Abstract
Abstract
Current available therapies control Myasthenia gravis (MG) reasonably well, but Health Related Quality of life (HRQOL) remains lower than expected. The aim was provide insights in how HRQOL in MG stands across borders and time, compare the scores to general population controls and other chronic disorders and assess the impact of potential predictors for quality of life such as a) clinical characteristics b) antibodies c) thymoma and d) treatment in a population-based cohort.
Methods
We designed a population-based cross-sectional study including 858 patients, 373 from Norway and 485 from the Netherlands. The Short Form Health Survey 36 (SF-36) and a cross-cultural validated questionnaire were used. Data were in addition compared to the general population, other chronic diseases and previous studies.
Results
Mean physical composite score was 59.4 and mental composite score 69.0 with no differences between the countries. The mean HRQOL score was lower in patients with bulbar and generalized symptoms (p < 0.001) compared to sex and age adjusted healthy controls, but not in patients with ocular symptoms or patients in remission. Multivariate analysis revealed that female gender, generalized symptoms and use of secondary immunosuppressive drugs at the time of testing were risk factors for reduced HRQOL.
Conclusions
Remission and absence of generalized symptoms were favorable factors for HRQOL in MG patients. Historically, the HRQOL levels have not changed since 2001 and no new clinical predictors could be detected in this exhaustive population-based study. Further studies should explore the impact of non clinical factors like ethnic variations, socio-economic and hormonal factors on HRQOL.
Similar content being viewed by others
Background
Myasthenia gravis (MG) is a heterogeneous neuromuscular autoimmune disease. Clinically, the symptoms range from mild ocular symptoms to severe generalized muscle weakness and disability. In the most severe cases the respiratory muscles are affected, causing problems breathing, a so-called “myasthenic crisis”. Nowadays, with optimal treatment, mortality is rare and most patients live normal lives. Nevertheless, health related quality of life (HRQOL) remains reduced compared to healthy controls in several studies (Table 1) [1–10].
These studies show that the disease has an extensive impact on physical, psychological and social wellbeing: the more severe muscle symptoms and disability, the lower the physical components of the outcome [1, 2, 7–10]. There are contradictory results as to what extend the mental wellbeing is affected in MG. Reported predictors for reduced HRQOL are among others use of prednisolone and side-effects, disease severity, depression, anxiety and disease duration, however, many others are also mentioned (Table 1). There are few larger studies and the impact of clinical subgroups based on antibodies, age of onset, thymus histology and clinical presentation remains unanswered [11–13].
Chronic immunomodulation with corticosteroid, other immunosuppressive drugs and thymectomy are often necessary to control the disease. Immunosuppressive medication produce marked improvement, however in many cases does the improvement not persist if treatment is discontinued. Consequently, treatment in MG is often a lifelong proces [14]. The choice of treatment depends on the severity of the symptoms, the specific subgroups and the pace of progression [14]. It is reported that MuSK MG and Thymoma MG are more likely to require secondary immunosuppressives than AChR MG and that elderly are more prone to side-effects [14–17]. As more advanced immunotherapy becomes available for MG patients, it is relevant to use HRQOL as an outcome for choice of treatment strategies. Long-term follow-up studies of representative MG cohorts assessing change of HRQOL during the last decades are lacking.
Up-to-date, there is no study reflecting the HRQOL of population-based MG cohorts covering the whole spectre of disease activity and immunological markers. Based on previous studies we hypothesized that serological subgroups, thymoma, disease course and treatment strategy are factors affecting HRQOL in MG patients. Our aim was to examine these factors and HRQOL in a MG cohort as large as possible, by combining population-based MG cohorts from two countries. We also compared the HRQOL outcomes of the MG patients to healthy controls, previous studies and other chronic diseases in order to get an impression of the burden of the disease.
Methods
The design was cross sectional including two large population based MG cohorts from the entire Norway and a contigous province of South-Holland and North-Holland in The Netherlands (Fig. 1). In order to increase the sample size of MuSK MG in the serological subgroup analysis, we included a national population based sample (n = 34) from a prevalence study in the Netherlands [18].
