Abstract
Background
The management of pediatric recurrent or metastatic soft tissue sarcoma after multimodal treatment remains challenging. We investigated the feasibility, efficacy, and morbidity of permanent interstitial 125I seed implantation under image guidance as a salvage treatment for pediatric patients with recurrent or metastatic soft tissue sarcoma.
Methods
This was a retrospective study of 10 patients who underwent percutaneous ultrasound or computed tomography (CT) guided permanent 125I seed implantation. Postoperative dosimetry was performed for all patients. Actuarial D90 was 121–187.1 Gy (median, 170.3 Gy). The number of 125I seeds implanted was 6–158 (median, 34.5), with a median specific activity of 0.7 mCi per seed (range, 0.62–0.8 mCi); total activity was 4.2–113.76 mCi. Follow-up time was 6–107 months (median, 27.5 months); no patients were lost to follow-up.
Results
The overall response rate (complete response + partial response) was 8/10 (80 %), including two patients with complete response (CR) (20 %) and five patients with partial response (PR) (60 %). Local control rates after 1 and 2 years were 70.1 and 62.3 %, respectively, with a mean local control time of 70.6 months (95 % confidence interval (CI) 45.1–96.0). Survival rates after 1 and 2 years were 68.6 and 57.1 %, respectively, with a mean survival time of 65.3 months (95 % CI 34.1–96.5). Three patients died from distant metastasis; one died from local recurrence 12 months after seed implantation. Three patients suffered a grade I skin reaction and one developed ulceration. No severe adverse neurologic sequelae or blood vessel damage occurred.
Conclusions
Image guided permanent interstitial 125I seed implantation as a salvage treatment appears to have a satisfactory outcome in children with recurrent or metastatic soft tissue sarcoma.
Similar content being viewed by others
Background
Soft tissue sarcomas (STSs) are rare mesenchymal tumors that represent 7–10 % of pediatric malignancies [1]. Although external beam radiotherapy (EBRT) after surgery has greatly improved local control, a series of clinical reports indicates that the locoregional recurrence rate is still about 8–20 % even after such management. Patients with local recurrence or metastasis of STS usually have a poor prognosis [1–4]. Recently, new therapeutic regimens for pediatric recurrent and metastatic STS have been developed; however, these have not resulted in favorable local control or survival rates, and the management of local recurrence and distant metastases thus remains challenging and nonstandardized. These difficulties are exacerbated by the fact that most pediatric patients undergo complex multidisciplinary management including numerous surgical procedures, radiotherapy, chemotherapy, and various combinations of these treatments.
In pediatric patients with recurrent or metastatic STS, local control may be regained by further surgery with adequate margins (wide or radical) and EBRT, though data on the survival benefit are limited. Adjuvant EBRT is known to be effective in reducing the recurrence rate [5] but is limited by the tolerance of the surrounding normal tissues or organs at risk (OARs), which makes it difficult to achieve a lethal dose to the sarcoma and ultimately leads to local recurrence or metastasis. Interstitial implantation of 125I seeds is a promising salvage therapy for many different recurrent and metastatic malignant tumors that has been used in, for example, re-recurrent rectal carcinoma [6], recurrent head and neck carcinoma [7], and metastatic lymph nodes [8, 9]. Interstitial permanent brachytherapy (BRT) brings new hope for the treatment of recurrent and metastatic STS in children because the radiation dose is well localized to the tumor bed and adjacent uninvolved tissues are spared [10–16]. However, the literature on experience with the use of permanent interstitial 125I seeds in pediatric patients is limited. It is therefore necessary to investigate the feasibility and efficacy of image guided permanent implantation of 125I seeds as a salvage therapy for locally recurrent STS in children and to determine local control, survival, and complications.
Methods
Patient information and selection
We retrospectively analyzed 10 pediatric patients (median age, 15 years; range, 4–20 years) with recurrence or metastasis of STS who underwent percutaneous ultrasound (color Doppler with probe and guidance stabilization devices; Aloka 550-5000) or computed tomography (CT) guided permanent 125I seed implantation at Peking University Third Hospital from December 2005 to March 2014. This study was approved by the ethics committee in Peking University Third Hospital and followed the guidelines for experimental investigation with human subjects required by our institution.
