Abstract
Background
Esophageal squamous cell carcinoma (ESCC) is a highly malignant neoplasm. DNA-damaging drugs, such as cisplatin (CDDP) and 5-fluorouracil (5-FU), are most frequently used in preoperative chemotherapy for ESCC. However, the response to preoperative chemotherapy varies among patients. p53, encoded by TP53, participates in apoptotic pathways following chemotherapy with DNA-damaging drugs, and mutation of TP53 contributes to chemoresistance. Organic cation transporter 1 (OCT1) participates in the uptake of CDDP, and its reduced expression is associated with CDDP resistance. The aim of this study was to evaluate the predictive impact of the expression status of p53 and OCT1 in response to preoperative chemotherapy in ESCC.
Methods
We retrospectively assessed 66 ESCC patients who received preoperative chemotherapy with CDDP/5-FU (CF) or docetaxel/CDDP/5-FU (DCF). p53 and OCT1 expression in pretreatment biopsy specimens was immunohistochemically determined and correlated with histological response to preoperative chemotherapy.
Results
p53 with wild-type (p53WT-ex) and mutant-type (p53MT-ex) expression patterns was identified in 40.9% and 59.1% of patients, respectively. High expression of OCT1 (OCT1High) was detected in 45.5%, and the remaining 54.5% showed low expression (OCT1Low). In a univariate analysis of the entire cohort, p53MT-ex was significantly correlated with poor response (P = 0.026), whereas OCT1Low showed marginal significance (P = 0.091). In a combined analysis, tumors with either p53MT-ex or OCT1Low showed a significant correlation with poor response compared with tumors with both p53WT-ex and OCT1High (P < 0.001). The sensitivity, specificity, and accuracy of combined p53/OCT1 were 93.9%, 47.1%, and 81.8%, respectively. Multivariate analysis identified p53 (P = 0.017), OCT1 (P = 0.032), and combined p53/OCT1 (P < 0.001) as independent predictors of histological response. When samples were stratified according to chemotherapy regimen in the univariate analysis, combined p53/OCT1 was the only significant factor for poor response in the CF (P = 0.011) and DCF (P = 0.021) groups, whereas p53 showed no statistical significance.
Conclusions
Our results suggest that either p53MT-ex or OCT1Low expression in pretreatment biopsy specimens may be a potential predictor of poor response to preoperative chemotherapy with the CF-based regimens in ESCC, although the specificity needs to be improved.
Similar content being viewed by others
Background
Esophageal cancer is the seventh most common cancer and the sixth leading cause of cancer deaths worldwide [1]. Preoperative chemotherapy followed by surgery is an effective treatment for advanced esophageal squamous cell carcinoma (ESCC) [2]. Among several chemotherapy regimens, cisplatin (CDDP)/5-fluorouracil (5-FU) (CF) and docetaxel (DTX)/CDDP/5-FU (DCF) are promising regimens [3,4,5], and cytotoxic drugs remain the mainstay of treatment for ESCC. However, the therapeutic effects of preoperative chemotherapy vary among patients, and satisfactory treatment outcomes cannot be obtained in a proportion of patients [3,4,5]. Therefore, the identification of predictors of response to preoperative chemotherapy may help to avoid the administration of ineffective anticancer drugs that have unpleasant side effects as well as mitigate the risk of delaying surgery in patients who do not respond to preoperative chemotherapy. However, no such predictors have been established for ESCC.
p53, which is encoded by TP53, is a tumor suppressor that plays a pivotal role in regulating cell proliferation [6,7,8]. p53 is activated by cellular stress that leads to DNA damage, hypoxia, and oncogene activation and induces either cell-cycle arrest to allow DNA repair or apoptosis to remove the damaged cells. However, TP53 is mutated in more than 50% of human cancers, including at least 40% of esophageal cancers [9,10,11,12], resulting in the disruption of its protective tumor-suppressor functions [7]. DNA-damaging drugs, such as CDDP and 5-FU, act by inducing DNA damage, which is a potent trigger for activation of TP53 [6, 13, 14]. Therefore, functional inactivation of p53 by mutation could be associated with resistance to DNA-damaging chemotherapy.
