Abstract
Background
Proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors have been shown to improve cardiovascular outcomes when added to conventional statin therapy. This study aims to investigate the efficacy and safety of in-hospital initiation of PCSK9 inhibitors among patients with acute myocardial infarction (AMI) based on real-world experience.
Methods and results
Data were collected from the Biobank of the First Affiliated Hospital of Xi’an Jiaotong University between January 2016 and December 2020. A total of 7556 AMI patients were screened for eligibility. Propensity Score Match (PSM) was employed, and covariates were age, sex, admission blood pressure and lipid profiles.
Eligible participants were (1) propensity-matched 1:2:2 of statin plus evolocumab (dual therapy) vs. statin vs. statin plus ezetimibe. Ninety-five statin plus evolocumab users achieved significantly decreased low density lipoprotein (LDL) levels (0.92 ± 0.62 mmol/L in the 1st month and 1.17 ± 0.73 in the 3rd month) and a promising attainment rate of LDL (79.5% in the 1st month and 80.0% in the 3rd month) compared to the other two groups. (2) Propensity-matched 1:2:2 of statin plus ezetimibe evolocumab (triple therapy) vs. statin vs. statin plus ezetimibe. Similarly, 75 triple medication users achieved significantly decreased LDL levels and a promising attainment rate of LDL compared to the other two groups. In-hospital mortality and readmission rates within 3 months were then analyzed, and a decreased readmission rate was observed with PCSK9i therapy.
Conclusions
Based on the present single-center real-world PSM-adjusted study, PCSK9i has been effective in short-term lipid control among AMI patients. The long-term effectiveness for reducing major cardiovascular events among AMI patients based on real-world experience remains to be explored.
Trial registration
The study was registered at ClinicalTrials.gov, ClinicalTrials.gov ID: NCT05184530
Graphical Abstract

Similar content being viewed by others
Introduction
The advent of the Proprotein Convertase Subtilisin-Kexin Type 9 (PCSK9) has brought a breakthrough in the treatment of atherosclerotic disease. PCSK9 is a secreted serine protease synthesized by the liver that can bind to and degrade LDL receptors, thereby reducing the clearance of serum LDL [1]. Previous clinical studies have shown that patients with atherosclerotic disease still have poor LDL-C level control under conventional statin and ezetimibe treatment. The recommended LDL target values for ASCVD patients tend to be lower and lower; currently, for patients at very high risk, an LDL reduction of ≥50% from baseline and an LDL goal of < 1.4 mmol/L (< 55 mg/dL) are suggested [2, 3]. A growing number of clinical studies of PCSK9i have proven that high-risk atherosclerosis patients can achieve satisfactory blood lipid (especially LDL-C) control by combining PCSK9i on the basis of statin treatment, thus further reducing the risk of myocardial infarction, stroke and other events [4,5,6].
According to contemporary guidelines [7, 8], PCSKi should be initiated when the initiation of statin and ezetimibe has not met the targeted LDL-C levels. However, few studies have focused on the effectiveness, safety and cardiovascular benefits of PCSK9i on LDL-C management when initiated during the acute phase of cardiovascular events. In the latest Chinese consensus on dyslipidemia management in patients with high-risk atherosclerosis disease [9], it is recommended that individualized lipid-lowering therapy should be selected according to the patient’s baseline LDL-C level and the expected reduction range of the lipid-lowering regime. As a result, some AMI patients with high baseline LDL-C levels might opt to receive the combined treatment of statins and PCSK9i in the early stage of AMI onset. However, clinical evidence for the efficacy and safety of this treatment regimen that combined PCSKi and statins could be initiated during the acute phase of AMI for high-risk patients with high baseline LDL-C levels based on real-world experience is still limited.
Therefore, this study aims to investigate the efficacy and safety of in-hospital initiation of PCSK9i in patients with AMI based on real-world experience. Through this single-center real-world study, in-hospital initiation of PCSK9i was shown to be effective in short-term lipid control among AMI patients. The long-term effectiveness for reducing major cardiovascular events remains to be explored.
Methods
Study design and clinical data collection
This was a single-center, retrospective cohort study. A total of 7556 consecutive patients admitted to the cardiology department of the First Affiliated Hospital of Xi’an Jiaotong University for AMI between January 2016 and December 2020 were enrolled. The inclusion criteria were confirmed admission diagnosis of AMI and were defined based on the universal definition criteria by the American Cardiology College [10]. The exclusion criteria were as follows: (1) severe noncardiac disease with an expected survival of less than 1 year and unwillingness to participate; (2) patients over the age of 80 years or living far away from the hospital’s catchment area. A patient could only be included once. In hospitals, PCSK9i was initiated according to the Chinese consensus on dyslipidemia management in patients with high-risk atherosclerosis disease [9].
