Abstract
Background
Heart failure is a worldwide health problem that significantly affects patients’ physical function and health state. The Kansas City Cardiomyopathy Questionnaire (KCCQ) is a disease-specific patient-reported outcome measure commonly used for the assessment of health states of patients with heart failure. This study aimed to evaluate the psychometric properties of the Japanese version of the KCCQ.
Methods
Using pooled data of 141 Japanese patients with chronic heart failure from three clinical trials, the Japanese version of the KCCQ was evaluated for validity and reliability, with a focus on the clinical summary score (CSS) and its component domains. For construct validity, the associations of baseline KCCQ scores with New York Heart Association (NYHA) class and the EuroQol five-dimension, three-level (EQ-5D-3L) scores at baseline were analyzed. For reliability, internal consistency was assessed using Cronbach’s α, and test–retest reliability (reproducibility) was assessed among stable patients. Responsiveness to changes in patients’ clinical status was assessed by analyzing score changes between two timepoints among patients whose health states improved.
Results
Among 141 patients (mean age, 73.7 ± 10.9 years), 76.6% were NYHA class II at baseline. For CSS and its component domains (physical limitations, symptom frequency, and symptom severity), baseline scores were all significantly lower in patients with a higher NYHA class (p < 0.001 for all, Jonckheere-Terpstra test). The physical limitations domain and CSS showed a moderate correlation (Spearman’s ρ = − 0.40 to − 0.54) with three functional status-related EQ-5D dimensions (mobility, self-care, and usual activities). The Cronbach’s standardized α was high (> 0.70) for all KCCQ domain/summary scores. In the test–retest analysis among 58 stable patients, all domain/summary scores minimally changed by 0.3–4.2 points with intraclass correlation coefficients of 0.65–0.84, demonstrating moderate to good reproducibility, except for the symptom stability domain. Among 44 patients with improved health states, all domain/summary scores except for the symptom stability and self-efficacy domains substantially improved from baseline with a medium to large effect size of 0.62–0.88.
Conclusions
The Japanese version of the KCCQ was demonstrated to be a valid and reliable tool for the assessment of symptoms and physical function of Japanese patients with chronic heart failure.
Similar content being viewed by others
Background
Heart failure (HF) is a clinical syndrome caused by a structural and/or functional cardiac abnormality that is characterized by signs and symptoms such as breathlessness, ankle swelling, and fatigue [1]. HF is a public health concern worldwide with a prevalence of 1–4% in most European countries [2], with the prevalence and incidence increasing progressively with age. In the US, the incidence of HF is reported to be 10 per 1000 after 65 years of age [3]. In Japan, the number of patients with HF is expected to increase rapidly with the aging of the population, and the number of patients with left ventricular dysfunction is estimated to reach 1.3 million by 2030 [4].
Although the prognosis of patients with HF has been improved with advances in treatments [5], it has been reported that the mortality and hospitalization rates still remain high [3, 6, 7]. A Japanese study reported that the rehospitalization rates for HF within 1 year after discharge were 23.7–25.7% [8]. Moreover, HF significantly affects physical function and health state of patients [9,10,11]. Thus, the goal of treatment is to improve the overall well-being of patients as well as survival, and the use of patient-reported outcomes (PROs) has been gaining momentum in cardiovascular research [12, 13]. PRO measures are reported by patients and are useful to capture the realities of disease burden and treatment impacts. Disease-specific PRO measures may be more useful than generic instruments because they quantify the health state related to a particular disease and are therefore more sensitive to clinical changes [12].
The Kansas City Cardiomyopathy Questionnaire (KCCQ) [14], originally developed in the English language in 2000, is one such disease-specific PRO measure for HF, which assesses symptoms, physical and social limitations, and health-related quality of life (HRQoL). Having been translated into various languages and validated in many country-specific settings [15,16,17,18,19], the KCCQ is now one of the most widely used PRO measures for patients with HF, along with the Minnesota Living with Heart Failure Questionnaire (MLHFQ) [20]. Among the many existing HF-specific PRO measures, the KCCQ and MLHFQ were the only two measures that fit all eight evaluation criteria (e.g., psychometric properties, feasibility, interpretability, and symptom coverage) in a previous systematic review [21]. One beneficial characteristic of the KCCQ is that it provides a summary score specifically focused on patient symptoms and physical limitations (physical function), along with the overall summary score. Symptoms and physical function are the most relevant domains for the clinical assessment of patients with HF, and these domains are also the main concepts of interest in the development of new HF treatments as they are proximal to patient experience of the disease [22].
