Abstract
Background
The World Health Organization has set a goal to reach world elimination of hepatitis C virus (HCV) by 2030. Needle and syringe programs (NSP) for people who inject drugs (PWID) are crucial to achieve this goal. The NSP in Uppsala, Sweden, was opened in 2016 and has since 2018 provided HCV treatment for PWID. The aim of this study was to investigate HCV prevalence, risk factors and treatment uptake and outcome in NSP participants.
Methods
Data from 450 PWID registered at the Uppsala NSP between 2016-11-01 and 2021-12-31 were collected from the national quality registry InfCare NSP. Data from the 101 PWID treated for HCV at the Uppsala NSP were collected through patient journal review. Descriptive and inferential analysis was performed. Ethical approval was obtained from the Ethical Review Board in Uppsala (dnr 2019/00215).
Results
The mean age was 35 years. 75% were males (336/450), and 25% were females (114/450). The overall HCV prevalence was 48% (215/450) with a declining trend over time. Factors associated with a higher risk of HCV were older age at registration (OR 1.025, 95% CI 1.004–1.046), lower age at injection drug debut (OR 0.963, 95% CI 0.932–0.996), lower education level (OR 1.829, 95% CI 1.185–2.821) and higher number of total visits at the NSP (OR 1.005, 95% CI 1.001–1.009). The overall HCV treatment uptake was 47% (101/215), of which 77% (78/101) completed HCV treatment. The HCV treatment compliance was 88% (78/89). 99% (77/78) were cured with a sustained virologic response 12 weeks after completed treatment. The reinfection rate over the study period was 9/77 (11.7%); all were male with mean age of 36.
Conclusions
HCV prevalence, treatment uptake and treatment outcome have improved since the opening of the Uppsala NSP. However, further measures are needed to reach the HCV elimination goal. Outreach HCV treatment programs for PWID should be explored and evaluated in combination with further implementation of low-threshold programs.
Similar content being viewed by others
Background
Hepatitis C virus (HCV) is a blood-borne virus that causes chronic liver inflammation, which over time leads to liver cirrhosis, liver cancer and liver-related death [1, 2]. The prevalence is estimated at 58–80 million people globally and the mortality at approximately 290,000 deaths in 2019 [3–5]. The most common transmission route for HCV in high-income countries is sharing of unsterile injection equipment (needle/syringes and/or paraphernalia) among people who inject drugs (PWID), making this subgroup subject for special attention [6, 7]. In Sweden, an estimated 80% of new HCV infections are caused by sharing of unsterile injection equipment among PWID [8].
The World Health Organization (WHO) has set a global goal to reach world elimination of HCV and hepatitis B virus (HBV) by 2030, which includes a 90% reduction in chronic infection and a 65% reduction in HCV-related deaths [9]. Available data show that although major progress has been made we are far from the 2030 goal with most countries not on track to reach the targets [5, 10]. An important service target to reach this goal is distribution of at least 300 sterile needles and syringes/PWID/year [9]. Needle and syringe programs (NSP) are harm reduction services that provide clean injection equipment and other health services to PWID. NSPs are a cornerstone to achieve the HCV elimination goal, as they contribute to the reduction of HCV transmission and injection risk behavior among PWID [11–13]. The number of NSPs in Sweden has increased dramatically in the last 10 years after a long period of political hesitancy. Following a change in the NSP law in 2017, a scale-up of NSPs in Sweden started [14]. In the end of 2020, 17 out of 21 regions had launched NSP [15]. The NSP in Uppsala opened in 2016 has since 2018 offered free HCV treatment to all patients.
Data regarding the size of the PWID population in Sweden have been estimated at between 8000 and 26,000; however, the data are outdated and inconclusive and estimation is hard due to methodological difficulties [12, 16–18]. Previous estimates have predicted the HCV prevalence in the PWID population in Sweden in 2016 at 60% and the treatment rate of HCV positive PWID in 2015/2016 to 0.5–2% [19]. A 2017 study from the NSP in Stockholm showed a HCV prevalence of 62.1%, but no such analysis has been performed on the PWID population in Uppsala [20]. HCV treatment is free in Sweden and consists of direct acting antivirals (DAA) [21, 22]. DAAs are an effective, well-tolerated and safe treatment with cure rates of > 95%; however, more data are needed on compliance and treatment results in the PWID population [23, 24]. An analysis from 2021 showed that achieving the WHO elimination goal in Sweden will require an expansion of harm reduction programs to reach 90% of the PWID population and treating 90% of HCV-positive NSP participants as well as > 7% of HCV-positive PWID not attending harm reduction programs [25]. To achieve this goal, an evaluation of the NSPs and its’ effects on HCV in the PWID population is needed.