Overview over study procedure. The study was conducted among all MG patients in Norway and the contiguous regions of South- and North Holland in the Netherlands, including an additional MuSK Sample from entire Netherlands. The case identification and inclusion criteria were the same in both countries. The case search in the Norwegian study area was performed nationwide including 4 university clinics, 15 local clinics and 11 private clinics. Recruitment started: 01.01.2008. Recruitment stopped: 01.11.2009. The case search in the Dutch study was conducted in two regions and the affiliation to the geographical area was defined by postal code. The area had 4 university clinics, 25 local clinics and one private clinic. Recruitment started: 01.10.2011. Recruitment stopped: 01.01.2012. 43 patients were not eligible for questionnaire study because of change of address, dementia and other co-morbidities and delay in registration of ICD-code. Abbreviations: ICD = international classification diagnosis. F: M = female: male ratio
Study procedure
The details of the study are reported in a previous study [19, 20]. The patients were mailed a self-administered validated questionnaire including the Short Form-36 (SF-36) and questions about disease severity and current treatment for the last three months [21]. Reminders were sent to non-responders twice and missing data was completed by phone or mail.
Clinical characteristics, disease onset and course, presence of antibodies and thymus histology were collected from medical records.
Definitions
Disease course was grouped into remission; either complete stable or pharmocological, ocular, bulbar or generalized symptoms at the time of testing. We subgrouped the ocular symptoms in those who started ocular and remained ocular throughout disease course (Ocular MG) and those who had residual ocular symptoms after generalized disease in the MG subgroup analysis. Non-steroid immunosuppresive medicines included azathioprine, cyclosporine, mycophenolate mofetil, tacrolimus, rituximab and cyclophosphamide.
Instruments
The Norwegian and Dutch translations of SF-36 (version 1) was used to assess HRQOL [22, 23] in the past four weeks. This instrument is constructed for population surveys, is short and easy and has good psychometric qualities.
The SF-36 consist of 36 questions, organized into eight domains. The eight domains are physical functioning (PF), Role physical (problems with work or daily acitivites as a results of physical health, RP), Bodily pain (BP), general health evaluation (GH), Vitality (VT), Social functioning (SF), Role emotional (RE; severe problems with work or daily acitivites as a result of emotional health) and mental health (MH). All items are coded, scaled and transformed linearly from 0 (worst health) to 100 (best health). The first four can be summarized into a physical composite score (PCS; PF, RP, BP, GH) and the last four into a mental summary score (MCS; VT, SF, RE, MH).
Control groups
We compared the two cohorts with published normative data, including reference data for chronic diseases (15 different conditions) and two population-based studies of Multiple sclerosis and Parkinsons disease [22, 24–26].
Regulatory and ethical issues
We obtained informed constent from all participants and approval of the regional ethical committee of South-Norway, the ethical review committee of the Leiden University Medical Center (LUMC), The Netherlands, and the Medical Review Ethics Committee (METC) of South-West Holland.
Statistical analysis
The statistical analysis was done using SPSS 22.0 (statistical package for social sciences, IBM, Armonk, NY, USA) and STATA 14 (StatCorp, Texas, USA). Scoring and calculation of the SF-36 scores were done according to the improved methods of Ware, McHorney and Sherbourne for version 1 [27, 28]. Method for impute missing data was followed for 0.7 % of the data. The MG patients were analyzed by domains and composite scores. Since the composite scores are considered as the most robust outcome measurement for the SF-36, we have focused on them in our comparisons. Differences in continuous variables were tested by independent sample t-tests and chi-square tests for contingency tables for categorical variables. When at least 25 % of expected cell frequencies were less than 5, Fischer’s exact test was applied. P < 0.05 was considered significant. Adjustment for the confounding effect of age, gender, disease severity and differences between both countries’ samples was done using linear regression analysis and stratum-specific estimates. We used the population-based cohort for all analysis (n = 837) either stratified by gender or country or pooled all together. For the immunological subgroup analysis, we included the responders of a national sample of MuSK MG patients (n = 21), leaving in total 856 MG patients for the analysis since the information about antibodies of eight patients was missing.
To examine the relationship between PCS/MCS and the significant covariates we used multiple regression analysis (p < 0.05) Afterwards, the model was employed on the MG subgroups with regard to antibodies to identify if the predictors played the same role in the subgroups.