Eligibility criteria were as follows: written informed consent obtained from parents/guardians before seed implantation; the recurrent or metastatic tumor diagnosed by CT or magnetic resonance imaging (MRI); histologically proven recurrent STS after surgery; EBRT, chemotherapy, or a combination of these treatments; Karnofsky Performance Status score 60 or higher; and no severe dysfunction of the kidneys, liver, or bone marrow. Before implantation, the history of all patients was taken and physical examination, routine hematology and biochemistry, CT or ultrasonography of the lesions, and chest radiography were performed. Patients and primary tumor characteristics are shown in Table 1.
Seven of the 10 patients were boys, and three were girls. Two patients had re-recurrence after their third and fourth surgical procedures, respectively. One patient developed recurrence and metastasis after radical resection. Two patients who suffered recurrence after surgery received EBRT (median, 59 Gy; range, 58–60 Gy) but were re-recurrence. One patient experienced recurrence after surgery in combination with EBRT at 60 Gy. Two patients who were deemed unsuitable for surgery when initially reviewed suffered recurrence after adjuvant chemotherapy (median, 14 cycles; range, 12–16 cycles) and EBRT (median, 45.3 Gy; range, 33–57.5 Gy). One patient with pulmonary metastasis had recurrence disease after neoadjuvant chemotherapy (4 cycles), radical resection, EBRT (36 Gy), and adjuvant chemotherapy (8 cycles). In one patient, recurrence developed 17 months after initial intraoperative 125I seed implantation and subsequent chemotherapy (12 cycles). There were six cases of distant metastasis among the 10 patients; these caused mild to moderate pain and limited movement of the limbs to differing degrees. One patient developed blindness with exophthalmos due to compression of the right optic nerve by a metastasis. Two patients had difficulty opening their mouth. The treatment history before 125I seed implantation for each patient is listed in Table 2. All of the cases in this study had been interviewed by surgeons and radiation oncologists who had considered them unsuitable for salvage surgery and EBRT or the parents/guardians had refused to undergo surgery or EBRT.
Pretreatment planning
One to two weeks before seed implantation, a detailed CT/ultrasound aided tumor volume study was performed for all patients. We obtained CT transverse images of the targets at 5 mm intervals. The images were transferred to a three-dimensional radiation therapy planning system (3D-TPS; Beijing Astro Technology Co. Ltd, Beijing, China). An experienced radiation oncologist outlined the gross tumor volume (GTV) and the OARs on each transverse image. The planning target volume included the entire GTV with a 0.5–1-cm margin that was covered by the 90 % isodose curve. The D90 (prescribed dose delivered to 90 % of the target volume) of seed implant was calculated by the 3D-TPS. The total number and activity of 125I seeds to be implanted were determined according to our experience in previous studies [6–8].
Image guided seed implant protocol
Under adequate local or general anesthesia, five patients underwent seed implant under CT guidance and the remainder underwent seed implant under ultrasound guidance. After the target volume had been determined, 18-gauge needles were implanted into the mass and spaced at a distance of 1.0 cm in a parallel array, extending at least 0.5–1.0 cm beyond the margins of the tumor. The direction of the needles was adjusted to avoid large blood vessels. The exact puncture process depended primarily on the operator’s experience. 125I seeds (Model 6711; t1/2, 59.4 days; energy, 27.4–31.4 keV; half-value layer of lead, 0.0025 cm; half-value layer of tissue, 2.0 cm; Beijing Atom and High Technique Industries Inc., Beijing, China) were implanted using a Mick applicator (Mick Radio-Nuclear Instruments Inc., Mount Vernon, NY, USA), with spaces between seeds (center to center) of approximately 1.0 cm. The needles were then removed.
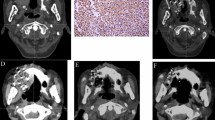
Postimplantation dosimetry
Postoperative dosimetry was routinely performed for all patients immediately or 24 h after implantation using three-dimensional seed identification and 5-mm thickness CT scans. The contoured images and sources were entered into TPS software. Actual isodose distributions for each slice (Fig. 1) and dose–volume histograms for the target were generated (Fig. 2). Post-planning evaluation showed the actuarial D90 to be 121–187.1 Gy, with a median of 170.3 Gy. The number of 125I seeds implanted ranged from 6 to 158, with a median of 34.5. The median specific activity of the 125I seeds was 0.7 mCi per seed (range, 0.62–0.8 mCi). The total activity was 4.2–113.76 mCi.