The aim of this study is to examine HCV prevalence, risk factors, treatment uptake and treatment outcome among participants at the Uppsala NSP. These data are needed to estimate the effect of the NSP as well as identify areas in need of improvement.
Methods
The NSP in Uppsala
The NSP in Uppsala opened in 1 November 2016 is located in a primary care facility. In addition to offering exchange of needles, syringes and paraphernalia, it also provides vaccine for hepatitis A (HAV) and HBV, testing for HAV, HBV, HCV, human immunodeficiency virus (HIV) and other sexually transmitted diseases (chlamydia, gonorrhea, syphilis), treatment for HCV (initiated in 2018), treatment for injection-related infections and primary care. The patients are offered nasal naloxone along with a brief education in cardiopulmonary resuscitation. At the NSP there is a broad competence consisting of two clinical nurse specialists and a counselor working full-time as well as a general practitioner, a psychiatrist, a midwife and a substance abuse counselor working part-time. There is also an infectious disease consultant available.
Study population and data
The study consists of two parts. First, an extraction of anonymous data from the national quality registry InfCare NSP of NSP participants in Uppsala during the study period was performed [26, 27]. Secondly, a patient journal review study was performed on longitudinal data from those treated for HCV at the Uppsala NSP who had provided an informed written consent.
The NSP national quality registry
The NSPs in Sweden collaborate on the national quality registry InfCare NSP where sociodemographic data and HCV test result data are entered at enrollment and follow-up visits [26, 27]. Anonymous data were extracted from the NSP quality registry for all individuals attending the Uppsala NSP between 1 November 2016 and 31 December 2021 that had registered in the InfCare NSP. NSP participants are at the first visit informed of the national quality registry by trained health staff and provide an oral informed consent according to the standards set for the national quality registry [26, 27]. Participants are also informed that they can opt out at any time, and written information of this is available in the NSP waiting area.
The requirements to register at an NSP in Sweden are served as inclusion criteria for the national quality registry and this study; these are: age 18 years or above, documented injection drug use, valid identification and no current admission to a hospital or substance abuse treatment center. Participants registered at other NSP and then transferring to Uppsala NSP were included, making possible date of first registration as early as 2013. Patients with missing registration data and/or missing HCV test were excluded as well as patients also registered at other NSP in Sweden who were registered in Uppsala less than 1 month in total during the study period. At the NSP registration visit participants are tested for HBV, HCV and HIV and they also engage in a face-to-face interview with NSP staff and fill out a standardized questionnaire regarding birth date, home municipality, residence municipality, education level, marital status, living situation, employment, if they have children, status and previous testing for HIV, HBV and HCV, vaccine status, age of drug debut, first drug used, age of injection drug debut, first injected drug, main drug used currently, injection use past month, past injected drug, injection risk behavior, custody/prison time past year, being in opioid substitution treatment, being in substance use treatment center past year, being admitted to a hospital past year, condom use during sex past month and selling or buying sex. After this, follow-up interviews and HCV testing are performed every 6 months, if possible. Our analysis used the HCV data from registration and follow-up testing from the national quality registry. For participants with negative HCV RNA test at registration, either negative HCV RNA or negative anti-HCV test was considered negative HCV status at follow-up testing. In the dataset from the national quality registry, we only had information on the seroprevalence of anti-HCV on some participants; therefore, no analysis on anti-HCV for the study population is presented in our results.
Patient journal review of NSP participants treated for HCV
The second part of the study consists of a patient journal review of the 101 NSP participants who have completed or started HCV treatment at the Uppsala NSP between 1 November 2016 and 31 December 2021.
For patients with positive HCV RNA, genotype analysis and risk of liver disease are determined. Patients at risk are examined with FibroScan. Patients with positive HCV status are then offered HCV treatment at the NSP. At the initial treatment visit at the NSP, the participants are given study information both orally and in writing by trained health staff. They then provide an informed written consent. Participants are also informed that they can withdraw from the study at any time.
Patient journal review was performed for the variables gender, age, liver status, virus type, virus level, way of transmission, date of transmission (when known), date of diagnosis, treatment received, complications from treatment, discontinued treatment, if SVR had occurred, if reinfection has occurred and mortality. An undetectable HCV RNA 12 weeks after therapy completion was considered a sustained virologic response (SVR).
Immunological and virological methods
All virological tests for HCV RNA were performed using the Abbott Alinity m system, with a limit of detection of 12 IU/mL. All serological tests for HCV were performed using the Abbott Alinity i system, with a sensitivity of 100% (95% confidence interval of 99.2–100%).
Statistical methods
The statistical program IBM SPSS 28.0.0.1 was used for all analyses. Descriptive analysis was performed for demographic variables and is presented as proportions, mean or median levels and range. The Chi-square test or Fisher exact test was used to test categorical variables.
