Abstract
Background
Functional dependence is highly prevalent in maintenance hemodialysis (MHD) settings. Also, poor health-related quality of life (HRQoL) and high levels of depressive symptoms have been reported by MHD patients. We investigated associations between functional status and mental aspects of quality of life in Brazilian MHD patients.
Methods
Cross sectional study of 235 patients enrolled in two of the four participating MHD clinics of the Prospective Study of the Prognosis of Chronic Hemodialysis Patients (PROHEMO) in Salvador, BA, Brazil. Data were collected from September 2016 to August 2017. The Katz’s questionnaire was used for basic activities of daily living (ADL) and the Lawton-Brody’s questionnaire for instrumental activities of daily living (IADL). ADL and IADL scores were combined to create 3 functional status groups: highly dependent (n = 47), moderately dependent (n = 109) and independent (n = 82). The validated Brazilian version of the Kidney Disease Quality of Life Short Form (KDQOL-SF) was used for scores of two distinct HRQoL measures, i.e., the mental component summary (MCS) and the 5-item mental health inventory (MHI-5). We used linear regression to estimate differences in scores with adjustment for possible confounders: months of dialysis, age, gender, other sociodemographic variables, body mass index, type of vascular access, dialysis dose by Kt/V, laboratory variables (albumin, blood hemoglobin, calcium, phosphorus, urea, creatinine and parathyroid hormone) and nine comorbid conditions.
Results
Mean age was 51.2 ± 12.4 yr (median age = 51.0 yr), 59.1% were male, 93.2% were non-White. The prevalence of self-reported functional status differed by age: 54.4% for age < 45 yr, 67.8% for age 45–60 yr and 73.9% for age ≥ 60 yr. Using functionally independent as reference, lower scores were observed for highly dependent patients in MCS (difference: -4.69, 95% CI: -8.09, -0.29) and MHI-5 (difference: -5.97, 95% CI: -8.09, -1.29) patients. These differences changed slightly with extensive adjustments for covariates.
Conclusions
Our results call attention to a high prevalence of functional dependence in younger and older MHD patients. The results suggest that the lower self-reported mental quality of life in functionally dependent MHD patients cannot be explained by differences in age and comorbidities.
Similar content being viewed by others
Background
Functional status is related to the individual’s ability to perform basic activities of daily living (ADL) and self-care instrumental activities of daily living (IADL) [1, 2]. ADL includes daily activities, such as eating, dressing, bathing, using the toilet and moving from one position to another. IADL includes more complex and refined activities that most people learn during their teenage years or early adulthood, such as grocery shopping, meal preparation and household chores. Reduction in functional status will lead patients to rely on others to perform their ADLs and IADLs.
Functional dependence is a problem expected to arise at an elder age, but may become apparent earlier in the lives of patients with chronic disease, as is the case of chronic kidney disease, including end-stage renal disease (ESRD) patients undergoing maintenance hemodialysis (MHD) [3,4,5,6,7]. Data from the Dialysis Outcomes and Practice Patterns Study (DOPPS), for example, show a high prevalence of functional dependence among younger and older ESRD patients undergoing MHD in the United States, Canada, European countries, Japan, New Zealand and Australia [7]. A high prevalence of comorbid conditions is also observed in MHD patients, particularly among those who report functional dependence [8, 9]. ESRD patients undergoing MHD also report, in general, poor health-related quality of life (HRQoL) and high levels of depressive symptoms [10, 11]. Moreover, there are data to indicate that functional status is an independent predictor of mortality in MHD patients [7, 12]. Studies are needed to investigate associations between self-reported functional status and psychological well-being in MHD patients and possible influences of potential confounders, such as, age and comorbidities in the association.
The main objectives of the present study in patients undergoing MHD in a large Brazilian city was to estimate the prevalence of functional dependence and investigate associations of functional status with mental aspects of quality of life. We assessed possible influences of age, and comorbidities in the comparisons of the HRQoL measures between patients with different levels of functional status.
Methods
Study design and sample
The study was a cross-sectional analysis of data of the Prospective Study of the Prognosis of Chronic Hemodialysis Patients (PROHEMO) [13,14,15], developed at satellite dialysis units in the city of Salvador (Bahia), Brazil. This Northeastern Brazilian town has a population of approximately three million people, 80% of which are Black or Mixed-race [16].
Data collection was initiated in 2016 when the questionnaires for functional status started to be applied to PROHEMO participants. The analysis was restricted to two (here identified as Clinic A and Clinic B) of the original four participating dialysis clinics of PROHEMO [14]. Approximately 19% of the patients were undergoing hemodialysis for less than 1 year, 50% for less than 4 years and 80% for less than 8 years at the time of data collection. In Clinic A, all 211 adult patients undergoing treatment from September 2016 to May 2017 were invited to participate. Among the 191 patients who agreed to participate, 179 were interviewed and 12 were not able to respond to the questionnaires because of cognitive impairment. In Clinic B, 70 patients were randomly selected from a population of 311 adult patients undergoing treatment in June 2017. Among 70 patients in Clinic B, 64 were interviewed from July 2017 to August 2017, four did not agree to participate and two were not able to respond to the questionnaires because of cognitive impairment.
