Abstract
Background
Due to better functional outcomes, pylorus-preserving gastrectomy (PPG) has been widely applied for early gastric cancer (EGC) patients as an alternative to distal gastrectomy (DG). However, controversies still persist regarding the surgical efficacy and oncological safety of PPG.
Methods
Original studies comparing PPG and DG for EGC were searched in PubMed, Embase, and the Cochrane Register of Controlled Trials up to December 2019. The weight mean difference, standardized mean difference, or odds risk was used to calculate the short-term and long-term outcomes between the two groups.
Results
Twenty-one comparative studies comprising 4871 patients (1955 in the PPG group and 2916 in the DG group) were enrolled in this systematic review and meta-analysis. PPG showed longer hospital day, decreased harvested lymph nodes, and more delayed gastric emptying. However, PPG had the benefits of lower incidence of anastomosis leakage, early dumping syndrome, gastritis and bile reflux, and better recovery of total protein, albumin, hemoglobin, and weight. No difference was found in operative time, blood loss, and overall complications. Moreover, the long-term survival and recurrence rate were similar in two groups.
Conclusion
Owing to the non-inferiority of surgery and oncology outcomes and the superiority of function outcomes in PPG, we revealed that PPG can be clinically applicable instead of DG in EGC. However, more high-quality comparative studies and randomized clinical trials would be required for further confirmation.
Similar content being viewed by others
Background
The development of cancer screening programs and the popularization of endoscopic techniques have allowed the increasing proportion of early gastric cancer (EGC), particularly in Korea and Japan [1, 2]. Radical gastrectomy with D2 lymphadenectomy was recommended as the gold standard treatment for EGC, and distal gastrectomy (DG) is one such conventional surgical procedure. Due to the excellent oncological outcomes of early gastric cancer, restoration of stomach function and better postoperative quality of life were recognized as important as the radical curability of primary tumor. Pylorus-preserving gastrectomy (PPG), which is considered as a representative example of function-preserving gastrectomy, had become an alternative to distal gastrectomy for the treatment of EGC. Since the first application of PPG in 1967 [3], this approach has been introduced as a minimally invasive surgery and even extended to combine with laparoscopic technique. Moreover, the retainment of pyloric cuff and vagal nerve in PPG provided advantages such as ameliorating postoperative gastritis, bile reflux, early dumping syndromes, and improving nutritional status [4, 5]. In PPG, the infra-pyloric lymph nodes (LNs) are routinely dissected with preserving the infra-pyloric vessels, and the supra-pyloric LNs are usually omitted to preserve the right gastric artery and the hepatic branch of the vagal nerve [6, 7]. However, technical difficulty and incomplete lymph resection, which raise concerns about compromising long-term survival, contribute to the restriction on extensive application of PPG.
Although many studies comparing PPG and DG in terms of surgical and functional outcomes have been published [7,8,9], whether PPG is better than DG for EGC without compromising oncological safety remains debatable because of lacking long-term oncologic outcomes and high-level evidence of randomized clinical trials (RCTs). The first meta-analysis, which was published in 2014 [10], demonstrated that PPG had superior benefits in terms of lower incidence rates of early dumping syndrome, gastritis, and bile reflux as well as regaining of weight. According to the Japanese Gastric Cancer Treatment Guidelines and considerable newly published studies with relatively comprehensive data [5, 7, 11, 12], indications as well as standardized management and treatment for PPG have been well established. Therefore, we performed an updated meta-analysis to demonstrate the surgery efficacy, oncologic safety, and function recovery of PPG.
Methods
Literature search
A systematic literature search was carried out up to December 2019 using the following databases: PubMed, Embase, and the Cochrane Register of Controlled Trials (CENTRAL). The searches were limited to studies published in English. The search terms were as follows: “gastric cancer or stomach cancer or stomach neoplasm or gastric neoplasm” and “pylorus-preserving or pylorus preserving or function-preserving or function preserving”. Two independent reviewers (Xinyu Mao and Xinlei Xu) carefully explored related citations of the retrieved reports to prevent potential additional articles from overlooking. This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [13].
Inclusion and exclusion criteria
Inclusion criteria are as follows: (1) studies of patients with pathologically confirmed early gastric cancer, (2) compared pylorus-preserving gastrectomy with distal gastrectomy, (3) both open and laparoscopic procedure, (4) any kind of comparative studies, (5) revealed adequate data of the surgical or functional outcomes.
Exclusion criteria are as follows: (1) overlapped publications or duplicated data; (2) reviews, case reports, comments, and conference abstracts; (3) not addressing the comparison between pylorus-preserving gastrectomy and distal gastrectomy; (4) not relevant or available data of target endpoints.