Simple and multiple univariate logistic regression was used to study the associations with the outcome variable, positive HCV RNA status. Eleven possible determinants were tested against the outcome selected based on HCV risk factors reported in previous research; gender, age at registration, age of drug use debut, age of injection drug use debut, number of visits to the NSP during the study period, level of education, living situation the past 3 months, employment in the past 3 months, primary drug used the past 12 months, shared needle/syringe and/or paraphernalia in the past month and HBV status at registration [12, 28]. The results are reported as odds ratios (OR) with confidence intervals (CI) set at 95%. A p value < 0.05 was considered statistically significant.
Ethics
Ethical approval for the study as described above was obtained from the Regional Ethical Review Board in Uppsala, Sweden, with dnr number: 2019/00215.
Results
Of the 519 participants identified in the NSP national quality registry according to the inclusion criteria, 17 were excluded due to missing registration data, 15 due to missing HCV test and 37 due to less registration time than one month at Uppsala NSP resulting in 450 participants included in the analysis.
Sociodemographic data
In Table 1 demographic data are presented in total and per HCV serostatus. Of the 450 included participants, 336 (74.7%) were male and 114 (25.3%) were female. The mean age at registration was 34.6. A majority was born in Sweden and had Uppsala as their home region, representing 310 (88.1%) and 283 (65.8%) participants, respectively. 42 patients were born outside of Sweden; 16 in Europe, 24 in Asia, 1 in Africa and 1 in South America. Of the 147 participants with other home region than Uppsala, the most common regions were the adjacent regions Gävleborg (42/147), Stockholm (32/147) and Västmanland (31/147).
Drug use
The overall mean age of debut of drug use and debut of injection drug use was 15 years (median 14) and 22 years (median 20), respectively. The most common first drug was tetrahydrocannabinol (THC) representing 282 participants (63.9%), followed by amphetamine representing 77 participants (17.5%). In contrast, the most common first injected drug was amphetamine representing 299 (67.8%), followed by heroin representing 79 (17.9%). Lastly, with regard to primary drug used the past 12 months, 264 participants (59.1%) answered amphetamine, whereas 102 participants (22.8%) reported heroin.
Mortality
Nineteen participants died during the study period, representing a mortality of 4.2%. Of these, 15 (78.9%) were male and 4 (21.1%) were female. The mean age was 36.8 years, and the cause of death was overdose in 10 cases (52.6%), accident in 1 case (5.3%) and unknown in 8 cases (42.1%). Of the deceased, 8 (42.1%) were HCV positive at NSP registration.
HCV prevalence
The overall HCV prevalence was 47.8% (215/450) with a declining trend over time, as presented in Fig. 1. Of the 215 HCV-positive patients, 170 (79.1%) had a positive HCV test at registration whereas 45 (20.9%) had a negative registration test and then positive HCV test at repeat testing (5 in 2016, 10 in 2017, 11 in 2018, 4 in 2019, 11 in 2020 and 4 in 2021). 343/450 (76.2%) participants had their NSP registration test taken in Uppsala, whereas 107/450 (23.8%) registered initially at an NSP in another region and had their HCV registration test taken there.
HCV risk factors
Table 2 displays OR and CI correlated to the outcome positive HCV RNA at registration. The simple univariate regression analysis showed a higher risk of HCV positivity correlated to younger age at debut of drug use (OR 0.927, 95% CI 0.879–0.977), younger age at debut of injection drug use (OR 0.956, 95% CI 0.931–0.982), higher number of visits at NSP (OR 1.004, 95% CI 1.003–1.011) and lower level of education (OR 2.216, 95% CI 1.510–3.251).
When adjusting for possible confounders in the multiple univariate logistic regression, determinants associated with a higher risk of HCV positivity were older age at registration (OR 1.025, 95% CI 1.004–1.046), younger age at debut of injection drug use (OR 0.963, 95% CI 0.932–0.996), lower education level (OR 1.829, 95% CI 1.185–2.821) and higher number of visits at NSP (OR 1.005, 95% CI 1.001–1.009).
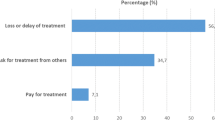
HCV treatment uptake
HCV treatment uptake is presented in Fig. 2. Out of the 215 HCV positive NSP participants, the proportion who consecutively received HCV treatment were 47% (101/215). After the Uppsala NSP started HCV treatment in 2018, the treatment uptake improved from 0% (0/51) in 2016–2017 to 70% (23/33) in 2021. Those with Uppsala as home region had a higher treatment uptake compared to those with other home region, 58.7% (71/121) versus 28% (23/82).