From the sample of 243 patients, 235 (173 from Clinic A and 62 from Clinic B) had data for both functional status and HRQoL measures. These 235 patients constitute the sample of the present analysis. The Institutional Review Board of the Medical School of the Federal University of Bahia approved the research protocol of the present study and all patients provided informed consent to participate.
Data collection and definitions
The collection of demographic, laboratory and clinical data began as soon as the patients provided informed consent to participate. The data were provided by the patient and supplemented with information from the attending nephrologist or extracted from medical records. The patient was classified by race as White or non-White by pre-defined criteria [17]. To determine economic class (A - E) we used the classification system of the Brazilian Institute of Market Research which is primarily based on possession of consumer goods [18]. We classified patients belonging to classes D and E as poor or very poor. We used the laboratory results closest to the collection of baseline clinical data and patient’s self-reported data on functional status and HRQoL. Blood samples for laboratory tests were collected before the dialysis session.
Predictors and outcomes
The predictor variable was functional status. The outcome variables were the scores of the mental component summary (MCS) and the mental health inventory (MHI-5). We used the ADL Katz’s questionnaire [19] and the IADL Lawton-Brody’s questionnaire [20, 21] to assess functional status. Katz’s questionnaire assesses the level of ability of the patient to perform 5 ADL tasks (Table 1). Interviewers asked patients if they were able to perform the following tasks, without assistance: eating, getting dressed, bathing, using the toilet and/or transferring from bed to chair. The options of responses for each ADL item were “yes” or “no”. The Lawton-Brody’s questionnaire was used to evaluate ability to 8 IADL tasks (Table 1). Patients were asked to choose the best answer to describe their ability to perform each of the following activities: using a telephone, getting places beyond walking distance, grocery shopping, preparing meals, doing housework or handyman work, doing laundry, taking medication or managing money. The options of responses for each IADL item were “need no help,” “need some help,” or “unable to do at all”. For the ADL, a “yes” response was scored as 1 and a “no” response was scored as 0.25 considering that was not possible to distinguish if the patient performed the task with some help or if he or she was unable to perform the task at all. For the IADL responses, “need no help” were scored 1; “need some help,” scored 0.5; and “unable to do at all” scored 0. Adequate to high internal consistency has been demonstrated earlier for the Katz’s ADL [22, 23] and the Lawton-Brody’s IADL instruments [20, 21]. In the present study, the Cronbach’s alpha for the 5 ADL questions was 0.94 and for the 8 items of the Lawton-Brody questions was 0.87.
The ADL and IADL scales were combined to create an expanded functional status scale. This approach was used to provide a more comprehensive evaluation of the functional status of the patients and it is supported by research on the psychometric properties [24,25,26]. The results of an analysis of a nationally representative survey of 25,470 adults using Guttman and item response theory scaling methods indicated that the expanded ADL/IADL scale was less biased by age and more useful than the ADL to assess functional status in individuals of different ages [24]. The predictive validity of the expanded scale for health outcomes was demonstrated in the international DOPPS that showed a strong association of greater functional dependence with mortality, dialysis therapy withdrawal, and hospitalization [7].
We determined the overall functional status score by summing up the scores of the 13 items of the expanded functional status scale. The functional status scores could range from 1.25 to 13. To define the categories of functional status, we took into account the classification described in the 2016 DOPPS publication, which was based on logistic regression proportional odds model [7]. In DOPPS the functional status score was categorized into four groups: < 8, 8 - < 11, 11 - < 13, and 13. Similar to DOPPS, patients with overall score of 13 were defined as functionally independent and corresponded to those who reported no need for assistance to execute all 13 functional status tasks. The range of scores used to define the moderately dependent group (score range: ≥11 - < 13) were also the same used in DOPPS. Because the percentage of patients with overall score < 8 was small (4%), we combined the groups with scores 8- < 11 and < 8 into a single category (< 11) to define the highly dependent group.
We used the validated Brazilian version of the Kidney Disease Quality of Life Short Form (KDQOL-SF) [27] to assess aspects of the mental dimension of quality of life. The KDQOL-SF is comprised of kidney disease-targeted items and generic items from the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) [28]. The patient responses to the questions from the generic core of KDQOL-SF were used to calculate MCS and MHI-5 scores. MCS scores were calculated by using the scoring algorithm proposed by Ware et al., which takes into account factor score coefficients for the all SF-36 domains [29]. According to the proposed algorithm for the MCS score, the coefficients are negative for physical functioning, role-physical, bodily pain and general health. The positive coefficients for MCS scores are those for vitality, social functioning, role-emotion and mental health (emotional well-being). The scores of each generic measure used for the MCS may vary from 0 to 100. However, because of the weighting used, the range of the MCS score is expected to be narrower than the ranges of the SF-36 scales used to determine the MCS score. In the present study the minimum MCS score was 18.9 and the maximum MCS score was 70.1. Higher MCS scores represent better HRQoL.