Data extraction and quality assessment
Two authors independently conducted the data extraction among all enrolled studies; including (1) study characteristics (authors, year, country, study design, sample size); (2) patient characteristics (age, sex, ASA, BMI, tumor size, tumor stage, tumor location, reconstruction type, proximal and distal resection margin); (3) surgical outcomes (operation time, blood loss, hospitalization day, examined lymph nodes) and postoperative complications (such as anastomosis leakage, bile reflux, gastritis, delayed gastric emptying, dumping syndrome, and gallbladder stones); (4) functional status (total protein, albumin, body weight, and hemoglobin) and long-term oncological outcomes (survival and recurrence rates). Any disagreements were resolved with discussion in conference by two independent researchers.
The Newcastle-Ottawa Quality Assessment Scale (NOS) checklist (Additional file 1), which consisted of three categories (selection, comparability, and outcome) and eight elements with a maximum score of nine, was used to evaluate the quality of enrolled observational research. Studies graded with 7 or above were considered as high-quality.
Statistical analysis
Odds ratio (OR), weight mean difference (WMD), and standardized mean difference (SMD) presented with 95% confidence interval (CI) were used to pool analysis dichotomous and continuous variables, respectively. When the reports included in our work only report mean and range, standard deviation (SD) was estimated based on the formulas reported by Hozo et al. [14]. Overall survival (OS) was measured with the hazard ratio (HR) and 95% CI which is calculated by Engauge Digitizer Version 4.1 according to the Kaplan-Meier survival curves.
Heterogeneity was assessed by the chi-squared-based Q test and Higgins I-squared test among studies. According to the high heterogeneity with I2 > 50% or P < 0.1, random effects model was chosen. On the contrary, fixed effects model was preferred in terms of appreciable heterogeneity. According to the study characteristics, we performed the subgroup analyses to explore the potential cause of the heterogeneity. Funnel plots and Egger’s test were used for evaluation of publication bias. We used trim-and-fill test to estimate the influence on the results of public bias. All analyses were carried out with the Stata software (version 15; Stata Corp LLC, College Station, TX).
Results
Literature search
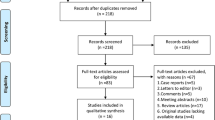
A total of 956 studies were identified in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Fig. 1). After removing 173 duplicates, 647 non-relevant studies were initially excluded by carefully screening the title and or abstract, and subsequently 109 articles were evaluated for eligibility via cautiously reviewing full-text and statistical data. Finally, one RCT and 20 non-RCTs [4,5,6,7,8,9, 12, 15,16,17,18,19,20,21,22,23,24,25,26,27,28] with 4871 patients were included in the quantitative synthesis.
Study characteristics
The details of these 21 comparative studies included in the meta-analysis are shown in Table 1. Among enrolled studies, 7 were performed laparoscopically, and open surgery was operated in the other fourteen studies, of which 96.9% patients were pathologically diagnosed with stage I gastric cancer. Sixteen papers were reported by Japan, and only 5 studies were published by Korea and China.
Additional file 2 showed the analysis of demographic characteristics. The gender distribution in the PPG group was significantly different in both groups (OR 0.83, 95% CI 0.73 to 0.94, I2 = .00%, P = 0.005). No difference in articles comparing age (WMD 0.19, 95% CI − 1.71 to 2.09, I2 = 87.90%, P = 0.845) and BMI was demonstrated between the two groups (WMD − 0.02, 95% CI − 0.24 to 0.19, I2 = 0.00%, P = 0.828). What’s more, similar tumor size was observed in enrolled studies (WMD 0.02, 95% CI − 0.09 to 0.13, I2 = 31.50%, P = 0.767). Eighteen reports which were identified as high-quality studies graded with NOS were included in this meta-analysis and NOS scores were presented in Additional file 3.
Intraoperative and postoperative findings
Table 2 showed the overall resutls between PPG and DG. Both procedures demonstrated comparative results regarding operation time (WMD − 5.00, 95% CI − 13.53 to 3.54, I2 = 76.30%, P = 0.251) (Fig. 2a) and blood loss (WMD − 19.85, 95% CI − 45.14 to 5.44, I2 = 74.90%, P = 0.124) (Fig. 2b) between the PPG and DG group. However, we observed significantly fewer retrieved lymph nodes among two groups (WMD − 1.10, 95% CI − 2.18 to − 0.01, I2 = 8.70%, P = 0.048) (Fig. 2c), which was also found between patients with the dissection No.5 lymph nodes compared with those with the preservation of No.5 lymph nodes. We also found longer hospital duration in PPG group (WMD 0.98, 95% CI 0.66 to 1.29, I2 = 30.60%, P = 0.000) (Fig. 2d). However, the PPG group had a significantly shorter proximal resection margin and distal resection margin when compared to DG group (WMD − 0.47, 95% CI − 0.91 to − 0.03, I2 = 74.30%, P = 0.038; WMD − 2.76, 95% CI − 4.96 to − 0.57, I2 = 98.20%, P = 0.013).
