Abstract
Background
Lymphocytes that surround cancer participate in tumor-related immune responses and are called tumor-infiltrating lymphocytes (TILs). Several recent reports suggest TILs index the tumor microenvironment and predict the therapeutic effect of chemotherapy. However, only few studies have studied the relationship between age and TILs. Aging reduces host immunity, and we predict that it may also affect TILs. Thus, we hypothesized that older breast cancer (BC) patients may have low TIL density than younger BC patients. Here, we retrospectively analyzed the differences in TILs by age and the therapeutic effects of preoperative chemotherapy (POC) in BC patients who were aged either less than 45 years or more than 60 years.
Methods
We retrospectively examined the data of 356 breast cancer patients who underwent POC, including 75 patients aged ≤ 45 years and 116 patients aged > 60 years. Using pre-treatment needle biopsy specimens, TIL density was compared for each age group by Student’s t-test. After analyzing different factors that affect TIL density, prognostic factors were also examined.
Results
Older patients with triple-negative BC had significantly lower TIL density than younger patients, while in human epidermal growth factor receptor 2 (HER2)-enriched BC, TIL density was significantly higher in the younger age group than that in the older age group. In addition, younger patients with HER2-rich breast cancer showed significantly higher complete pathological response rates than older patients with HER2-rich BC. In addition, significant differences in overall survival were observed among these patients with triple-negative BC.
Conclusions
Our study suggests that younger BC patients possess significantly higher TIL density than older patients. These differences may influence the therapeutic efficacy in highly immunogenic subtypes.
Similar content being viewed by others
Background
Tumor-infiltrating lymphocytes (TILs) surround cancer tissue and are involved in tumor-related immune responses [1]. Moreover, as components of the tumor microenvironment (TME), TILs allow the prediction of the therapeutic efficacy of chemotherapy [2,3,4]. In patients with breast cancer (BC), an increase in TIL density correlated with an increase in the pathologic complete response (pCR) rate, along with improved disease-free survival (DFS) and overall survival (OS) [5, 6]. Further, the TIL density in breast cancer differs depending on the subtype. For instance, hormone receptor-negative breast cancers (HR-BC), such as triple-negative breast cancer (TNBC) and human epidermal growth factor receptor 2-enriched breast cancer (HER2-enriched BC), show high TIL density [7,8,9]. However, there are fewer reports on factors other than BC subtypes that affect the TIL density.
Currently, the standard treatment is based on the results of various clinical trials. For instance, some clinical trials suggest the prognosis and treatment effect differ depending on the age of the patients [10,11,12], and several pooled studies have reported differences in the treatment effect due to age [5, 13, 14]. However, until now, only few studies have assessed the relationship between age and TIL density. While increased age may reduce host immunity [15], we can also hypothesize that it affects TIL density. Moreover, clinical trials on the association of TILs and therapeutic effects have not correlated age and TILs [12, 16,17,18,19], and most of them have stratified patients into two groups based on TILs or age and performed only t-test analyses to compare the groups.
First, we decided to compare TIL density for each age group, and if the TIL density decreased with age, we hypothesized that omitting the middle-aged group would polarize the younger and the older age groups. We also tested the hypothesis that the therapeutic effect and prognoses of patients may differ with TIL density. Thus, here, we retrospectively analyzed the differences in TIL density by age and analyzed the therapeutic effects in patients with BC ≤ 45 years or > 60 years of age who were treated with preoperative chemotherapy (POC).