Results
858 MG patients (72 %) of the 1189 MG patients responded with a slightly higher response rate in Norway (76.2 %) than in the Netherlands (68.7 %). There was no difference considering age, sex, age onset, antibody profile and clinical remission rate between responders and non-responders of the questionnaire. The Dutch national sample of MuSK MG comprised more females (p = 0.011), but was otherwise similar to the Dutch regional MuSK MG cohort. No significant differences were found in the composite scores of HRQOL, and only minor differences in the subdomains (Table 2).
Comparison to healthy controls (Fig. 2)
HRQOL in Myasthenia Gravis compared with healthy controls. The figure illustrates the population based MG cohorts in Netherlands (a) and the Norway (b) compared with healthy controls from their own countries. Healthy control data is provided by Loge et al.; Norway [24] and Aaronesen et al. [22]. In summary, MG patients scored lower than healthy controls and females scored lower than males and those in remission similar to healthy controls. The Score range from 0-100. Higher score indicate better Health related quality of life (HRQOL). Solid line is score of reference population for men, and dotted line is score of reference population for women in their respective countries. Horizontal axes show the 8 domains of SF-36 and composite scores
The total cohort of MG patients had lower scores than healthy controls (p-value <0.005, adjusted for age and gender), except for the domains of bodily pain (BP) and problems with daily activities due to mental health problems (RE). Female MG patients systematically scored lower than male MG patients, with significant p-values <0.001 on all domains and composite scores (Additional file 1: Table e-1).
Patients in remission (MGFA class 0) (n = 196, 23.4 % of the cohort) and those with ocular symptoms (MGFA class 1) (n = 102, 12.2 %) scored similar or better than their national normative controls on composite scores. For both groups, the HRQOL of the domains were similar to controls, except for the domain of general health (GH), were the score was significantly worse in male MG patients in both the Netherlands as in Norway.
MCS in particular showed age-dependent divergent results (Additional file 1: Table e-1). In the Netherlands, the MCS was lower for those below 60 years of age; 50 % of the females and 31 % of the males compared to controls. In contrast, the elderly MG patients from 70 years of age had reduced MCS in Norway compared to controls, representing 16.3 % of the females and 46 % of the males.
HRQOL in MG subgroups (Table 3, Fig. 3)
Despite different disease course and more immuno-suppressives in MuSK MG and Thymoma MG, there were no differences in HRQOL. No differences were observed between early and late onset MG groups (adjusted for age). Patients with generalized and bulbar symptoms had lower HRQOL scores compared to those with OMG, residual ocular symptoms after generalized disease and those in remission (p < 0.001). No difference could be detected between those with OMG and those with residual ocular symptoms after generalized disease. No difference in PCS or MCS could be detected when stratifying the cohort into those early MG (0-3 years after onset) and longer follow-up (>3 years after onset).
HRQOL and treatment
Current treatment with non-steroid immunosuppressive drugs affected PCS negatively independent of disease activity (p-value <0.05 when adjusted for age, sex and disease activity). Prednisolone alone did not lower the PCS, but did so in combination with other immunosuppressive medicines (p = 0.002) . Thymectomy did not affect HRQOL, regardless of the histology results, thymoma, atrophy or hyperplasia.
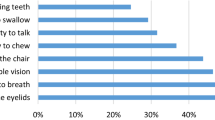
Correlations between SF 36 composite scores and clinical variables
We used a multiple regression model with the PCS and MCS as outcome variables and gender, current disease symptoms and use of immunosuppresiva in general (prednisolon included) as possible predictors. Fourty-nine percent of the variance within Physical HRQOL were explained by these markers. Together the muscular weakness explained 44.2 % of the variance. Dyspnoe and muscular weakness in the legs were the strongest predictors (Table 4) compared to those without symptoms. The use of immunosuppressive drugs and gender were minor contributors each explaining around 4 %, p = 0 < 0.001.
The same variables only explained 26 % of the Mental HRQOL in MG patients. Together dyspnoe and muscular weakness in legs, arms and neck contributed with 35.3 % of the variance. Gender was a minor marker, explaining around 5 %, and secondary immunosuppressivedrugs was not a significant risk factors for decreased mental health (Table 5).