Morbidity and mortality
This meta-analysis demonstrated that there was no significant difference in the incidence of postoperative complications (OR 0.97, 95% CI 0.76 to 1.25, I2 = 5.70%, P = 0.835) (Fig. 2e). Incidence rate of anastomotic leakage was significant lower in PPG (OR 0.49, 95% CI 0.24 to 0.97, I2 = 0.00%, P = 0.041) (Fig. 2f). In addition, there was significant difference in delayed gastric emptying (OR 1.88, 95% CI 1.23 to 2.87, I2 = 38.40%, P = 0.003) (Fig. 3a) between two groups, which was also confirmed by assessing gastric emptying times (WMD 8.86, 95% CI 1.71 to 16.00, I2 = 0.00%, P = 0.015).What’s more, PPG group revealed similar gallbladder stone rate (OR 0.63, 95% CI 0.38 to 1.03, I2 = 14.60%, P = 0.063) (Fig. 3b), but lower incidence of early dumping syndrome (OR 0.18, 95% CI 0.07 to 0.44, I2 = 0.00%, P = 0.000). In terms of postoperative endoscopic findings and symptoms (Additional file 4), patients performed with PPG procedure suffered fewer gastritis and bile regurgitation (OR 0.22, 95% CI 0.07 to 0.74, I2 = 71.30%, P = 0.014; OR 0.30, 95% CI 0.10 to 0.89, I2 = 57.90%, P = 0.031), which was not found in esophagitis (OR 1.21, 95% CI 0.56 to 2.61, I2 = 37.90%, P = 0.621).
Long-term oncological and nutritional outcomes
Discrepancy was not found on the overall survival rate described by three included studies (WMD 0.63, 95% CI − 0.06 to 1.32, I2 = 0.00%, P = 0.074), and patients receiving PPG did not have a higher incidence of recurrence (OR 1.41, 95% CI 0.68 to 2.89, I2 = 0.00%, P = 0.355) (Additional file 5). As shown in Fig. 3, the serum total protein and albumin level in patients with PPG were higher compared with those with DG (SMD 0.39, 95% CI 0.25 to 0.53, I2 = 34.60%, P = 0.000; SMD 0.31, 95% CI 0.17 to 0.44, I2 = 22.00%, P = 0.000). Hemoglobin investigated in five articles showed better recovery (SMD 0.55, 95% CI 0.39 to 0.71, I2 = 0.00%, P = 0.000). Moreover, PPG was found a better selection with fewer decreased body weight (WMD 3.24, 95% CI 1.79 to 4.69, I2 = 65.30%, P = 0.000).
Subgroup analysis
According to year of publication, study type, and operation procedure, subgroup analysis was performed to explain heterogeneity and evaluate the possible effect of these parameters (Table 3). Shorter operative time and less blood loss of PPG was only detected in the non-retrospective studies. Significant lower incident rate of gastritis in PPG group was observed in the retrospective studies, the studies with laparoscopic procedure and the studies before 2010. Higher incidence of delayed gastric emptying was found in the PPG group of retrospective and non-retrospective studies, the studies with open surgery and the studies after 2010. In terms of postoperative body weight change, we observe significant differences in all subgroup analysis.
Sensitivity and publication bias
Possibility of publication bias was detected with constructing funnel plots and Egger’s linear regression test. We did not find significant publication bias except for gastritis and body weight change (Fig. 4, Fig. 5 and Additional file 6). However, trim-and-fill test indicated the stability of these results. Furthermore, Galbraith plot was used to assess every individual study which account for the heterogeneity, and similar results were observed after exclusion of these researches in the supplemental information (Additional file 7, 8, 9).
Discussion
Since the first report on the PPG for the treatment of gastric ulcer was published in 1967 [3], the indication of this procedure has been broadened to early gastric cancer [29, 30]. Moreover, this procedure was often performed with laparoscopic approach as less-invasive surgery. In addition, PPG is recommended for cT1N0M0 gastric cancer located in the middle-third of the stomach according to the Japanese Gastric Cancer Treatment Guidelines [11]. Although numerous published studies confirmed the non-inferiority of surgical outcomes and better function status of PPG, controversies still exist because of lacking high-quality RCTs. The ongoing KLASS-04 (NCT No.02595086) comparing LAPPG and LADG for EGC is expected to provide conclusive evidence. Therefore, this meta-analysis aimed to assess the surgery efficacy, oncologic safety,and function recovery of PPG.
The first meta-analysis published in 2014 included 16 studies with 1774 patients and demonstrated that PPG provided the benefits of preventing early dumping syndrome, bile reflux, and gastritis [10]. Given more additional articles published to compare PPG with DG for early gastric cancer, we accordingly performed an updated meta-analysis to corroborate surgical safety, oncological efficacy, and better function status for PPG. Moreover, depending on the published date, study design, and surgical procedure, we grouped enrolled studies to compare PPG and DG more precisely. Additionally, we matched factors such as the length of antral cuff and the vagus nerve preserved that might influence postoperative outcomes like gastritis and delayed gastric emptying (DGE). Furthermore, long-term oncological adequacy published with three studies followed for more than 3 years and function outcomes (total protein, albumin, hemoglobin, and body weight loss) were particularly evaluated on the comparison of PPG versus DG. To the best of knowledge, this is the biggest sample size meta-analysis and systematic review on PPG and DG including long-term oncological and functional outcomes up to date.