Methods
Patient background
A total of 356 patients with BC received POC between February 2007 and March 2018 at the Osaka City University Hospital, Japan, and were retrospectively recruited in the study. Further, we compared the TIL density in patients aged ≤ 45 years (younger group, n = 75) versus those aged > 60 years (older group, n = 116). The patients were pathologically diagnosed with BC using core needle biopsy (CNB) or vacuum-assisted biopsy (VAB), and by immunohistochemical staining of the specimen to evaluate the expression of estrogen receptor (ER), progesterone receptor (PgR), HER2, and Ki67. Based on the results, the subtypes were classified as follows: HER2-enriched BC (ER−, PgR−, and HER2+); TNBC (ER−, PgR−, and HER2−); HR+HER2+BC (ER+ and/or PgR+, and HER2+); and HR+HER2-BC (ER+ and/or PgR+, and HER2−). Before chemotherapy, the staging of BC was evaluated using ultrasonography (US), computed tomography (CT), and bone scintigraphy. POC was administered in BC patients diagnosed with stage IIA (T1, N1, M0 or T2, N0, M0), IIB (T2, N1, M0 or T3, N0, M0), IIIA (T1–2, N2, M0 or T3, N1–2, M0), IIIB (T4, N0–2, M0), or IIIC (T1–4, N3, M0). The POC regimen was comprised of four courses of FEC100 (500 mg/m2 fluorouracil, 100 mg/m2 epirubicin, and 500 mg/m2 cyclophosphamide) every 3 weeks, followed by 12 courses of 80 mg/m2 paclitaxel administered weekly. For HER2+ BC patients, an additional weekly (2 mg/kg) or tri-weekly (6 mg/kg) dosage of trastuzumab was administered during paclitaxel treatment [20,21,22]. The anti-tumor effects of POC were evaluated according to the Response Evaluation Criteria in Solid Tumors [23]. Further, patients with clinical partial response (cPR) and complete response (cCR) were defined as “responders” in the objective response rate (ORR), whereas patients with clinical stable disease (cSD) and clinical progressive disease (cPD) were defined as “non-responders.” After POC, all the patients underwent mastectomy or breast-conserving surgery [24]. A pathologic complete response (pCR) was defined as the complete disappearance of the invasive components of the lesion with or without intraductal components, including that in the lymph nodes according to the National Surgical Adjuvant Breast and Bowel Project B-18 protocol [25].
Post-surgery, standard adjuvant therapy was administered according to each subtype and surgical procedure. During adjuvant therapy, all the patients were evaluated for tumor recurrence by physical examination, US, and CT and bone scintigraphy every 3, 6, and 12 months, respectively. The median follow-up time was 1281 days (range, 13–3675 days) after surgery.
Histopathological evaluation of TIL density
TIL density was evaluated using pretreatment specimens obtained by CNB or VAB. The TILs were defined and evaluated based on the International TILs Working Group 2014 [1] as the average of the infiltrating lymphocytes within the tumor stroma at five randomly selected fields. Next, the results were classified into four classes (3: > 50%; 2: > 10–50%; 1: ≤ 10%; or 0: absent) (Supplementary Fig. S1). Further, we defined scores 2 and 3 as “high,”, and scores 1 and 0 as “low” according to previous reports [26, 27]. Thus, in brief, the cut-off value of TIL density was set to 10%.
Statistical analysis
All statistical analyses were performed using the JMP software package (SAS, Tokyo, Japan). The distribution of TIL density by age was evaluated using Student’s t-test. Pearson’s chi-square test was used to evaluate the relationship between each categorical variable. Prognostic analyses, such as DFS or OS, were examined using the Kaplan–Meier method and log-rank test. The hazard ratio (HR) and 95% confidence interval (CIs) were calculated using the Cox proportional hazards model. Multivariable analysis was performed using the Cox regression model. A P-value < 0.05 was considered statistically significant.
Results
Clinicopathological features of BC patients
The clinicopathological features of patients (n = 356) treated with POC have been summarized in Table 1. The patients were operated on at a median age of 55 years (range, 24–78 years) and the median tumor diameter was 28.7 mm (range, 9.2–119.8 mm). Skin infiltration was observed in 58 patients (16.3%). Further, imaging methods of diagnosis did not indicate lymph node metastasis in 121 patients (34.0 %). The number of ER-negative, PgR-negative, and HER2-positive patients was 187 (52.5 %), 242 (68.0 %), and 125 (35.1 %), respectively. Moreover, Ki67-high (above 14%) was observed in 239 patients (67.1 %). Based on these results, the BC subtypes were classified as follows—HR+HER2−: 126 patients (35.4 %), HR+HER2+: 47 patients (13.2 %), HER2-enriched: 78 patients (21.9 %), and TNBC: 105 patients (29.5 %). Furthermore, the responders for ORR reached 88.8%, the rate of pCR post-operative pathology was 33.1%, and 161 patients (45.2%) showed high TIL density.
Further, while most of the clinicopathological factors were not significantly different, the rate of skin infiltration and PgR-negative status were significantly higher in the older than in the younger patients (P = 0.002 and P = 0.003, respectively) (Table 2). Moreover, the ORR, although statistically insignificant, was found to be higher in the younger than in the older patients (P = 0.091).
Correlation of TIL density with clinicopathological features and prognosis of patients
First, the 356 patients were divided into high and low TIL density groups, and their correlation with clinicopathological factors was examined (Supplementary Table S1). The following characteristics were significantly different between the low TILs and high TILs group: ≥ 45 years (P = 0.008), skin invasion (P = 0.001), ER-positive (P < 0.001), PgR-positive (P < 0.001), HER2-negative (P = 0.011), Ki67-high (P < 0.001), low ORR (P = 0.001), and low pCR rate (P < 0.001).
