Abstract
Background
Mycobacterium tuberculosis (Mtb) remains an unresolved threat resulting in great annual loss of life. The role of B cells during the protective immunity to Mtb is still unclear. B cells have been described as effector cells in addition to their role as antibody producing cells during disease.
Here we aim to identify and characterize the frequency of peripheral B-cell subpopulations during active Tuberculosis and over treatment response. Analysis were done for both class switched (CS) and non-class switched (NCS) phenotypes.
Methods
We recruited participants with active untreated pulmonary Tuberculosis, other lung diseases and healthy community controls. All groups were followed up for one week from recruitment and the TB cases till the end of treatment (month 6).
Results
Peripheral blood samples were collected, stained with monoclonal antibodies to CD19+ cells, Immunoglobulin (Ig) M, plasma cells (CD 138+), marker of memory (CD27+), immune activation (CD23+) and acquired on a flow cytometer. Circulating Marginal zone B cells (CD19+IgM+CD23−CD27+) and memory phenotypes are able to distinguish between TB diagnosis and end of treatment. The frequency of mature B cells from TB cases are lower than that of other-lung diseases at diagnosis. A subpopulation of activated memory B cells (CD19+IgM+CD23+CD27+) cells are present at the end of TB treatment.
Conclusions
This study identified distinctive B cell subpopulations present during active TB disease and other lung disease conditions. These cell populations warrants further examination in larger studies as it may be informative as cell markers or as effectors/regulators in TB disease or TB treatment response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Tuberculosis (TB), remains an unresolved threat that is responsible for great mortality and morbidity in humans. Its causative agent, Mycobacterium tuberculosis (Mtb), was ultimately responsible for 9 million newly reported cases and 1.5 million deaths during 2013 [1]. Although great progress has been made on T cell based tuberculosis research, it is imperative that new avenues have to be explored and that previously underappreciated cell types are re-evaluated for their roles during the tuberculosis infection with the expectation of bringing an end to the epidemic. It is commonly accepted that B cell and antibody-mediated responses confers protection against extracellular pathogens and that the regulation and control of intracellular organisms are through cellular immune mechanisms.
There is increasing evidence that demonstrate B cells functioning as mediators (in both effector and regulatory roles) of immunity outside of their classically designated profession as the facilitators of humoral immunity. B cell activation by Toll-like receptor (TLR) antigens or whole organisms (like BCG or Mtb) can lead to a range of outcomes to the host, either by producing antibody, secreting cytokines (including interleukin (IL)-6, IL-10, and interferon (IFN)-gamma) or presenting antigen to naïve T cells [2–5]. B cell responses are beneficial to the host during infections and damaging during autoimmune disease. Conversely, B cells have the capacity to limit the hosts defence (inflammatory response) against pathogens and shield against autoimmune pathologies. This demonstrates that B cells can have distinct roles as drivers and regulators of immunity depending on the functional properties they gain following receptor activation and differentiation.
Although ongoing studies and literature supports the functional role of B cells during TB [6], the respective change in the frequency of the circulating B cell repertoire during active Mtb infection remains a topic for discussion as some studies report either a significant decrease [7] or increase [8] of peripheral blood B cell populations in actively infected patients.
Immuno-phenotyping has proven to be a very useful tool in the identification, monitoring and management of various clinical diseases [9–11]. Although recent publications have sought to develop in depth multicolour flow cytometric panels for the accurate delineation of various lymphocyte populations and subpopulations (including B cells) during immunodeficiencies [12, 13], very few studies exist that specifically assess immune-phenotypic change during active Mycobacterium tuberculosis infection [7, 14]. Little is known about the immune-phenotypic change of the B cell lineage during active Mtb as current literature largely focuses on the general B cell presence (primarily looking at CD19+ B cells only) [7, 14], rather than on an in-depth analysis of various populations and subpopulations. This results in a lack of knowledge pertaining to changes in B cell populations implicated in effector roles such as circulating memory B cells or plasma populations. It also does not elucidate the current activation state of B cells nor the expression of surface molecules, thus highlighting the need for further investigation regarding this matter.
In this brief preliminary report, a total of 96 participant samples spanning three groups (tuberculosis – active infection; 52 samples, other-lung disease; 24 samples, and healthy community controls; 20 samples) and various time points relating to treatment were used to assess the B cell repertoire in detail with the hope of identifying unique phenotypic differences between the groups that could suffice as biomarkers of disease. The primary contribution of this data would be to map the phenotypic distribution of B cells between these groups with a vast range, as it would include phenotypes for both IgM+ and IgM− B cells. The actual isotype linked to the IgM− phenotypes have not been determined for this study.