A linguistically validated Japanese version of the KCCQ is available and used often in clinical trials involving Japanese HF patients [23,24,25]. However, the psychometric properties of the tool have not yet been evaluated. Therefore, in this study, we evaluated the validity and reliability of the Japanese version of the KCCQ in Japanese patients with chronic HF, with a focus on its domains and summary scores related to symptoms and physical function.
Methods
Sample and design of source trials
Data of Japanese patients with chronic HF were drawn from three phase II trials: the SOCRATES-REDUCED [23], SOCRATES-PRESERVED [24], and ARTS-HF Japan [25].
SOCRATES studies
The SOCRATES-REDUCED and SOCRATES-PRESERVED studies were both multicenter, international, randomized, double-blind, placebo-controlled, dose-finding, phase II trials of vericiguat in patients with chronic HF. Details of the study methods have been previously described [23, 24]. In brief, patients with worsening chronic HF who had either reduced ejection fraction (EF) (EF < 45%, HFrEF) for the SOCRATES-REDUCED or preserved EF (EF ≥45%, HFpEF) for the SOCRATES-PRESERVED were randomized to one of five treatment arms (4 vericiguat and 1 placebo) and received the treatment for 12 weeks.
In the present study, data from the following assessments of patients’ symptoms, functional status, or health state were analyzed: New York Heart Association (NYHA) class [26] recorded at baseline, and the KCCQ and the EuroQol five-dimension, three-level questionnaire (EQ-5D-3L) [27] scores assessed at baseline and at weeks 4, 8, and 12. The present study did not use other clinical data such as biomarkers (e.g., B-type natriuretic peptide [BNP], NT-proBNP), which have low correlation with the patients’ perception of their own health status [28, 29].
ARTS-HF Japan
ARTS-HF Japan was a randomized, double-blind, active-comparator-controlled, dose-finding phase IIb trial of finerenone in Japanese patients with worsening chronic HF with reduced EF (< 40%) and type 2 diabetes mellitus and/or chronic kidney disease. Patients were randomized to one of six treatment arms (5 finerenone and 1 eplerenone) and received the treatment for 90 days. More detailed study methods including inclusion/exclusion criteria have been described previously [25]. Data from the following assessments were used in the present analysis: NYHA class at baseline and the KCCQ and EQ-5D-3L scores at baseline, days 30 and 90, and 30 days after the last day of treatment (follow-up visit).
Clinical and health state measures
NYHA class
NYHA classification is a system to categorize the extent of physical limitations in patients with HF [26]. Physicians classify patients into one of four classes based on their functional limitations and symptom severity: I (no limitations of physical activity); II (slight limitation); III (marked limitation); and IV (unable to carry on any physical activity without discomfort).
KCCQ
The KCCQ is a 23-item (15 questions), self-administered questionnaire quantifying the following clinically relevant domains: physical limitations, symptom frequency, symptom severity, symptom stability, self-efficacy, social limitation, and QoL [14]. The questions refer to the patient’s heart failure symptoms over the past 2 weeks, and each item is scored on a 5- to 7-point Likert scale. A missing value is assigned the average score of the scored items within the domain, and all item scores are summed within each domain. A domain score is transformed to a 0 to 100 scale, with a higher score indicating a better state. Three summary scores are calculated as follows: 1) the total symptom score (TSS)—the average of the symptom frequency and symptom severity domain scores; 2) the clinical summary score (CSS)—the average of the physical limitations domain score and the TSS; and 3) the overall summary score (OSS)—the average of the CSS and the QoL and social limitations domain scores. The symptom stability and self-efficacy domains are not incorporated into any of the KCCQ summary scores [14]. The Japanese version of the KCCQ was translated and linguistically validated by the Mapi Research Institute (Lyon, France).
EQ-5D-3L
The EQ-5D-3L is a generic HRQoL measure, consisting of a five-dimension descriptive system and visual analogue scale (VAS) [27]. In the descriptive system, mobility, self-care, usual activities, pain/discomfort, and anxiety/depression are each rated on a 3-point scale (1 = no problems, 2 = some problems, 3 = extreme problems). A patient’s responses to these five dimensions are then converted into a Japanese value set describing the patient’s overall health state, which ranges from − 0.111 to 1.000 (a higher value indicates a better health state) [30]. The EQ-5D VAS records the patient’s health state on a scale of 0 (worst imaginable) to 100 (best imaginable).