Definition of treatment response
Pain intensity was evaluated and graded according to the Numeric Rating Scale for chronic pain: 1–3 represented mild pain, 4–6 moderate pain, and 7–10 severe pain [17].
Local tumor response was evaluated by CT 2 months after seed implantation according to the Response Evaluation Criteria in Solid Tumors version 1.1 (RECIST) [18]. Briefly, complete response (CR) was defined as the complete disappearance of the lesion, without the appearance of any new lesions and then maintained for 4 weeks. Partial response (PR) referred to a more than 30 % decrease in the sum of the largest diameters of target lesions. Progressive disease (PD) was defined as at least a 20 % increase in the sum of the largest diameters of target lesions or the appearance of any new lesions. Stable disease (SD) was defined as neither sufficient shrinkage to qualify for PR nor sufficient increase to qualify for PD. The response rate was equal to the CR + PR.
Complications were scored using the Radiation Therapy Oncology Group (RTOG)/European Organisation for Research and Treatment of Cancer Late Radiation Morbidity Score Criteria [19].
Follow-up
Patients were initially evaluated by radiation oncologists and surgeons 4 weeks after seed implantation and thereafter every 2–3 months, or more frequently if a new clinical sign or symptom appeared. After 2 years, the patients were followed-up every 6 months. Patient follow-up time was calculated from the date of seed implant and ranged from 7 to 107 months (median, 27.5 months); no patients were lost to follow-up. Disease status was assessed by physical examination, liver function tests, and complete blood and platelet counts. Imaging, including CT, MRI, and ultrasonography was used to confirm relapse events.
Statistical analysis
Overall survival and local control rates were analyzed with PASW Statistics version 18.0 using the Kaplan–Meier method. Survival time was determined from the date of seed implantation to the date of death or the last follow-up. Deaths for any reason were scored as events when calculating survival rates. Local recurrence was defined as tumor progression within the implanted area or surrounding regions observed on CT, MRI, or ultrasonography.
Results
Response to treatment
Ten pediatric patients with 12 recurrent and two metastatic lesions were studied. After seed implant, the intensity of pain decreased to mild pain for the two patients who had suffered moderate pain and had difficulty opening their mouth. In the patient with exophthalmos, this was alleviated. One patient with limited right upper limb outreach recovered completely to normal. However, two other patients did not experience relief of limb movement restriction (one right upper limb, one right leg). 125I seed treatment details and outcomes are summarized in Table 3.
Tumor local control
The overall response rate (CR + PR) was 8/10 (80 %), including two patients with CR (20 %) and five patients with PR (60 %). One of the 10 patients had stable disease (SD; 10 %) and one had progressive disease (PD;10 %). Local control rates after 1 and 2 years were 70.1 and 62.3 %, respectively, with a mean local control time of 70.6 months (95 % confidence interval (CI) 45.1–96.0) (Fig. 3).
Overall survival
Survival rates after 1 and 2 years were 68.6 and 57.1 %, respectively, with a mean survival time of 65.3 months (95 % CI 34.1–96.5) (Fig. 4). At the time of writing, three of the patients had died from multiple metastasis; one patient died from local recurrence 12 months after seed implantation. Six patients were still alive with no evidence of local recurrence or distant metastases.
Toxicity and complications
Three patients suffered a grade I skin reaction that presented with local pigmentation after seed implantation. One patient developed an ulceration associated with disease progression and died due to pulmonary metastasis 6 months after seed implantation. No seeds were found to have migrated. No adverse neurologic sequelae or blood vessel damage occurred. No serious RTOG grade IV late complications were observed.
Discussion
EBRT plays an important role in the treatment of STS in children. Radiotherapeutic approaches include EBRT, BRT, and intraoperative radiotherapy. However, EBRT can cause severe complications in the pediatric population, including growth retardation and effects on organ function. Although there are no randomized clinical trials comparing the curative effect of EBRT and BRT in patients with recurrent STS, theoretically, compared with EBRT, BRT has several advantages for pediatric patients with recurrent and/or metastatic STS after surgical resection. Due to its radiobiologic characteristics, BRT can deliver higher doses of radiation to the area most susceptible to recurrence while delivering a lower dose to the normal tissues surrounding the target. Furthermore, BRT enables a short overall treatment time, and the rate of local control is comparatively high. Given the data in the literature, we can conclude that BRT is generally the only radiotherapeutic option available when high grade STS recurs in a previously irradiated area [13–15, 20–22].