Methods
Patients
This study was done in the Western Cape Province of South Africa where a 2003 report showed that the TB detection rate was 678/100,000 population [15]. Previous publications have defined the characteristics associated with the economically depressed and disadvantaged metropolitan population of homogeneous ethnicity primarily found in the Western Cape Province, presenting high incidence rates of Mtb and transmission [16, 17]. The study participants included all attendees of the Infectious Diseases Clinics at Tygerberg Hospital, all community members of surrounding areas including Ravensmead, Uitsig, Adriaanse, Elsiesriver and local health care clinics. A total of 96 HIV negative participants, spanning three groups, were recruited for this study. All the study participants were also negative for Hep B. Fifty-two had active drug susceptible tuberculosis disease (on standard TB treatment regime) (TB disease status was confirmed by two separate positive sputum smear tests and a PCR for DNA of bacteria of the Mtb complex, by utilising the GeneXpert platform), 20 were healthy community controls (Mtb culture negative, Quantiferon test positive, therefor assuming latently infected with Mtb) and the third group consisted of 24 other-lung disease (OLD) patients. These OLD patients were all TB and HIV negative and presented with at least one of the following: a) febrile illness with chest symptoms, b) radiographic evidence of viral or bacterial pneumonia, c) bronchiectasis with acute exacerbation, or d) acute exacerbation of asthma or COPD (chronic obstructive pulmonary disease). The OLD patients were not on any steroid treatment at the time on recruitment. Table 1 summarizes the demographic data of study participants.
B cell phenotyping
Peripheral blood samples from the two control groups and patients were collected on various scheduled visits which included diagnoses, day 7 on treatment and at week 24 (end of TB treatment). White blood cells were obtained by subjecting each sample to a red blood cell lysing step using BD FACSlyse solution (BD Bioscience Pharmingen – San Jose, CA, USA). Leukocytes were stained following a standard procedure with anti-human CD3 (APC/Cy7, clone HIT3a), anti-human CD4 (PerCP/Cy5.5, clone OKT4), anti-human CD8a (Brilliant Violet 510, clone RPA-T8), anti-human CD19 (PE/Cy7, clone HIB19), anti-human CD23 (FITC, clone EBVCS-5), anti-human CD27 (PE, clone M-T271), anti-human CD138 (APC, clone DL-101) and anti-human IgM (Brilliant Violet, clone MHM-88). All antibodies were purchased from BioLegend (San Diego, California, United States of America). A total of 100,000 lymphocytes/sample were acquired on a FACS Canto II (BD Biosciences). All post acquisition analysis was done with FlowJo Software v10 (Tree Star Inc.) and the frequencies of the parent populations determined (Fig. 1). The assessed phenotypes (Fig. 1 showing the gating strategy using an treated TB case) were defined as follows: (1) Mature B cells (CD19+IgM+), (2) Activated B cells (CD19+IgM+CD23+), (3) Naïve B cells (CD19+IgM+CD23+CD27+), (4) Circulating Marginal Zone (MZ) B cells (CD19+IgM+CD23−CD27+), (5) Memory B cells (CD19+IgM+CD27+), (6) Plasmablasts with memory phenotype B cells (CD19+IgM+CD27++) (7) Total plasma cells (CD19+IgM+CD138+), (8) Plasmablasts cells (CD19+IgM+CD27+CD138+) and (9) Plasmablasts with memory phenotype B cells (CD19+IgM+CD138+CD27++). All IgM+ phenotypes are referred to as non-class switched (NCS) and IgM− phenotypes as class switched (CS) in text.
Statistical analysis
Differences in the frequency of B cell subsets between the groups were analysed using the non-parametric analysis with a Mann-Whitney correction and performed by Dr Justin Harvey (Stellenbosch University). All analysis were performed with the Statistica 12 software (Statsoft, Ohio, USA).
