Abstract
Background
The efficacy of preoperative biliary drainage (PBD) has been debated for several decades, and yet indications for PBD remain controversial. The aim of this study was to compare the postoperative morbidity and mortality in patients with malignant obstructive jaundice undergoing direct surgery versus surgery with PBD.
Methods
All consecutive patients with malignant obstructive jaundice who underwent radical resection between June 2017 and December 2019 at Zhongshan Hospital were analyzed retrospectively. The study population was divided into two groups: PBD group (PG) and direct surgery group (DG). The subgroups were chosen based on the site of obstruction. Perioperative indicators and postoperative complications were compared and analyzed.
Results
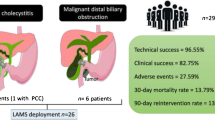
A total of 290 patients were analyzed. Postoperative complications occurred in 134 patients (46.4%). Patients in the PG group had a lower overall rate of postoperative complications compared with the DG group, with perioperative total bilirubin (TB) identified as an independent risk factor in multivariate analysis (hazard ratio = 1.004; 95% confidence interval 1.001–1.007; P = 0.017). Subgroup analysis showed that PBD reduced the complication rate in patients with proximal obstruction. In the proximal-obstruction subgroup, a preoperative TB level > 162 μmol/L predicted postoperative complications.
Conclusions
PBD may reduce the overall rate of postoperative complications among patients with proximal malignant obstructive jaundice.
Trial registration
ClinicalTrials.gov, 2018ZSLC 24. Registered May 17, 2018, https://clinicaltrials.gov/.
Similar content being viewed by others
Introduction
Biliary obstruction is commonly the first presentation in several cancers affecting the region from the perihilar bile duct to the pancreatic head, including perihilar cholangiocarcinoma (pCCA), distal cholangiocarcinoma (dCCA), ampullary carcinoma, and pancreatic ductal adenocarcinoma (PDAC) [1, 2]. Patients with intrahepatic cholangiocarcinoma (iCCA), gallbladder carcinoma (GBC), or other tumors invading the extrahepatic bile duct may also present with biliary obstruction as the first symptom [3,4,5]. However, these types of tumors are distinct in their presentation, natural history, and approach to diagnosis and management [6]. Surgical resection is the only well-established option that provides the best chance for long-term survival. However, the procedure is very challenging [7, 8]. Prolonged and progressive obstructive jaundice induces fatigue, malnutrition, bile stasis, cholangitis, and endotoxemia, and is associated with hepatic dysfunction, coagulopathy, infections, anastomotic leakage, and delayed recovery after the surgical operation [6, 9, 10]. Preoperative biliary drainage (PBD) procedures have been introduced to alleviate the negative effects of biliary obstruction. Nonetheless, PBD is an invasive treatment and carries a risk of procedure-related complications. Although it has theoretical value, routine PBD does not improve perioperative outcomes in patients with jaundice. Indications for PBD in malignant obstructive jaundice are still debated [11, 12].
In China, several large medical centers have attempted different kinds of perioperative management to improve resectability and curability, and to reduce surgical mortality and morbidity rates for radical resections. Advances in surgical techniques have enabled resection of locally advanced tumors. Three-dimensional printing technology provides certain guiding significance in the preoperative evaluation of accurate resection, and resection and reconstruction of the portal vein and hepatic artery are increasingly performed. PBD may have played a substantial role in these possible improvements, but there is no widely accepted standard.
Therefore, the present study aimed to assess the impact of PBD on postoperative outcomes and to identify in which cases PBD should be recommended.