HCV treatment outcome
Of those treated, 73 patients (72.3%) were male whereas 28 patients (27.7%) were female. The mean age at treatment was 39. 68 patients (82.9%) were born in Sweden and 14 patients (17.1%) were born abroad. Genotype analysis showed that 51 participants had genotype 1 (50.5%), 44 participants had genotype 3 (43.6%), 4 participants had genotype 2 (4%) and 1 participant had genotype 1 and 3 (1%). In one participant (1%), genotype could not be determined.
Of all 101 patients where treatment was initiated, 78 patients (77.2%) completed the treatment, 11 patients (10.9%) discontinued the therapy and 12 patients (11.9%) were still under treatment at end of study. Excluding those who were still under treatment, this results in a treatment compliance of 87.6% (78/89). Out of the 11 discontinued therapies, 6 were discontinued during treatment, whereas 5 were lost to follow-up (negative HCV RNA at therapy completion, but missing HCV RNA 12 weeks after therapy completion). 77 out of the 78 who completed the therapy had undetectable HCV RNA 12 weeks after therapy completion, indicating a cured infection. One patient had a positive HCV RNA at therapy completion and at follow-up testing 12 weeks after therapy completion. This represents a SVR of 98.7% (77/78).
Reinfection after HCV treatment
At data extraction, 9/77 patients (11.7%) had gotten a HCV reinfection after therapy completion, of which 6 had started or completed HCV treatment for the reinfection. In the reinfection group, all were male with a mean age of 36.
Discussion
The HCV prevalence at the first NSP visit among Uppsala NSP participants was 48%, with a declining trend over time. HCV treatment uptake was at 47% and HCV treatment compliance 88%. Of those who completed HCV treatment, the 12-week SVR rate showed an optimal treatment outcome of 99%. The HCV reinfection rate among those treated was 11.7%. The data point out the importance of NSPs providing HCV treatment as well as the need of NSP scale-up and outreach programs to increase access for PWID in order to reach the HCV elimination goal.
HCV prevalence at the Uppsala NSP compared to NSPs in other settings
The overall HCV prevalence of 48% proved to be lower than both the HCV prevalence projection among PWID in Sweden of 60% and the HCV prevalence shown at the NSP in Stockholm of 62% in 2017 [19, 20]. One possible reason for this could include that NSP participants in Uppsala were younger than in Stockholm, considering that older age could equal an increased number of exposure times for HCV. Conversely, a 2021 Norwegian study showed a very similar HCV prevalence of 42% among people who use drugs [30]. Further data on HCV prevalence among PWID show a range from 16% from NSP data in Australia in 2021, 26% in England in 2021 and 37% in Canada in 2017–2019 [31–33]. The decreasing HCV prevalence over time indicates a reduction of HCV transmission in the PWID community after the NSP opened and HCV treatment started; however, further analysis of the prevalence subgroups is needed to examine this further.
High prevalence of HCV among PWID produces a risk of transmitting HCV through unsafe injection practice. Although the prevalence is lower than earlier Swedish projection data, the studies clearly show that other countries report lower HCV prevalence rates among NSP participants. The HCV prevalence data consolidates that scale-up of low threshold HCV test and treatment opportunities for PWID, such as NSPs, are of importance in Sweden to keep step with the global improvements.
Improving treatment uptake and compliance
Curing HCV in PWID prevents further HCV transmission and reduces HCV related mortality as well as HCV prevalence. Data from 2019 suggest that 62% of those diagnosed with HCV globally are treated, representing an almost ten-fold increase since 2015 [5]. Compared to the 0.5–2% treatment rate in HCV positive PWID from 2015/2016, our data show a remarkable increase with a total treatment uptake of 47% [19]. By comparison, a NSP report from Australia showed a lifetime treatment uptake among NSP participants of 62% in 2021 [32].
When looking at compliance to HCV treatment, a study among NSP participants in Malmö (Sweden) showed a treatment compliance of 95% in 2018–2019 [34]. A Canadian meta-analysis from 2018 showed that among individuals with recent injecting drug use treatment completion was 96.9%. Both these studies showed somewhat higher rates than our treatment compliance of 88% [35].
To reach the WHO elimination goal, the treatment uptake needs to increase to 90% [25]. Multiple factors can be suggested as underlying causes for absence of treatment or treatment completion in HCV positive NSP participants. For example, participants who only attended the NSP once must return to the NSP on their own to be informed and offered treatment. This is a main obstacle since many NSP participants are lost to follow-up. Similarly, a 2020 Swedish study found a high occurrence of lost to follow-up among patients after HCV diagnosis [36]. Further, patients travelling from neighboring regions may reject treatment due to long distance to the NSP. This hypothesis is strengthened by our data showing a higher treatment uptake for those with Uppsala as home region [37, 38]. Two of the neighboring regions to Uppsala (together comprising half of NSP participants from another region) did not have NSPs in their home region during the study period, highlighting a need of NSPs in these regions. Lastly, the patient must accept and be willing to comply to treatment which may not be a possible choice due to the life situation for some PWID.