Results and discussion
Circulating marginal zone B cells and memory phenotypes distinguish between TB diagnosis and end of treatment
We firstly aimed to identify phenotypes that were significantly different at diagnosis and the end of treatment (week 24). In Fig. 2 it is seen that the CD27high memory B cells (CD19+IgM+CD27++), p = 0.02880, and plasmablasts B cells (CD19+IgM+CD138+CD27+), p = 0.00389, populations were significantly higher at diagnosis as when compared to levels at the end of treatment. Sebina et al. [18] observed that UK donors who previously lived in, or visited areas denoted as highly TB-endemic had higher frequencies of memory B cells in their peripheral blood as compared to their counterparts who have not. This study also reported that BCG elicited the production of long-lived mycobacteria-specific memory B cells [18], which supports the notion of high observed frequencies of memory B cells at diagnosis as BCG vaccination is a common practice at birth in South Africa. It has been shown that the maintenance of memory B cells are dependent on the presence of antigen, and that they are lost within 10–12 weeks following its absence [19]. Although this is opposite to other publications stating the longevity of B cells [18, 20–22], it corresponds to the observed result of lower memory B cell frequencies at the end of treatment. The high numbers of TB-specific (or BCG-specific, or mycobacteria-specific) memory B cells might be maintained in this population due to the continual exposure to antigen (either M.tb exposure in this high prevalence setting, or environmental or non-tuberculous mycobacterial exposure). It is reasonable that the decrease of memory B cells towards the end of treatment don’t relate to a complete loss of memory B cells, but rather represents an overall decrease in line with the reduction of bacterial burden. Figure 3 shows that memory based B cell phenotypes were significant in the CS cohort as well with memory B cells (CD19+IgM−CD27+); p = 0.01398, plasmablasts B cells (CD19+IgM−CD138+CD27+); p = 0.00968 and plasmablasts with memory phenotype a (CD19+IgM−CD138+CD27++); p = 0.03616. This continual significance in both NCS and CS phenotypes strengthens their importance as distinguishing factors. Circulating Marginal zone B cells (CD19+CD27+CD23−) were also significant in both NCS (p = 0.04680) and CS (p = 0.02138) analyses and between groups over time (Fig. 4). Together these results warrants further research into these phenotypes as potential biomarkers for treatment response.
Circulating marginal zone- and Mature B cells can distinguish TB from other-lung diseases at diagnosis
In the attempt to identify phenotypes that were unique to tuberculosis when compared to other-lung based diseases, two results showed to be significant. The first was NCS marginal zone (MZ) B cells (CD19+IgM+CD27+CD23−) with p = 0.02092 and secondly CS mature B cells were significant with p = 0.00026 (Fig. 4). With both of these phenotypes significantly lower in peripheral circulation during active TB disease (especially the CS mature B cells), it raises the question whether TB actively suppresses the B cell repertoire during disease. The NCS mature B cell repertoire does not recover to baseline levels during the first week of treatment as one would expect (in line with chemotherapeutic treatment alleviating bacterial burden). These findings support the notion that there is a possible underlying mechanism exploited by Mtb that could be crucial to the management of the infection as both MZ and mature B cells are implicated in effector functions of the adaptive immune system, as seen with the overexpression of programmed death 1 (PD-1) on lymphocyte frequencies during active TB infection [23].
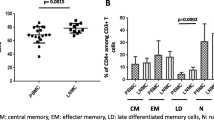
Class switched and non-class switched mature B cells distinguish between tuberculosis, other-lung based diseases and healthy controls
Class switched mature B cells from participants with active TB are present in significantly different levels when compared to other-lung diseases (p = 0.043711) and the healthy control group (p = 0.024488) (Fig. 5). Mature B cells were not only able to distinguish between these groups in the class switched category, but also in the non-class switched category where the difference between TB and OLD was highly significant (p = 0.000016) and between TB and the healthy control group where p = 0.025939 (not shown)). An interesting observation is that the class switched mature B cells from TB is present at higher frequencies when compared to the OLD group (Fig. 5), but that the inverse is observed with non-class switched mature B cells where they are present in significantly lower levels when compared to the OLD group (not shown). This would suggest that a strong preference is displayed towards class switched mature B cells during active tuberculosis. The differences present in the CS and NCS mature B cells are consistent when compared during the first week of treatment (not shown), where the NCS mature B cells are present in higher frequencies as when compared to the class switched mature B cells. Further in this study, NCS activated B cells in TB could distinguish from OLD (p = 0.008391), but not from healthy controls (p = 0.122877) (Fig. 6). This result identifies another combination of markers that could be used to distinguish TB from other lung based diseases and should be further investigated as a measure in the early diagnosis of TB.
