounting for 1 − 2% of all pancreatic tumors. Since its discovery in 1959, public knowledge of this disease has steadily increased.
The average age of onset of SPN is 27 years in the Chinese population, mostly affecting young people [3]. Patients older than 45 years have been reported to constitute only a small percentage of all SPN cases [6]. In our study, patients with ages < 40 years accounted for 70% of all cases, consistent with data in Germany. Kang et al. correlated tumor size with the age of patients and observed that older patients had relatively smaller tumors than younger patients [13], which was not directly found in our patients. However, older patients had lower Ki-67 index, and there was no significant difference in the margin lymph node metastasis, angioinvasion, nerve infiltration, and postoperative metastasis among patients subgrouped by age. SPN predominately occurs in female whereas males are rarely affected [7, 14]. Our study appears to have a little larger number of male patients than previously reported [3, 14]. Female preponderance could be explained by proximity to the ovarian ridge during development and the presence of progesterone receptors in malignant cells [5, 15]. Patients with SPN usually lack specific manifestations. Non-specific abdominal pain and discomfort and incidentally detection are common chief presentation of patients. Other chief complaint included nausea and vomiting, obstructive jaundice, and discovery in a laparotomy due to abdominal trauma in our cases.
Preoperative image has become the most commonly used tool for diagnosing SPN. The advantages of multidetector CT and magnetic resonance imaging are non-invasion and convenience [16]. SPN on CT is typically characterized by a well-defined, low-attenuation mass with peripheral enhancement and complex cystic components. Besides, necrosis and internal hemorrhage may coexist [17]. However, not all lesions include both solid and cystic components [18,19,20]. Based on our findings, SPN on the image may also present pure cystic component, largely cystic and rarely solid component, largely solid and rarely cystic component, or pure solid component. These atypical lesions may characterize as PNET, MCN, PDAC, gastrointestinal stroma tumors, or other unspecified solid tumors [21, 22]. Calcification is also reported in the tumor, and its presence may aid in diagnosis [3]. Recently, radiomics has also been applied in the differential diagnosis of SPN [23, 24]. In addition, endoscopic ultrasound is useful for differentiating SPN from other tumors [25]. Combination with fine needle aspiration could increase the pre-operative diagnostic yield of SPN [26], without increasing the risk of metastasis and recurrence [27].
For the treatment for the patients with SPN, operation is a priority for the primary and metastatic lesion. Routine lymphadenectomy has been shown to be unnecessary for the disease [5,6,7]. In recent years, the incidence of parenchyma-preserving surgery has increased, which means endocrine and exocrine function are more reserved [13]. Liu et al. compared enucleation with conventional pancreatectomy [19]. They observed that enucleation had a shorter operation duration, less blood loss, lower rate of exocrine insufficiency, and comparable morbidity, with no increased risk of tumor recurrence than conventional pancreatectomy. In this study, we included patients experiencing enucleation and MSP in the parenchyma-preserving surgery group. This classification was appropriate since pancreatic parenchyma was utmost preserved with enucleation and MSP. We found patients in parenchyma-preserving surgery group experience less endocrine insufficiency containing diabetes deterioration and new-onset diabetes mellitus and has less complaints of fatty stools and unintentional weight loss reflecting exocrine insufficiency. Even in this case, control of risk factors for diabetes mellitus as well as early detection and management may reduce the burden of endocrine insufficiency and its complications [28]. Meanwhile, pancreatic enzyme supplementation, especially correct dosing or intake of pancreatic enzymes, contributes to the prevention of exocrine insufficiency [29]. Besides, compared with those in the regular pancreatectomy group, patients in the parenchyma-preserving surgery group had smaller tumor sizes and fewer lymph nodes, with no significant difference observed among the other pathological parameters including the number of lymph node metastasis, Ki-67 index, angioinvasion, or nerve infiltration. Moreover, the incidence of perioperative complications and recurrence did not increase in the parenchyma-preserving surgery group. Furthermore, the adoption of minimally invasive techniques increased [13]. Data of Mou et al. revealed that laparoscopy DP for SPN had short-term benefits including first flatus time, diet onset time, and postoperative hospital stay compared with open DP [30]. Long-term outcomes of laparoscopic DP were identical to those of open DP. This is consistent with another single center [31]. Robot approach is likely to be useful in laparoscopic parenchyma-preserving surgery and more experience of robot-assisted pancreatectomy are needed. Based on our experience and existed studies, surgical choice is determined by a combination of several factors. Preoperative diagnosis should be as precise as possible. In the condition that preoperative imaging is highly suspected of SPN or pathology results have been obtained, parenchyma-preserving pancreatectomy might be possible. If a patient is diagnosed preoperatively with SPN or pancreatic cancer without pathological evidence, regular pancreatectomy and routine lymph node dissection, rather than parenchyma-preserving surgery, might be performed for safety. In addition, it is noteworthy that the final surgical strategy may be influenced by abdominal exploration and the surgeon's preference and experience [6]. The location and size of tumor have influence on surgical choice. For example, if tumor located in pancreatic head is too large or close to the intrapancreatic bile duct, parenchyma-preserving surgery might not be performed due to increased risk of biliary and pancreatic fistula. For tumor located in the neck or body, parenchyma-preserving surgery is more likely to be performed. Middle segment pancreatectomy is a prior choice if residual parenchyma of pancreas distal to the expected left pancreatic transection plane was enough. Enucleation could be performed when tumor located on the surface of the pancreas and is not closely related to the pancreatic duct. Thus, parenchyma-preserving surgery and a minimally invasive approach may be preferable if comprehensive conditions allow. Adjuvant chemotherapy or radiotherapy is an alternative for patients when the operation is unsuccessful [7]. However, no consensus has been achieved, and additional evidence is required to justify the role of adjuvant radiotherapy or chemotherapy.