Statistical analyses
Pooled data of Japanese patients with chronic HF from the above-described three trials were analyzed to evaluate the validity and reliability of the Japanese version of the KCCQ. Since symptoms and physical function are more proximal to the patient experience of the disease, our particular focus was on the CSS, a summary scale of symptoms and physical function, and its component domains (i.e., physical limitations, symptom frequency, symptom severity, and TSS). However, every domain and the OSS were also evaluated in this study. Analyses were performed using SAS Release 9.4 (SAS Institute Inc., Cary, NC, USA).
Validity
Construct validity was assessed by the known-group analysis, in which we assessed whether the KCCQ scores could differentiate different groups of patients using the NYHA classes to represent groups of patients with different levels of disease severity. The baseline KCCQ scores were summarized for each NYHA class at baseline. To test an increasing or decreasing trend in scores across NYHA classes, the Jonckheere-Terpstra test [31] was performed.
To further evaluate whether the KCCQ scores measured the constructs of interest, correlations between the baseline scores of the KCCQ and a related but different measure, the EQ-5D-3L, were analyzed using the Pearson’s correlation for the EQ-5D VAS and the Spearman rank correlation for the five EQ-5D dimensions. The physical limitations domain score and CSS were both expected to have a moderate correlation with the three EQ-5D dimensions (i.e., mobility, self-care, and usual activities), which are considered to be related to functional domains. The symptom stability domain assesses the change in symptoms over the past 2 weeks, and the self-efficacy domain assesses knowledge or understanding of how to manage their symptoms. As these two domains assess distinctively different concepts from those evaluated by the EQ-5D dimensions, no meaningful correlation was expected between these domains and the EQ-5D-3L.
Reliability
To assess whether items designed to measure the same construct actually do so, the internal consistency of each KCCQ domain/summary score, except for the symptom stability domain, which is a single-item domain, was assessed using Cronbach’s standardized α. An α of ≥0.7 is considered to indicate good interrelatedness among the items within the domain or summary score [32].
Test-retest reliability, or reproducibility, was assessed by analyzing whether the scores were stable when the patients’ conditions did not change. The test-retest analysis included patients in a stable condition, which was defined as no change in EQ-5D-3L scores between two timepoints [33]: between week 8 and week 12 for the SOCRATES studies and between the last day of treatment and 30 days after the last treatment for the ARTS-HF Japan study. The concordance of the scores at these two timepoints was evaluated using the intraclass correlation coefficient (ICC) [34]. An ICC of ≥0.7 is considered to indicate good agreement [35], i.e., good reproducibility of the scale.
Responsiveness
Responsiveness to patients’ clinical change was evaluated by analyzing whether the KCCQ scores improved when the patients’ health states improved. Patients with improved health states were defined as those with improvement in at least one EQ-5D dimension by ≥1 point without worsening in any EQ-5D dimension [33]. We used the EQ-5D to define those who improved because it was shown to be responsive to clinical changes in patients with HF [36]. Among the patients whose health states were expected to show improvement, changes in the KCCQ scores from baseline to 1 month (more precisely, at week 4 for the SOCRATES studies and at day 30 for the ARTS-HF Japan study) was analyzed by calculating the mean change in scores between the two timepoints and the effect size (mean change in score divided by standard deviation [SD] at baseline). An effect size of 0.2 is interpreted as small, 0.5 as medium, and 0.8 as large [37]. Changes in scores between the two timepoints were also tested using a paired t-test with equal variances assumed.
Results
Patient characteristics
This study used the pooled data of 141 Japanese patients with chronic HF: 30 patients from SOCRATES-REDUCED; 39 patients from SOCRATES-PRESERVED; and 72 patients from ARTS-HF Japan. Although the SOCRATES-PRESERVED contained more female than the other two trials, no noticeable differences were observed for other baseline data such as NYHA class distribution among the three source trials (Additional file 1).