Further, the high TIL density group showed significantly better DFS than the low TIL density group in HER2-enriched (P = 0.012) and TNBC (P = 0.002) categories (Supplementary Fig. S2). Therefore, DFS was better in the high TIL density group despite no significant difference in HR+ BC (P = 0.011). However, the high TIL density group had better OS, although not statistically significant, than the low TIL density group in TNBC category (P = 0.057, log-rank), but there was no significant difference between the difference of TIL density (Supplementary Fig. S3). Further, in the univariate analysis for DFS, the high TIL density group was associated with significantly better DFS (P = 0.010, HR = 0.512) than the low TIL density group (Supplementary Table S2). However, in the multivariate analysis, TIL density was not an significant independent factor for DFS (P = 0.227, HR = 0.699) and since skin invasion (P = 0.012, HR = 2.180), lymph node metastasis (P = 0.001, HR = 2.918), HER2-positive (P = 0.020, HR = 0.498), responders in ORR (P < 0.001, HR = 0.247), and pCR (P < 0.001, HR = 0.315) influenced the DFS. Additionally, difference in OS due to TILs was insignificant even in the univariate analysis (P=0.214, HR = 0.660) (Supplementary Table S3).
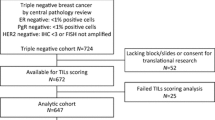
Further, the patients were classified based on age as ≤ 45 years, 46–60 years, and ≥ 61 years, and the distribution of TIL density was analyzed using a t-test (Fig. 1). Our analysis did not indicate a significant difference in HR+ BC for any of the age groups. However, for HER2-enriched BC, patients aged ≤ 45 years had significantly higher TIL density than patients in the other age groups (vs. 46–60 years: P = 0.002, and vs. ≥ 61 years: P = 0.018). Furthermore, in the TNBC category, the patients aged ≥ 61 years had significantly higher TIL density than patients in other age groups (vs. ≤ 40 years: P = 0.035, and vs. 46–60 years: P = 0.047).
Correlation of TIL density with age of BC patients. Patients were grouped based on their BC subtype as: a) all cases, b) HR+HER2-, c) HR+HER2+, d) HER2-enriched, and e) TNBC. The TIL density in each age group in each subtype has been indicated using box-plot distribution analysis. P-values in the figure indicate statistical significance for each comparison obtained using t-test
Examination of clinicopathological factors and prognosis in the younger and older BC patients
First, we studied the correlation between TIL density and clinicopathological factors in the younger and older patients (Table 2). Although patients aged 46–60 years were excluded from the analysis, the characteristics of the high TIL density group were similar to those for all patients: > 60 years (P = 0.047), skin infiltration (P = 0.001), ER-positive (P < 0.001), PgR-positive (P = 0.001), HER2-negative (P = 0.002), lower ORR (P = 0.002), and lower pCR rate (P < 0.001).
Further, younger patients showed significantly higher pCR rates than older patients in the HR+HER2- and HER2-enriched BC category (P = 0.021 and P = 0.048, respectively) (Table 3). Moreover, in HR+HER2+BC, the responder rate for ORR was significantly higher in the younger patients than in the older patients (P = 0.009). However, no significant difference was observed in the effect of POC on TNBC.
Next, when DFS was compared between the younger and older patients, no significant difference was found overall or in any subtype (Fig. 2). Moreover, our analysis indicated that age or TILs was not a predictor of DFS in the univariate analysis (P = 0.619 and P = 0.066, respectively) (Table 4). Although upon comparison of OS, a significant difference was observed between younger and older patients with TNBC (P = 0.039, log-rank) (Fig. 3), the results were contrasting and suggested better OS in older patients than in younger patients. Additionally, in univariate analysis with OS, no significant difference in age and TIL density was observed (P = 0.346 and P = 0.216, respectively) (Table 5).
