Abstract
Background
Nivolumab, an immune checkpoint inhibitor, is recently clinically applied to non-small cell lung cancer (NSCLC) treatment, and this causes T cell activation and T cell infiltration to tumor tissue through the blockade of the interaction between programmed cell death 1 (PD-1) and programmed cell death ligand 1 (PD-L1). 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) sometimes shows false positive because of the recruitment of neutrophils, lymphocytes, and macrophages. To date, there is only one report except our case, which described the correlation between FDG-PET and nivolumab.
Case presentation
We report on a 75-year-old man on nivolumab treatment for metastatic non-small cell lung cancer. He had undergone right lower lobectomy for lung adenocarcinoma in the right S8 segment 10 months prior to recurrence. Pathological findings revealed invasive adenocarcinoma, pT1bN2M0 stage IIIA. Epidermal growth factor receptor (EGFR) mutation was positive for de novo T790M and anaplastic lymphoma kinase (ALK) rearrangement was negative. Immunohistochemistry was negative for PD-L1. He underwent chemotherapy with a combination of cisplatin and pemetrexed for four cycles but developed progressive disease involving the right hemithorax, multiple lymph nodes, and multiple osseous sites. Nivolumab was instituted as a second-line chemotherapy. After six courses of this immunotherapy, FDG-PET scan showed decreased FDG uptake in each recurrent lesion despite T lymphocyte activation by nivolumab. Serum carcinoembryonic antigen (CEA) level was also remarkably decreased.
Conclusions
Nivolumab’s effect on recurrent NSCLC may be monitored by PET; larger studies are needed.
Similar content being viewed by others
Background
Lung cancer is the leading cause of cancer-related death worldwide [1]. Advances in the treatment of non-smallcell lung cancer (NSCLC) in the past decade include third-generation platinum doublets, epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) in EGFR mutation-positive lung cancer, anaplastic lymphoma kinase (ALK) TKIs in ALK rearrangement-positive disease, maintenance systemic therapy, and second- or third-line treatment, which improve survival [2–9]. In recent years, immune checkpoint inhibitors have been introduced [10–12], and their effectiveness is promising. Nivolumab, an immune checkpoint inhibitor that is an antibody against programmed death-1 (PD-1), causes T cell activation and demonstrates clinically relevant antitumor activity. In some phase III trials, overall survival (OS), objective response rate (ORR), and progression-free survival (PFS) were better with nivolumab than with docetaxel in NSCLC [13, 14].
18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) is an effective tool for assessing treatment response and surveillance of disease recurrence; however, it sometimes shows increased FDG uptake at sites of local inflammatory changes caused by the recruitment of neutrophils, lymphocytes, and macrophages [15]. We present a case of a patient with metastatic NSCLC who underwent nivolumab treatment as a second line chemotherapy and whose PET scan showed decreased FDG uptake after treatment in spite of nivolumab’s known T cell activation properties.
Case presentation
A 75-year-old man was admitted to our hospital because of metastatic NSCLC. He had undergone right lower lobectomy for lung adenocarcinoma originating in the right S8 segment as initial treatment. Postoperative findings revealed invasive adenocarcinoma with pT1bN2M0 stage IIIA. An EGFR mutation was positive for de novo T790M, and ALK rearrangement was negative. Immunohistochemistry was negative for programmed death ligand 1 (PD-L1) (Fig. 1). Ten months after his initial surgery, recurrence was detected in the form of multiple bone and lymph nodes metastases and right intrathoracic dissemination. He underwent chemotherapy with a combination of cisplatin and pemetrexed for four cycles (Bevacizumab was withheld because of his past history of cerebral hemorrhage.). After first line chemotherapy, his clinical imaging revealed increasing size and number of metastatic sites, which were graded as progressive disease (PD) according to the Response Evaluation Criteria in Solid Tumors 1.1 (RECIST) [16]. We decided to administer nivolumab (3 mg/kg) every 2 weeks as a second-line chemotherapy. Before starting this immunotherapy, his medical check-up revealed stable borderline diabetes. Hormonal examination such as adrenocorticotropic hormone (ACTH), ftee T3 (FT3), free T4 (FT4), thyroid-stimulating hormone (TSH), and anti-acetylcholine receptor antibody (anti-AchR Ab) were also within normal range. No adverse events occurred during the course of this immunotherapy.
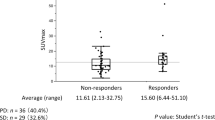
After six courses of this immunotherapy, an FDG-PET scan showed decreased FDG uptake in each recurrent lesion (Fig. 2). Serum carcinoembryonic antigen (CEA) levels were also decreased (Fig. 3).