The mean age ± SD of the pooled sample was 73.7 ± 10.9 years, and 71.6% were male (Table 1). Patients with HFrEF accounted for 72.3% of the sample. The majority of patients were classified as NYHA class II (76.6%) at baseline, followed by class III (12.8%), class I (8.5%), and class IV (2.1%). At baseline, all patients responded to all 23 items of the KCCQ (no missing responses). Table 2 summarizes the KCCQ scores at baseline, and Fig. 1 shows the distribution of each domain score and the CSS at baseline. The mean ± SD KCCQ CSS at baseline was 71.6 ± 23.0. As shown in Fig. 1h, the score distribution was negatively skewed (skewness value − 0.75); over 70% of patients had a CSS of ≥60, while 27.7% of patients had a CSS of ≥90.
Distribution of the KCCQ domain scores and clinical summary score at baseline (n = 141a). aN = 127 for (a) physical limitations domain score due to responses coded as missing data in question 1 (6 items), and N = 118 for (f) social limitations domain score due to responses coded as missing data in question 15 (4 items). KCCQ, Kansas City Cardiomyopathy Questionnaire
Validity
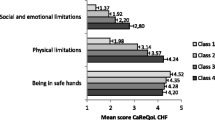
Mean baseline CSSs were lower in patients with higher NYHA classes (91.9 for NYHA class I, 72.2 for class II, 57.4 for class III, and 54.2 for class IV), with a decreasing trend in the scores across NYHA classes (p < 0.001, Jonckheere-Terpstra test) (Fig. 2b & Table 3). A decreasing trend was also observed for all three component domains of the CSS and the other summary scores (p < 0.001 for all; Table 3, Fig. 2), indicating that symptoms or physical function-related domains and all KCCQ summary scores can differentiate patients with different disease severity. As for other domains, the QoL domain scores were significantly lower in patients with higher NYHA classes (p = 0.003), but such a trend was not observed for the symptom stability, self-efficacy, and social limitations domains.
Table 4 summarizes the correlations between the KCCQ and the EQ-5D-3L. The CSS was moderately correlated with the three EQ-5D dimensions (mobility, ρ = − 0.54; self-care, ρ = − 0.41; and usual activities, ρ = − 0.45), as was the physical limitations domain (ρ = − 0.46, − 0.40, and − 0.44, respectively). The correlation coefficient with the EQ-5D VAS, a more general measure of health, was low (r < 0.3) for all the KCCQ scores except for the physical limitations and QoL domains, and the OSS. As expected, the symptom stability and self-efficacy domains had no correlations with any of the EQ-5D dimensions.
Reliability
The Cronbach’s standardized α was high for all KCCQ scores (Table 5), indicating good internal consistency for all domain scores (α = 0.74–0.88) and excellent consistency for all summary scores including the CSS (α = 0.90 for all).
Test-retest reliability, or reproducibility, was analyzed using data of 58 patients who were considered clinically stable between the two timepoints (i.e., weeks 8 and 12 for the SOCRATES studies, and the last day of treatment and 30 days after the last treatment for the ARTS-HF Japan study). The demographic characteristics of these 58 patients were similar to those of the entire pooled sample (mean age ± SD, 74.1 ± 11.6 years; male, 72.4%) (Additional file 2). As shown in Table 6, scores changed only minimally between the two timepoints (by 0.3–4.2 points on a 100-point scale) for all domain/summary scores. Although moderate reproducibility was demonstrated for the QoL (ICC = 0.65), self-efficacy (0.66), symptom severity (0.68), and physical limitations (0.69) domains, the ICCs were high (> 0.7) for all summary scores including the CSS, indicating high reproducibility for these scales. The only exception was the symptom stability domain, which had a low ICC of 0.19.
Responsiveness
Responsiveness of the KCCQ was analyzed using the data of 44 patients who showed improvement in their health state. Changes in the KCCQ scores among these patients are summarized in Table 7. For the three component domains of the CSS, scores significantly increased after 1 month of treatment (p < 0.001 for all, paired t-test), with the greatest increase in the symptom frequency domain score by 26.9 points. The social limitations and QoL domain scores also substantially increased by more than 20 points, but the symptom stability and self-efficacy domain scores did not largely change with a small effect size of < 0.4. All three summary scores including the CSS substantially increased by more than 20 points with a large effect size of > 0.80, demonstrating the substantial responsiveness of the KCCQ to changes in patients’ clinical status.