When applying the model on the different antibody subgroups, the model fit better for physical than for mental HRQOL and in particular better for MuSK MG and Thymoma MG (Tables 4 and 5).
Comparison to other chronic diseases (Fig. 4)
We compared a stratified sample of Norwegian MG patients with symptoms in their early disease phase (0-3 years after onset) with patients with Norwegian Multiple sclerosis, Parkinson’s disease and Swedisch Rheumatoid Arthritis of similar disease duration and mean age. MG patients scored similar than MS patients and higher than Parkinson patients and Rheumatoid Arthritis patients (tested by t-test).
Discussion
In this population-based double cohort study, we report a reduced self-perceived HRQOL in Myasthenia Gravis patients with bulbar and generalized symptoms, while patients in remission, those with OMG and those with residual symptoms after generalized disease scored similar to healthy controls. Generalized disease course, gender, and treatment with secondary immunosuppressives were risk factors for decreased HRQOL. Having a distinct subgroup with an antibody marker, thymoma or early or late onset subtype did not influence the HRQOL outcome.
The reduced quality of life was determined by lowered physical capacities, but psychological wellbeing was affected in roughly half of the patients as well. There was no differences in HRQOL between MG patients in Norway and the Netherlands. Pooling the data could therefore be done without affecting the validity of the results and confirms the reliability of the results. Put into an historical context, the HRQOL has not changed much for MG patients over the last 10-15 years and we found the same levels as reported in 2001 [2, 5–10] (Fig. 5). The reduced results of Padua et al. [1] may be explained by a low percentage in clinical remission and many patients with generalized symptoms compared to our cohort. The result of “the more generalized disease or active” disease, the poorer HRQOL” is in accordance with other reports [1, 3, 7, 8, 29]. Leonardi et al. [4] reported that patients in remission scored similar to Italian general population, supporting our findings from the Dutch and Norwegian MG patients. We did not find any harmful impact of antibodies or thymectomy in accordance with other studies [1, 8, 30]. Our findings of normal levels of HRQOL in ocular MG is supported by another study of 91 ocular Italian MG patients [11]. In contrast, a Japanese study reported QOL impairment of 123 ocular MG patients in those who not responded to therapy [13]. One explanation of these contradictory results may be patients selection, since ocular MG includes several symptoms (ptosis, diplopia, complete ophthalmoplegia), with potentially different grades of disability. Additionnally, the use of another questionnaire and cultural factors may account for the difference.
Overview over HRQOL measured by SF-36 from 2001-2012. Studies providing norm-based scoring are shown. Bars illustrate the distribution of MGFA score within the cohorts, lines illustrate the PCS and MCS. Vertical axis shows SF-36 score 0-100 for lines and distribution of MGFA class within the cohort. Padua et al. reported lower scores in 2002 than we did (p < 0.001), however the cohort consisted of fewer patients in remission (7 %) and 89 % in MGFA class II-IV [1]. Paul et al. 2001 [2], provided not norm-based scoring, but PCS 57.6 (27) and 65.5 (24.8) were not significant different from our study
In addition to generalized weakness, dyspnoe and dysphagia, female gender, usage of secondary immunosuppressives were minor risk factors to reduced HRQOL, similarly to results form previous studies [9, 30, 31]. Some of the gender variability could be explained by a general gender effect as the pattern is similar as seen in the normal population [22, 24]. However, we know that hormonal factors affect the symptoms [32, 33] and could thus also contribute. The second finding may suggest that long term immunosuppressive therapy may not be as harmless as assumed. This is supported by a HRQOL study from Japan, which documented an impact of steroids and calcineurin inhibitors in two studies [30, 31]. The negative effects may be related to side-effects or to the burden of constant need of medication. As reviewed by Sanders [14], the initial goal of therapy should be reducing weakness as much and as quickly as possible. Balancing side effects of immunotherapeutic agents and treatment effect remains a challenge for the clinician. The correlation between secondary immunosupressive agents and reduction of HRQOL in MG patients indicates that it is important to keep in mind the benefits of usage contra the side effects, and aim at reducing dosage to lowest possible maintenance dose. This may in particular be important for ocular MG in which no RCT has yet documented effect of any secondary immunosuppressive treatment, neither on symptoms remission nor on prevention of generalized disease [34, 35].