The prognosis of patients with SPN is quite favorable with 5-year and 10-year survival rates [31]. The surviving patients had a median follow-up duration of 31 months in this study. However, the probability of recurrence and metastasis remained to exist. The incidence of recurrence and distant metastasis varies among reported cohorts, ranging from 0% to more than 10% [20, 21]. Two large sample-sized meta-analyses revealed recurrence rates of 2.6% and 3.5%, respectively. Within the first 5 years following operation, SPN most frequently recurs and spreads to distant organs, with the liver being the most common site [8]. In our study, except for 18 patients who lost follow-up, three patients (1.7%) had a relapse at 6, 12, and 39 months, respectively, following initial operation. All three patients had metastatic lesions in the liver and underwent radiofrequency ablation. One of them relapsed and required liver resection. No deaths owing to relapse were recorded among them at the last follow-up. No consensus has been reported on risk factors for recurrence and metastasis so far. The most addressed pathological risk factors were tumor size and the Ki-67 index. Overall, larger tumor diameter predicted a poor prognosis with different cutoff value [13, 32]. A meta-analysis by Fu et al. indicated that the gradual increase in Ki-67 index is associated with the risk of malignancy in SPN [33] and Ki-67 > 4% might be an adverse prognostic factor in their own data [34], which is inconsistent with classification for pancreatic neuroendocrine neoplasia. Our study observed tumor size as a risk factor for metastasis rather than the Ki-67 index. Besides, recurrence might be more common when tumors are associated with other pathological features including lymph node metastasis, tumor cell infiltration of the peripancreatic adipose tissue, lymphangion invasion, neural invasion, and tumor necrosis [13, 21, 35]. Angioinvasion and nerve infiltration were risk factors of metastasis based on our data. However, margins status is not a risk factor [36], consistent with our observation. In patients with underlying risk factors for recurrence and metastasis, a relatively long follow-up is recommended.
To our knowledge, this is one of the few single-center retrospective studies on SPN comparing perioperative safety and outcome of patients classified based on parenchyma-preserving pancreatectomy and regular pancreatectomy. We also evaluated CT images of SPN to improve diagnosis and analyzed risk factors predicting metastasis and recurrence of SPN to guide follow-up. However, this study had several limitations. All data were collected retrospectively from a single center. The inherent bias of retrospective collection was inevitable and the results might be influenced by center-specific practices. Due to small number of metastasis, several risk factors for metastasis might not expose in this study. Moreover, the two groups in this study were based on whether the operative method itself preserved the parenchyma or not. The extent of parenchyma preservation was not quantified. Patients were not equally clarified into two groups. Fox example, patients with large tumor located in pancreatic head or patients with tumor close to the splenic hilum could only undergo regular pancreatectomy. This might reduce comparability to some extent. Other limitations of our study included a paucity of data on long-term complications and molecular pathogenesis. Overall, these limitations indicate that more comprehensive facts should be studied further.
Conclusively, parenchyma-preserving surgery did not significantly increase the incidence of perioperative complications and recurrence and is preferable if comprehensive conditions permit.
Availability of data and materials
Data supporting the findings of this study are available from the respective authors upon reasonable request.
References
Frantz V: Tumors of the pancreas: Atlas of tumor Pathology. Afip 1959.