To determine scores of the MHI-5, interviewers asked patients to indicate how much of their time over the previous 4 weeks they had felt “so down in the dumps that nothing could cheer you up,” “downhearted and blue,” “very nervous,” “calm and peaceful,” and “a happy person.” Possible responses to these five questions were “All of the time,” “Most of the time,” “A good bit of the time,” “Some of the time,” “A little of the time,” or “None of the time”. The scores of the MHI-5 may range from 0 to 100. The minimum and maximum values of the MHI-5 were 8.0 and 100, respectively. Similar to the MCS score, higher MHI-5 scores also represent better HRQoL. The recommended cutoff of 52 for MHI-5 was used to categorize the patients into two groups with scores ≤52 representing worse mental quality of life [30].
Statistical methods
We used mean ± standard deviation to describe characteristics consistent with normal distribution and median [interquartile range] to describe variables that were not consistent with a normal distribution. Percentages were used to describe frequencies of categorical attributes. A standardized effect size measure was used to assess the magnitude of the difference in scores. The effect size measure was determined by using as numerator the mean difference in scores between the two groups and as denominator the pooled standard deviation of the scores [31]. A value ≤0.20 was interpreted as small effect size, 0.50 as moderate effect size and ≥ 0.80 as large effect size.
Logistic regression and linear regression models were used to estimate associations with adjustment for potential effects of covariates. The inclusion of covariates in the multivariable models was based on characteristics shown to be associated with functional status [7, 12] and poor HRQoL in hemodialysis patients [10], independent of p value or statistical significance [32, 33]. The linear and logistic regression models had similar structures regarding the inclusion of covariates: Adjusted-1 model included months on dialysis and age; Adjusted-2 model included months on dialysis, age, and the other sociodemographic variables, i.e., sex, race, marital status (married vs not married), education (<high school vs ≥ high school), living status (living with family vs not living with family), economic class (poor/very poor vs higher level); Adjusted-3 model included all covariates listed in Table 2, except hypertension that was omitted because of collinearity. Economic class was the only covariate with missing values. Missing value for this covariate was present for 6 of the 235 patients (2.6%). To handle missing data, we performed multiple imputation with 20 repetitions using logistic regression with economic class as the outcome variable (code as 1 for poor or very poor and 0 for higher levels) and the set of sociodemographic variables shown in Table 2 as the independent variables. A sensitivity analysis with the 229 patients with complete data was also performed for comparison of the results. We used 95% confidence interval (95% CI) to describe the precision of the estimates. The STATA version 15.1 for Mac was used for the statistical analysis.
Results
Our sample consisted of 235 MHD patients with a mean age of 51.2 ± 12.4 yr (median age = 51.0 yr), 59% were male and 93% were non-White. The distribution of patient’s characteristics did not differ markedly between Clinic A and Clinic B. The most common cause of ESRD was hypertensive nephropathy (26%), followed by diabetic nephropathy (25%) and glomerulonephritis (18%).
The distribution of ADL and IADL scores in the study sample of 235 patients is displayed in Table 1. The patients reported more often to be able to perform ADL than IADL tasks without help. Less than half (47%) of the patients reported to be able to shop for grocery without help. Approximately 40% of the patients needed some help or were unable to go to places beyond walking distance or to do housework/handyman work.
Table 2 describes patient characteristics by the three functional status groups. There were 44 patients in the highly dependent group (18.7%), 109 in the moderately independent group (46.4%) and 82 in the functionally independent group (34.9%). Compared to functionally independent patients, those reporting functional dependence had a higher mean age, lower concentrations of parathyroid hormone (PTH) and serum creatinine, higher proportion of hemodialysis by catheter and higher prevalence of comorbidities (except hypertension).
Table 3 shows unadjusted and adjusted associations of selected characteristics with the prevalence of self-reported moderate to greater functional dependence as compared to functional independence. The prevalence of self-reported functional dependence was 54.4% for age < 45 yr, 67.8% for age 45 to 60 yr and 73.9% for age ≥ 60 yr. The strength of the association between age and functional status was reduced with adjustments for comorbidities and laboratory variables. The prevalence of functional dependence was higher for diabetics (85%) than for non-diabetics (56.6%) and for patients undergoing dialysis by catheter (77.6%) than by arteriovenous fistulae (61.8%). The strength of the associations between functional status with both diabetes and dialysis by catheter were not reduced with adjustments for covariates. Higher prevalence of self-reported functional dependence was also observed for patients with serum PTH < 150 pg/mL (89.2% for PTH < 150 pg/mL vs 40.9% for PTH > 300 pg/mL) and for patients with serum creatinine ≤9 mg/dL (81.3% for creatinine ≤9 mg/dL vs 54.9% for creatinine > 9 mg/dL). The associations of low serum PTH and creatinine concentrations with higher likelihood of functional dependence were observed both in models with minimal and extensive adjustments for covariates.