This meta-analysis presented similar operation duration and blood loss between PPG and DG. Interestingly, shorter operative time and lesser blood loss were demonstrated in PPG group in one RCT [8]. This phenomenon may be explained by the relatively few prospective articles and small sample size. However, shorter operating time and lesser blood loss may be noted with the accumulation of PPG experience, but further big-sample researches or RCTs are needed. Additionally, postoperative hospitalization is a very important indicator of recovery and hospital expenses. We found that PPG had the disadvantage of longer hospital day, which was also demonstrated in the subcategory analysis except for the prospective cohort studies. The same reason as decreased operation time and blood loss may account for exception of the prospective studies. This revealed that PPG might delay earlier recovery in both laparoscopic and open operation.
Owing to the skepticism regarding the incomplete lymphadenectomy, the oncological safety remains as the main issue, and the number of retrieved lymph nodes is related to the long-term survival. However, the harvested lymph nodes in PPG was significantly less than that in conventional DG, which can be attributed to incomplete dissection of supra-pyloric (5) and infra-pyloric (6) lymph nodes in PPG. The outcomes of the studies after 2010 and the prospective cohort studies were in favor of DG. The disparity might be explained by the difference in preserving No.5 lymph nodes. The preserving of No.5 lymph nodes was usually performed in the studies after 2010 but omitted in the studies before 2010. Furthermore, there was significant difference of dissected lymph nodes in studies with the preservation of No.5 lymph nodes. Lack of No.5 lymph node station is considered to preserve the right gastric artery and pyloric branch of vagal nerve, and preserving the infra-pyloric artery may lead to incomplete No.6 LN dissection. Given the relatively easy technique of dissecting infra-pyloric lymph nodes with infra-pyloric artery preservation, all studies enrolled in this meta-analysis from 2017 to 2019 radically resected LN station 6 but omitted LN station 5, which bring about incomplete D1 lymphadenectomy and concerns over oncological safety. Despite the significantly lower number of retrieved LNs in PPG, long-term survival rates were comparable for both groups in the meta-analysis. One possible explanation was the low metastasis rate of supra-pyloric lymph nodes in EGC. As described in a Korean report, the incidence of lymph node metastasis at the LN station 5 was 0.45% (1/220) [31]. A study of 219 cases revealed only 0.46% metastasis rate of supra-pyloric stations for gastric cancer invading mucosal or submucosal [32]. Oh et al. reported that the metastasis rate to supra-pyloric nodes was 4.2% (52/1245) [33].
According to the current version of the Japanese Gastric Cancer Treatment Guidelines [11], patients with cT1N0M0 gastric cancer located in the middle one-third of the stomach and at least 4.0 cm away from the pylorus can be candidates for PPG. This corroborates that PPG has a similar oncologic safety for intramucosal or submucosal carcinoma without on evidence of metastasis. However, Kong et al. [32] suggested that T1a and T2 cancers of the ≥ 6 DRM group showed no metastasis to LNS 5 and supported pylorus-preserving gastrectomy as a safe treatment for T2 cases with preoperatively diagnosed as T1. A retrospective study reported on better prognoses of T2 gastric cancers that were diagnosed preoperatively as T1 than the other T2 cancers [34]. Therefore, PPG may be a safe procedure for T2 cancers with no evidence of lymph metastasis. Nevertheless, further validations are needed to expand the indication for PPG in T2 cancers.
Due to preservation of the infra-pyloric vessels and hepatic branch of the vagus nerve, PPG has the advantage of better pyloric function and quality of life. Although similar postoperative overall complications were observed in both procedures, fewer anastomotic leakages were found in the PPG groups despite no significant difference was observed in the subgroup analysis. The decreased anastomotic fistula may be associated with better blood supply and function recovery. As described in previous reports [35], several risk factors such as advanced age, anemia, and malnourishment may contribute to anastomotic leakage. In our experience, reducing the anastomosis tension and ensuring the blood supply extremity have a beneficial effect on the healing of anastomosis, no matter to the patients' physical condition. For patients with PPG, higher hemoglobin level might be partly responsible for this result, as well as retaining the tissue around anastomosis and leaving the right gastric artery and the infra-pyloric artery. Thereby, PPG has a similar or even better short-term technical safety compared with DG. This should be corroborated by the final outcomes of large-scale RCTs.