Methods
Patients and study design
Data on the patients that underwent radical resection due to malignant biliary obstruction at Zhongshan Hospital Fudan University, Shanghai, China, between June 2017 and December 2019, were retrieved from the Hospital Information System and retrospectively analyzed. Only patients who achieved preoperative total bilirubin > 51 μmol/L were included. They either underwent radical resection or received PBD preoperatively. Only cases with full medical records wherein PBD was performed at our institution were included. The full medical records comprised initial imaging data, PBD and surgical operation records, hospitalization records, and perioperative laboratory testing results (within 3 days before operation, on the first, third, and seventh days after PBD or operation, and once a week after operation). Demographic and clinical data, including age, sex, the American Society of Anesthesiologists (ASA) score, body–mass index (BMI), medical history, histopathological diagnosis, preoperative physical examinations, laboratory tests, chest X-ray imaging, and computed tomography or magnetic resonance imaging of the abdomen, were collected. Informed written consent was obtained from each participating patient. A radical resection was considered complete if the entire gross tumor volume was removed with negative resection margins (R0 resection), while an incomplete resection was defined as the presence of a microscopic tumor in the surgical resection margin (R1 resection). Palliative resection was defined as the presence of any gross residual tumors (R2 resection), and such cases were excluded from this study. Antibiotic prophylaxis was administered and continued until at least postoperative day 5. All patients were treated with the second-generation cephalosporin intravenously ½ to 1 h prior to the start of the surgery. For lengthy procedures (e.g., ≥ 3 h) or if the amount of bleeding exceeded 1500 mL, additional dose was administered intravenously during surgery (administration modified depending on the duration of the operative procedure). Finally, 290 patients were enrolled in the study, of whom 159 had PBD before the resection (“PBD group”; PG) and 131 underwent an early surgical resection without PBD (“direct surgery group”; DG). The study protocol was approved by the ethics committees of Zhongshan Hospital and Fudan University. The methods were used in accordance with the approved guidelines. All postoperative complications were scored and classified using Common Terminology Criteria for Adverse Events 5.0. We assessed study quality using STROBE guidelines.
The PBD procedure
According to the clinical practice guidelines of Zhongshan Hospital, patients with jaundice with a total bilirubin level > 200 μmol/L or with malnutrition and cholangitis were treated with PBD as a “bridge therapy” before a radical surgical resection was attempted. PBD types included percutaneous transhepatic biliary drainage (PTBD), endoscopic nasobiliary drainage (ENBD), and endoscopic biliary stenting (EBS). In cases of failure, PTBD is usually carried out as a remedial treatment. Some patients treated had been referred from low-volume centers or other hospitals where PBD had already been performed as the first intervention. For these reasons, there were no standardized indications for jaundice palliation during the study period.
The definitions of radical resections are as follows. Radical resections for proximal obstruction, mainly in pCCA and gallbladder carcinoma, were normally hepatectomies, while those for distal obstructions, mainly in biliary carcinoma, ampullary carcinoma, and PDAC, were normally pancreatoduodenectomies. Standard lymph node dissection was also performed. All the patients received intraoperative antibiotic prophylaxis.
Statistics
The data were analyzed using the SPSS software version 25.0 (IBM Corp., Armonk, NY, USA). Categorical data are presented as percentages, and frequencies were compared by the χ2 test or McNemar’s test, as appropriate. Continuous variables were analyzed for normality using the Kolmogorov-Smirnov test. Normally distributed continuous variables are presented as means and standard deviations (SD), and the significance of pairwise differences was assessed by the independent-sample or dependent-sample t test, as appropriate. Non-normally distributed continuous variables are presented as medians and interquartile ranges, and the significance of their differences was evaluated by the Mann–Whitney U test or Wilcoxon signed-rank test, as appropriate. To identify the best cutoff of preoperative total bilirubin (TB) for distinguishing patients with postoperative complication(s), a receiver-operating characteristic (ROC) were generated, and the area under the ROC curve (AUC), sensitivity, and specificity were used to investigate the validity of TB diagnostic models. Differences with a P value < 0.05 were considered statistically significant.
Results
A total of 290 consecutive patients with malignant obstructive jaundice who underwent a radical resection at Zhongshan Hospital between June 2017 and December 2019 were included in the study. Among these, 159 (54.8%) patients had received PBD (PG group) before the resection, and 131 (45.2%) had undergone a radical resection directly after admission (DG group). In PG, for 5 (3.1%), and 149 (93.7%) patients, EBS, ENBD, and PTBD were chosen as the initial PBD, respectively. Eight patients (5.0% of the 159) needed second PBD, which was PTBD in all cases. The frequency of the second PBD was not significantly different among the three subgroups (P = 0.082; Table 1). Radical resections included pancreaticoduodenectomy, radical resection for pCCA, and other procedures, according to the tumor site.