FDG uptake before (a) and after (b) immunotherapy. Maximum standardized uptake value (SUVmax) of supraclavicular lymph node and disseminated lesions before and after immunotherapy decreased from 9.8 to no accumulation and 5.9 to 3.4, respectively. Each SUVmax was decreased after six courses of nivolumab treatment
Discussion
In patients with recurrent or advanced NSCLC, who have relapsed after previous platinum-based chemotherapy or EGFR-TKI, docetaxel monotherapy is considered to be the current standard treatment regimen [5, 7]. In a phase III study involving docetaxel in patients with NSCLC previously treated with platinum-based chemotherapy, the time to progression and median survival time (MST) after docetaxel monotherapy has been reported to be 10.6 weeks and 7.0 months, respectively [6]. Recent prospective studies including CheckMate 017 [13] and CheckMate 057 [14] showed that nivolumab was superior to docetaxel for squamous cell carcinoma and non-squamous cell carcinoma previously treated with platinum-based agents. Based on these studies, the current second-line chemotherapy in patients failing platinum-based chemotherapy is considered to be nivolumab. These studies suggested that a radiological response had been detected approximately 8 weeks (4th course) after initial administration of nivolumab.
The combination of FDG-PET and computed tomography (CT) is an effective tool for assessing treatment response and for surveillance for disease recurrence in cases treated with chemotherapy or radiation. Many investigators have reported the utility of FDG-PET or FDG-PET/CT in evaluating therapeutic response prospectively or retrospectively [17–20]. Complete disappearance of abnormal FDG accumulation is an indicator of a low probability of local recurrence and better prognosis after treatment such as surgery, radiation, and chemotherapy. Immunotherapy presents a potential problem because the inflammatory changes caused by the recruitment of neutrophils, lymphocytes, and macrophages [15] may lower the specificity because these cells take up FDG. More specifically, immune checkpoint inhibitors activate T cells, which infiltrate tumor tissue. Uptake by the T cells might affect the evaluation of immunotherapy. To date, there is only one report except our case, which showed the usefulness of FDG-PET/CT to evaluate the efficacy of nivolumab in a patient with indolent Hodgkin lymphoma [21]. Although we usually evaluate the anatomic tumor response with RECIST [16] or immune-related Response Criteria (irRC) [22] after cancer treatment, Wall et al. [23] proposed PET Response Criteria in Solid Tumors version 1.0 (PERCIST) to assess the treatment response instead of RECIST. PERCIST evaluates the metabolic tumor response using the change of SUV ratio in the region of interest between the tumor and liver. The evaluation criteria of PERCIST would be more helpful to evaluate the treatment effects in the cases with FDG-PET.
The optimal follow-up schedule of FDG-PET scan during immunotherapy is unclear. In fact, little is known about the role of FDG-PET and CT scan as appropriate radiological modalities. Some exploratory clinical studies (UMIN000020707 and UMIN000020814) have been conducted and ongoing in Japan to evaluate FDG-PET in nivolumab therapy. In our case, FDG-PET was considered to be a useful tool for the evaluation during immunotherapy. However, it is uncertain what the optimal timing of FDG-PET scanning will yield the highest specificity and sensitivity. More research in this area is needed.
An urgent issue to be resolved is to explore more specific biomarker of this treatment because the correlation between PD-L1 expression by the tumor tissue and treatment effect with nivolumab has not been quantified. However, immunotherapy shows promise to improve the prognosis of patients with unresectable or recurrent NSCLC.
Conclusions
We have found decreased FDG uptake by tumor after six courses of nivolumab treatment, suggesting the potential value of FDG-PET in monitoring the response to this immunotherapy. T cell activation and infiltration into tumor tissue did not affect the results of FDG-PET in this case. We await detailed results of ongoing clinical studies using FDG-PET for the evaluation of this immunotherapy.
Abbreviations
- ALK:
-
Anaplastic lymphoma kinase
- CEA:
-
Carcinoembryonic antigen
- CT:
-
Computed tomography
- EGFR:
-
Epidermal growth factor receptor
- FDG-PET:
-
18F-fluorodeoxyglucose-positron emission tomography
- MST:
-
Median survival time
- NSCLC:
-
Non-smallcell lung cancer
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PD-1:
-
Programmed death-1
- PD-L1:
-
Programmed death ligand 1
- PFS:
-
Progression-free survival
- RECIST:
-
Response Evaluation Criteria in Solid Tumors 1.1
- TKIs:
-
Tyrosine kinase inhibitors
- ACTH:
-
Adrenocorticotropic hormone
- FT3:
-
Free T3 (free triiodothyronine)
- FT4:
-
Free T4 (free tetraiodothyronine)
- TSH:
-
Thyroid-stimulating hormone
References
Surveillance, epidemiology, and end results (SEER) cancer statistics review, 1975-2010. http://seer.cancer.gov/csr/1975_2010. Accessed 14 June 2013.