Discussion
The use of a valid PRO measure is essential for the adequate assessment of patients’ health states. In this study, to assess the psychometric properties of the Japanese version of the KCCQ, we evaluated the validity and reliability of the tool with a focus on the CSS and its component domains, which are considered most relevant for the clinical assessment of patients’ symptoms and physical functioning. The results of this study demonstrated that the Japanese version of the KCCQ had construct validity, good internal consistency, and high reproducibility and responsiveness when used in Japanese patients with chronic HF.
The known-group analysis showed that the three symptoms or physical function-related domain scores (i.e., physical limitations, symptom frequency, and symptom severity) and KCCQ summary scores were all associated with NYHA class, indicating that these scores accurately differentiated patients with differing disease severity. However, the social limitation domain score did not show a decreasing trend with the NYHA class. This result may be due to the disproportionate distribution of patients across NYHA classes (i.e., few patients were in higher NYHA classes III and IV) in this pooled sample. In addition, there was a response option that was coded as missing, which further contributed to the small number of patients with analyzable data in this domain. Although the known-group validity of this domain remains to be confirmed, a moderate correlation of this domain with the EQ-5D usual activity (ρ = − 0.43) partially supports its construct validity. The construct validity of the tool for the assessment of patients’ symptoms and physical functioning was further supported by moderate correlations of the CSS and physical limitations domain with the three EQ-5D dimensions that are related to functional domains. Considering that the EQ-5D-3L is a generic measure and the KCCQ is a HF-specific measure, their scores do not represent an exactly comparable assessment of domains, leading to understandably moderate rather than high correlation.
For reliability, all KCCQ domain/summary scores showed good internal consistency, as demonstrated by a high Cronbach’s α (> 0.7), which indicates that the items constituting the domain or summary scale can be considered to measure the same construct. In particular, the CSS had excellent internal consistency with an α of 0.90, which was almost equivalent to that of its original KCCQ counterpart (α = 0.93 [14]). In the test-retest analysis using clinically stable patients, minimal changes in scores between the two assessments with ICCs of 0.69–0.78 demonstrated the moderate to high reproducibility of the three component domains of the CSS. The CSS and the other two summary scores also had high ICCs of 0.77–0.84, showing good reproducibility of these scales. The mean changes in scores between the two assessments were minimal (by 0.4–4.2 points on a 100-point scale) for other domains as well; however, the ICC of the symptom stability domain was exceptionally low (ICC = 0.19). This was probably because this is a single-item domain, and thus even a one-point change on a 5-point scale in a patient’s response was converted into a substantial score change on a scale of 0 to 100 for the domain score.
One advantage of the KCCQ over the MLHFQ is that the KCCQ is more sensitive to clinical change [14]. Although a comparison with existing tools could not be performed in this study due to secondary use of trial data, our analyses showed that the Japanese version of the KCCQ was highly responsive to patients’ clinical change. All domain scores significantly increased by 17.2–26.9 points after 1 month of treatment in patients with improved health states, except for the symptom stability and self-efficacy domains. In particular, the symptom frequency domain and all summary scores, including the CSS, showed especially high responsiveness with a large effect size (> 0.80). However, the responsiveness of the symptom stability and self-efficacy domains, neither of which are incorporated into any of the KCCQ summary scores, could not be confirmed in this analysis. As they are conceptually different from other domains, their responsiveness may need to be evaluated in a more appropriate method.
In the development study of the original KCCQ, the baseline CSS was significantly lower in patients who subsequently died or required rehospitalization than in event-free survivors (35.1 vs. 55.3, p < 0.001), suggesting the prognostic value of the tool [14]. Unfortunately, we were unable to assess the prognostic value of the Japanese version of the KCCQ in this study owing to certain methodological limitations, such as a small number of patients with few numbers of prognostic events, which may be due to a short observation period and a disproportionately large proportion of patients with less severe symptoms (85.1% were classed as NYHA class I–II at baseline), as well as confounding by treatment effects (e.g., patients received different treatments according to their treatment group). The prognostic value of the Japanese version of the KCCQ would be worthy of further investigation.