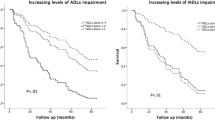
Table 4 shows the results from the regression analysis of the association between functional status and scores of HRQoL measures (MCS and MHI-5). Compared with functionally independent, the MCS score was lower by approximately 5 points for the moderately dependent (difference: -4.56, 95% CI: -8.30, -1.60; effect size: 0.42). Similar difference in MCS score was observed in the comparison between highly dependent and functionally independent (difference: -4.65, 95% CI: -9.00, -0.31; effect size: 0.39). The differences in MCS scores by functional status changed slightly with adjustments for months on dialysis, treatment variables, laboratory exams and comorbid conditions.
Compared with the MCS scores, a steadier reduction in the MHI-5 scores from the functionally independent to the highly dependent groups was observed (Table 4). Using functionally independent as reference, it was observed that the MHI-5 score was lower by approximately 7 points for the moderately dependent (difference: -7.42, 95% CI: -13.6, -1.21; effect size: 0.35) and by almost 14 points for the highly dependent (difference: -13.8, 95% CI: -21.8, -5.88; effect size: 0.63). As observed for MCS, the differences in the MHI-5 by functional status did not change markedly with extensive adjustments for covariates.
Similar results of the association between functional status with MCS and MHI-5 were observed in a sensitivity analysis restricted to a sample of 229 patients without missing data. Similar results were also observed using the complete sample of 235 patients with indicator variables, instead of imputation, to account for missing data on economic class. These results are not shown in the Table.
In an analysis using data of the whole sample, the MCS scores stratified for the age groups < 45 yr, 45–60 yr and > 60 yr were, respectively, 47.0 ± 12.2, 51.9 ± 9.82 and 50.5 ± 12.1. The corresponding MHI-5 scores by these age categories were 70.7 ± 24.4, 77.7 ± 19.8 and 77.6 ± 21.4. In linear models with extensive adjustments for the covariates listed in Table 2 and with age < 45 yr as reference the MCS score was higher by approximately 6.4 points for age 45–60 yr (difference: 6.4, 95% CI: 2.3, 10.4) and 3.9 points for age > 60 yr (difference: 3.9, 95% CI: -0.4, 8.3). For MHI-5, the score was higher by approximately 8.6 points for age 45–60 yr (difference: 8.6, 95% CI: 1.2, 16.1) and 6 points for ages > 60 yr (difference: 6.0, 95% CI: -2.1, 14.0). These results are not shown in the Table.
The prevalence of MHI-5 ≤ 52 was 8.5% (7/82) for functionally independent, 20.2% (22/109) for moderately dependent and 25% (11/44) for highly dependent patients. The prevalence of MHI-5 ≤ 52 points was approximately 2.5 times higher (prevalence ratio 2.53, 95% CI: 1.17, 5.46) in patients who reported any degree of functional dependence than in those functionally independent. The results of the multivariate logistic regression show that the direction of the association between functional status and MHI-5 ≤ 52 did not change and the strength of association was not reduced with extensive adjustments for covariates. These results are not shown in Table 4.
We also evaluated the data to estimate differences in MCS and MHI-5 scores by ADL (5 versus lower score) and the IADL tasks (need help versus not need help). In the comparisons between ADL task groups, larger difference was observed for MHI-5 (70.7 ± 22.8 for ADL score < 5 and 75.6 ± 22.0 for ADL score = 5, effect size: 0.22), than for MCS (48.4 ± 13.0 for ADL score < 5 and 49.8 ± 11.5 for ADL score = 5, effect size: 0.11). In the comparisons between IADL task groups, larger differences were also observed for MHI-5 than for MCS. For the task “go to places beyond walking distance”, the MCS score were 47.8 ± 12.4 in patients who need help and 51.0 ± 10.7 in patients who did not need help, with effect size of 0.28. The MHI-5 scores between patients who need and do not need help for the task “walking distance” were, respectively, 69.2 ± 23.1 and 79.6 ± 20.3, with effect size of 0.48. For the task “be able to shop for grocery,” the MCS score were 47.9 ± 11.5 in patients who need help and 51.8 ± 11.3 in patients who did not need help, with effect size of 0.34. The MHI-5 scores between patients who need and do not need help for the task “shop for groceries” were, respectively, 71.3 ± 21.7 and 79.9 ± 21.6, with effect size of 0.40. For the task “doing housework or handyman work”, the MCS score were 47.4 ± 11.9 in patients who need help and 51.2 ± 11.1 in patients who did not need help, with effect size of 0.33. The MHI-5 scores between patients who need help and those who do not need help for the task “housework/handyman work” were, respectively, 69.9 ± 22.5 and 78.8 ± 21.1, with effect size of 0.41. The results of the comparisons of MCS and MHI-5 scores by ADL and IADL tasks are not shown in the Table.