Moreover, fewer patients in PPG group suffered from postoperative early dumping syndromes. The mechanisms of early dumping syndromes have yet to been confirmed. The resection of pyloric and/or vagus nerve might be associated with this phenomenon [36], and this is why there is a clear distinction between PPG patients and DG patients. However, few studies after 2010 have tried to report this complication after PPG, and a standard definition and diagnostic criteria of early dumping syndromes have not been identified. In addition, compromising hepatic and pyloric branches of the vagus nerve can increase the incidence of gallstones. In PPG, the physiological reconstruction without vagotomy maintains the contraction of Oddi sphincter and secretion of cholecystokinin [37, 38], whereas the risk of gallstones formation was decreased in the PPG group but not significantly in comparison with DG.
What’s more, the most frequent postoperative dysfunction in PPG was generally thought as DGE, and similar phenomenon was observed in our analysis. More DGE was found in the PPG group in the studies after 2010, the retrospective studies, and studies performed with laparoscopic PPG. This result may be caused by lesser extent of gastric resection, and subsequently the remaining pylorus and remnant stomach can result in postprandial fullness and dyspepsia. The influence of the antral cuff on DGE was investigated in our meta-analysis, in which studies with an antral cuff length of > 3 cm showed a significantly higher incidence of DGE, but one study with the antral cuff maintained < 3 cm did not reach a level of significance. Owing to just one article with < 3 cm antral cuff was published, the results may be influenced by the relatively small sample size. Additionally, Morita et al. retrospectively analyzed 408 patients with an antral cuff greater than 3 cm and less than 3 cm [39]. The difference among postoperative symptoms, including DGE, was not statistically significant. Moreover, comparing with patients with an antral cuff of 1.5 cm, better postoperative outcomes were found in those who had a 2.5 cm antral cuff [40]. In addition, the incidence of gastric stasis was lower with preservation of infra-pyloric blood supply in conventional pylorus-preserving gastrectomy (cPPG), which ranged from 5.7 to 8.0% reported previously [7, 9, 41, 42]. Kiyokawa et al. showed that delayed gastric emptying was found in 8.5% patients from the cPPG group but no patient in group with the preservation of infra-pyloric vein [42]. Moreover, intraoperative manual dilatation of pylorus also significantly reduced the DGE rate. The DGE rate in the cPPG group (8.6%) was significantly higher to that with manual dilatation (1.1%) among a total of 232 patients [43]. Therefore, the manual pyloric dilatation as well as preservation of infra-pyloric vessels might be an important step to minimize the most disturbing complications.
Postoperative endoscopic finding in this meta-analysis showed a favorable trend toward PPG. In the present study, the incidence of gastritis and bile regurgitation was significantly lower in PPG group, but significant difference in esophagitis was not found. For all enrolled studies, endoscopy was performed at least 6 months after the operation to evaluate esophagitis, gastritis, or bile reflux. In one retrospective study enrolled in this study with a follow-up of more than 5 years, the frequency of gastritis was significantly lower in the PPG group (10.0%) than in the DG group (63.6%), but the esophagitis frequency suggested no significant difference [18]. Park et al. demonstrated that gastritis and bile regurgitation postoperatively were only found in the DG group [4]. We think the most important factor was the reduction of the range of gastrectomy and retainment of pylorus function. The delayed gastric emptying resulting in food residue would be relevant to the development of inflammation in the remnant gastric [44]. Moreover, the chronic injury mediated by reflux of bile or gastric contents showed significant correlation with the increased incidence of Barrett’s esophagus, which is a known precursor of most esophageal adenocarcinomas [45]. Genco et al. recently reported 17.2% patients diagnosed with Barrett’s esophagus after bariatric surgery, while Barrett’s esophagus developed in 73.6% patients with reflux symptoms [46]. In the paper by Braghetto et al., Barrett’s esophagus was diagnosed between 5 and 6 years after surgery [47]. In terms of reducing the incidence of Barrett’s esophagus and the progression to esophageal adenocarcinomas, PPG has a significant advantage over DG, but a long-lasting screening and surveillance program is still necessary for early detection.
It was generally expected that PPG would improve nutrition index and decrease weight loss. For PPG cases, the recovery of total protein, albumin, and hemoglobin was better than DG cases. More extent of gastrectomy considerably reduced absorption and reservoir function of the stomach such as the secretion of gastric acid, and resection of the vagus nerve also influences the peristalsis of the stomach and duodenum. It is important that postoperative gastritis, bile regurgitation, and dumping syndrome may be associated with decreased oral intake and weight loss [17]. In the subgroup analysis, PPG leads to better function outcomes except the studies before 2010 had a similar albumin level compared with DG. For nutritional assessment, body weight loss was also a useful indictor, and the lower decreased rate of body weight was seen in our studies and subgroup analysis.
This meta-analysis had several limitations. First, given only one randomized controlled published to compare PPG and DG, most of enrolled studies were retrospective studies, and the inherent selection bias reduced the level of evidence. Second, all the participants in this meta-analysis were enrolled in the East Asia, therefore the results should be carefully generalizable to Western countries. Third, publication bias with Egger’s test was found in gastritis and body weight loss while not performed on parameters with insufficient studies. Despite performing considerable stratification analyses, we could not fully eliminate the statistical heterogeneity. Fourth, total protein, albumin, and hemoglobin were analyzed by SMD because of different assessment methods. Thus, large-scale RCTs compared with PPG and DG are needed to further corroborate these conclusions.