Early MG scored similar to early MS, however when looking at longer follow- up reports HRQOL turns worse in MS [36]. The explanation is probably because MS and Parkinsons’ disease have often a more progressive course with no or less treatment that stops progression. Rheumatoid arthritis, on the other hand, is associated with more pain and disability than MG which can explain the marked lower scores. Improvement of HRQOL scores are reported in RA within the same patients, but also improvement over the last decades [37, 38]. According to Grob et al.’s lifetime study of MG, the distribution, severity and course of disease is determined within the first two years [39] and many MG patients experience the worst phase of the disease in these years. One should therefore expect improvement in HRQOL with longer disease duration. Our study design was cross-sectional and limits therefore interpretation of HRQOL over time in the same patient. Hence, follow-up studies both of individuals over time are needed to learn more about HRQOL in MG. With better treatment strategies and therapautic options we do also expect improvement over the last decade, however the comparison with earlier studies did not confirm this. Limitations in these inter-study comparisons are that the patients are not matched in the study and many variables are not controlled, therefore the results are purely indicative.
The main strength of the study is the design, which is a true population-based, cross sectional survey of two well defined groups. Finding the same levels of HRQOL in both countries makes the results more reliable. All clinical subtypes of MG were present in sufficient numbers to give useful results. Disease specific questionnaires have been advocated for MG, and indeed may enable a more specific follow-up for the patients [40]. Our intention was, however, to use a broadly validated questionnaire to provide insights in how HRQOL in MG stands across borders and time, compare the scores to general population controls and other chronic disorders. Correlations between the SF-36 and MG disease status has been proven in several studies, and may thus be trusted to give a fair picture of the burden of MG disease. A more disease specific instrument would be able to detect smaller changes in vision, speaking, chewing and swallowing better [1, 4–6], which was not the purpose in this study. Since the SF-36 has norm-based scoring, group level results of this study can be used to compare MG patients across countries and further improve the quality of health care systems in places where it is not optimal.
Conclusion
Taken together, this population based study of 857 MG patients found the same HRQOL levels as in 2001 [2], indicating no improvement in quality of life for MG patients despite more available immunotherapy choices and better diagnostics of MG subgroups. Although we included a large sample and patients with different clinical characteristics, we could not find any new clinical predictors for reduced HRQOL compared to the other studies. Therefore we suggest that the impact of non-clinical factors like job, socio-economic factors, physical activity and hormonal factors on HRQOL in MG patients should be explored in order to improve the quality of life in MG patients.
References
Padua L, Evoli A, Aprile I, Caliandro P, D'Amico P, Rabini A, et al. Quality of life in patients with myasthenia gravis. Muscle Nerve. 2002;25:466–7.
Paul RH, Nash JM, Cohen RA, Gilchrist JM, Goldstein JM. Quality of life and well-being of patients with myasthenia gravis. Muscle Nerve. 2001;24:512–6.
Raggi A, Leonardi M, Antozzi C, Confalonieri P, Maggi L, Cornelio F, et al. Concordance between severity of disease, disability and health-related quality of life in myasthenia gravis. NeurolSci. 2010;31:41–5.
Leonardi M, Raggi A, Antozzi C, Confalonieri P, Maggi L, Cornelio F, et al. The relationship between health, disability and quality of life in myasthenia gravis: results from an Italian study. JNeurol. 2010;257:98–102. doi: 10.1007/s00415-009-5279-z. Epub 2009 Aug 8.
Rostedt A, Padua L, Stalberg EV. Correlation between regional myasthenic weakness and mental aspects of quality of life. EurJNeurol. 2006;13:191–3.
Rostedt A, Padua L, Stalberg EV. Correlation between a patient-derived functional questionnaire and abnormal neuromuscular transmission in Myasthenia Gravis patients. ClinNeurophysiol. 2005;116:2058–64.
Winter Y, Schepelmann K, Spottke AE, Claus D, Grothe C, Schroder R, et al. Health-related quality of life in ALS, myasthenia gravis and facioscapulohumeral muscular dystrophy. JNeurol. 2010;257:1473–81.