BRT usually involves the temporary or permanent surface, intracavitary, or interstitial application of radioisotopes. Many types of BRT are being investigated, including interstitial high dose rate BRT (HBRT), low dose rate brachytherapy (LBRT), intraoperative HBRT, and combinations of these modalities. However, no clinical trial has compared HBRT with LBRT for recurrent STS. In some pediatric cases, HBRT with 192Ir has been used either alone or in combination with EBRT in the management of STS and has been shown to provide good local control and overall survival rates. Gustavo et al. [16] reported their experience of treating STS with HBRT alone or in combination with EBRT in 18 pediatric patients (age, 2–16 years; median, 11 years) who had intermediate to high grade tumors at the time that HBRT was performed. With a median follow-up of 79.5 months (range, 12–159 months), overall survival rates at 5 and 10 years were 84.4 and 72.4 % and the overall local control rates for the HBRT group (eight cases) and the HBRT plus EBRT group (10 cases) were 100 and 90 %, respectively. Merchant et al. [10] previously reported that, for pediatric patients with STS, BRT was an excellent treatment option. In their study, 31 patients of median age 11 years (range, 1–21 years) were managed with BRT initially or at the time of recurrence using 125I or 192Ir in a temporary or permanent manner. At the time of follow-up, 25 patients were alive, with a median survival time of 34 months.
In the present study, all patients were treated with interstitial permanent implantation of 125I seeds. Interstitial 125I seed implantation is a method of LBRT that for many years has been a gold standard prostate BRT in low risk patients. 125I seeds implanted in a tumor continuously emit low dose X-rays and γ-rays; during the half-life of 125I, they deliver a dose of 160–180 Gy to the local tissues, sparing adjacent normal structures and medical personnel. This slow emission allows any normal tissue that does receive a sublethal or potentially lethal dose of radiation to repair and recover [23]. Also, continuous low dose irradiation may reduce the oxygen enhancement ratio, which may improve the efficacy of the treatment in hypoxic portions of the tumor [24]. In addition, the therapeutic benefit may theoretically be enhanced by natural increases in local dose after radiation-induced tumor shrinkage brings the 125I seeds closer together [25]. Finally, permanent interstitial 125I seed implantation is a quick, 1 day therapy with a low complication rate both during and after the procedure [6–9]. Taking all of these benefits into account, permanent 125I seed implantation may be well suited for the management of pediatric STS, especially in patients with recurrence and/or metastasis who have already received multimodal treatment.
Hentz and Barrett [26] reviewed eight pediatric patients with rhabdomyosarcoma who were treated with temporary LBRT using 125I, with promising results. The local recurrence rate was 12.5 % after treatment, and the side effects were endurable, especially in patients who had no prior history of irradiation. Zhang et al. [27] reported a total survival rate of 88 % in eight children during a median follow-up of 43 months. Li et al. [28] demonstrated that when a combination of 125I seeds and an artificial prosthesis was used to replace tumor tissue in three patients, limb function recovered well. The patients remained disease-free for 14–18 months and experienced no severe complications such as infection or wound bleeding.
The success of 125I BRT mainly depends on the precise location of the implant needles. In the present study, 125I seed implant was guided by CT or ultrasound, which ensures accurate placement of seeds within a known volume of tumor [29, 30]. Optimization of seed distribution and dose homogeneity can easily be achieved by adjusting the position of each needle and seed during implant according to the pretreatment plan. In this respect, 125I seed implantation is a safe radiotherapy and delivers more conformal radiation. However, few authors have reported on percutaneous seed implantation as a sole therapy for recurrent or metastatic STS under image guidance, especially in pediatric patients. In the present study, we performed permanent interstitial 125I seed implantation as a salvage therapy for pediatric recurrent and metastatic STS. Our results demonstrate satisfactory tumor local control and overall survival rates. Organ function and cosmetic appearance were maintained and uncompromised.