In conclusion, PPG is a feasible and safe option for early gastric cancer due to similar clinical effects as compared with DG. PPG has the benefits of decreasing risk of anastomotic leakage, early dumping syndrome, gastritis and bile reflux. It can prevent the deficiency of total protein, albumin and hemoglobin, and the loss of weight. However, the longer hospital day, decreased lymph node retrieval and more DGE may be the disadvantages of PPG. Moreover, the operation time, the blood loss, and the long-term survival rate showed no difference when compared to DG. These observations need to be confirmed by well-designed multicenter RCTs.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and its additional files.
Abbreviations
- PPG:
-
Pylorus-preserving gastrectomy
- DG:
-
Distal gastrectomy
- EGC:
-
Early gastric cancer
- LNs:
-
lymph nodes
- RCT:
-
Randomized clinical trial
- OR:
-
Odds ratio
- WMD:
-
Weight mean difference
- SMD:
-
Standardized mean difference
- CI:
-
Confidence interval
- SD:
-
Standard deviation
- HR:
-
Hazard ratio
- OS:
-
Overall survival
- DGE:
-
Delayed gastric emptying
- cPPG:
-
Conventional pylorus-preserving gastrectomy
References
Information Committee of Korean Gastric Cancer A. Korean Gastric Cancer Association Nationwide Survey on Gastric Cancer in 2014. Journal of gastric cancer. 2016;16(3):131–40.
Lee KJ, Inoue M, Otani T, Iwasaki M, Sasazuki S, Tsugane S, et al. Gastric cancer screening and subsequent risk of gastric cancer: a large-scale population-based cohort study, with a 13-year follow-up in Japan. Int J Cancer. 2006;118(9):2315–21.
Maki T, Shiratori T, Hatafuku T, Sugawara K. Pylorus-preserving gastrectomy as an improved operation for gastric ulcer. Surgery. 1967;61(6):838–45.
Park DJ, Lee HJ, Jung HC, Kim WH, Lee KU, Yang HK. Clinical outcome of pylorus-preserving gastrectomy in gastric cancer in comparison with conventional distal gastrectomy with Billroth I anastomosis. World J Surg. 2008;32(6):1029–36.
Zhu CC, Cao H, Berlth F, Xu J, Park SH, Choe HN, et al. Pylorus-preserving gastrectomy for early cancer involving the upper third: can we go higher? Gastric Cancer. 2019;22(4):881–91.
Imada T, Rino Y, Takahashi M, Suzuki M, Tanaka J, Shiozawa M, et al. Postoperative functional evaluation of pylorus-preserving gastrectomy for early gastric cancer compared with conventional distal gastrectomy. Surgery. 1998;123(2):165–70.
Xia X, Xu J, Zhu C, Cao H, Yu F, Zhao G. Objective evaluation of clinical outcomes of laparoscopy-assisted pylorus-preserving gastrectomy for middle-third early gastric cancer. BMC Cancer. 2019;19(1):481.
Shibata C, Shiiba KI, Funayama Y, Ishii S, Fukushima K, Mizoi T, et al. Outcomes after pylorus-preserving gastrectomy for early gastric cancer: a prospective multicenter trial. World J Surg. 2004;28(9):857–61.
Suh YS, Han DS, Kong SH, Kwon S, Shin CI, Kim WH, et al. Laparoscopy-assisted pylorus-preserving gastrectomy is better than laparoscopy-assisted distal gastrectomy for middle-third early gastric cancer. Ann Surg. 2014;259(3):485–93.
Song P, Lu M, Pu F, Zhang D, Wang B, Zhao Q. Meta-analysis of pylorus-preserving gastrectomy for middle-third early gastric cancer. Journal of Laparoendoscopic and Advanced Surgical Techniques. 2014;24:10.
Japanese Gastric Cancer A. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20(1):1–19.
Tsujiura M, Hiki N, Ohashi M, Nunobe S, Kumagai K, Ida S, et al. Should pylorus-preserving gastrectomy be performed for overweight/obese patients with gastric cancer? Gastric Cancer. 2019;22(6):1247–55.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Isozaki H, Okajima K, Momura E, Ichinona T, Fujii K, Izumi N, et al. Postoperative evaluation of pylorus-preserving gastrectomy for early gastric cancer. Br J Surg. 1996;83(2):266–9.
Zhang D, Shimoyama S, Kaminishi M. Feasibility of pylorus-preserving gastrectomy with a wider scope of lymphadenectomy. Arch Surg (Chicago, Ill : 1960). 1998;133(9):993-997.