Comparison of disease-free survival (DFS) between younger and older patients with varied BC subtypes. Kaplan-Meier DFS analysis has been indicated for patients grouped based on their BC subtype as: a) all cases, b) HR+HER2-, c) HR+HER2+, d) HER2-enriched, and e) TNBC. P-values in the figure indicate statistical significance for each comparison obtained using log-rank test
Comparison of overall survival (OS) between younger and older patients with varied BC subtypes. Kaplan-Meier OS analysis has been indicated for patients grouped based on their BC subtype as: a) all cases, b) HR+HER2-, c) HR+HER2+, d) HER2-enriched, and e) TNBC. P-values in the figure indicate statistical significance for each comparison obtained using log-rank test
Discussion
The characteristics of BC in the older patients have been often reported. For example, large tumor size [13, 28,29,30], frequent skin infiltration [29, 31], infrequent lymph node metastasis [28, 30], high rate of HR positivity [13, 28], and fewer HER2-positive tumors [28,29,30] have been reported in older patients. The clinicopathological characteristics of older BC patients in our study show a strong correlation to the decision of administering POC or not, though some features similar to those reported by others were identified.
While age-related differences in pCR rates have not been reported in several clinical trials, a pooled analysis observed a high pCR rate in younger BC patients [14]. Moreover, reports suggest that the pCR rate decreased with age [10, 13]. Analysis of BC based on subtype in these studies suggested a strong correlation between HR+HER2- and TNBC, whereas no significant difference with age was observed in HER2-positive BC, which differed in our study, and the exact reason remains to be identified. Further, there are various molecular subtypes of TNBC, and the age at onset and pCR rates differ across studies [32,33,34]. We anticipate that our analysis may have been affected by differences in molecular subtypes of TNBC or due to differences in the chemotherapy regimen. Furthermore, reports suggest that the expression of androgen receptor (AR) increases with age in BC patients [35,36,37] and that the AR-positive cases show low pCR rates than the AR-negative cases [38]. Additionally, newer biomarkers may also affect these outcomes.
Moreover, von Waldenfels et al. have reported that prognosis worsens with age in BC patients [13]. However, their study observed significant differences in prognoses between patients aged ≥ 65 years and those aged 40–50 or 51–65 years, but no significant difference between patients aged ≥ 65 years and those aged < 40 years. Furthermore, studies reporting a higher pCR rate in younger patients did not observe a significant difference in prognosis in patients with TNBC [14]. In contrast, studies reported more than 10 years back suggest poor prognosis [39,40,41] and aggressive cellular properties in the younger BC patients [39, 42,43,44]. AR expression also affects prognosis and may contribute [38]. Additionally, with the advent of newer biological treatments, the number of clinical trials claiming prognosis to differ with age has decreased.
Here, when we studied TILs at all ages, we observed a correlation between TILs and clinicopathological factors, treatment effects, and prognosis similar to those reported previously. Moreover, our analysis suggests that younger BC patients had significantly higher TIL density than older BC patients. Additionally, age-related ORR and pCR rates differed in HER2-positive BC. Moreover, a pooled analysis for TNBC alone reported that the older patients had significantly lower TILs than the younger patients [45]. This result can be attributed to the decrease in host immunity due to aging, and to the inherent cellular characteristics of BC that vary with age.
However, this study has a limitation that the criteria for dividing patients into younger and older patients were not well-defined and that the clinicopathological factors other than TIL density differed with age. In addition, genetic predisposition, medications such as steroids, and lifestyle may also affect the immune microenvironment, but these factors could not be examined because this was a retrospective study. Furthermore, in this study, TILs were collectively examined, but they have various subclasses. As a typical example, CD8-positive cytotoxic T cells are reported to have a better prognosis as they are highly expressed [46,47,48], on the other hand, regulatory T cells, which were famous for being positive for FOXP3, were reported to be involved in poor prognosis [46]. PD-1 / PD-L1, which is also a target molecule in clinical treatment, might also affect TILs and prognosis [47, 49]. In addition, a study has reported that the host’s immune environment itself affects the pCR of preoperative chemotherapy [50]. In the future, it will be necessary to study immunohistochemical staining in our research as well. However, it was important to know the difference depending on the age in the evaluation of TILs by hematoxylin and eosin staining. And our study is considered to be the key study to show the reason why the therapeutic effect by age was different. The change with age in TME suggests that it may have influenced the therapeutic effect due to the characteristics of the host’s immune system, and the differences in cancer itself depending on the age. Additionally, in lung cancer, it has been reported that the therapeutic effect of the immune checkpoint inhibitors (ICIs) decreases in the older patients [51,52,53]. Therefore, age may also serve as an important clinical factor in deciding the course of treatment of BC patients with ICIs.