Discussion
This study shows a very high prevalence of patient-reported functional dependence in a sample of Brazilian ESRD patients undergoing MHD; more than half of the participants reported functional dependence. In general, the patients reported more difficulty in performing IADL than ADL tasks. The prevalence of self-reported functional dependence in MHD patients observed in our study was similar to that reported in a DOPPS analysis of MHD patients treated in 12 countries [7] and, apparently, was much higher than in prior reports for older adults in the general population [34]. The results indicate that self-reported functional status is strongly associated with poorer mental quality of life in MHD patients. The average MCS and MHI-5 scores were much lower for patients who reported to be moderately or highly functionally dependent than the functionally independent patients. In the comparisons using the overall functional status scores, the reduction in the scores of the mental components of quality of life from the functionally independent (overall score 13) to the highly dependent group (overall score < 11) was more remarkable for MHI-5 than for MCS, following a monotonic pattern. The larger differences in the MHI-5 than in the MCS scores were also observed both for the comparisons between ADL task groups and between IADL task groups.
Functionally dependent MHD patients were, in general, older and presented higher prevalence of comorbidities. However, the associations between functional status and the mental components of quality of life were not attenuated after adjustment for age and preexisting comorbidities. This finding may be explained, at least partially, by effects of age on functional status and the mental components of quality of life. Whereas the prevalence of self-reported functional dependence was higher for the older patients, the scores of MCS and MHI-5 was higher for the older than for the younger patients. Similar results on the associations between age and HRQoL scores in MHD patients were observed in the international DOPPS. In a sample of 9526 MHD patients enrolled in DOPPS, it was observed that, differently from the Physical Component Summary (PCS), older age was not associated with lower MCS score [10]. Moreover, no association was seen between age and depression symptoms, assessed by the Center for Epidemiological Studies Depression Index (CES-D), in another DOPPS investigation [11]. These findings are consistent with the claim that patient experiences, expectations and perceptions regarding health could influence their HRQoL, independent of age and health status [35, 36].
Patients who referred to be functionally dependent were more often undergoing hemodialysis by catheter and had lower serum concentrations of creatinine and PTH. The higher prevalence of hemodialysis by central venous catheter (compared with arteriovenous fistulae) in functionally dependent patients is consistent with previous observations [37, 38]. It has been suggested that if the patient has a poor functional status or limited life expectancy, the placement of an arteriovenous fistulae may be postponed until after the start of hemodialysis [38].
The association of low PTH and low serum creatinine with higher likelihood of functional dependence in the present study could not be explained by effects of age and comorbidities. Prior evidence suggests that lower concentration of PTH observed in patients referring functional dependence might be due to adynamic bone disease, a prevalent cause of pain and bone fractures in MHD patients [39]. The lower serum creatinine in patients reporting functional dependence is consistent with possible role of reduced muscle mass and poor nutritional status in the functional status of MHD patients [40,41,42]. These findings may suggest an influence of protein energy wasting and inflammation in sicker MHD patients [43].
While the present study offers insights into the association between functional status and the mental quality of life of MHD patients, methodological limitations cannot be ignored. Because the study is cross-sectional, causal inference cannot be reached and directional ambiguity in the association is possible. Although a stronger monotonic association of functional status with MHI-5 than with MCS scores was observed, it is not possible to conclude that the MHI-5 scale is more sensitive than the MCS scale to changes in the functional status of MHD patients considering that cross-sectional differences in HRQoL score may not equate to longitudinal changes [36]. Our results suggest poor mental quality of life in MHD patients who report functional dependence, but they do not permit to identify what disorder, such as, depressive symptoms and anxiety play a major role in the association of functional status with MCS and MHI-5. Another limitation is to determine if the differences in HRQoL scores are clinically significant considering that it depends on several factors, including the criteria to define what constitute clinically important difference in scores, the patient’s perspective, and if the HRQoL was assessed using data collected at single time point in a cross-sectional study or using repeated measures in an observational cohort study or in a randomized clinical trial [44,45,46]. Differences of at least 3–5 points in the SF-36 scales have been proposed as a clinically relevant or minimum clinically important difference (MCID) [47, 48]. However, this proposal for the use of mean difference to define clinical relevance has been criticized and the use of a standardized effect size measures has been favored by some experts [49, 50]. Samsa et al. advocate a threshold of 0.20 in standardized effect size as clinically relevant [50]. The observed differences in the scores of MCS and MHI-5 between functional status categories in the present study exceeded the threshold proposed for MCID, both for mean difference and effect size, but we should be cautious to conclude that the observed differences are relevant in the context of clinical practice considering the observational, cross-sectional, design of the study.