Hackeng WM, Hruban RH, Offerhaus GJ, Brosens LA. Surgical and molecular pathology of pancreatic neoplasms. Diagn Pathol. 2016;11:47.
Yao J, Song H. A Review of Clinicopathological Characteristics and treatment of solid pseudopapillary tumor of the pancreas with 2450 cases in Chinese population. Biomed Res Int. 2020;2020:2829647.
Wu J, Mao Y, Jiang Y, Song Y, Yu P, Sun S, Li S. Sex differences in solid pseudopapillary neoplasm of the pancreas: a population-based study. Cancer Med. 2020;9:6030–41.
Tipton SG, Smyrk TC, Sarr MG, Thompson GB. Malignant potential of solid pseudopapillary neoplasm of the pancreas. Br J Surg. 2006;93:733–7.
Hao CY, Lu AP, Xing BC, Huang XF, Gao F, Ji JF. Solid pseudopapillary tumor of the pancreas: report of 8 cases in a single institution and review of the Chinese literature. Pancreatology. 2006;6:291–6.
Romics L Jr, Oláh A, Belágyi T, Hajdú N, Gyurus P, Ruszinkó V. Solid pseudopapillary neoplasm of the pancreas–proposed algorithms for diagnosis and surgical treatment. Langenbecks Arch Surg. 2010;395:747–55.
Yepuri N, Naous R, Meier AH, Cooney RN, Kittur D, Are C, Jain A, Dhir M. A systematic review and meta-analysis of predictors of recurrence in patients with Solid Pseudopapillary Tumors of the Pancreas. HPB (Oxford). 2020;22:12–9.
Wei J, Liu X, Wu J, Xu W, Zhou J, Lu Z, Chen J, Guo F, Gao W, Li Q, et al: Modified one-layer duct-to-mucosa pancreaticojejunostomy reduces pancreatic fistula after pancreaticoduodenectomy. Int Surg 2015.
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20–5.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161:584–91.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761–8.
Kang CM, Choi SH, Kim SC, Lee WJ, Choi DW, Kim SW. Predicting recurrence of pancreatic solid pseudopapillary tumors after surgical resection: a multicenter analysis in Korea. Ann Surg. 2014;260:348–55.
Papavramidis T, Papavramidis S. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. J Am Coll Surg. 2005;200:965–72.
La Rosa S, Bongiovanni M. Pancreatic solid pseudopapillary neoplasm: key pathologic and genetic features. Arch Pathol Lab Med. 2020;144:829–37.
Patil TB, Shrikhande SV, Kanhere HA, Saoji RR, Ramadwar MR, Shukla PJ. Solid pseudopapillary neoplasm of the pancreas: a single institution experience of 14 cases. HPB (Oxford). 2006;8:148–50.
Mortenson MM, Katz MH, Tamm EP, Bhutani MS, Wang H, Evans DB, Fleming JB. Current diagnosis and management of unusual pancreatic tumors. Am J Surg. 2008;196:100–13.
Song H, Dong M, Zhou J, Sheng W, Zhong B, Gao W. Solid pseudopapillary neoplasm of the pancreas: clinicopathologic feature, risk factors of malignancy, and survival analysis of 53 cases from a single center. Biomed Res Int. 2017;2017:5465261.
Wang X, Chen YH, Tan CL, Zhang H, Xiong JJ, Chen HY, Ke NW, Liu XB. Enucleation of pancreatic solid pseudopapillary neoplasm: short-term and long-term outcomes from a 7-year large single-center experience. Eur J Surg Oncol. 2018;44:644–50.
Guo T, Wang L, Xie P, Zhang Z, Yu Y. Diagnosis and surgical treatment and pathological findings of solid pseudopapillary tumor of the pancreas: a single-institution experience. Cancer Manag Res. 2020;12:581–8.
Tjaden C, Hassenpflug M, Hinz U, Klaiber U, Klauss M, Büchler MW, Hackert T. Outcome and prognosis after pancreatectomy in patients with solid pseudopapillary neoplasms. Pancreatology. 2019;19:699–709.
Deniz K, Arıkan TB, Başkol M, Karahan Ö. Solid Pseudopapillary Neoplasm of the Pancreas. J Gastrointest Surg. 2021;25:322–4.
Shi YJ, Zhu HT, Liu YL, Wei YY, Qin XB, Zhang XY, Li XT, Sun YS. Radiomics analysis based on diffusion kurtosis imaging and T2 weighted imaging for differentiation of pancreatic neuroendocrine tumors from solid pseudopapillary tumors. Front Oncol. 2020;10:1624.