Hotta T, Taniguchi K, Kobayashi Y, Johata K, Sahara M, Naka T, et al. Postoperative evaluation of pylorus-preserving procedures compared with conventional distal gastrectomy for early gastric cancer. Surg Today. 2001;31(9):774–9.
Tomita R, Fujisaki S, Tanjoh K. Pathophysiological studies on the relationship between postgastrectomy syndrome and gastric emptying function at 5 years after pylorus-preserving distal gastrectomy for early gastric cancer. World J Surg. 2003;27(6):725–33.
Urushihara T, Sumimoto K, Shimokado K, Kuroda Y. Gastric motility after laparoscopically assisted distal gastrectomy, with or without preservation of the pylorus, for early gastric cancer, as assessed by digital dynamic x-ray imaging. Surg Endosc. 2004;18(6):964–8.
Nunobe S, Sasako M, Saka M, Fukagawa T, Katai H, Sano T. Symptom evaluation of long-term postoperative outcomes after pylorus-preserving gastrectomy for early gastric cancer. Gastric Cancer. 2007;10(3):167–72.
Ikeguchi M, Hatada T, Yamamoto M, Miyake T, Matsunaga T, Fukuda K, et al. Evaluation of a pylorus-preserving gastrectomy for patients preoperatively diagnosed with early gastric cancer located in the middle third of the stomach. Surg Today. 2010;40(3):228–33.
Lee SW, Nomura E, Bouras G, Tokuhara T, Tsunemi S, Tanigawa N. Long-term oncologic outcomes from laparoscopic gastrectomy for gastric cancer: a single-center experience of 601 consecutive resections. J Am Coll Surg. 2010;211(1):33–40.
Tomikawa M, Korenaga D, Akahoshi T, Kohshi K, Sugimachi K, Nagao Y, et al. Quality of life after laparoscopy-assisted pylorus-preserving gastrectomy: an evaluation using a questionnaire mailed to the patients. Surg Today. 2012;42(7):625–32.
Fujita J, Takahashi M, Urushihara T, Tanabe K, Kodera Y, Yumiba T, et al. Assessment of postoperative quality of life following pylorus-preserving gastrectomy and Billroth-I distal gastrectomy in gastric cancer patients: results of the nationwide postgastrectomy syndrome assessment study. Gastric Cancer. 2016;19(1):302–11.
Isozaki H, Matsumoto S, Murakami S, Takama T, Sho T, Ishihara K, et al. Diminished gastric resection preserves better quality of life in patients with early gastric cancer. Acta Med Okayama. 2016;70(2):119–30.
Aizawa M, Honda M, Hiki N, Kinoshita T, Yabusaki H, Nunobe S, et al. Oncological outcomes of function-preserving gastrectomy for early gastric cancer: a multicenter propensity score matched cohort analysis comparing pylorus-preserving gastrectomy versus conventional distal gastrectomy. Gastric Cancer. 2017;20(4):709–17.
Hosoda K, Yamashita K, Sakuramoto S, Katada N, Moriya H, Mieno H, et al. Postoperative quality of life after laparoscopy-assisted pylorus-preserving gastrectomy compared with laparoscopy-assisted distal gastrectomy: a cross-sectional postal questionnaire survey. Am J Surg. 2017;213(4):763–70.
Eom BW, Park B, Yoon HM, Ryu KW, Kim YW. Laparoscopy-assisted pylorus-preserving gastrectomy for early gastric cancer: a retrospective study of long-term functional outcomes and quality of life. World J Gastroenterol. 2019;25(36):5494–504.
Kodama M, Koyama K. Indications for pylorus preserving gastrectomy for early gastric cancer located in the middle third of the stomach. World J Surg. 1991;15(5):628–33 discussion 33-4.
Sawai K, Takahashi T, Fujioka T, Minato H, Taniguchi H, Yamaguchi T. Pylorus-preserving gastrectomy with radical lymph node dissection based on anatomical variations of the infrapyloric artery. Am J Surg. 1995;170(3):285–8.
Kim BH, Hong SW, Kim JW, Choi SH, Yoon SO. Oncologic safety of pylorus-preserving gastrectomy in the aspect of micrometastasis in lymph nodes at stations 5 and 6. Ann Surg Oncol. 2014;21(2):533–8.
Kong SH, Kim JW, Lee HJ, Kim WH, Lee KU, Yang HK. The safety of the dissection of lymph node stations 5 and 6 in pylorus-preserving gastrectomy. Ann Surg Oncol. 2009;16(12):3252–8.
Oh SY, Lee HJ, Yang HK. Pylorus-preserving gastrectomy for gastric cancer. Journal of gastric cancer. 2016;16(2):63–71.
Tokunaga M, Hiki N, Fukunaga T, Ohyama S, Yamada K, Yamaguchi T. Better prognosis of T2 gastric cancer with preoperative diagnosis of early gastric cancer. Ann Surg Oncol. 2009;16(6):1514–9.