IgM+ Activated B cells are significantly different at diagnosis when compared to other disease states. An alpha level of 95 % was used in the LSD test, whose results is displayed in the accompanying table. P- Values show significance between specific comparisons. TB = tuberculosis, OLD = other-lung disease, HC = healthy control
Conclusion
This pilot study identified unique variations in the B cell repertoire during active tuberculosis infection when compared to healthy controls, other-lung based diseases and over the course of TB treatment. The first observation of memory-based phenotypes being the major distinguishers between diagnosis and end of treatment in both class switched and non-class switched phenotypes holds promise as markers for treatment response. The second important finding of this study is that circulating marginal zone B cells could not only distinguish between TB diagnosis and the end of treatment, but also has significantly different frequencies when compared to other-lung based diseases making it a candidate as biomarker for not only treatment response, but distinguishing active TB disease from other-lung based diseases. The observation that NCS and CS mature B cells could best distinguish between TB and the two control groups (healthy controls and other lung diseases) at diagnosis, but that their respective peripheral frequencies are present at an inverse level. Taken together, these results show that mainly B cell phenotypes implicated in activation and subsequent effector functions are influenced by TB and warrants further research to confirm their potential as biomarkers for TB disease and treatment response. These results are further strengthened if the assumption holds that only 10 % of the ongoing immunologic response is represented in the peripheral blood when compared to the site of disease, namely the lungs. Further studies is thus needed to replicate this experiment on broncho-alveolar lavage (BAL) fluid from active TB diseased participants and other lung diseases to ascertain if the phenotype remains the same. Although the results from the BAL fluid experiment might give a better representation of the on-site B cell frequencies, the challenges associated with obtaining the bio fluid and characterisation of the (mostly activated) cells could hamper the process of finding biomarkers of disease or TB treatment response.
Abbreviations
BAL, broncho alveolar lavage; COPD, chronic obstructive pulmonary disease; CS, class switched; IFN, interferon; M.tb, mycobacterium tuberculosis; NCS, non class switched; OLD, other lung diseases; PD-1, programmed death 1; TB, tuberculosis; TLR, toll like receptor
References
WHO. Global Tuberculosis Report 2014 [Internet]. World Health Organization. 2014. Available from: http://reliefweb.int/report/world/global-tuberculosis-report-2014. Accessed 25 July 2016.
Harris DP, Haynes L, Sayles PC, Duso DK, Eaton SM, Lepak NM, et al. Reciprocal regulation of polarized cytokine production by effector B and T cells. Nat Immunol. 2000;1(6):475–82.
Lampropoulou V, Hoehlig K, Roch T, Neves P, Calderón Gómez E, Sweenie CH, et al. TLR-activated B cells suppress T cell-mediated autoimmunity. J Immunol Baltim Md 1950. 2008;180(7):4763–73.
Hoehlig K, Lampropoulou V, Roch T, Neves P, Calderon-Gomez E, Anderton SM, et al. Immune regulation by B cells and antibodies a view towards the clinic. Adv Immunol. 2008;98:1–38.
Neves P, Lampropoulou V, Calderon-Gomez E, Roch T, Stervbo U, Shen P, et al. Signaling via the MyD88 adaptor protein in B cells suppresses protective immunity during Salmonella typhimurium infection. Immunity. 2010;33(5):777–90.
du Plessis WJ, Kleynhans L, du Plessis N, Stanley K, Malherbe ST, Maasdorp E, et al. The functional response of B Cells to antigenic stimulation: a preliminary report of latent tuberculosis. PLoS One. 2016;11(4):e0152710.
Hernandez J, Velazquez C, Valenzuela O, Robles-Zepeda R, Ruiz-Bustos E, Navarro M, et al. Low number of peripheral blood B lymphocytes in patients with pulmonary tuberculosis. Immunol Invest. 2010;39(3):197–205.
Wu YE, Zhang SW, Peng WG, Li KS, Li K, Jiang JK, et al. Changes in lymphocyte subsets in the peripheral blood of patients with active pulmonary tuberculosis. J Int Med Res. 2009;37(6):1742–9.
Hrušák O, Basso G, Ratei R, Gaipa G, Luria D, Mejstříková E, et al. Flow diagnostics essential code: a simple and brief format for the summary of leukemia phenotyping. Cytometry B Clin Cytom. 2014;86(4):288–91.
Orfao A, Schmitz G, Brando B, Ruiz-Arguelles A, Basso G, Braylan R, et al. Clinically useful information provided by the flow cytometric immunophenotyping of hematological malignancies: current status and future directions. Clin Chem. 1999;45(10):1708–17.