Conclusions
The analysis presented in this study suggests that younger BC patients show significantly higher TIL density than older patients, along with differences in prognoses between the groups. Moreover, these differences may allow selection of better treatment modalities for the highly immunogenic subtypes of BC.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AR:
-
Androgen receptor
- BC:
-
Breast cancer
- CIs:
-
Confidence intervals
- cCR:
-
Clinical complete response
- CNB:
-
Core needle biopsy
- CT:
-
Computed tomography
- cPD:
-
Clinical progressive disease
- cPR:
-
Clinical partial response
- cSD:
-
Clinical stable disease
- DFS:
-
Disease-free survival
- ER:
-
Estrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
- HR:
-
Hormone receptor
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- pCR:
-
Pathological complete response
- PgR:
-
Progesterone receptor
- POC:
-
Pre-operative chemotherapy
- TN:
-
Triple-negative
- TILs:
-
Tumor-infiltrating lymphocytes
- TIME:
-
Tumor microenvironment
- US:
-
Ultrasonography
- VAB:
-
Vacuum-assisted biopsy
References
Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol. 2015;26(2):259–71. https://doi.org/10.1093/annonc/mdu450.
Zitvogel L, Kepp O, Kroemer G. Immune parameters affecting the efficacy of chemotherapeutic regimens. Nat Rev Clin Oncol. 2011;8(3):151–60. https://doi.org/10.1038/nrclinonc.2010.223.
Fridman WH, Pages F, Sautes-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer. 2012;12(4):298–306. https://doi.org/10.1038/nrc3245.
Couzin-Frankel J. Breakthrough of the year 2013. Cancer Immunother Sci. 2013;342(6165):1432–3. https://doi.org/10.1126/science.342.6165.1432.
Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, et al. Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol. 2014;32(27):2959–66. https://doi.org/10.1200/JCO.2013.55.0491.
Denkert C, von Minckwitz G, Brase JC, Sinn BV, Gade S, Kronenwett R, et al. Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. J Clin Oncol. 2015;33(9):983–91. https://doi.org/10.1200/JCO.2014.58.1967.
Ohtani H, Mori-Shiraishi K, Nakajima M, Ueki H. Defining lymphocyte-predominant breast cancer by the proportion of lymphocyte-rich stroma and its significance in routine histopathological diagnosis. Pathol Int. 2015;65(12):644–51. https://doi.org/10.1111/pin.12355.
Stanton SE, Adams S, Disis ML. Variation in the incidence and magnitude of tumor-infiltrating lymphocytes in breast cancer subtypes: a systematic review. JAMA Oncol. 2016;2(10):1354–60. https://doi.org/10.1001/jamaoncol.2016.1061.
Asano Y, Kashiwagi S, Goto W, Takada K, Takahashi K, Hatano T, et al. Prediction of treatment response to neoadjuvant chemotherapy in breast cancer by subtype using tumor-infiltrating lymphocytes. Anticancer Res. 2018;38(4):2311–21. https://doi.org/10.21873/anticanres.12476.
Huober J, von Minckwitz G, Denkert C, Tesch H, Weiss E, Zahm DM, et al. Effect of neoadjuvant anthracycline-taxane-based chemotherapy in different biological breast cancer phenotypes: overall results from the GeparTrio study. Breast Cancer Res Treat. 2010;124(1):133–40. https://doi.org/10.1007/s10549-010-1103-9.
Loibl S, Untch M, Burchardi N, Huober J, Sinn BV, Blohmer JU, et al. A randomised phase II study investigating durvalumab in addition to an anthracycline taxane-based neoadjuvant therapy in early triple-negative breast cancer: clinical results and biomarker analysis of GeparNuevo study. Ann Oncol. 2019;30(8):1279–88. https://doi.org/10.1093/annonc/mdz158.
Loi S, Michiels S, Salgado R, Sirtaine N, Jose V, Fumagalli D, et al. Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann Oncol. 2014;25(8):1544–50. https://doi.org/10.1093/annonc/mdu112.
von Waldenfels G, Loibl S, Furlanetto J, Machleidt A, Lederer B, Denkert C, et al. Outcome after neoadjuvant chemotherapy in elderly breast cancer patients - a pooled analysis of individual patient data from eight prospectively randomized controlled trials. Oncotarget. 2018;9(20):15168–79. https://doi.org/10.18632/oncotarget.24586.
Loibl S, Jackisch C, Lederer B, Untch M, Paepke S, Kummel S, et al. Outcome after neoadjuvant chemotherapy in young breast cancer patients: a pooled analysis of individual patient data from eight prospectively randomized controlled trials. Breast Cancer Res Treat. 2015;152(2):377–87. https://doi.org/10.1007/s10549-015-3479-z.
Yaqoob P. Ageing alters the impact of nutrition on immune function. Proc Nutr Soc. 2017;76(3):347–51. https://doi.org/10.1017/S0029665116000781.