PRO measures have been historically underused as metrics in clinical studies [12]. However, in light of the increased focus on improving the overall well-being of patients, they are encouraged to be used as endpoints in cardiovascular studies [13], and selected KCCQ domains are increasingly being used as such in heart failure trials. The KCCQ not only assesses all three principal components of patients’ health states, i.e., symptoms, functional status, and HRQoL, but can also be an independent predictor of poor prognosis [38] and future healthcare costs [39]. In addition, because the KCCQ is available in many languages, its use as a metric in clinical studies would enable international comparison of the health states of patients with HF. Furthermore, the KCCQ may also help to enhance patient care by directly informing clinicians of the patients’ disease burden and treatment impacts when used in clinical setting. Continued exploration of the usefulness of the KCCQ in clinical practice is warranted in future studies.
This study has several limitations. First, because this study involved the secondary use of three trials’ data and analyzed a pooled sample, the generalizability of the results of this study may be limited by the inclusion/exclusion criteria of the source trials. For example, as the majority of patients (76.6%) were classed as NYHA class II at baseline, our results may not be applicable to patients with more severe symptoms. Second, construct validity was assessed using only NYHA class and the EQ-5D-3L because of the limited measures available in the secondary use of trial data. For the symptoms and physical function-related scales of the KCCQ, assessment of correlations with measures with more similar constructs (e.g., MLHFQ) and measures that assess related functional domains (e.g., 6-min walk test) would have been useful. Moreover, construct validity of other domains, especially the self-efficacy and social limitations domains, require further evaluation using a more related, appropriate reference measures for each domain. Third, the reliability and validity of the single-item, symptom stability domain could not be confirmed in the present analysis. This item is inherently different from the other KCCQ items because it asks the patient to rate the degree of change in their symptoms over the past 2 weeks. Therefore, it was not expected to perform similarly to the other items and domain scores that do not require a comparison of current and previous experiences. Further assessment of this domain is warranted. However, the present analysis confirmed the reliability and validity of the CSS, the most relevant KCCQ summary score for clinical assessment. Thus, we believe that our results would provide valuable information for users of the Japanese version of the KCCQ. Lastly, although we defined patients’ symptom stability and changes in clinical status using the EQ-5D-3L, which has been reported to be responsive to clinical changes in patients with HF [36], they may not have been adequately captured by the EQ-5D-3L. The EQ-5D-3L may be responsive to only relatively large changes, thereby limiting the analysis sample for the assessment of responsiveness, which may have contributed somewhat to the better responsiveness of the KCCQ. Likewise, although we observed robust stability estimated in the test–retest analysis, the analysis may have included some patients who had clinical changes.
Conclusions
This study showed that the Japanese version of the KCCQ, especially its scales related to symptoms and physical functioning, is a valid and reliable measure, with construct validity, good internal consistency, and high reproducibility and responsiveness. Further evaluation of the psychometric properties of some domains as well as its prognostic value is warranted in Japanese patients with HF.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- HF:
-
Heart failure
- EF:
-
Ejection fraction
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduced ejection fraction
- PRO:
-
Patient-reported outcome
- KCCQ:
-
The Kansas City Cardiomyopathy Questionnaire
- HRQoL:
-
Health-related quality of life
- NYHA:
-
New York Heart Association
- EQ-5D-3L:
-
EuroQol, five-dimension, three-level
- TSS:
-
Total symptom score
- CSS:
-
Clinical summary score
- VAS:
-
Visual analogue scale
- ICC:
-
Intraclass correlation coefficient
- SD:
-
Standard deviation
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200.
Seferovic PM, Stoerk S, Filippatos G, Mareev V, Kavoliuniene A, Ristic AD, et al. Organization of heart failure management in European Society of Cardiology member countries: survey of the heart failure Association of the European Society of cardiology in collaboration with the heart failure National Societies/working groups. Eur J Heart Fail. 2013;15:947–59.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–360.
Okura Y, Ramadan MM, Ohno Y, Mitsuma W, Tanaka K, Ito M, et al. Impending epidemic: future projection of heart failure in Japan to the year 2055. Circ J. 2008;72:489–91.
Ushigome R, Sakata Y, Nochioka K, Miyata S, Miura M, Tadaki S, et al. Temporal trends in clinical characteristics, management and prognosis of patients with symptomatic heart failure in Japan—report from the CHART studies. Circ J. 2015;79:2396–407.
Gerber Y, Weston SA, Redfield MM, Chamberlain AM, Manemann SM, Jiang R, et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med. 2015;175:996–1004.