Generalizability of findings from the present study to other hemodialysis populations have to be pondered, due to unique cultural and demographic characteristics of our study population, composed of more than 90% non-White (mostly of African descent) participants. Additionally, the mean age (< 60 yr) in our study sample is lower than that of studies with MHD patients developed outside Brazil, especially in developed countries.
Conclusions
This study calls attention to a very high prevalence of self-reported functional dependence in younger and older MHD patients. The results suggest that functionally dependent patients have poorer mental quality of life than functionally independent patients. According to the results, the poorer mental quality of life associated with functional dependence cannot be explained by age and the presence of prevalent comorbid conditions in MHD patients.
Availability of data and materials
Data is deposited in the repository of the Federal University of Bahia, Salvador, BA, Brazil.
Abbreviations
- ADL:
-
Activities of daily living
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CES-D:
-
Center for Epidemiological Studies Depression Index
- DOPPS:
-
Dialysis Outcomes and Practice Patterns Study
- ESRD:
-
End-stage renal disease
- HIV/AIDS:
-
Human immunodeficiency virus/Acquired immune deficiency syndrome
- HRQoL:
-
Health-related quality of life
- IADL:
-
Instrumental activities of daily living
- IQR:
-
Interquartile range
- KDQOL-SF:
-
Kidney Disease Quality of Life Short Form
- MCID:
-
Minimum clinically important difference
- MCS:
-
Mental component summary
- MHD:
-
Maintenance Hemodialysis
- MHI-5:
-
5-Item Mental health inventory
- PCS:
-
Physical Component Summary
- PROHEMO:
-
Prospective Study of the Prognosis of Chronic Hemodialysis Patients
- PTH:
-
Parathyroid hormone
References
Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31:721–7.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86.
Fuchs Z, Blumstein T, Novikov I, Walter-Ginzburg A, Lyanders M, Gindin J, Habot B, Modan B. Morbidity, comorbidity, and their association with disability among community-dwelling oldest-old in Israel. J Gerontol A Biol Sci Med Sci. 1998;53:M447–55.
Bowling CB, Sawyer P, Campbell RC, Ahmed A, Allman RM. Impact of chronic kidney disease on activities of daily living in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2011;66:689–94.
Bostrom G, Conradsson M, Rosendahl E, Nordstrom P, Gustafson Y, Littbrand H. Functional capacity and dependency in transfer and dressing are associated with depressive symptoms in older people. Clin Interv Aging. 2014;9:249–56.
Kuvalekar K, Kamath R, Ashok L, Shetty B, Mayya S, Chandrasekaran V. Quality of life among persons with physical disability in Udupi Taluk: a cross sectional study. J Family Med Prim Care. 2015;4:69–73.
Jassal SV, Karaboyas A, Comment LA, Bieber BA, Morgenstern H, Sen A, Gillespie BW, De Sequera P, Marshall MR, Fukuhara S, et al. Functional dependence and mortality in the international Dialysis outcomes and practice patterns study (DOPPS). Am J Kidney Dis. 2016;67:283–92.
Shaheen FA, Al Wakeel J, Al-Ghamdi SM, Alhelal B, AlGhareeb S, Al Obaidli AA, AlSalmi I, Abdulaziz HE, Bieber BA, Pisoni RL. Cardiovascular and cerebrovascular comorbidities in hemodialysis patients from the Gulf cooperation council countries enrolled in the dialysis outcome and practice pattern study phase 5 (2012-2015). Saudi J Kidney Dis Transpl. 2016;27:S24–30.
Miskulin D, Bragg-Gresham J, Gillespie BW, Tentori F, Pisoni RL, Tighiouart H, Levey AS, Port FK. Key comorbid conditions that are predictive of survival among hemodialysis patients. Clin J Am Soc Nephrol. 2009;4:1818–26.
Lopes AA, Bragg-Gresham JL, Goodkin DA, Fukuhara S, Mapes DL, Young EW, Gillespie BW, Akizawa T, Greenwood RN, Andreucci VE, et al. Factors associated with health-related quality of life among hemodialysis patients in the DOPPS. Qual Life Res. 2007;16:545–57.
Lopes AA, Albert JM, Young EW, Satayathum S, Pisoni RL, Andreucci VE, Mapes DL, Mason NA, Fukuhara S, Wikstrom B, et al. Screening for depression in hemodialysis patients: associations with diagnosis, treatment, and outcomes in the DOPPS. Kidney Int. 2004;66:2047–53.
Cook WL, Jassal SV. Functional dependencies among the elderly on hemodialysis. Kidney Int. 2008;73:1289–95.