Patient characteristics
Baseline characteristics of the patients with malignant obstructive jaundice in groups DG and PG are described in Table 2. The baseline characteristics (on admission), including age, sex, and BMI, were not significantly different between the two groups. ASA scores were significantly different between the two groups: the PG group had a higher ASA score III–IV (P < 0.001). One hundred seventy-two (59.1%) patients had proximal biliary obstruction, and 119 (40.9%) had distal biliary obstruction. The site of obstruction did not significantly affect the choice of PBD (P = 0.301). Final histopathological diagnoses were as follows: four iCCAs and 14 GBCs with invasion of an extrahepatic bile duct, 153 pCCAs, 51 distal biliary carcinomas, 47 ampullary carcinomas, 20 PDACs, and 1 hepatocellular carcinoma with invasion of an extrahepatic bile duct. The prevalence rates of these diagnoses were not significantly different between the groups, DG and PG (P = 0.301).
Laboratory testing results
A comparison of these data between the time of initial diagnosis and the time of perioperative testing is presented in Table 3. Within the DG group, initial laboratory test results, including hemoglobin (Hb) and ALB (albumin), were significantly higher compared with the perioperative test (P < 0.001 and P = 0.016). ALT and AST levels also decreased significantly (P < 0.001 and P = 0.005, respectively), while TB and direct bilirubin (DB) levels evidently increased (both P < 0.001). PBD was found to prevent the deterioration of liver function. Within the PG group, Hb levels improved significantly (P < 0.001), while ALT, AST, TB, and DB decreased significantly (P < 0.001, P < 0.001, P < 0.001, and P < 0.001, respectively).
A comparison of the laboratory test results between the two groups is presented in Table 4. At the time of initial diagnosis, the PG patients had worse anemia, higher percentage of neutrophils (NEUT %), hypoalbuminemia, and jaundice (P = 0.015, P = 0.001, P = 0.038, and P < 0.001, respectively). As to the perioperative laboratory findings, the PG patients’ condition reversed in terms of neutrophil percentage, hypoalbuminemia, and jaundice (P = 0.050, < 0.001, and < 0.001, respectively), but their anemia did not improve (P < 0.001).
All postoperative outcomes and risk factors for postoperative complications
The postoperative outcomes are shown in Table 5. The overall rate of postoperative complications was 46.4% (134 patients out of 290), and complications occurred more frequently in the DG group (P = 0.029). The postoperative hemorrhage rate was significantly higher in the DG group (P = 0.038), whereas postoperative delayed gastric emptying was significantly more frequent in the PG group (P = 0.065). The rates of mortality and other complications were similar between the two groups. The location of obstruction was used to decide on the main surgical procedure, and each group was divided into a proximal-obstruction subgroup and distal-obstruction subgroup. The overall rate of postoperative complications in the combined proximal-obstruction group was 77.9%, and complications occurred more frequently in the proximal-obstruction DG subgroup (P = 0.038, Table 6). In the combined distal-obstruction group, the overall rate of postoperative complications was 50.8%, and PBD did not affect this rate (P = 0.249, Table 6).
In univariate analysis, PBD was found to be associated with better postoperative outcomes (P = 0.025; Table 7). Perioperative Hb and perioperative TB were associated with postoperative complications (P = 0.027 and P = 0.016, respectively). Multivariate analysis indicated that perioperative TB is an independent risk factor for postoperative complications (Table 7).
Preoperative TB concentration > 162 μmol/L distinguished patients with postoperative complication(s) from those without (Fig. 1, ROC curve analysis). For this cutoff, the area under the ROC curve was 0.7024 (95% confidence interval 0.588–0.816) (P = 0.002, sensitivity 62.8%, specificity 74.4%).
Discussion
In this retrospective study, we analyzed the efficacy of PBD in patients with malignant obstructive jaundice. The incidence of patients with several different malignancies seemed puzzling. However, we want to emphasize that patients often do not undergo full medical examination at their first visit but receive preliminary treatment with limited data. Thus, we wanted to identify some easily accessible indicators that could help patients receive treatments as early as possible.