Salgado R, Denkert C, Campbell C, Savas P, Nuciforo P, Aura C, et al. Tumor-infiltrating lymphocytes and associations with pathological complete response and event-free survival in HER2-positive early-stage breast cancer treated with lapatinib and trastuzumab: a secondary analysis of the NeoALTTO trial. JAMA Oncol. 2015;1(4):448–54. https://doi.org/10.1001/jamaoncol.2015.0830.
Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F, et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J Clin Oncol. 2013;31(7):860–7. https://doi.org/10.1200/JCO.2011.41.0902.
Luen SJ, Salgado R, Fox S, Savas P, Eng-Wong J, Clark E, et al. Tumour-infiltrating lymphocytes in advanced HER2-positive breast cancer treated with pertuzumab or placebo in addition to trastuzumab and docetaxel: a retrospective analysis of the CLEOPATRA study. Lancet Oncol. 2017;18(1):52–62. https://doi.org/10.1016/S1470-2045(16)30631-3.
Perez EA, Ballman KV, Tenner KS, Thompson EA, Badve SS, Bailey H, et al. Association of stromal tumor-infiltrating lymphocytes with recurrence-free survival in the N9831 adjuvant trial in patients with early-stage HER2-positive breast cancer. JAMA Oncol. 2016;2(1):56–64. https://doi.org/10.1001/jamaoncol.2015.3239.
Mauri D, Pavlidis N, Ioannidis JP. Neoadjuvant versus adjuvant systemic treatment in breast cancer: a meta-analysis. J Natl Cancer Inst. 2005;97(3):188–94. https://doi.org/10.1093/jnci/dji021.
Mieog JS, van der Hage JA, van de Velde CJ. Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst Rev. 2007;2:CD005002. https://doi.org/10.1002/14651858.CD005002.pub2.
Kawajiri H, Takashima T, Onoda N, Kashiwagi S, Noda S, Ishikawa T, et al. Efficacy and feasibility of neoadjuvant chemotherapy with FEC 100 followed by weekly paclitaxel for operable breast cancer. Oncol Lett. 2012;4(4):612–6. https://doi.org/10.3892/ol.2012.801.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Kashiwagi S, Onoda N, Asano Y, Kurata K, Morisaki T, Noda S, et al. Partial mastectomy using manual blunt dissection (MBD) in early breast cancer. BMC Surg. 2015;15:117. https://doi.org/10.1186/s12893-015-0102-5.
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr. 2001;30:96–102. https://doi.org/10.1093/oxfordjournals.jncimonographs.a003469.
Kashiwagi S, Asano Y, Goto W, Takada K, Takahashi K, Noda S, et al. Use of tumor-infiltrating lymphocytes (TILs) to predict the treatment response to eribulin chemotherapy in breast cancer. PLoS One. 2017;12(2):e0170634. https://doi.org/10.1371/journal.pone.0170634.
Asano Y, Kashiwagi S, Goto W, Takada K, Takahashi K, Hatano T, et al. Prediction of survival after neoadjuvant chemotherapy for breast cancer by evaluation of tumor-infiltrating lymphocytes and residual cancer burden. BMC Cancer. 2017;17(1):888. https://doi.org/10.1186/s12885-017-3927-8.
Gennari R, Curigliano G, Rotmensz N, Robertson C, Colleoni M, Zurrida S, et al. Breast carcinoma in elderly women: features of disease presentation, choice of local and systemic treatments compared with younger postmenopasual patients. Cancer. 2004;101(6):1302–10. https://doi.org/10.1002/cncr.20535.
Wildiers H, Kunkler I, Biganzoli L, Fracheboud J, Vlastos G, Bernard-Marty C, et al. Management of breast cancer in elderly individuals: recommendations of the International Society of Geriatric Oncology. Lancet Oncol. 2007;8(12):1101–15. https://doi.org/10.1016/S1470-2045(07)70378-9.
Crivellari D, Aapro M, Leonard R, von Minckwitz G, Brain E, Goldhirsch A, et al. Breast cancer in the elderly. J Clin Oncol. 2007;25(14):1882–90. https://doi.org/10.1200/JCO.2006.10.2079.
Louwman WJ, Vulto JC, Verhoeven RH, Nieuwenhuijzen GA, Coebergh JW, Voogd AC. Clinical epidemiology of breast cancer in the elderly. Eur J Cancer. 2007;43(15):2242–52. https://doi.org/10.1016/j.ejca.2007.08.005.