To increase treatment uptake and treatment completion PWID access to NSP program, including HCV treatment, is necessary. Additional studies of the HCV positive group not reached with HCV treatment and the PWID group not attending the NSP is needed to find effective ways of approaching this ‘difficult to reach’ part of the PWID population to identify all in need of HCV treatment [39].
Reinfection rate
A meta-analysis from 2016 showed a 5-year HCV recurrence rate after interferon treatment of 10.67% in the high-risk population, driven mainly by reinfection rather than late relapse [40]. When looking at reinfection among PWID after DAA treatment, data from 2017–2018 show reinfection rates from 3.11 per 100 person years to 8.8 per 100 person years [41, 42]. A 2018 study analyzing HCV treatment of 94 PWID at an NSP in Scotland showed a reinfections rate of 6.5% after 6 months, and 19% after 18 months [43].
Correspondingly, we found a HCV reinfection rate of 11.7% among those treated. This highlights that a high risk of HCV re-exposure prevails among NSP participants in Uppsala. The overall HCV prevalence among PWID must be lowered further through increasing treatment efforts, to decrease this rather high reinfection rate. Further implementation of low-threshold programs (i.e., a further scale-up of NSPs) and outreach programs within current NSPs, such as peer-based ‘secondary needle exchange’ and mobile HCV testing and treatment clinics, are measures that could serve this purpose which have already been implemented successfully in Norway, Denmark and Spain [44–48].
HCV risk factors
The results show the need for special attention and information on HCV treatment to the subgroups of NSP participants at higher risk for HCV. Older age at registration as a risk factor for HCV most likely illustrates the accumulated need for an NSP over time, as the PWID group have been unaware of their HCV status and therefore also undiagnosed and untreated. Younger age at injection debut as a HCV risk factor is most likely explained by a longer period of injection drug use which equals to an increased number of exposure times, i.e., sharing of unsterile injection equipment. Lower education level is a known factor correlated to higher morbidity and mortality among NSP participants and has been connected to a higher level of injection risk behavior at the Stockholm NSP [12, 28]. In contrast to data reported from the neighboring Stockholm NSP, no association was found between HCV status and female gender, living situation, amphetamine use or younger age in our study.
Mortality
A Swedish study from 2018, with a mean follow-up time of 13.7 years, among PWID who inject amphetamine showed a mortality of 22%, a mean age of death of 48 years and a majority of fatalities due to external causes (accidents, undetermined intents, suicide and poisoning) [49]. On the other hand, an Australian study from 2018 report a 7% mortality and median age at death of 30.6 years in PWID with high incidence of HCV infection [50]. To further establish mortality data on the PWID group in Uppsala, a longer follow-up period and further examination of the group is needed. This would also be useful for further evaluation of national mortality data among PWID in Sweden.
Strengths
The standardization of the national quality registry InfCare NSP registration data has enabled the study to include the same information on all participants registered at the NSP since opening, making data comprehensive and thorough. Since the InfCare NSP database is used nationally, registration data from participants first registered at other NSP were available and identical. By following repeat HCV testing results after registration, a longitudinal study design was made possible with information on HCV incidence and HCV reinfection.
Limitations
Self-reported data include a risk for recall bias as well as social desirability bias as study participants took a face to face survey with NSP staff. When looking at repeat testing all repeat tests were entered, not considering at what NSP the test was taken. Some participants switch NSP intermittently and therefore do repeat testing at different NSP locations. There may be some underreporting on having received HCV treatment in our analysis as some intermittent NSP participants in Uppsala may have received HCV treatment elsewhere. This could possibly cause a risk of underestimation of HCV treatment uptake.
Conclusions
HCV prevalence, treatment uptake and treatment outcome have improved since the opening of the Uppsala NSP in 2016. However, further measures are still needed to reduce HCV transmission, increase HCV treatment and increase compliance, to reach the global HCV elimination goal. This includes further scale-up of NSPs, efforts to facilitate higher NSP enrolment and exploring and evaluating outreach programs for PWID, such as mobile HCV testing and treatment.
Availability of data and materials
Data are available from the Needle and Syringe Program quality registry board. Requests can be submitted via email to: Styrgruppen.for.nationellt.sprutbyte.slso@regionstockholm.se.