The effectiveness of chemotherapy is also dependent on the intracellular accumulation of anticancer drugs. Cellular uptake of anticancer drugs is mediated by facilitated transport systems via solute carrier (SLC) transporters, suggesting that the expression of SLC transporters may help to predict the response to chemotherapy [15,16,17,18]. The organic cation transporters (OCTs) of the SLC22A family consist of three isoforms, OCT1, OCT2, and OCT3, which mediate the uptake transport of various organic cations including endogenous compounds, xenobiotics, and anticancer drugs [15,16,17,18]. An in vitro study demonstrated that transfection of OCT1 increased the accumulation and cytotoxicity of CDDP in human embryonic kidney cells [19], although another study presented results that were negative for the involvement of OCT1 in the accumulation and cytotoxicity of CDDP [20]. Furthermore, it was reported that OCT1 silencing impaired the cytotoxic effects of CDDP in ESCC cells, and that the level of OCT1 mRNA expression was downregulated in CDDP-resistant ESCC cells [21]. However, the clinical significance of OCT1 in ESCC, including its correlation with chemotherapeutic effects, remains to be elucidated.
Considering the above data, we speculated that a tumor-specific expression pattern of p53 and OCT1 could have a potential impact for predicting the effects of preoperative chemotherapy in ESCC. Therefore, we evaluated the expression status of p53 and OCT1 in the pretreatment biopsy specimens of patients with ESCC receiving preoperative chemotherapy and analyzed their correlation with response to preoperative chemotherapy.
Methods
Patients and tissue samples
This was a retrospective observational study. A total of 95 esophageal cancer patients with clinical stages (cStages) II to IVa were treated with preoperative chemotherapy followed by esophagectomy and regional lymph node dissection at Fujita Health University Hospital from 2013 to 2021. No patients received adjuvant therapy until relapse occurred. Four adenocarcinoma patients were excluded from the present study because critical molecular differences underlying ESCC and esophageal adenocarcinoma have been demonstrated in comprehensive genomic analyses [22]. Moreover, 25 patients were excluded because the tissue specimens were too small for immunohistochemical analysis, and thus, the remaining 66 ESCC patients were included in the present study.
Biopsy specimens with multiple samples (median, 3; range 2–7) obtained before preoperative chemotherapy (pretreatment biopsy specimens) and resection materials obtained after preoperative chemotherapy (posttreatment resection materials) were fixed in 10% neutral buffered formalin and embedded in paraffin. Three-micrometer-thick sections were cut, mounted on aminopropyltriethoxysilane-coated slides, and stained with hematoxylin and eosin (H&E) to assess the histological response to preoperative chemotherapy. All the patients provided written informed consent regarding the use of their tissue specimens, and this study was conducted with the approval of the ethics committees of Fujita Health University School of Medicine and Kobe University Graduate School of Health Sciences (reference numbers HM20-146 and 980, respectively).
Chemotherapy regimen
All patients had a performance status of 0 or 1. Forty-seven patients with cStage II or III disease received the CF regimen, which consisted of CDDP 80 mg/m2 administered as a 2-h intravenous infusion on day 1 and 5-FU 800 mg/m2 as a 24-h continuous infusion on days 1–5 of a 21-day cycle. The remaining 19 patients with cStage III or IVa received the DCF regimen, which consisted of DTX 70 mg/m2 administered as a 1-h intravenous infusion on day 1, CDDP 70 mg/m2 as a 2-h intravenous infusion on day 1, and 5-FU 750 mg/m2 as a 24-h continuous infusion on days 1–5 of a 21-day cycle.
Two cycles of these regimens were administered. For patients who had or seemed to have adjacent organ invasion, two additional cycles were performed depending on their responsiveness to preoperative chemotherapy and the resectability of their tumor. Surgery was conducted approximately 4–6 weeks after the end of preoperative chemotherapy.
Assessment of tumor response to preoperative chemotherapy
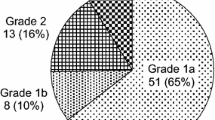
Histological response to preoperative chemotherapy was evaluated according to the proportion of viable cells in whole tumor tissue on H&E-stained sections of the posttreatment resection materials, according to the Japanese Classification of Esophageal Cancer, 11th edition [23], as follows: grade 0, no effect (no therapeutic effect is recognized in cancer cells and tissues); grade 1, slight effect (grade 1a, viable cancer cells occupy two-thirds or more of the entire tumor area; grade 1b, viable cancer cells remain in more than one-third but less than two-thirds of the entire tumor area); grade 2, considerable effect (viable cancer cells remain in less than one-third of the entire tumor area); and grade 3, complete response (no viable cancer cells remain). The response of tumors with grades 1b, 2, and 3 was judged as a “good response,” and that of tumors with grades 0 and 1a as a “poor response,” in accordance with previous studies [24].