Lopes GB, Silva LF, Pinto GB, Catto LF, Martins MT, Dutra MM, Lopes AA. Patient's response to a simple question on recovery after hemodialysis session strongly associated with scores of comprehensive tools for quality of life and depression symptoms. Qual Life Res. 2014;23:2247–56.
Lopes GB, Matos CM, Leite EB, Martins MT, Martins MS, Silva LF, Robinson BM, Port FK, James SA, Lopes AA. Depression as a potential explanation for gender differences in health-related quality of life among patients on maintenance hemodialysis. Nephron Clin Pract. 2010;115:c35–40.
Lopes GB, Nogueira FC, de Souza MR, Penalva MA, de Amorim JL, Pisoni RL, Robinson BM, Lopes AA. Assessment of the psychological burden associated with pruritus in hemodialysis patients using the kidney disease quality of life short form. Qual Life Res. 2012;21:603–12.
Brazilian Institute of Geography and Statistics - 2010 Census. https://cidades.ibge.gov.br/brasil/ba/salvador/pesquisa/23/22107. Accessed 22 July 2019.
Krieger H, Morton NE, Mi MP, Azevedo E, Freire-Maia A, Yasuda N. Racial admixture in North-Eastern Brazil. Ann Hum Genet. 1965;29:113–25.
Standard Criterion of Economic Classes, Brazil 2010. http://www.aba.com.br/wp-content/uploads/content/7727632a373615b34f2a5726fcc5c9e2.pdf. Accessed 19 Dec 2017.
Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10:20–30.
Hassani Mehraban A, Soltanmohamadi Y, Akbarfahimi M, Taghizadeh G. Validity and reliability of the persian version of Lawton instrumental activities of daily living scale in patients with dementia. Med J Islam Repub Iran. 2014;28:25.
Mystakidou K, Parpa E, Tsilika E, Panagiotou I, Roumeliotou A, Symeonidi M, Galanos A, Kouvaris I. Evaluation of instrumental activities of daily living in Greek patients with advanced cancer. Int J Rehabil Res. 2013;36:75–80.
Ferretti-Rebustini RE, Balbinotti MA, Jacob-Filho W, Rebustini F, Suemoto CK, Pasqualucci CA, Farfel JM, Leite RE, Grinberg LT, Nitrini R. Validity of the Katz index to assess activities of daily living by informants in neuropathological studies. Rev Esc Enferm USP. 2015;49:946–52.
Lino VT, Pereira SR, Camacho LA, Ribeiro Filho ST. Buksman S: [cross-cultural adaptation of the Independence in activities of daily living index (Katz index)]. Cad Saude Publica. 2008;24:103–12.
LaPlante MP. The classic measure of disability in activities of daily living is biased by age but an expanded IADL/ADL measure is not. J Gerontol B Psychol Sci Soc Sci. 2010;65:720–32.
Spector WD, Fleishman JA. Combining activities of daily living with instrumental activities of daily living to measure functional disability. J Gerontol B Psychol Sci Soc Sci. 1998;53:S46–57.
Laan W, Zuithoff NP, Drubbel I, Bleijenberg N, Numans ME, de Wit NJ, Schuurmans MJ. Validity and reliability of the Katz-15 scale to measure unfavorable health outcomes in community-dwelling older people. J Nutr Health Aging. 2014;18:848–54.
Duarte PS, Ciconelli RM, Sesso R. Cultural adaptation and validation of the “kidney disease and quality of life--short form (KDQOL-SF 1.3)” in Brazil. Braz J Med Biol Res. 2005;38:261–70.
Hays RD, Kallich JD, Mapes DL, Coons SJ, Carter WB. Development of the kidney disease quality of life (KDQOL) instrument. Qual Life Res. 1994;3:329–38.
Ware JE, Kosinski M, Keller SD. SF-36 physical and mental health summary scales: a User's manual. Boston: New England Medical Center- The Health Institute; 1994.
van den Beukel TO, Siegert CE, van Dijk S, Ter Wee PM, Dekker FW, Honig A. Comparison of the SF-36 five-item mental health inventory and Beck depression inventory for the screening of depressive symptoms in chronic dialysis patients. Nephrol Dial Transplant. 2012;27:4453–7.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum Assoc.: Hillsdale; 1988.
Dales LG, Ury HK. An improper use of statistical significance testing in studying covariables. Int J Epidemiol. 1978;7:373–5.
Greenland S, Neutra R. Control of confounding in the assessment of medical technology. Int J Epidemiol. 1980;9:361–7.
Lin SF, Beck AN, Finch BK, Hummer RA, Masters RK. Trends in US older adult disability: exploring age, period, and cohort effects. Am J Public Health. 2012;102:2157–63.
Testa MA, Simonson DC. Assesment of quality-of-life outcomes. N Engl J Med. 1996;334:835–40.
Crosby RD, Kolotkin RL, Williams GR. Defining clinically meaningful change in health-related quality of life. J Clin Epidemiol. 2003;56:395–407.