Subasic D, Karamehic J, Delic-Sarac M, Kasumovic M, Mekic M, Eminovic I, et al. Monitoring of disease biomarkers activity and immunophenotyping as important factors in SLE clinical management. Med Arch Sarajevo Bosnia Herzeg. 2012;66(5):336–9.
Boldt A, Borte S, Fricke S, Kentouche K, Emmrich F, Borte M, et al. Eight-color immunophenotyping of T-, B-, and NK-cell subpopulations for characterization of chronic immunodeficiencies. Cytom Part B - Clin Cytom. 2014;206(January):191–206.
Abreu MT, Carvalheiro H, Rodrigues-Sousa T, Domingos A, Segorbe-Luis A, Rodrigues-Santos P, Souto-Carneiro MM. Alterations in the peripheral blood B cell subpopulations of multidrug-resistant tuberculosis patients. Clin Exp Med. 2014;14(4):423-9. doi:10.1007/s10238-013-0258-1. Epub 2013 Sep 26. PubMed PMID: 24068613.
Barcelos W, Martins-Filho OA, Guimarães TMPD, Oliveira MHP, Spíndola-de-Miranda S, Carvalho BN, et al. Peripheral blood mononuclear cells immunophenotyping in pulmonary tuberculosis patients before and after treatment. Microbiol Immunol. 2006;50(8):597–605.
Partnership A, Metropole C. TB control in Cape Town - progress report 1997–2003. 2003.
Classen CN, Warren R, Richardson M, Hauman JH, Gie RP, Ellis JHP, et al. Impact of social interactions in the community on the transmission of tuberculosis in a high incidence area. Thorax. 1999;54(2):136–40.
Verver S, Warren RM, Munch Z, Vynnycky E, van Helden PD, Richardson M, et al. Transmission of tuberculosis in a high incidence urban community in South Africa. Int J Epidemiol. 2004;33(2):351–7.
Sebina I, Cliff JM, Smith SG, Nogaro S, Webb EL, Riley EM, et al. Long-lived memory B-cell responses following BCG vaccination. PLoS One. 2012;7(12):e51381.
Gray D, Skarvall H. B-cell memory is short-lived in the absence of antigen. Nature. 1988;336(6194):70–3.
Wipasa J, Suphavilai C, Okell LC, Cook J, Corran PH, Thaikla K, et al. Long-lived antibody and B Cell memory responses to the human malaria parasites, Plasmodium falciparum and Plasmodium vivax. PLoS Pathog. 2010;6(2):e1000770.
Ward SM, Phalora P, Bradshaw D, Leyendeckers H, Klenerman P. Direct ex vivo evaluation of long-lived protective antiviral memory B cell responses against hepatitis B virus. J Infect Dis. 2008;198(6):813–7.
Schittek B, Rajewsky K. Maintenance of B-cell memory by long-lived cells generated from proliferating precursors. Nature. 1990;346(6286):749–51.
Singh A, Mohan A, Dey AB, Mitra DK. Inhibiting the programmed death 1 pathway rescues Mycobacterium tuberculosis-specific interferon γ-producing T cells from apoptosis in patients with pulmonary tuberculosis. J Infect Dis. 2013;208(4):603–15.
Acknowledgements
Special thank you to all the study participants and field staff of the Immunology Research Group (SUNIRG).
Funding
The financial assistance of the National Research Foundation (NRF) towards the research project of WJ du Plessis is hereby acknowledged. Opinions expressed and conclusions arrived at, are those of the authors and are not to be attributed to the NRF.
Availability of data and materials
All the data are presented in the manuscript. A spreadsheet of the data is attached as supporting document.
Authors’ contributions
WJdP carried out the laboratory experiments. AK performed the flow cytometric analysis. AGL and GW planned the study. WJdP and AGL drafted the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
All participants gave written informed consent for partaking in the study after being briefed about the study’s aims and goals. The participants were also required to have their HIV status tested or declared to field workers. Samples were collected from two TB treatment studies. Ethical approval was obtained for both of these studies from the Health Research Ethics Committee of Stellenbosch University with ethics reference #: N10/01/013 and N13/05/064.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
du Plessis, W.J., Keyser, A., Walzl, G. et al. Phenotypic analysis of peripheral B cell populations during Mycobacterium tuberculosis infection and disease. J Inflamm 13, 23 (2016). https://doi.org/10.1186/s12950-016-0133-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12950-016-0133-4