Immunostaining
Sections were deparaffinized in xylene, rehydrated in graded alcohol, and immersed in 0.3% hydrogen peroxide in methanol for 10 min to block endogenous peroxidase activity. Heat-induced antigen retrieval (HIAR) was performed in an electric pressure cooker for 5 min in 10 mM citrate buffer (pH 6.0) for p53 and 10 mM Tris base containing 1 mM ethylenediaminetetraacetic acid (pH 9.0) for OCT1. After HIAR, the sections were cooled to room temperature (RT) for 25 min. The sections were rinsed with 50 mM Tris-buffered saline (TBS, pH 7.6) and incubated with mouse monoclonal anti-p53 (1:100 dilution, clone DO-7; Dako, Glostrup, Denmark) or mouse monoclonal anti-OCT1 (1:2000 dilution, clone 2C5; Novus Biologicals, Centennial, CO, USA) primary antibodies overnight at RT. After rinsing with TBS, sections for p53 staining were incubated with anti-mouse horseradish peroxidase polymer (Histofine Simple Stain MAX-PO; Nichirei Bioscience, Tokyo, Japan) for 1 h at RT. Sections for OCT1 staining were incubated with post-primary block for 30 min at RT, rinsed with TBS, and then incubated with Novolink polymer (Novolink Polymer Detection Systems; Leica Microsystems, Wetzlar, Germany) for 30 min at RT. Sections were then rinsed again with TBS, and the reaction products were developed with a diaminobenzidine solution (Dako). Finally, sections were lightly counterstained with Mayer’s hematoxylin, dehydrated in graded alcohol, cleared in xylene, and coverslipped. Positive controls were sections of colon cancer for p53 and normal liver for OCT1. The primary antibody was replaced with TBS containing 1% bovine serum albumin to provide a negative control.
Assessment of immunostaining results
The immunostained sections were reviewed by three investigators (MI, TD, and SK) who were blinded to the clinical data. If a disagreement in the scores occurred, the slides were reviewed again, and a consensus was reached. Nuclear staining of p53 was considered positive. Mutation of TP53 leads to excessive accumulation or loss of p53 protein, and thus, both positive staining in the majority of tumor cells and completely negative staining could be associated with TP53 mutation [25]. Therefore, we considered that positive staining in ≤ 70% of tumor cells was wild-type expression of p53 (p53WT-ex), and positive staining in > 70% of tumor cells or completely negative staining was mutant-type expression of p53 (p53MT-ex) [26].
Membranous staining of OCT1 was considered positive. OCT1 expression levels were assessed according to the intensity and percentage of the positive tumor cells. The staining intensity was graded as follows: score 0 (negative), score 1 (weak), score 2 (moderate), and score 3 (strong). The percentage of positive tumor cells was classified as follows: score 0 (none), score 1 (1%–10%), score 2 (11%–50%), and score 3 (> 50%). Furthermore, the immunoreactive score was calculated by adding the intensity score to the percentage score (0–6). Tumors with an immunoreactive score of 0–3 were designated as “low” (OCT1Low) and tumors with an immunoreactive score of 4–6 as “high” (OCT1High).
Statistical analysis
Correlations between two variables were estimated using Fisher’s exact test. Multivariate analysis using a logistic regression model was performed to identify independent predictors of histological response. Parameters with a P-value of < 0.2 in the univariate analysis were included in the multivariate analysis. P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS Statistics 28 software (IBM Corp., Armonk, NY, USA).
Results
Patients’ characteristics
The pretreatment characteristics of patients and tumors are provided in Table 1. This study included 51 men and 15 women with a median age of 67 years (range, 38–79 years). The primary tumor location was the upper thoracic esophagus in eight patients, middle thoracic esophagus in 38 patients, lower thoracic esophagus in 18 patients, and abdominal esophagus in two patients. Regarding histological type, 12 tumors were well differentiated, 42 were moderately differentiated, 7 were poorly differentiated, and 5 were basaloid squamous cell carcinoma. The clinical T factors were cT1 in 2 patients, cT2 in 20 patients, cT3 in 32 patients, and cT4 in 12 patients. Forty-nine patients had lymph node metastasis (clinical N factors were cN1 in 21 patients, cN2 in 19 patients, cN3 in 8 patients, and cN4 in 1 patient). Eighteen patients had cStage II disease, 32 patients had cStage III, and 16 patients had cStage IVa.
Forty-seven patients received preoperative chemotherapy with the CF regimen, and the remaining 19 patients received the DCF regimen. Patients with higher advanced cT and cStage were more frequently included in the DCF group than in the CF group (P = 0.019 and P < 0.001, respectively). No significant differences in other characteristics were detected between the CF and DCF groups.