Tu RH, Lin JX, Zheng CH, Li P, Xie JW, Wang JB, et al. Development of a nomogram for predicting the risk of anastomotic leakage after a gastrectomy for gastric cancer. Eur J Surg Oncol. 2017;43(2):485–92.
Machella TE. The mechanism of the post-gastrectomy “Dumping” syndrome. Ann Surg. 1949;130(2):145–59.
Kobayashi T, Hisanaga M, Kanehiro H, Yamada Y, Ko S, Nakajima Y. Analysis of risk factors for the development of gallstones after gastrectomy. Br J Surg. 2005;92(11):1399–403.
Nabae T, Takahata S, Konomi H, Deng ZL, Yokohata K, Chijiiwa K, et al. Effect of prepyloric gastric transection and anastomosis on sphincter of Oddi cyclic motility in conscious dogs. J Gastroenterol. 2001;36(8):530–7.
Morita S, Sasako M, Saka M, Fukagawa T, Sano T, Katai H. Correlation between the length of the pyloric cuff and postoperative evaluation after pylorus-preserving gastrectomy. Gastric Cancer. 2010;13(2):109–16.
Nakane Y, Michiura T, Inoue K, Sato M, Nakai K, Yamamichi K. Length of the antral segment in pylorus-preserving gastrectomy. Br J Surg. 2002;89(2):220–4.
Nunobe S, Hiki N, Fukunaga T, Tokunaga M, Ohyama S, Seto Y, et al. Laparoscopy-assisted pylorus-preserving gastrectomy: preservation of vagus nerve and infrapyloric blood flow induces less stasis. World J Surg. 2007;31(12):2335–40.
Kiyokawa T, Hiki N, Nunobe S, Honda M, Ohashi M, Sano T. Preserving infrapyloric vein reduces postoperative gastric stasis after laparoscopic pylorus-preserving gastrectomy. Langenbeck's Arch Surg. 2017;402(1):49–56.
Zhu CC, Kim TH, Berlth F, Park SH, Suh YS, Kong SH, et al. Clinical outcomes of intraoperative manual dilatation of pylorus in pylorus-preserving gastrectomy: a retrospective analysis. Gastric Cancer. 2018;21(5):864–70.
Lee Y, Tokunaga A, Tajiri T, Masuda G, Okuda T, Fujita I, et al. Inflammation of the gastric remnant after gastrectomy: mucosal erythema is associated with bile reflux and inflammatory cellular infiltration is associated with Helicobacter pylori infection. J Gastroenterol. 2004;39(6):520–6.
Spechler SJ, Souza RF. Barrett’s esophagus. N Engl J Med. 2014;371(9):836–45.
Genco A, Soricelli E, Casella G, Maselli R, Castagneto-Gissey L, Di Lorenzo N, et al. Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2017;13(4):568–74.
Braghetto I, Csendes A. Prevalence of Barrett’s esophagus in bariatric patients undergoing sleeve gastrectomy. Obes Surg. 2016;26(4):710–4.
Acknowledgements
We would like to appreciate the teams for their tremendous contribution to these high-quality studies.
Funding
There was no sponsor for this study.
Author information
Authors and Affiliations
Contributions
XYM was the major contributor in data collection, data analysis, and manuscript writing. XLX contributed to data collection and analysis. BLW was the major contributor of the design of the study. HZ, CPJ, and XL were substantially involved in data check and data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Newcastle–Ottawa quality assessment scale.
Additional file 2.
Forest plot of each outcome. (a) Age; (b) Sex; (c) BMI; (d) Tumor size; (e) PRM; (f) DRM; PRM, proximal resection margin; DRM, distal resection margin.
Additional file 3.
Assessment of quality of studies.
Additional file 4.
Forest plot of each outcome. (a) Gastritis; (b) Esophagitis; (c) Bile reflux; (d) Early dumping syndrome; (e) Time to half gastric emptying.
Additional file 5.
Forest plot of each outcome. (a) Survival rate; (b) Recurrence.
Additional file 6.
Funnel plots comparing (a) Gastritis, (b) Esophagitis, (c) Bile reflux, (d) Early dumping.
Additional file 7.
Galbraith plots comparing (a) Operative time, (b) Blood loss, (c) Number of retrieved lymph nodes, (d) Hospital day, (e) Postoperative complication, (f) Anastomotic leakage.
Additional file 8.
Galbraith plots comparing (a) Delayed gastric emptying, (b) Gallstone, (c) Total protein, (d) Albumin, (e) Hemoglobin, (f) Body weight loss.
Additional file 9.
Galbraith plots comparing (a) Gastritis, (b) Esophagitis, (c) Bile reflux, (d) Early dumping syndrome.
Additional file 10.
PRISIMA checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mao, X., Xu, X., Zhu, H. et al. A comparison between pylorus-preserving and distal gastrectomy in surgical safety and functional benefit with gastric cancer: a systematic review and meta-analysis. World J Surg Onc 18, 160 (2020). https://doi.org/10.1186/s12957-020-01910-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-020-01910-y