Scagliotti GV, Parikh P, von Pawel J, Biesma B, Vansteenkiste J, Manegold C, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naïve patients with advanced-stage non small cell lung cancer. J Clin Oncol. 2008;26:3543–51.
Mok TS, Wu Y, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–57.
Ciuleanu T, Brodowicz T, Zielinski C, Kim JH, Krzakowski M, Laack E, et al. Maintenance pemetrexed plus best supportive care versus placebo plus best supportive care for non-small cell lung cancer: a randomized, double-blind, phase 3 study. Lancet. 2009;374:1432–40.
Fossella FV, DeVore R, Kerr RN, Crawford J, Natale RR, Dunphy F, et al. Randomized phase III trial of docetaxel versus vinorelbine or ifosfamide in patients with advanced non-small cell lung cancer previously treated with platinum-containing chemotherapy regimens. J Clin Oncol. 2000;18:2354–62.
Shepherd FA, Dancey J, Pamlau R, Mattson K, Gralla R, O’Rourke M, et al. Prospective randomized trial of docetaxel versus best supportive care in patients with non-small cell lung cancer previously treated with platinum-based chemotherapy. J Clin Oncol. 2000;18:2095–103.
Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh V, et al. Erlotinib in previously treated non-small cell lung cancer. N Engl J Med. 2005;353:123–32.
Hanna N, Shepherd FA, Fossella FV, Pereira JR, De Marinis F, von Pawel J, et al. Randomized phase III trial of pemetrexed versus docetaxel in patients with non-small cell lung cancer previously treated with chemotherapy. J Clin Oncol. 2004;22:1589–97.
Shaw AT, Kim DW, Nakagawa K, Seto T, Crinó L, Ahn MJ, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368:2385–94.
Ishida Y, Agata Y, Shibahara K, Honjo T. Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J. 1992;11:3887–95.
Nishimura H, Minato N, Nakano T, Honjo T. Immuno-logical studies on PD-1 deficient mice: implication of PD-1 as a negative regulator for B cell responses. Int Immunol. 1998;10:1563–72.
Iwai Y, Ishida M, Tanaka Y, Okazaki T, Honjo T, Minato N. Involvement of PD-L1 on tumor cells in the escape from host immune system and tumor immunotherapy by PD-L1 blockade. PNAS. 2002;22:12293–7.
Brahmer J, Reckamp KL, Baas P, Crino L, Eberhardt WE, Poddubskaya E, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373:123–35.
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–39.
Higuchi M, Suzuki H, Gotoh M. Role od PET/computed tomography in radiofrequency ablation for malignant pulmonary tumors. PET Clin. 2016;11:47–55.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Higuchi M, Honjo H, Shigihara T, Shishido F, Suzuki H, Gotoh M. A phase II study of radiofrequency ablation therapy for thoracic malignancies with evaluation by FDG-PET. J Cancer Res Clin Oncol. 2014;140:1957–63.
Alafate A, Shinya T, Okumura Y, Sato S, Hiraki T, Ishii H, et al. The maximum standardized uptake value is more reliable than size measurement in early follow-up to evaluate potential pulmonary malignancies following radiofrequency ablation. Acta Med Okayama. 2013;67:105–12.
Higaki F, Okumura Y, Sato S, Hiraki T, Gobara H, Mimura H, et al. Preliminary retrospective investigation of FDG-PET/CT timing in follow-up of ablated lung tumor. Ann Nucl Med. 2008;22:157–63.
Weber WA. Use of PET for monitoring cancer therapy and for predicting outcome. J Nucl Med. 2005;46:983–95.
Alagoz E, Ince S, Okuyucu K, Ayan A, San H, Balkan E, et al. Complete remission on 18-fluorodeoxyglucose positron emission tomography/computed tomography after nivolumab treatment in a patient with indolent Hodgkin lymphoma. Transl Cancer Res. 2016;5:320–3.
Wolchok JD, Hoos A, O’Day S, Weber JS, Hamid O, Lebbe C, et al. Guideline for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res. 2009;15:7412–20.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50 Suppl 1:122S–50.
Acknowledgements
None.
Funding
None.
Availability of data and materials
Data will not be shared because this is a case report and privacy of this participant should be protected.
Authors’ contributions
MH collected and assembled data and drafted the article. YO, TI, YW, TY, MF, and TH helped to collect data. HS helped to draft the article and finally approved the article. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written consent was obtained from the patient for the publication of this case report and accompanying images.
Ethics approval and consent to participate
This case report was approved by Ethics Committee of Fukushima Medical University, and written consent was obtained from the patient for the publication of this case report and accompanying images.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Higuchi, M., Owada, Y., Inoue, T. et al. FDG-PET in the evaluation of response to nivolumab in recurrent non-small-cell lung cancer. World J Surg Onc 14, 238 (2016). https://doi.org/10.1186/s12957-016-0998-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-016-0998-y