Expression of p53 and OCT1
Representative staining patterns of p53 and OCT1 in pretreatment biopsy specimens are shown in Figs. 1 and 2, respectively. p53 was expressed in the nucleus, and OCT1 showed membranous staining. p53WT-ex was observed in 27 (40.9%) of 66 tumors, and the remaining 39 (59.1%) tumors were p53MT-ex (28 tumors had positive staining in > 70% of tumor cells, and 11 tumors showed completely negative staining). OCT1High and OCT1Low were observed in 30 (45.5%) and 36 (54.5%) tumors, respectively. No significant correlation of expression status was observed between p53 and OCT1 (r = –0.079; P = 0.530). p53-positive cells were scattered in the basal layer of nonneoplastic esophageal epithelia. Epithelial cells in the middle and basal layers of nonneoplastic esophageal epithelia showed weak or negative staining of OCT1. In the negative control slides, no positive reaction was observed.
Representative immunostaining patterns of p53 in pretreatment biopsy specimens from ESCC patients. A Wild-type expression of p53 with heterogeneous staining, B mutant-type expression of p53 with homogeneous (diffuse) staining, and C mutant-type expression of p53 with completely negative staining. p53 staining was observed in the nuclei of tumor cells (A, B)
Representative immunostaining patterns of OCT1 in pretreatment biopsy specimens from ESCC patients. A High expression of OCT1, with a large number of positive tumor cells, and B low expression of OCT1, with only a few positive tumor cells (arrows). OCT1 staining was observed in the cell membranes of tumor cells
Correlation between expression status of p53 or OCT1 and clinicopathological characteristics
Table 2 shows the correlation between the expression status of p53 or OCT1 in pretreatment biopsy specimens and clinicopathological characteristics. No significant correlation was found between the expression status of p53 and OCT1 and the clinicopathological parameters of the patients.
Correlation of p53 and OCT1 expression status with histological response in the entire cohort
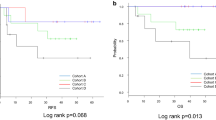
A histological complete response (grade 3) in posttreatment resection materials was achieved in 5 tumors. Grade 2 was achieved in 5 tumors (Fig. 3A), 9 tumors were grade 1b, 45 tumors were grade 1a, and 4 tumors were grade 0 (Fig. 3B). The endoscopic findings of a tumor with a histological grade 2 response are shown in Fig. 4. Table 3 shows the correlation of clinicopathological parameters or the expression status of p53 and OCT1 in the pretreatment biopsy specimens with histological response in the entire cohort. In the univariate analysis, no correlation with histological response was detected for age, sex, tumor location, histological type, clinical T factor, clinical N factor, clinical stage, or chemotherapy regimen, whereas p53MT-ex was significantly correlated with poor response. Indeed, 33 (84.6%) of the 39 tumors with p53MT-ex and 16 (59.3%) of the 27 tumors with p53WT-ex showed a poor response (P = 0.026). Interestingly, all 11 tumors with completely negative staining showed a poor response. The sensitivity of p53 expression for predicting poor response was 67.3% (33 tumors with p53MT-ex out of the 49 poorly responsive tumors), and the specificity was 64.7% (11 tumors with p53WT-ex out of the 17 responsive tumors). The accuracy was 66.7%, 44 (33 poorly responsive tumors with p53MT-ex and 11 responsive tumors with p53WT-ex) out of the 66 tumors. OCT1Low was marginally correlated with poor response (P = 0.091).
Multiple biological processes are involved in tumor response to chemotherapy, and therefore, we also investigated the combination of p53 and OCT1 expression. Poor response was observed in 46 (83.6%) of the 55 tumors with either p53MT-ex or OCT1Low expression and 3 (27.3%) of the 11 tumors with both p53WT-ex and OCT1High (P < 0.001: a higher level of statistical significance compared with p53 alone). The sensitivity of combined p53/OCT1 for predicting poor response was 93.9% (46 tumors with either p53MT-ex or OCT1Low out of the 49 poorly responsive tumors), and the specificity was 47.1% (8 tumors with both p53WT-ex and OCT1High out of the 17 responsive tumors). The accuracy was 81.8%: 54 (46 poorly responsive tumors with either p53MT-ex or OCT1Low and 8 responsive tumors with both p53WT-ex and OCT1High) out of the 66 tumors. Combined p53/OCT1 had higher sensitivity and accuracy but lower specificity compared with p53 alone.