Crespo-Leiro MG, Anker SD, Maggioni AP, Coats AJ, Filippatos G, Ruschitzka F, et al. European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur J Heart Fail. 2016;18:613–25.
Jtsuchihashi-Makaya M, Hamaguchi S, Kinugawa S, Yokota T, Goto D, Yokoshiki H, et al. Characteristics and outcomes of hospitalized patients with heart failure and reduced vs preserved ejection fraction. Report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J. 2009;73:1893–900.
Calvert MJ, Freemantle N, Cleland JG. The impact of chronic heart failure on health-related quality of life data acquired in the baseline phase of the CARE-HF study. Eur J Heart Fail. 2005;7:243–51.
Juenger J, Schellberg D, Kraemer S, Haunstetter A, Zugck C, Herzog W, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart. 2002;87:235–41.
Hobbs FD, Kenkre JE, Roalfe AK, Davis RC, Hare R, Davies MK. Impact of heart failure and left ventricular systolic dysfunction on quality of life: a cross-sectional study comparing common chronic cardiac and medical disorders and a representative adult population. Eur Heart J. 2002;23:1867–76.
Rumsfeld JS, Alexander KP, Goff DC Jr, Graham MM, Ho PM, Masoudi FA, et al. Cardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart Association. Circulation. 2013;127:2233–49.
Anker SD, Agewall S, Borggrefe M, Calvert M, Jaime Caro J, Cowie MR, et al. The importance of patient-reported outcomes: a call for their comprehensive integration in cardiovascular clinical trials. Eur Heart J. 2014;35:2001–9.
Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City cardiomyopathy questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35:1245–55.
Miani D, Rozbowsky P, Gregori D, Pilotto L, Albanese MC, Fresco C, et al. The Kansas City cardiomyopathy questionnaire: Italian translation and validation. Ital Heart J. 2003;4:620–6.
Faller H, Steinbüchel T, Schowalter M, Spertus JA, Störk S, Angermann CE, et al. The Kansas City cardiomyopathy questionnaire (KCCQ)—a new disease-specific quality of life measure for patients with chronic heart failure. Psychother Psychosom Med Psychol. 2005;55:200–8 German.
Patel H, Ekman I, Spertus JA, Wasserman SM, Persson LO. Psychometric properties of a Swedish version of the Kansas City cardiomyopathy questionnaire in a chronic heart failure population. Eur J Cardiovasc Nurs. 2008;7:214–21.
Nave-Leal E, Pais-Ribeiro J, Oliveira MM, Da Silva N, Soares R, Fragata J, et al. Psychometric properties of the portuguese version of the Kansas City cardiomyopathy questionnaire in dilated cardiomyopathy with congestive heart failure. Rev Port Cardiol. 2010;29:353–72 English, Portuguese.
Comín-Colet J, Garin O, Lupón J, Manito N, Crespo-Leiro MG, Gómez-Bueno M, et al. Validation of the Spanish version of the Kansas city cardiomyopathy questionnaire. Rev Esp Cardiol. 2011;64:51–8. English. Spanish. .
Rector TS, Cohn JN. Assessment of patient outcome with the Minnesota living with heart failure questionnaire: reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. Pimobendan Multicenter research group. Am Heart J. 1992;124:1017–25.
Kelkar AA, Spertus J, Pang P, Pierson RF, Cody RJ, Pina IL, et al. Utility of patient-reported outcome instruments in heart failure. JACC Heart Fail. 2016;4:165–75.
U.S. Food & Drug Administration. Clinical Outcome Assessments (COA) Qualification Submissions. https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/clinical-outcome-assessments-coa-qualification-submissions. Accessed 18 February 2020.
Gheorghiade M, Greene SJ, Butler J, Filippatos G, Lam CS, Maggioni AP, et al. Effect of vericiguat, a soluble guanylate cyclase stimulator, on natriuretic peptide levels in patients with worsening chronic heart failure and reduced ejection fraction: the SOCRATES-REDUCED randomized trial. Jama. 2015;314:2251–62.
Pieske B, Maggioni AP, Lam CSP, Pieske-Kraigher E, Filippatos G, Butler J, et al. Vericiguat in patients with worsening chronic heart failure and preserved ejection fraction: results of the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED EF (SOCRATES-PRESERVED) study. Eur Heart J. 2017;38:1119–27.