Abbreviations
- Anti-Hbc:
-
Antibody to HBV core
- Anti-HCV:
-
Antibody to HCV
- CI:
-
Confidence interval
- DAA:
-
Direct acting antiviral
- HAV:
-
Hepatitis A
- HBV:
-
Hepatitis B
- HCV:
-
Hepatitis C
- HIV:
-
Human immunodeficiency virus
- NSP:
-
Needle and syringe programs
- OR:
-
Odds ratio
- PWID:
-
People who inject drugs
- RNA:
-
Ribonucleic acid
- SVR:
-
Sustained virologic response, defined in this report as undetectable levels of HCV RNA in plasma 12 weeks after completed therapy
- THC:
-
Tetrahydrocannabinol
- WHO:
-
World Health Organization
References
Liang TJ, Rehermann B, Seeff LB, Hoofnagle JH. Pathogenesis, Natural history, treatment, and prevention of hepatitis C. Ann Intern Med. 2000;132(4):296.
Seeff LB. The history of the “natural history” of hepatitis C (1968–2009). Liver Int. 2009;29:89–99.
Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61(1):S45-57.
Blach S, Zeuzem S, Manns M, Altraif I, Duberg AS, Muljono DH, et al. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol. 2017;2(3):161–76.
World Health Organization. Global progress report on HIV, viral hepatitis and sexually transmitted infections [Internet]. 2021 [cited 2022 Oct 22]. https://www.who.int/publications/i/item/9789240027077
Alter MJ. Epidemiology of hepatitis C virus infection. World J Gastroenterol WJG. 2007;13(17):2436–41.
Palmateer N, Hutchinson S, McAllister G, Munro A, Cameron S, Goldberg D, et al. Risk of transmission associated with sharing drug injecting paraphernalia: analysis of recent hepatitis C virus (HCV) infection using cross-sectional survey data. J Viral Hepat. 2014;21(1):25–32.
Folkhälsomyndigheten [The Public Health Agency of Sweden]. Hepatit C—sjukdomsstatistik [Hepatitis C—disease statistics] [Internet]. [cited 2022 Oct 22]. http://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/statistik-a-o/sjukdomsstatistik/hepatit-c/
World Health Organization. Combating hepatitis B and C to reach elimination by 2030 [Internet]. Geneva; 2016 [cited 2022 Oct 22]. Available from: https://www.who.int/publications-detail-redirect/combating-hepatitis-b-and-c-to-reach-elimination-by-2030
European Centre for Disease Prevention and Control (ECDC). The Sustainable Development Goals and Hepatitis B and C in the EU/EEA. Stockholm; 2021.
Platt L, Minozzi S, Reed J, Vickerman P, Hagan H, French C, et al. Needle and syringe programmes and opioid substitution therapy for preventing HCV transmission among people who inject drugs: findings from a Cochrane Review and meta-analysis: OST and NSP to prevent HCV transmission. Addiction. 2018;113(3):545–63.
Kåberg M, Karlsson N, Discacciati A, Widgren K, Weiland O, Ekström AM, et al. Significant decrease in injection risk behaviours among participants in a needle exchange programme. Infect Dis. 2020;52(5):336–46.
Larney S, Peacock A, Leung J, Colledge S, Hickman M, Vickerman P, et al. Global, regional, and country-level coverage of interventions to prevent and manage HIV and hepatitis C among people who inject drugs: a systematic review. Lancet Glob Health. 2017;5(12):e1208–20.
Socialstyrelsen [The National Board of Health and Welfare]. Ändringar i lagen om utbyte av sprutor och kanyler [Changes in the law of needle and syringe exchange] [Internet]. 2019 [cited 2022 Oct 22]. Report No.: 2019–12–6462. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2019-12-6462.pdf
Socialstyrelsen [The National Board of Health and Welfare]. Naloxon och sprututbyten nu i nästan alla regioner [Naloxone and needle syringe programs in almost all regions] [Internet]. 2021 [cited 2022 Oct 22]. Available from: https://www.socialstyrelsen.se/om-socialstyrelsen/pressrum/press/naloxon-och-sprututbyten-nu-i-nastan-alla-regioner/
Folkhälsomyndigheten [The Public Health Agency of Sweden]. Hälsofrämjande och förebyggande arbete med hepatit och hiv för personer som injicerar droger [Health promoting and preventive work of hepatitis and HIV for people who inject drugs] [Internet]. 2015 [cited 2022 Oct 22] p. 6–7, 10, 15–6. Available from: http://www.folkhalsomyndigheten.se/publicerat-material/publikationsarkiv/h/halsoframjande-och-forebyggande-arbete-med-hepatit-och-hiv-for-personer-som-injicerar-droger-en-vagledning/
Centralförbundet för alkohol- och narkotikaupplysning [The Swedish Council for Information on Alcohol and Other Drugs]. Drogutvecklingen i Sverige 2019 [Drug development in Sweden 2019] [Internet]. Stockholm; 2019 [cited 2022 Oct 22] p. 26–7. Available from: https://www.can.se/publikationer/drogutvecklingen-i-sverige-2019/
Socialstyrelsen [The National Board of Health and Welfare]. En uppskattning av omfattningen av injektionsmissbruket i Sverige [An estimation of injection drug use in Sweden] [Internet]. Stockholm; 2013 [cited 2022 May 10] p. 19. Available from: https://www.socialstyrelsen.se/publikationer/
Fraser H, Martin NK, Brummer-Korvenkontio H, Carrieri P, Dalgard O, Dillon J, et al. Model projections on the impact of HCV treatment in the prevention of HCV transmission among people who inject drugs in Europe. J Hepatol. 2018;68(3):402–11.