Multivariate analysis of predictors of histological response in the entire cohort
p53 expression and combined p53/OCT1 were not included in the same multivariate model to avoid multicollinearity (Table 4). Patient sex and p53 and OCT1 expression were included in Model 1, and patient sex and combined p53/OCT1 was included in Model 2. p53 expression (odds ratio [OR], 2.16; 95% confidence interval [CI], 1.15–4.07; P = 0.017), OCT1 (OR, 2.02; 95% CI, 1.06–3.85; P = 0.032), and combined p53/OCT1 (OR, 3.79; 95% CI, 1.75–8.21; P < 0.001; the highest level of statistical significance) were significant predictors of histological response. However, patient sex was not identified as an independent predictor of histological response.
Correlation of the expression status of p53 and OCT1 with histological response according to chemotherapy regimen
We attempted to perform further analyses in which CF and DCF groups were assessed separately. In the CF group (n = 47), p53 (P = 0.165) and OCT1 (P = 0.318) expression did not correlate with histological response (Table 5). However, when evaluated according to the combination of p53 and OCT1 data, a poor response was observed in 33 (84.6%) of the 39 tumors with either p53MT-ex or OCT1Low and 3 (37.5%) of the 8 tumors with both p53WT-ex and OCT1High (P = 0.011). No other parameters were correlated with histological response. Because the parameters with P<0 .2 were p53 alone and combined p53/OCT1, we did not perform the multivariate analysis.
Combined p53/OCT1 was also the only significant parameter in the DCF group, although the values should only be used as references because of the small number of cases (n = 19): a poor response was observed in 13 (81.3%) of the 16 tumors with either p53MT-ex or OCT1Low and in none of the 3 tumors with both p53WT-ex and OCT1High (P = 0.021).
Discussion
Although preoperative chemotherapy with the CF-based (CF and DCF) regimens has been established as an effective therapy for ESCC patients, the treatment outcomes remain unsatisfactory [3,4,5]. Therefore, the identification of predictive biomarkers is important for selecting subgroups of patients who will be responsive or unresponsive to preoperative chemotherapy. In this study, we evaluated whether response to preoperative chemotherapy for ESCC could be predicted by immunohistochemical staining of p53 and OCT1 in pretreatment biopsy specimens.
We found that p53MT-ex, which is used as a surrogate marker of TP53 mutation, was significantly correlated with poor response in the univariate (P = 0.026) and multivariate (P = 0.017) analyses of the entire cohort. The value of p53 protein expression for predicting response to preoperative chemotherapy in ESCC remains controversial. Several studies suggested a higher response rate of p53-negative tumors to preoperative chemotherapy than p53-positive tumors [24, 27, 28], while others reported no significant difference in responsiveness between p53-positive and p53-negative tumors [10, 29,30,31]. Conversely, data from TP53 mutation analyses indicated the correlation of TP53 mutation and poor response to preoperative chemotherapy [10, 32].
Generally, it is accepted that wild-type p53 has a short half-life, which makes it immunohistochemically undetectable [33]. In contrast, mutation of TP53 increases the half-life of p53 protein, leading to nuclear accumulation of mutant-type p53, which is immunohistochemically detectable. However, p53-positive staining does not consistently indicate the presence of TP53 mutation, and negative staining does not represent the absence of abnormalities in TP53 [34, 35]. Indeed, previous studies demonstrated that the concordance rate between p53 protein expression and TP53 mutation in esophageal cancer was approximately 50% when staining of > 10% of tumor cells was regarded as positive [11, 12].
We would like to emphasize that the expression pattern of p53 protein, that is, the proportion of p53-positive cells, is of great importance in discussing the correlation between p53 protein expression and TP53 gene mutation [25, 33, 35]. A diffuse (homogeneous) expression pattern could correlate with TP53 mutation. Furthermore, completely negative staining should also be interpreted as being consistent with mutant-type p53 because the presence of null mutations, such as frameshift or nonsense mutations, could result in the complete absence of immunoexpression due to the abolishment of protein production [7, 25]. Conversely, a focal or heterogeneous expression pattern does not seem to be associated with obvious abnormalities of TP53. This may be explained by a non-mutational mechanism for p53 protein accumulation, such as inactivation of the p53 degradation process and spontaneous genetic errors [33, 34]. Therefore, in our study, p53 expression was classified into two groups: p53MT-ex (positive staining in > 70% of tumor cells or completely negative staining) versus p53WT-ex (positive staining in ≤ 70% of tumor cells) [26]. In previous studies, however, different criteria for determining p53 immunopositivity were provided. Several studies defined p53 positivity as nuclear staining in > 10% of the tumor cells [10, 24, 28] but others as nuclear staining in > 25% [30] or > 50% [31] of the tumor cells. In these criteria, however, completely negative staining is judged as consistent with wild-type p53, which may be an important cause of discordance between the p53 immunopositivity and the genetic abnormality. Importantly, in our study, completely negative staining was noted in 11 tumors, all of which showed a poor response. Taken together, a significant correlation between p53MT-ex and poor response to preoperative chemotherapy in the univariate analysis of our series may reflect the presence of mutant-type p53 that leads to the resistance to chemotherapy-induced apoptosis. However, our results must be confirmed by further studies using a TP53 mutational analysis, such as single-strand conformational polymorphism and direct sequencing.