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y, et al. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest. 2011;121(7):2750–67. https://doi.org/10.1172/JCI45014.
Masuda H, Baggerly KA, Wang Y, Zhang Y, Gonzalez-Angulo AM, Meric-Bernstam F, et al. Differential response to neoadjuvant chemotherapy among 7 triple-negative breast cancer molecular subtypes. Clin Cancer Res. 2013;19(19):5533–40. https://doi.org/10.1158/1078-0432.CCR-13-0799.
Echavarria I, Lopez-Tarruella S, Picornell A, Garcia-Saenz JA, Jerez Y, Hoadley K, et al. Pathological response in a triple-negative breast cancer cohort treated with neoadjuvant carboplatin and docetaxel according to Lehmann's refined classification. Clin Cancer Res. 2018;24(8):1845–52. https://doi.org/10.1158/1078-0432.CCR-17-1912.
Asano Y, Kashiwagi S, Goto W, Tanaka S, Morisaki T, Takashima T, et al. Expression and clinical significance of androgen receptor in triple-negative breast cancer. Cancers (Basel). 2017;9(1):doi:10.3390/cancers9010004.
Astvatsaturyan K, Yue Y, Walts AE, Bose S. Androgen receptor positive triple negative breast cancer: clinicopathologic, prognostic, and predictive features. PLoS One. 2018;13(6):e0197827. https://doi.org/10.1371/journal.pone.0197827.
Jongen L, Floris G, Wildiers H, Claessens F, Richard F, Laenen A, et al. Tumor characteristics and outcome by androgen receptor expression in triple-negative breast cancer patients treated with neo-adjuvant chemotherapy. Breast Cancer Res Treat. 2019;176(3):699–708. https://doi.org/10.1007/s10549-019-05252-6.
Asano Y, Kashiwagi S, Onoda N, Kurata K, Morisaki T, Noda S, et al. Clinical verification of sensitivity to preoperative chemotherapy in cases of androgen receptor-expressing positive breast cancer. Br J Cancer. 2016;114(1):14–20. https://doi.org/10.1038/bjc.2015.434.
Anders CK, Hsu DS, Broadwater G, Acharya CR, Foekens JA, Zhang Y, et al. Young age at diagnosis correlates with worse prognosis and defines a subset of breast cancers with shared patterns of gene expression. J Clin Oncol. 2008;26(20):3324–30. https://doi.org/10.1200/JCO.2007.14.2471.
Adami HO, Malker B, Holmberg L, Persson I, Stone B. The relation between survival and age at diagnosis in breast cancer. N Engl J Med. 1986;315(9):559–63. https://doi.org/10.1056/NEJM198608283150906.
Fredholm H, Eaker S, Frisell J, Holmberg L, Fredriksson I, Lindman H. Breast cancer in young women: poor survival despite intensive treatment. PLoS One. 2009;4(11):e7695. https://doi.org/10.1371/journal.pone.0007695.
Colleoni M, Rotmensz N, Robertson C, Orlando L, Viale G, Renne G, et al. Very young women (<35 years) with operable breast cancer: features of disease at presentation. Ann Oncol. 2002;13(2):273–9. https://doi.org/10.1093/annonc/mdf039.
Ding J, Jiang L, Wu W. Predictive value of clinicopathological characteristics for sentinel lymph node metastasis in early breast cancer. Med Sci Monit. 2017;23:4102–8. https://doi.org/10.12659/msm.902795.
Nouh MA, Ismail H, El-Din NH, El-Bolkainy MN. Lymph node metastasis in breast carcinoma: clinicopathological correlations in 3747 patients. J Egypt Natl Canc Inst. 2004;16(1):50–6.
Loi S, Drubay D, Adams S, Pruneri G, Francis PA, Lacroix-Triki M, et al. Tumor-infiltrating lymphocytes and prognosis: a pooled individual patient analysis of early-stage triple-negative breast cancers. J Clin Oncol. 2019;37(7):559–69. https://doi.org/10.1200/JCO.18.01010.
Lingyu H, Mingyuan Z, Yiyu S, Zhengxiang Z, Bin W. The prognostic value of intratumoral and peritumoral tumor-infiltrating FoxP3+Treg cells in of pancreatic adenocarcinoma: a meta-analysis. World J Surg Oncol. 2021;19(1):300. https://doi.org/10.1186/s12957-021-02420-1.