Obstructive jaundice is a life-threatening problem in patients with malignant tumors. Although the degree of hyperbilirubinemia is not necessarily related to tumor stage, hyperbilirubinemia interferes with many organ functions and limits treatment choices. Bilirubin, as a product of heme metabolism, is nearly nontoxic in its normal physiological range of concentrations, whereas hyperbilirubinemia is toxic requiring immediate attention. In particular, it has been associated with an increased risk of postoperative complications. PBD is a kind of “bridge therapy” before a radical surgical resection is attempted for malignant obstructive jaundice. There is no consensus on indications for PBD so far.
The retrospective data showed that PBD may reduce the overall rate of postoperative complications among patients with proximal obstructive jaundice. Perioperative TB turned out to be an independent risk factor for postoperative complications. Moreover, preoperative TB > 162 μmol/L distinguished patients with postoperative complications from those without.
PBD has had varied effects in different studies. Specifically, different PBD options have manifested various effects in different cancers. It must be emphasized that the data published so far came from diverse studies, where the patients had a small number of cancer types affecting the biliary tree. In 2010, van der Gaag et al. conducted a multicenter randomized controlled trial regarding the cancer of the pancreatic head and demonstrated that routine PBD increases the rate of complications. This conclusion was based on the bilirubin range of 40 to 250 μmol/L and was made about the cancer of the pancreatic head [12]. In 2016, a meta-analysis suggested that the PBD group has significantly fewer major adverse effects than the direct surgery group [11]. This conclusion was made about a series of tumors, e.g., cancers of the biliary tract, cancers of the head and neck, and cancers of the duodenum. On the other hand, the studies included in this meta-analysis took place between 1981 and 2011. Nearly simultaneously, another meta-analysis suggested that PBD worsens postoperative outcomes, increasing the prevalence rate of infectious complications, surgical site infections, and delayed gastric emptying [13]. Few studies have been conducted on multicenter randomized controlled trials for malignant obstructive jaundice [14]. In recent years, several PBD methods were simultaneously employed, and new drainage brackets are developed [15, 16]. The management of obstructive jaundice is complicated and involves not only surgeons and medical centers but also the entire healthcare system [17]. Hegel’s principle of “what exists is reasonable” is thought to be applicable worldwide, but we found a more accurate observation by examining the current methods in some clinical settings. For example, a Japanese retrospective study covered a 10-year clinical experience and revealed that PBD reduces postoperative morbidity and mortality in the whole country regardless of the PBD type [18]. This finding suggests that a beneficial modality can also be found at our medical center. During the study period, we applied a mature surgical technology and advanced equipment, and the observed prevalence of postoperative complications is not consistent with other hospitals and countries.
Our results show a clear difference made by PBD among patients with malignant obstructive jaundice. This report is the first retrospective study with the latest technology to show benefits of PBD for patients with malignant obstructive jaundice in China. Accurate preoperative diagnosis of biliary tract tumors is difficult, but the estimation of an obstruction site is easier. On the basis of our study, we believe that patients with proximal obstruction should consider PBD more often. Due to the limited number of cases in the recent 2 years under study, we did not obtain strong evidence that PBD affects postoperative complications of patients with distal obstruction.
This study has certain limitations. First, this study was retrospective, so selection bias potentially occurred. Although the best way to reduce or eliminate selection bias is a randomized controlled trial, such a trial is not feasible for patients with malignant obstructive jaundice. Second, the study involved a small sample size from only one hospital in China with predominantly Chinese patients. Medical treatment level differs widely among regions of China, so data in this study could not be widely representative.
Conclusion
Our study indicates that PBD may reduce the overall rate of postoperative complications in patients with proximal malignant obstructive jaundice. Perioperative TB is an independent risk factor for postoperative complications and supports the decision to recommend preoperative PBD when preoperative TB is > 162 μmol/L.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
References
Banales JM, et al. Cholangiocarcinoma 2020: the next horizon in mechanisms and management. Nat Rev Gastroenterol Hepatol. 2020;17(9):557–88.