Different regimens, doses, and courses of preoperative chemotherapy, different evaluation criteria of response to preoperative chemotherapy, and different staining protocols and sensitivity of p53 immunohistochemistry may result in conflicting results. Thus, standardization is necessary to obtain an accurate assessment of the significance of p53 expression in response to preoperative chemotherapy in ESCC.
An in vitro study demonstrated that OCT1 silencing impaired the cytotoxic effect of CDDP in ESCC cells, and that the level of OCT1 mRNA expression was downregulated in CDDP-resistant cells compared with the parental cells [11]. However, the movement of CDDP across membranes is greatly influenced not only by OCT1 but also by OCT2 and copper transporter 1 (CTR1) [15,16,17,18]. Although we investigated OCT2 and CTR1 as a preliminary examination, high expression of OCT2 and CTR1 was observed in only 6 and 2 of the 66 tumors, respectively (data not shown). These findings suggest that OCT1 may be a major CDDP-uptake transporter in ESCC. However, to our knowledge, no previous studies have investigated the predictive significance of OCT1 expression in response to preoperative chemotherapy in clinical ESCC samples. Therefore, in the present study, we assessed whether OCT1 expression in pretreatment biopsy specimens was significantly correlated with histological response to preoperative chemotherapy in ESCC. The correlation of OCT1 with histological response was marginal in the univariate analysis (P = 0.091) but significant in the multivariate analysis (P = 0.032). This suggests that the effects of preoperative chemotherapy for ESCC are difficult to predict by OCT1 alone because of its low levels of statistical significance.
Tumor response to chemotherapy is a multifactorial event, and therefore, a combination of biomarkers seems reasonable for accurately and/or reliably predicting the effectiveness of preoperative chemotherapy in ESCC. In this study, when p53 and OCT1 expression data were combined, either p53MT-ex or OCT1Low was a significant predictor of poor response in univariate and multivariate analyses of the entire cohort (univariate, P < 0.001; multivariate, P < 0.001), with higher levels of statistical significance compared with p53 alone, and in the univariate analysis of the CF group (P = 0.011) and the DCF group (P = 0.021). The poor responsiveness of tumors with either p53MT-ex or OCT1Low suggests that the restricted function of p53 and OCT1 may determine the decreased response through impairing the intracellular uptake of CDDP and/or drug-induced apoptosis. Conversely, combined p53/OCT1 had high sensitivity and accuracy, whereas the specificity was insufficient. The identification of additional biomarkers is required to improve the predictive specificity.
This retrospective study had several limitations: (1) the chemotherapy regimen included CF and DCF, (2) the patients were at different clinical stages, (3) this study was performed at a single institution and lacked TP53 gene analysis, and (4) the sample size was small, resulting in low statistical power. Therefore, our results are still exploratory. They should be interpreted cautiously and need to be confirmed in prospective studies of large patient cohorts at the same stage of disease and in patients receiving the same chemotherapy regimen.
Conclusions
This study suggests that either p53MT-ex or OCT1Low in pretreatment biopsy specimens may be a potential predictor of poor response to preoperative chemotherapy with the CF-based regimens in ESCC. Patients with p53MT-ex/OCT1Low tumors may be candidates for a more aggressive combination protocol or new drugs. However, several issues, particularly the insufficient specificity, need to be resolved.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- CDDP:
-
Cisplatin
- CF:
-
Cisplatin/5-fluorouracil
- CI:
-
Confidence interval
- CTR1:
-
Copper transporter 1
- DCF:
-
Docetaxel/cisplatin/5-fluorouracil
- ESCC:
-
Esophageal squamous cell carcinoma
- 5-FU:
-
5-fluorouracil
- HIAR:
-
Heat-induced antigen retrieval
- OCT1:
-
Organic cation transporter 1
- OCT1High :
-
High expression of organic cation transporter 1
- OCT1Low :
-
Low expression of organic cation transporter 1
- OR:
-
Odds ratio
- p53MT-ex :
-
Mutant-type expression pattern of p53
- p53WT-ex :
-
Wild-type expression pattern of p53
- RT:
-
Room temperature
- SLC:
-
Solute carrier
- TBS:
-
Tris-buffered saline
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Kitagawa Y, Uno T, Oyama T, Kato K, Kato H, Kawakubo H, et al. Esophageal cancer practice guidelines 2017 edited by the Japan Esophageal Society: part 1. Esophagus. 2019;16:1–24.