Conclusions
Image guided permanent interstitial 125I seed implantation as a sole salvage modality is a feasible, minimally invasive treatment for pediatric recurrent or metastatic STS, with few complications. It avoids the morbidity associated with further surgery or EBRT and achieves high survival and local control rates with endurable toxicity. The long-term results of this promising procedure with a greater number of cases are needed to reach a definite conclusion.
Abbreviations
- 3D-TPS:
-
three-dimensional radiation therapy planning system
- AJCC:
-
American Joint Committee on Cancer
- BRT:
-
interstitial permanent brachytherapy
- CDU:
-
color Doppler ultrasound guided
- CI:
-
confidence interval
- CR:
-
complete response
- CT:
-
computed tomography
- CTx:
-
chemotherapy
- EBRT:
-
external beam radiotherapy
- GTV:
-
gross tumor volume
- HBRT:
-
high dose rate BRT
- LBRT:
-
low dose rate brachytherapy.
- LR:
-
local recurrence
- m:
-
months
- MM:
-
multiple metastasis
- MRI:
-
magnetic resonance imaging
- OAR:
-
organs at risk
- PD:
-
progressive disease
- PR:
-
partial response
- RR:
-
response rate
- RTOG:
-
Radiation Therapy Oncology Group
- SD:
-
stable disease
- STSs:
-
soft tissue sarcomas
References
Grimer R, Judson I, Peake D, Seddon B. Guidelines for the management of soft tissue sarcomas. Sarcoma. 2010;2010:506182.
Nystrom LM, Reimer NB, Reith JD, Long D, Zlotecki RA, Scarborough MT, et al. Multidisciplinary management of soft tissue sarcoma. ScientificWorldJournal. 2013;2013:852462.
Somaiah N, von Mehren M. New drugs and combinations for the treatment of soft-tissue sarcoma: a review. Cancer Manag Res. 2012;4:397–411.
Prendergast B, Fiveash JB, Gibbs CP, Scarborough MT, Indelicato DJ. Radiotherapy for soft tissue sarcoma of the proximal lower extremity. Sarcoma. 2010;2010:829498.
Strander H, Turesson I, Cavallin-Ståhl E. A systematic overview of radiation therapy effects in soft tissue sarcomas. Acta Oncol. 2003;42:516–31.
Wang JJ, Yuan HS, Li JN, Jiang WJ, Jiang YL, Tian SQ. Interstitial permanent implantation of 125I seeds as salvage therapy for re-recurrent rectal carcinoma. Int J Colorectal Dis. 2009;24:391–9.
Jiang YL, Meng N, Wang JJ, Ran WQ, Yuan HS, Qu A, et al. Percutaneous computed tomography/ultrasonography-guided permanent iodine-125 implantation as salvage therapy for recurrent squamous cell cancers of head and neck. Cancer Biol Ther. 2010;9:959–66.
Lin L, Wang J, Jiang Y, Meng N, Tian S, Yang R, et al. Interstitial 125I seed implantation for cervical lymph node recurrence after multimodal treatment of thoracic esophageal squamous cell carcinoma. Technol Cancer Res Treat. 2014 [Epub ahead of print].
Gao F, Li C, Gu Y, Huang J, Wu P. CT-guided 125I brachytherapy for mediastinal metastatic lymph nodes recurrence from esophageal carcinoma: effectiveness and safety in 16 patients. Eur J Radiol. 2013;82:e70–5.
Merchant TE, Parsh N, del Valle PL, Coffey DH, Galindo CR, Jenkins JJ, et al. Brachytherapy for pediatric soft-tissue sarcoma. Int J Radiat Oncol Biol Phys. 2000;46:427–32.
Janjan N, Crane C, Delclos M, Ballo M. Brachytherapy for locally recurrent soft-tissue sarcoma. Am J Clin Oncol. 2002;25:9–15.
Gemer LS, Trowbridge DR, Neff J, Lin F, Reddy E, Evans RG, et al. Local recurrence of soft tissue sarcoma following brachytherapy. Int J Radiat Oncol Biol Phys. 1991;20:587–92.
Curran Jr WJ, Littman P, Raney RB. Interstitial radiation therapy in the treatment of childhood soft-tissue sarcomas. Int J Radiat Oncol Biol Phys. 1988;14:169–74.