Basta IZ, Pekmezovic TD, Peric SZ, Kisic-Tepavcevic DB, Rakocevic-Stojanovic VM, Stevic ZD, et al. Assessment of health-related quality of life in patients with myasthenia gravis in Belgrade (Serbia). NeurolSci. 2012;33:1375–81.
Twork S, Wiesmeth S, Klewer J, Pohlau D, Kugler J. Quality of life and life circumstances in German myasthenia gravis patients. Health QualLife Outcomes. 2010;8:129.
Kulkantrakorn K, Jarungkiatkul W. Quality of life of myasthenia gravis patients. JMedAssocThai. 2010;93:1167–71.
Ariatti A, Stefani M, Miceli P, Benuzzi F, Galassi G. Prognostic factors and health-related quality of life in ocular Myasthenia Gravis (OMG). Int J Neurosci. 2014;124:427–35.
Busch C, Machens A, Pichlmeier U, Emskotter T, Izbicki JR. Long-term outcome and quality of life after thymectomy for myasthenia gravis. AnnSurg. 1996;224:225–32.
Suzuki S, Murai H, Imai T, Nagane Y, Masuda M, Tsuda E, et al. Quality of life in purely ocular myasthenia in Japan. BMC Neurol. 2014;14:142.
Sanders DB, Evoli A. Immunosuppressive therapies in myasthenia gravis. Autoimmunity. 2010;43:428–35.
Evoli A, Bianchi MR, Riso R, Minicuci GM, Batocchi AP, Servidei S, et al. Response to therapy in myasthenia gravis with anti-MuSK antibodies. Ann N Y Acad Sci. 2008;1132:76–83.
Guptill JT, Sanders DB, Evoli A. Anti-MuSK antibody myasthenia gravis: clinical findings and response to treatment in two large cohorts. Muscle Nerve. 2011;44:36–40.
Romi F, Gilhus NE, Varhaug JE, Myking A, Aarli JA. Disease severity and outcome in thymoma myasthenia gravis: a long-term observation study. EurJNeurol. 2003;10:701–6.
Niks EH, Kuks JB, Verschuuren JJ. Epidemiology of myasthenia gravis with anti-muscle specific kinase antibodies in The Netherlands. JNeurolNeurosurgPsychiatry. 2007;78:417–8.
Maniaol AH, Boldingh M, Brunborg C, Harbo HF, Tallaksen CM. Smoking and socio-economic status may affect myasthenia gravis. EurJNeurol. 2013;20:453–60.
Boldingh MI, Maniaol AH, Brunborg C, Dekker L, Heldal AT, Lipka AF, et al. Geographical Distribution of Myasthenia Gravis in Northern Europe - Results from a Population-Based Study from Two Countries. Neuroepidemiology. 2015;44:221-31.
Maniaol AH, Brunborg C, Tallaksen CM. Development and validation of a self-administered questionnaire for myasthenia gravis patients. Neuroepidemiology. 2010;34:253–61.
Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51:1055–68.
Loge JH, Kaasa S, Hjermstad MJ, Kvien TK. Translation and performance of the Norwegian SF-36 Health Survey in patients with rheumatoid arthritis. I. Data quality, scaling assumptions, reliability, and construct validity. J Clin Epidemiol. 1998;51:1069–76.
Loge JH, Kaasa S. Short form 36 (SF-36) health survey: normative data from the general Norwegian population. Scand J Soc Med. 1998;26:250–8.
Klevan G, Jacobsen CO, Aarseth JH, Myhr KM, Nyland H, Glad S, et al. Health related quality of life in patients recently diagnosed with multiple sclerosis. Acta Neurol Scand. 2014;129:21–6.
Muller B, Assmus J, Herlofson K, Larsen JP, Tysnes OB. Importance of motor vs. non-motor symptoms for health-related quality of life in early Parkinson’s disease. Parkinsonism Relat Disord. 2013;19:1027–32.
Ware Jr JE, Snow KK, Kosinski M. SF-36 Health Survey: Manual and Interpretation Guide. 2000th ed. Lincoln RI: QualityMetric, Incorporated; 1993.
Ware Jr JE, Kosinski MA. SF-36 Physical & Mental Health Summary scales: A manual for Users of Version 1, Second edition. 2nd ed. Lincoln, Rhode Island: QualityMetric Incorporated; 2001.