Medical Research Council Oesophageal Cancer Working Group. Surgical resection with or without preoperative chemotherapy in oesophageal cancer: a randomised controlled trial. Lancet. 2002;359:1727–33.
Ando N, Kato H, Igaki H, Shinoda M, Ozawa S, Shimizu H, et al. A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol. 2012;19:68–74.
Yamashita K, Katada N, Moriya H, Hosoda K, Mieno H, Katada C, et al. Neoadjuvant chemotherapy of triplet regimens of docetaxel/cisplatin/5-FU (DCF NAC) may improve patient prognosis of cStage II/III esophageal squamous cell carcinoma-propensity score analysis. Gen Thorac Cardiovasc Surg. 2016;64:209–15.
Harris CC. Structure and function of the p53 tumor suppressor gene: clues for rational cancer therapeutic strategies. J Natl Cancer Inst. 1996;88:1442–55.
Soussi T, Béroud C. Assessing TP53 status in human tumours to evaluate clinical outcome. Nat Rev Cancer. 2001;1:233–40.
Oren M. Decision making by p53: life, death and cancer. Cell Death Differ. 2003;10:431–42.
Hollstein MC, Metcalf RA, Welsh JA, Montesano R, Harris CC. Frequent mutation of the p53 gene in human esophageal cancer. Proc Natl Acad Sci U S A. 1990;87:9958–61.
Yamasaki M, Miyata H, Fujiwara Y, Takiguchi S, Nakajima K, Nishida T, et al. p53 genotype predicts response to chemotherapy in patients with squamous cell carcinoma of the esophagus. Ann Surg Oncol. 2010;17:634–42.
Coggi G, Bosari S, Roncalli M, Graziani D, Bossi P, Viale G, et al. p53 protein accumulation and p53 gene mutation in esophageal carcinoma. A molecular and immunohistochemical study with clinicopathologic correlations. Cancer. 1997;79:425–32.
Egashira A, Morita M, Yoshida R, Saeki H, Oki E, Sadanaga N, et al. Loss of p53 in esophageal squamous cell carcinoma and the correlation with survival: analyses of gene mutations, protein expression, and loss of heterozygosity in Japanese patients. J Surg Oncol. 2011;104:169–75.
Lowe SW, Bodis S, McClatchey A, Remington L, Ruley HE, Fisher DE, et al. p53 status and the efficacy of cancer therapy in vivo. Science. 1994;266:807–10.
Harrison DJ. Molecular mechanisms of drug resistance in tumours. J Pathol. 1995;175:7–12.
Cutler MJ, Choo EF. Overview of SLC22A and SLCO families of drug uptake transporters in the context of cancer treatments. Curr Drug Metab. 2011;12:793–807.
Sprowl JA, Mikkelsen TS, Giovinazzo H, Sparreboom A. Contribution of tumoral and host solute carriers to clinical drug response. Drug Resist Updat. 2012;15:5–20.
Li Q, Shu Y. Role of solute carriers in response to anticancer drugs. Mol Cell Ther. 2014;2:15.
Brecht K, Schäfer AM, Meyer Zu Schwabedissen HE. Uptake transporters of the SLC21, SLC22A, and SLC15A families in anticancer therapy-modulators of cellular entry or pharmacokinetics? Cancers (Basel). 2020;12:2263.
Yonezawa A, Masuda S, Yokoo S, Katsura T, Inui K. Cisplatin and oxaliplatin, but not carboplatin and nedaplatin, are substrates for human organic cation transporters (SLC22A1-3 and multidrug and toxin extrusion family). J Pharmacol Exp Ther. 2006;319:879–86.
Zhang S, Lovejoy KS, Shima JE, Lagpacan LL, Shu Y, Lapuk A, et al. Organic cation transporters are determinants of oxaliplatin cytotoxicity. Cancer Res. 2006;66:8847–57.
Lin R, Li X, Li J, Zhang L, Xu F, Chu Y, et al. Long-term cisplatin exposure promotes methylation of the OCT1 gene in human esophageal cancer cells. Dig Dis Sci. 2013;58:694–8.