Pearlstone DB, Janjan NA, Feig BW, Yasko AW, Hunt KK, Pollock RE, et al. Re-resection with brachytherapy for locally recurrent soft tissue sarcoma arising in a previously irradiated field. Cancer J Sci Am. 1999;5:26–33.
Fontanesi J, Rao BN, Fleming ID, Bowman LC, Pratt CB, Furman WL, et al. Pediatric brachytherapy. The St. Jude Children’s Research Hospital experience. Cancer. 1994;74:733–9.
Viani GA, Novaes PE, Jacinto AA, Antonelli CB, Pellizzon AC, Saito EY, et al. High-dose-rate brachytherapy for soft tissue sarcoma in children: a single institution experience. Radiat Oncol. 2008;3:9.
Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the international association for the study of pain subcommittee on taxonomy. Pain Suppl. 1986;3:S1-226
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumors: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995;31:1341–6.
Nori D, Schupak K, Shiu MH, Brennan MF. Role of brachytherapy in recurrent extremity sarcoma in patients treated with prior surgery and irradiation. Int J Radiat Oncol Biol Phys. 1991;20:1229–33.
Habrand JL, Gerbaulet A, Pejovic MH, Contesso G, Durand S, Haie C, et al. Twenty years experience of interstitial iridium brachytherapy in the management of soft tissue sarcomas. Int J Radiat Oncol Biol Phys. 1991;20:405–11.
Shiu MH, Turnbull AD, Nori D, Hajdu S, Hilaris B. Control of locally advanced extremity soft tissue sarcomas by function-saving resection and brachytherapy. Cancer. 1984;53:1385–92.
Zhang FJ, Li CX, Zhang L, Wu PH, Jiao DC, Duan GF. Short- to mid-term evaluation of CT guided 125I brachytherapy on intra-hepatic recurrent tumors and/or extra-hepatic metastases after liver transplantation for hepatocellular carcinoma. Cancer Biol Ther. 2009;8:585–90.
Blasko JC, Mate T, Sylvester JE, Grimm PD, Cavanagh W. Brachytherapy for carcinoma of the prostate: techniques, patient selection and clinical outcome. Semin Radiat Oncol. 2002;12:81–94.
Mazeron JJ, Noël G, Simon JM. Head and neck brachytherapy. Semin Radiat Oncol. 2002;12:95–108.
Hentz C, Barrett W. Efficacy and morbidity of temporary (125)I brachytherapy in pediatric rhabdomyosarcomas. Brachytherapy. 2014;13:196–202.
Zhang Y, Guo F, Zhang WL, Huang DS, Hong L, Han T. Clinical application of 125I particle implantation in children with rhabdomysarcoma of the head and neck. Zhongguo Dang Dai Er Ke Za Zhi. 2012;14:437–40.
Li DF, Cui Q, Wang Q, Su H, Zhang WJ, Zhang P. Application of 125I brachytherapy combined artificial joint prosthesis in malignant osteo- and soft tissue sarcoma. Cancer Biother Radiopharm. 2006;21:167–72.
Rivard MJ. Comment on “Dosimetry of interstitial brachytherpy sources: recommendations of the AAPM Radiation Therapy Committee Task Group 43” [Med Phys 22, 209-234(1995)]. American Association of Physicists in Medicine. Med Phys. 1999;26:2514.
Jones D, Washington JT, Christopherson DA. Comments on “Dosimetry of interstitial brachytherapy source: recommendations of the AAPM Radiation Therapy Committee Task Group No. 43” [Med Phys 22, 209-234(1995)]. Med Phys. 1995;22:1349–51.
Acknowledgements
We would like to thank Dr. Suqing Tian and Fuxin Guo for their skillful technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JJW conceived and designed the study; LHY, JNL, and LL contributed to the data collection and performed the statistical analysis; WQR and CL carried out the needle penetration; YLJ and JJW performed seed implantation; LHY and LL carried the dose calculation of seed implantation. All authors read and approved the final version of the manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yao, L., Wang, J., Jiang, Y. et al. Permanent interstitial 125I seed implantation as a salvage therapy for pediatric recurrent or metastatic soft tissue sarcoma after multidisciplinary treatment. World J Surg Onc 13, 335 (2015). https://doi.org/10.1186/s12957-015-0747-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-015-0747-7