Kåberg M, Hammarberg A, Lidman C, Weiland O. Prevalence of hepatitis C and pre-testing awareness of hepatitis C status in 1500 consecutive PWID participants at the Stockholm needle exchange program. Infect Dis. 2017;49(10):728–36.
Referensgruppen för Antiviral Terapi [Advisory group for antiviral therapy]. Läkemedelsbehandling av hepatit C-virusinfektion hos vuxna och barn 2017 [Drug treatment of hepatitis C virus infection in adults and children 2017] [Internet]. 2020 [cited 2022 Oct 22]. Available from: https://www.sls.se/rav/rekommendationer/hepatit-c-virus/
Lagging M, Wejstål R, Duberg AS, Aleman S, Weiland O, Westin J, et al. Treatment of hepatitis C virus infection for adults and children: updated Swedish consensus guidelines 2017. Infect Dis. 2018;50(8):569–83.
Grebely J, Hajarizadeh B, Dore GJ. Direct-acting antiviral agents for HCV infection affecting people who inject drugs. Nat Rev Gastroenterol Hepatol. 2017;14(11):641–51.
Götte M, Feld JJ. Direct-acting antiviral agents for hepatitis C: structural and mechanistic insights. Nat Rev Gastroenterol Hepatol. 2016;13(6):338–51.
Blach S, Blomé M, Duberg A, Jerkeman A, Kåberg M, Klasa P, et al. Hepatitis C elimination in Sweden: progress, challenges and opportunities for growth in the time of COVID-19. Liver Int. 2021;41(9):2024–31.
Anslutna register - qrcstockholm.se [Internet]. [cited 2023 May 15]. Available from: https://qrcstockholm.se/kvalitetsregister/anslutna-register
Karolinska Universitetssjukhuset [Karolinska University Hospital] Verkställighetsbeslut [Enforcement decision] 20160502, K1746-2016
Karlsson N, Santacatterina M, Käll K, Hägerstrand M, Wallin S, Berglund T, et al. Risk behaviour determinants among people who inject drugs in Stockholm, Sweden over a 10-year period, from 2002 to 2012. Harm Reduct J. 2017;14(1):57.
WMA - The World Medical Association-WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects [Internet]. [cited 2023 Apr 14]. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
Hannula R, Söderholm J, Svendsen T, Skaland M, Nordbø SA, Steinum H, et al. Hepatitis C outreach project and cross-sectional epidemiology in high-risk populations in Trondheim, Norway. Ther Adv Infect Dis. 2021;8:204993612110539.
Tarasuk J, Zhang J, Lemyre A, Cholette F, Bryson M, Paquette D. National findings from the Tracks survey of people who inject drugs in Canada, Phase 4, 2017–2019. Can Commun Dis Rep. 2020;46(5):138–48.
Kirby Institute, Faculty of Medicine & Health. Australian NSP Survey National Data Report 2017–2021. 2022.
UK Health Security Agency. Unlinked Anonymous Monitoring (UAM) Survey of HIV and viral hepatitis among PWID: 2022 Report. 2022.
Blomé MA, Bråbäck M, Alsterberg S, Jerkeman A. Hepatitis C treatment at a Swedish needle exchange program, a successful model of care—the ACTIONNE study. Int J Drug Policy. 2021;96:103407.
Lanièce Delaunay C, Maheu-Giroux M, Marathe G, Saeed S, Martel-Laferrière V, Cooper CL, et al. Gaps in hepatitis C virus prevention and care for HIV-hepatitis C virus co-infected people who inject drugs in Canada. Int J Drug Policy. 2022;103:103627.
Aleman S, Söderholm J, Büsch K, Kövamees J, Duberg A. Frequent loss to follow-up after diagnosis of hepatitis C virus infection: A barrier towards the elimination of hepatitis C virus. Liver Int. 2020;40(8):1832–40.