Wang VE, Grandis JR, Ko AH. New strategies in esophageal carcinoma: translational insights from signaling pathways and immune checkpoints. Clin Cancer Res. 2016;22:4283–90.
Japan Esophageal Society. Japanese Classification of Esophageal Cancer, 11th Edition: part II and III. Esophagus. 2017;14:37–65.
Nakashima S, Natsugoe S, Matsumoto M, Kijima F, Takebayashi Y, Okumura H, et al. Expression of p53 and p21 is useful for the prediction of preoperative chemotherapeutic effects in esophageal carcinoma. Anticancer Res. 2000;20:1933–7.
Yemelyanova A, Vang R, Kshirsagar M, Lu D, Marks MA, Shih IM, et al. Immunohistochemical staining patterns of p53 can serve as a surrogate marker for TP53 mutations in ovarian carcinoma: an immunohistochemical and nucleotide sequencing analysis. Mod Pathol. 2011;24:1248–53.
Sakanashi F, Shintani M, Tsuneyoshi M, Ohsaki H, Kamoshida S. Apoptosis, necroptosis and autophagy in colorectal cancer: associations with tumor aggressiveness and p53 status. Pathol Res Pract. 2019;215:152425.
Shimada Y, Watanabe G, Yamasaki S, Maeda M, Kawabe A, Kaganoi JI, et al. Histological response of cisplatin predicts patients’ survival in oesophageal cancer and p53 protein accumulation in pretreatment biopsy is associated with cisplatin sensitivity. Eur J Cancer. 2000;36:987–93.
Kajiyama Y, Hattori K, Tomita N, Amano T, Iwanuma Y, Narumi K, et al. Histopathologic effects of neoadjuvant therapies for advanced squamous cell carcinoma of the esophagus: multivariate analysis of predictive factors and p53 overexpression. Dis Esophagus. 2002;15:61–6.
Lam KY, Law S, Ma LT, Ong SK, Wong J. Pre-operative chemotherapy for squamous cell carcinoma of the oesophagus: do histological assessment and p53 overexpression predict chemoresponsiveness? Eur J Cancer. 1997;33:1221–5.
Szumilo J, Chibowski D, Dąbrowski A. Assessment of the predictive value of clinical and histopathological factors as well as the immunoexpression of p53 and bcl-2 proteins in response to preoperative chemotherapy for esophageal squamous cell carcinoma. Dis Esophagus. 2000;13:191–7.
Yamamoto Y, Yamai H, Seike J, Yoshida T, Takechi H, Furukita Y, et al. Prognosis of esophageal squamous cell carcinoma in patients positive for human epidermal growth factor receptor family can be improved by initial chemotherapy with docetaxel, fluorouracil, and cisplatin. Ann Surg Oncol. 2012;19:757–65.
Kandioler D, Schoppmann SF, Zwrtek R, Kappel S, Wolf B, Mittlböck M, et al. The biomarker TP53 divides patients with neoadjuvantly treated esophageal cancer into 2 subgroups with markedly different outcomes. A p53 Research Group study. J Thorac Cardiovasc Surg. 2014;148:2280–6.
Hall PA, Lane DP. p53 in tumour pathology: can we trust immunohistochemistry? Revisited! J Pathol. 1994;172:1–4.
Wynford-Thomas D. p53 in tumour pathology: can we trust immunocytochemistry? J Pathol. 1992;166:329–30.
Fisher CJ, Gillett CE, Vojtesek B, Barnes DM, Millis RR. Problems with p53 immunohistochemical staining: the effect of fixation and variation in the methods of evaluation. Br J Cancer. 1994;69:26–31.
Acknowledgements
We thank H. Nikki March, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
This study was supported by a Grant-in-Aid for Scientific Research Program from the Japan Society for the Promotion of Science (JSPS KAKENHI; grant number 20K07391).
Author information
Authors and Affiliations
Contributions
MI and SK designed the study, interpreted the data, and wrote the manuscript. MI and TD performed the immunostaining and statistical analysis. HO, HM, YU, KSu, and IU participated in the design of the study and assisted with the data analysis. KSh and MH prepared the paraffin sections. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted with the approval of the ethics committees of Fujita Health University School of Medicine and Kobe University Graduate School of Health Sciences (reference numbers HM20-146 and 980, respectively). All patients provided written informed consent regarding the use of their tissue specimens.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Izutsu, M., Domoto, T., Kamoshida, S. et al. Expression status of p53 and organic cation transporter 1 is correlated with poor response to preoperative chemotherapy in esophageal squamous cell carcinoma. World J Surg Onc 20, 105 (2022). https://doi.org/10.1186/s12957-022-02571-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02571-9