Sato N, Ajioka M, Yamada T, Kato M, Myoishi M, Yamada T, et al. A randomized controlled study of finerenone vs. eplerenone in Japanese patients with worsening chronic heart failure and diabetes and/or chronic kidney disease. Circ J. 2016;80:1113–22.
The Criteria Committee of the New York Heart Association. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9th ed. Boston: Little, Brown & Co; 1994.
EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
Luther SA, McCullough PA, Havranek EP, Rumsfeld JS, Jones PG, Heidenreich PA, et al. The relationship between B-type natriuretic peptide and health status in patients with heart failure. J Card Fail. 2005;11:414–21.
Spertus J, Peterson E, Conard MW, Heidenreich PA, Krumholz HM, Jones P, et al. Monitoring clinical changes in patients with heart failure: a comparison of methods. Am Heart J. 2005;150:707–15.
Tsuchiya A, Ikeda S, Ikegami N, Nishimura S, Sakai I, Fukuda T, et al. Estimating an EQ-5D population value set: the case of Japan. Health Econ. 2002;11:341–53.
Jonckheere AR. A distribution-free k-sample test against ordered alternatives. Biometrika. 1954;41:133–45.
Nunnally JC, Bernstein IR. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994.
Devlin N, Parkin D, Browne J. Using the EQ-5D as a performance measurement tool in the NHS (09/03). London, UK: Department of Economics, City University London; 2009.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–8.
Haywood KL, Garratt AM, Dziedzic K, Dawes PT. Generic measures of health-related quality of life in ankylosing spondylitis: reliability, validity and responsiveness. Rheumatology. 2002;41:1380–7.
Eurich DT, Johnson JA, Reid KJ, Spertus JA. Assessing responsiveness of generic and specific health related quality of life measures in heart failure. Health Qual Life Outcomes. 2006;4:89.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.
Heidenreich PA, Spertus JA, Jones PG, Weintraub WS, Rumsfeld JS, Rathore SS, et al. Health status identifies heart failure outpatients at risk for hospitalization or death. J Am Coll Cardiol. 2006;47:752–6.
Chan PS, Soto G, Jones PG, Nallamothu BK, Zhang Z, Weintraub WS, et al. Patient health status and costs in heart failure: insights from the eplerenone post-acute myocardial infarction heart failure efficacy and survival study (EPHESUS). Circulation. 2009;119:398–407.
Acknowledgments
Not applicable.
Funding
This study was supported by Bayer Yakuhin, Ltd.
Author information
Authors and Affiliations
Contributions
EF set up this study and contributed to the protocol development. HO and CG contributed to the statistical methodology and data interpretation. LB contributed to the protocol development and statistical methodology. LR contributed to the statistical methodology. TT conducted data analysis. YH drafted the manuscript. BP substantially contributed to the revision of the manuscript. All authors reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the NPO Clinical Research Promotion Network Japan. This was a retrospective, observational study with the secondary use of trial data, and thus it involved no patient recruitment.
Consent for publication
Not applicable.
Competing interests
EF is an employee of Bayer Yakuhin, Ltd. HO has received advisory fee from Bayer Yakuhin, Ltd. LB and LR are employees of Bayer AG. TT and YH are employees of Clinical Study Support, Inc. CG has received consulting fees from Bayer AG, Bayer HealthCare Pharmaceuticals, and Bayer Yakuhin, Ltd. BP has received research funds from Bayer Healthcare, Servier, and Astra-Zeneca, as well as speakers honoraria/committee membership fees from Novartis, Bayer Healthcare, Daiichi-Sankyo, MSD, Stealth Peptides, Astra-Zeneca, Sanofi, Vifor, and Servier.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Baseline characteristics and KCCQ scores of patients in each source trial. Patient characteristics and baseline KCCQ scores are summarized by each trial.
Additional file 2
Baseline characteristics of patients who were clinically stable between the two timepoints. Patient characteristics (n = 58) are summarily analyzed for test-retest reliability.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Watanabe-Fujinuma, E., Origasa, H., Bamber, L. et al. Psychometric properties of the Japanese version of the Kansas City Cardiomyopathy Questionnaire in Japanese patients with chronic heart failure. Health Qual Life Outcomes 18, 236 (2020). https://doi.org/10.1186/s12955-020-01483-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-020-01483-0