Simpson H, Manley P, Lawler J, Morey S, Buchanan E, Hewett M, et al. Distance to treatment as a factor for loss to follow up of hepatitis C patients in North East England. J Public Health. 2019;41(4):700–6.
Monnet E, Ramée C, Minello A, Jooste V, Carel D, Di Martino V. Socioeconomic context, distance to primary care and detection of hepatitis C: A French population-based study. Soc Sci Med. 2008;66(5):1046–56.
Dunn R, Wetten A, McPherson S, Donnelly MC. Viral hepatitis in 2021: The challenges remaining and how we should tackle them. World J Gastroenterol. 2022;28(1):76–95.
Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of late relapse or reinfection with hepatitis C virus after achieving a sustained virological response: a systematic review and meta-analysis. Clin Infect Dis. 2016;62(6):683–94.
Rossi C, Butt ZA, Wong S, Buxton JA, Islam N, Yu A, et al. Hepatitis C virus reinfection after successful treatment with direct-acting antiviral therapy in a large population-based cohort. J Hepatol. 2018;69(5):1007–14.
Yeung A, Palmateer NE, Dillon JF, McDonald SA, Smith S, Barclay S, et al. Population-level estimates of hepatitis C reinfection post scale-up of direct-acting antivirals among people who inject drugs. J Hepatol. 2022;76(3):549–57.
Schulkind J, Stephens B, Ahmad F, Johnston L, Hutchinson S, Thain D, et al. High response and re-infection rates among people who inject drugs treated for hepatitis C in a community needle and syringe programme. J Viral Hepat. 2019;26(5):519–28.
Palmateer NE, Taylor A, Goldberg DJ, Munro A, Aitken C, Shepherd SJ, et al. Rapid decline in HCV Incidence among people who inject drugs associated with national scale-up in coverage of a combination of harm reduction interventions. Ho W, editor. PLoS ONE. 2014;9(8):e104515.
Midgard H, Bjørnestad R, Egeland M, Dahl E, Finbråten A, Kielland KB, et al. Peer support in small towns: A decentralized mobile Hepatitis C virus clinic for people who inject drugs. Liver Int. 2022;liv.15266.
Lindqvist K, Wallmofeldt C, Holmén E, Hammarberg A, Kåberg M. Health literacy and changes in pattern of drug use among participants at the Stockholm Needle Exchange Program during the COVID-19 pandemic. Harm Reduct J. 2021;18(1):52.
Valencia J, Lazarus JV, Ceballos FC, Troya J, Cuevas G, Resino S, et al. Differences in the hepatitis C virus cascade of care and time to initiation of therapy among vulnerable subpopulations using a mobile unit as point-of-care. Liver Int. 2022;42(2):309–19.
Lazarus JV, Øvrehus A, Demant J, Krohn-Dehli L, Weis N. The Copenhagen test and treat hepatitis C in a mobile clinic study: a protocol for an intervention study to enhance the HCV cascade of care for people who inject drugs (T’N’T HepC). BMJ Open. 2020;10(11):e039724.
Åhman A, Jerkeman A, Blomé MA, Björkman P, Håkansson A. Mortality and causes of death among people who inject amphetamine: a long-term follow-up cohort study from a needle exchange program in Sweden. Drug Alcohol Depend. 2018;188:274–80.
Kimber J, Stoové M, Maher L. Mortality among people who inject drugs: Ten-year follow-up of the hepatitis C virus cohort. Drug Alcohol Rev. 2019;38(3):270–3.
Acknowledgements
We would like to express our gratitude to the participants at the Uppsala Needle and Syringe Program for generously sharing their experiences.
Funding
Open access funding provided by Uppsala University. This study has been supported with an educational grant via the Gilead Nordic Fellowship Programme. Susanne Strömdahl’s salary was supported by Akademiska University Hospital.
Author information
Authors and Affiliations
Contributions
S.S and A.L designed and planned the study. E.K and S.S analyzed the data and wrote the main manuscript text. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Ethical Review Board in Uppsala (dnr 2019/00215). Participants were informed by trained personnel and provided oral informed consent to participate in the quality registry, they could opt out at any time. Participants that received Hepatitis C virus treatment did, in addition, provide written informed consent.
Consent for publication
Consent to publish was collected from the participants as part of the informed consent procedure.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kågström, E., Lannergård, A., El Khosht, J. et al. Prevalence, risk factors, treatment uptake and treatment outcome of hepatitis C virus in people who inject drugs at the needle and syringe program in Uppsala, Sweden. Harm Reduct J 20, 77 (2023). https://doi.org/10.1186/s12954-023-00806-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12954-023-00806-w