Gu H, Liang H, Zhong J, Wei Y, Ma Y. How does the pancreatic solid pseudopapillary neoplasm confuse us: Analyzing from the point view of MRI-based radiomics? Magn Reson Imaging. 2022;85:38–43.
Kataoka K, Ishikawa T, Ohno E, Mizutani Y, Iida T, Furukawa K, Nakamura M, Honda T, Ishigami M, Kawashima H, et al. Differentiation between solid pseudopapillary neoplasm of the pancreas and nonfunctional pancreatic neuroendocrine neoplasm using endoscopic ultrasound. Pancreas. 2022;51:106–11.
Law JK, Stoita A, Wever W, Gleeson FC, Dries AM, Blackford A, Kiswani V, Shin EJ, Khashab MA, Canto MI, et al. Endoscopic ultrasound-guided fine needle aspiration improves the pre-operative diagnostic yield of solid-pseudopapillary neoplasm of the pancreas: an international multicenter case series (with video). Surg Endosc. 2014;28:2592–8.
Karsenti D, Caillol F, Chaput U, Perrot B, Koch S, Vuitton L, Jacques J, Valats JC, Poincloux L, Subtil C, et al. Safety of endoscopic ultrasound-guided fine-needle aspiration for pancreatic solid pseudopapillary neoplasm before surgical resection: a european multicenter registry-based study on 149 patients. Pancreas. 2020;49:34–8.
Kusakabe J, Anderson B, Liu J, Williams GA, Chapman WC, Doyle MMB, Khan AS, Sanford DE, Hammill CW, Strasberg SM, et al. Long-term endocrine and exocrine insufficiency after pancreatectomy. J Gastrointest Surg. 2019;23:1604–13.
Latenstein AEJ, Blonk L, Tjahjadi NS, de Jong N, Busch OR, de Hingh I, van Hooft JE, Liem MSL, Molenaar IQ, van Santvoort HC, et al. Long-term quality of life and exocrine and endocrine insufficiency after pancreatic surgery: a multicenter, cross-sectional study. HPB (Oxford). 2021;23:1722–31.
Zhang RC, Yan JF, Xu XW, Chen K, Ajoodhea H, Mou YP. Laparoscopic vs open distal pancreatectomy for solid pseudopapillary tumor of the pancreas. World J Gastroenterol. 2013;19:6272–7.
Kang CM, Choi SH, Hwang HK, Lee WJ, Chi HS. Minimally invasive (laparoscopic and robot-assisted) approach for solid pseudopapillary tumor of the distal pancreas: a single-center experience. J Hepatobiliary Pancreat Sci. 2011;18:87–93.
Wang WB, Zhang TP, Sun MQ, Peng Z, Chen G, Zhao YP. Solid pseudopapillary tumor of the pancreas with liver metastasis: clinical features and management. Eur J Surg Oncol. 2014;40:1572–7.
Zou C, Yang F, Fu D. Meta-analysis of Ki-67 expression for recurrence in patients with solid pseudopapillary tumor of the pancreas. HPB (Oxford). 2020;22:631–2.
Yang F, Yu X, Bao Y, Du Z, Jin C, Fu D. Prognostic value of Ki-67 in solid pseudopapillary tumor of the pancreas: Huashan experience and systematic review of the literature. Surgery. 2016;159:1023–31.
Xu Y, Zhao G, Pu N, Nuerxiati A, Ji Y, Zhang L, Rong Y, Lou W, Wang D, Kuang T, et al. One hundred twenty-one resected solid pseudopapillary tumors of the pancreas: an 8-year single-institution experience at Zhongshan Hospital, Shanghai. China Pancreas. 2017;46:1023–8.
Butte JM, Brennan MF, Gönen M, Tang LH, D'Angelica MI, Fong Y, Dematteo RP, Jarnagin WR, Allen PJ: Solid pseudopapillary tumors of the pancreas. Clinical features, surgical outcomes, and long-term survival in 45 consecutive patients from a single center. J Gastrointest Surg 2011, 15:350–357.
Funding
This work was supported by the grant from the National Natural Science Foundation of China (82173206).
Author information
Authors and Affiliations
Contributions
Conceptualization (WJL, CJM), methodology (WJL, JKR), formal analysis (GY, GF), data curation (GY, LZP, XCH, WJS), writing—original draft (GY), writing—review and editing (GF, CJM), visualization (GY), funding acquisition (MY). All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gao, Y., Guo, F., Lu, Z. et al. Perioperative safety and prognosis following parenchyma-preserving surgery for solid pseudopapillary neoplasm of the pancreas. World J Surg Onc 21, 119 (2023). https://doi.org/10.1186/s12957-023-03003-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-03003-y