Chu D, Adler DG. Malignant biliary tract obstruction: evaluation and therapy. J Natl Compr Canc Netw. 2010;8(9):1033–44.
Krasinskas AM. Cholangiocarcinoma. Surg Pathol Clin. 2018;11(2):403–29.
Oliveira IS, et al. Cholangiocarcinoma: classification, diagnosis, staging, imaging features, and management. Abdom Radiol (NY). 2017;42(6):1637–49.
Lee AJ, Chun YS. Intrahepatic cholangiocarcinoma: the AJCC/UICC 8th edition updates. Chin Clin Oncol. 2018;7(5):52.
Waseem D, Tushar P. Intrahepatic, perihilar and distal cholangiocarcinoma: management and outcomes. Ann Hepatol. 2017;16(1):133–9.
Weber SM, et al. Intrahepatic cholangiocarcinoma: expert consensus statement. HPB (Oxford). 2015;17(8):669–80.
Feng JW, et al. Progress in diagnosis and surgical treatment of perihilar cholangiocarcinoma. Gastroenterol Hepatol. 2019;42(4):271–9.
Kendall T, et al. Anatomical, histomorphological and molecular classification of cholangiocarcinoma. Liver Int. 2019;39(Suppl 1):7–18.
Lee RM, Maithel SK. Approaches and outcomes to distal cholangiocarcinoma. Surg Oncol Clin N Am. 2019;28(4):631–43.
Moole H, Bechtold M, Puli SR. Efficacy of preoperative biliary drainage in malignant obstructive jaundice: a meta-analysis and systematic review. World J Surg Oncol. 2016;14(1):182.
Neuhaus H. Preoperative biliary drainage in hilar cholangiocarcinoma: when and how? Endosc Int Open. 2020;8(2):E211–3.
Celotti A, et al. Preoperative biliary drainage in hilar cholangiocarcinoma: systematic review and meta-analysis. Eur J Surg Oncol. 2017;43(9):1628–35.
van der Gaag NA, et al. Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med. 2010;362(2):129–37.
Liu JG, et al. Endoscopic biliary drainage versus percutaneous transhepatic biliary drainage in patients with resectable hilar cholangiocarcinoma: a systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A. 2018;28(9):1053–60.
Tringali A, Boskoski I, Costamagna G. Endoscopic stenting in hilar cholangiocarcinoma: when, how, and how much to drain? Gastroenterol Res Pract. 2019;2019:5161350.
Shin SH, et al. Optimal timing of pancreaticoduodenectomy following preoperative biliary drainage considering major morbidity and postoperative survival. J Hepatobiliary Pancreat Sci. 2019;26(10):449–58.
Chaudhary RJ, et al. Survey of preoperative management protocol for perihilar cholangiocarcinoma at 10 Japanese high-volume centers with a combined experience of 2,778 cases. J Hepatobiliary Pancreat Sci. 2019;26(11):490–502.
Acknowledgements
The authors gratefully thank all of the participants in this study for supporting this study.
Funding
This study was supported by the Clinical research in Zhongshan Hospital, No. 2018ZSLC24.
Author information
Authors and Affiliations
Contributions
Houbao Liu and Sheng Shen conceived the study. Zhihui Gao and Lihong Huang analyzed and interpreted the data. Zhihui Gao wrote the manuscript. Jie Wang, Xiaobo Bo, Tao Suo, Xiaoling Ni, and Han Liu collected and assembled the data. Houbao Liu submitted the manuscript and is the corresponding author. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committees of Zhongshan Hospital and Fudan University. All patients signed informed consent.
Consent for publication
The patients have given their consent for revealing information about themselves to be published in World Journal of Surgical Oncology.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gao, Z., Wang, J., Shen, S. et al. The impact of preoperative biliary drainage on postoperative outcomes in patients with malignant obstructive jaundice: a retrospective analysis of 290 consecutive cases at a single medical center. World J Surg Onc 20, 7 (2022). https://doi.org/10.1186/s12957-021-02476-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-021-02476-z