Xiao-Wei D, Gao L, Juan L, Chun-Yan Z, Qiong L, Hao W, et al. Comprehensive analysis of the cancer driver genes in breast cancer demonstrates their roles in cancer prognosis and tumor microenvironment. World J Surg Oncol. 2021;19(1):273. https://doi.org/10.1186/s12957-021-02387-z.
Evan M, Anupama S, Akaansha G, Daniel GS, Robert W, Sagar S, et al. Assessment of outcomes and novel immune biomarkers in metaplastic breast cancer: a single institution retrospective study. World J Surg Oncol. 2020;18(1):11. https://doi.org/10.1186/s12957-019-1780-8.
Oner G, Önder S, Karatay H, Naziye AK, Tükenmez M, Müslümanoğlu M, et al. Clinical impact of PD-L1 expression in triple-negative breast cancer patients with residual tumor burden after neoadjuvant chemotherapy. World J Surg Oncol. 2021;19(1):264. https://doi.org/10.1186/s12957-021-02361-9.
Lingfeng T, Xiujie S, Gang T. Exploring the influencing factors of the pathologic complete response in estrogen receptor-positive, HER2-negative breast cancer after neoadjuvant chemotherapy: a retrospective study. World J Surg Oncol. 2022;20(1):27. https://doi.org/10.1186/s12957-022-02492-7.
Herbst RS, Baas P, Kim DW, Felip E, Perez-Gracia JL, Han JY, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387(10027):1540–50. https://doi.org/10.1016/S0140-6736(15)01281-7.
Brahmer J, Reckamp KL, Baas P, Crino L, Eberhardt WE, Poddubskaya E, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373(2):123–35. https://doi.org/10.1056/NEJMoa1504627.
Nishijima TF, Muss HB, Shachar SS, Moschos SJ. Comparison of efficacy of immune checkpoint inhibitors (ICIs) between younger and older patients: a systematic review and meta-analysis. Cancer Treat Rev. 2016;45:30–7. https://doi.org/10.1016/j.ctrv.2016.02.006.
Acknowledgements
We thank Natsumi Okahara and Tomomi Okawa (Department of Breast and Endocrine Surgery, Osaka City University Graduate School of Medicine) for helpful advice regarding data management.
Funding
This study was supported in part by Grants-in-Aid for Scientific Research (KAKENHI, Nos. 17K10559, 19K18067, and 20K08938) from the Ministry of Education, Science, Sports, Culture and Technology of Japan.
Author information
Authors and Affiliations
Contributions
KT participated in the design of the study and drafted the manuscript. SK participated in the design of the study and manuscript editing. YA, WG, and TM helped with study data collection and manuscript preparation. MS, HT, KH, and MO conceived the study and participated in its design and coordination and helped in drafting the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent to participate in the study was obtained from each subject in accordance with the Declaration of Helsinki principles. Each patient or the patient’s family was fully informed of the investigational nature of this study and provided their written, informed consent. The study protocol was approved by the Ethics Committee of Osaka City University (approve number #926).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Figure S1.
Histopathological analysis of TIL density. The TIL density was calculated as average of infiltrating lymphocytes in the tumor stroma from five random fields, and graded as: a) 3 (>50%), b) 2 (10–50%), c) 1 (≤10%), and d) 0 (absent).
Additional file 2: Supplementary Figure S2.
Comparison of disease-free survival (DFS) between high and low TIL density with varied BC subtypes. Kaplan-Meier DFS analysis has been indicated for patients grouped based on their BC subtype as: a) all cases, b) HR+HER2-, c) HR+HER2+, d) HER2-enriched, and e) TNBC. P-values in the figure indicate statistical significance for each comparison obtained using log-rank.
Additional file 3: Supplementary Figure S3.
Comparison of overall survival (OS) between high and low TIL density with varied BC subtypes. Kaplan-Meier OS analysis has been indicated for patients grouped based on their BC subtype as: a) all cases, b) HR+HER2-, c) HR+HER2+, d) HER2-enriched, and e) TNBC. P-values in the figure indicate statistical significance for each comparison obtained using log-rank test.
Additional file 4: Supplementary Table S1.
Difference in clinicopathological features due to TILs in all patients.
Additional file 5: Supplementary Table S2.
Univariate and multivariate analysis with respect to DFS in all patients.
Additional file 6: Supplementary Table S3.
Univariate and multivariate analysis with respect to OS in all patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Takada, K., Kashiwagi, S., Asano, Y. et al. Differences in tumor-infiltrating lymphocyte density and prognostic factors for breast cancer by patient age. World J Surg Onc 20, 38 (2022). https://doi.org/10.1186/s12957-022-02513-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02513-5