Kulkantrakorn K, Sawanyawisuth K, Tiamkao S. Factors correlating quality of life in patients with myasthenia gravis. NeurolSci. 2010;31:571–3.
Utsugisawa K, Suzuki S, Nagane Y, Masuda M, Murai H, Imai T, et al. Health-related quality of life and treatment targets in myasthenia gravis. Muscle Nerve. 2014.
Masuda M, Utsugisawa K, Suzuki S, Nagane Y, Ito S, Kabasawa C, et al. The MG-QOL15 Japanese version: validation and associations with clinical factors. Rinsho Shinkeigaku. 2012;52:1043–6.
Stickler DE, Stickler LL. Single-fiber electromyography during menstrual exacerbation and ovulatory suppression in MuSK antibody-positive myasthenia gravis. Muscle Nerve. 2007;35:808–11.
Massey JM, Sanders DB. Single fiber electromyography in myasthenia gravis during pregnancy. Muscle Nerve. 1993;16:458–60.
Benatar M, Kaminski HJ. Evidence report: the medical treatment of ocular myasthenia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2007;68:2144–9.
Kerty E, Elsais A, Argov Z, Evoli A, Gilhus NE. EFNS/ENS Guidelines for the treatment of ocular myasthenia. Eur J Neurol. 2014;21(5):687–93.
Nortvedt MW, Riise T, Myhr KM, Nyland HI. Quality of life in multiple sclerosis: measuring the disease effects more broadly. Neurology. 1999;53:1098–103.
West E, Wallberg-Jonsson S. Health-related quality of life in Swedish men and women with early rheumatoid arthritis. Gend Med. 2009;6:544–54.
Uutela T, Kautiainen H, Jarvenpaa S, Salomaa S, Hakala M, Hakkinen A. Patients with rheumatoid arthritis have better functional and working ability but poorer general health and higher comorbidity rates today than in the late. Scand J Rheumatol. 1990;2014:1–9.
Grob D, Brunner N, Namba T, Pagala M. Lifetime course of myasthenia gravis. Muscle Nerve. 2008;37:141–9.
Burns TM, Graham CD, Rose MR, Simmons Z. Quality of life and measures of quality of life in patients with neuromuscular disorders. Muscle Nerve. 2012;46:9–25.
Acknowledgements
The authors are grateful to all participating neurological departments and clinics in Norway and the Netherlands. We also thank all MG patients for their participation. We are grateful to Marit Elverhøy (technical assistance) and collaborators within the FIGHT-MG project for their contribution in the study.
Study funding
The project was mainly supported by FIGHT- MG EU FP7 frame program grant no 242210 (to MIB) and Euromyasthenia EU FP7 no 2005105 (to AHM). The project was also supported by grants from Unifor.no, Valsøe’s foundation, Wilhelmsen’s foundation, the Norwegian association for patients with muscle disease, Princes Beatrix foundation, Association Francaise contre les Myopathies.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
MIB, LD, AM, AFL, EHN and CT have no conflicts of interest to declare. JJGMV was involved in the thymectomy trial, sponsored by NIH, and in a FP7-HEALTH-2013-INNOVATION-1 European grant number 602420 on MG. The Neurology department of the LUMC has received royalties from antibody tests. JJGMV did not receive any personal payments.
Authors’ contributions
MIB designed study, conceptualized study, analysis and interpretation of data, drafted and revised the manuscript. AHM designed and conceptualized study, analysis and interpretation of data, revised the manuscript. CB statistical analysis and interpretation, revised the manuscript. LD, AFL, EHN acquired clinical data and revised the manuscript. JJGMV designed study, analysis and interpretation of data, drafted and revised the manuscript. CMET initiated the project, designed study, analysis and interpretation of data, drafted and revised the manuscript. All authors read and approved the final manuscript.
Additional file
Additional file 1:
Table e-1. Mean SF-36 scale scores of MG patients versus healthy controls (stratified by gender).
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Boldingh, M.I., Dekker, L., Maniaol, A.H. et al. An up-date on health-related quality of life in myasthenia gravis -results from population based cohorts. Health Qual Life Outcomes 13, 115 (2015). https://doi.org/10.1186/s12955-015-0298-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-015-0298-1