Shah S, Leonard AC, Thakar CV. Functional status, pre-dialysis health and clinical outcomes among elderly dialysis patients. BMC Nephrol. 2018;19:100.
Allon M. Vascular access for Hemodialysis patients: new data should guide decision making. Clin J Am Soc Nephrol. 2019;14:954–61.
Leinau L, Murphy TE, Bradley E, Fried T. Relationship between conditions addressed by hemodialysis guidelines and non-ESRD-specific conditions affecting quality of life. Clin J Am Soc Nephrol. 2009;4:572–8.
Patel SS, Molnar MZ, Tayek JA, Ix JH, Noori N, Benner D, Heymsfield S, Kopple JD, Kovesdy CP, Kalantar-Zadeh K. Serum creatinine as a marker of muscle mass in chronic kidney disease: results of a cross-sectional study and review of literature. J Cachexia Sarcopenia Muscle. 2013;4:19–29.
Avram MM, Bonomini LV, Sreedhara R, Mittman N. Predictive value of nutritional markers (albumin, creatinine, cholesterol, and hematocrit) for patients on dialysis for up to 30 years. Am J Kidney Dis. 1996;28:910–7.
Johansen KL, Shubert T, Doyle J, Soher B, Sakkas GK, Kent-Braun JA. Muscle atrophy in patients receiving hemodialysis: effects on muscle strength, muscle quality, and physical function. Kidney Int. 2003;63:291–7.
Kalantar-Zadeh K, Ikizler TA, Block G, Avram MM, Kopple JD. Malnutrition-inflammation complex syndrome in dialysis patients: causes and consequences. Am J Kidney Dis. 2003;42:864–81.
Bottomley A, Pe M, Sloan J, Basch E, Bonnetain F, Calvert M, Campbell A, Cleeland C, Cocks K, Collette L, et al. Analysing data from patient-reported outcome and quality of life endpoints for cancer clinical trials: a start in setting international standards. Lancet Oncol. 2016;17:e510–4.
Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific quality of life questionnaire. J Clin Epidemiol. 1994;47:81–7.
Temple L, Fuzesi S, Patil S. The importance of determining quality of life in clinical trials. Surgery. 2009;145:622–6.
Stewart AL, Greenfield S, Hays RD, Wells K, Rogers WH, Berry SD, McGlynn EA, Ware JE Jr. Functional status and well-being of patients with chronic conditions. Results from the medical outcomes study. JAMA. 1989;262:907–13.
Strand V, Boers M, Idzerda L, Kirwan JR, Kvien TK, Tugwell PS, Dougados M. It's good to feel better but it's better to feel good and even better to feel good as soon as possible for as long as possible. Response criteria and the importance of change at OMERACT 10. J Rheumatol. 2011;38:1720–7.
Wyrwich KW, Tierney WM, Babu AN, Kroenke K, Wolinsky FD. A comparison of clinically important differences in health-related quality of life for patients with chronic lung disease, asthma, or heart disease. Health Serv Res. 2005;40:577–91.
Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D. Determining clinically important differences in health status measures: a general approach with illustration to the health utilities index mark II. Pharmacoeconomics. 1999;15:141–55.
Acknowledgements
We are grateful for the support received from the medical directors and staff of the following dialysis units: CLINIRIM and Clínica NEPHRON of Barris.
Funding
Brazilian National Council for Scientific and Technological Development (CNPq)”, grant #486138/2013-5, from 2014-2017.
Author information
Authors and Affiliations
Contributions
Gabriel Brayan Gutiérrez Peredo: Research concept and design; analysis and interpretation of data; acquisition of data, drafting of manuscript; administrative and technical support. Marcia Tereza Silva Martins: Drafting of manuscript; acquisition of data and administrative and material support. Fernanda Albuquerque da Silva: Drafting of manuscript; acquisition of data; administrative, technical and material support. Marcelo Barreto Lopes: Drafting of manuscript; analysis and interpretation of data; statistical and epidemiological expertise; technical support. Gildete Barreto Lopes: Analysis and interpretation of data, drafting of manuscript supervision, data management, administrative and technical support. Antonio Alberto Lopes: Research concept and design; drafting of manuscript; analysis and interpretation of data; statistical and epidemiological expertise; supervision; administrative, technical and material support. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Comitê de Ética do Hospital Universitário Professor Edgard Santos, Salvador, BA, Brazil.
Certificate of Presentation for Ethical Consideration (CAAE): 38839014.0.0000.0049
Number of the Process: 1.104.632
Consent for publication
Not Applicable.
Competing interests
None to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gutiérrez-Peredo, G.B., Martins, M.T.S., da Silva, F.A. et al. Functional dependence and the mental dimension of quality of life in Hemodialysis patients: the PROHEMO study. Health Qual Life Outcomes 18, 234 (2020). https://doi.org/10.1186/s12955-020-01464-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-020-01464-3