The medical records of the patients were collected from the Biobank of the First Affiliated Hospital of Xi’an Jiaotong University, which contains the identified data derived from raw medical records, information about patients’ detailed medical histories, present medication, and biochemical and echocardiography results. Follow-up information, including in-hospital mortality, readmission rate and short-term lipid profile alterations, was obtained via biobanks, telephones and questionnaires by the general practitioner (GP). Written informed consent was obtained from all study participants, with ethics committee approval at the First Affiliated Hospital of Xi’an Jiaotong University. The study was registered at ClinicalTrials.gov, ClinicalTrials.gov ID: NCT05184530.
Study cohorts and treatments
Participants were allocated into four groups according to different lipid-lowering strategies: 1). Statin, 2). Statin plus ezetimibe, 3). Statin plus evolocumab and 4). Statin plus ezetimibe plus evolocumab, contingent on whether they began evolocumab during hospitalization. Patients were initiated with evolocumab (140 mg per 2 weeks, subcutaneous injection) during hospitalization either due to extremely high LDL levels and/or large area myocardial infarction based on the Chinese consensus on dyslipidemia management in patients with high-risk atherosclerosis disease [9]. The use of statin (20 mg atorvastatin or 10 mg rosuvastatin per day) or statin plus ezetimibe (10 mg per day) therapy was based on the present guidelines for the treatment of AMI [11].
Propensity score match
Because patients received statin, ezetimibe and evolocumab according to their admission LDL levels and varied greatly in baseline characteristics, propensity score matching (PSM) was employed, and covariates were age, sex, admission blood pressure and lipid profiles. All eligible participants were (1) propensity-matched 1:2:2 of statin plus evolocumab vs. statin vs. statin plus ezetimibe and (2) propensity-matched 1:2:2 of statin plus ezetimibe evolocumab vs. statin vs. statin plus ezetimibe. The propensity score was determined by R 3.6.0 and the package MatchIt and calculated using the values of the covariates.
Statistical analyses
All statistical analyses were performed by using SPSS for Mac 22.0 (SPSS Inc., Chicago, IL), GraphPad 9.0 Prism (GraphPad Software San Diego, CA) or R 3.6.0. Data are presented as frequencies or percentages for categorical variables and the mean ± SD for continuous variables, unless otherwise indicated. A simple t test was used to compare continuous variables that were normally distributed. The Mann–Whitney U test was used to compare continuous variables that did not conform to a normal distribution. The χ2 test was used to compare categorical variables. One-way ANOVA was used to compare continuous variables of three or more independent (unrelated) groups. A value of P < 0.05 was considered statistically significant.
Results
Study cohort
A total of 7556 AMI patients from the biobank database between January 2016 and December 2020 were screened for eligibility. After excluding those without revascularization or statin-based therapy, the remaining 5802 statin users, 801 statin plus ezetimibe users and 170 statin plus evolocumab users (including 95 users without and 75 users with ezetimibe) were selected for this study. Then, 1− and 3-month follow-up data were collected and analyzed, including in-hospital mortality, readmission rate and lipid profiles (Fig. 1).
As admission LDL level and crowd size vary among different lipid-lowering strategy groups, propensity score matching (PSM) was performed for further analysis. First, PSM was based on statin plus evolocumab therapy, and of these, 95 users were successfully matched with 190 statin users and 190 statin plus ezetimibe users. Second PSM was based on statin plus ezetimibe plus evolocumab (triple) therapy, and of these, 75 users were successfully matched with 150 statin users and 150 statin plus ezetimibe users. The matched groups were well balanced in terms of demographic and clinical characteristics (Appendix Tables 1 and 2, Appendix Figs. 1 and 2).
Baseline characteristics and short-term follow-up in the whole cohort
In the whole cohort, the mean ages were 62.90 ± 11.91, 58.73 ± 12.16, 57.72 ± 11.07 and 54.38 ± 11.77 years among the statin, statin plus ezetimibe, statin plus evolocumab and triple therapy groups. The admission LDL levels were 2.25 ± 0.74, 2.95 ± 1.03, 3.24 ± 0.98 and 3.90 ± 1.45 mmol/L, respectively (Table 1), which is also inconsistent with the basic strategy that higher LDL levels require intensive lipid-lowering therapy in AMI patients. According to 2019 ESC/EAS Guidelines for the management of dyslipidemias [2], for patients at very high cardiovascular risk, LDL reduction of ≥50% from baseline and an LDL goal of < 1.4 mmol/L (< 55 mg/dL) are recommended. We further analyzed the control situation of LDL (< 1.4 mmol/L) among each group. On admission, the target rate was 11.8, 4.0, 3.2 and 1.3% among each group. In the 1-month follow-up, approximately 37.0, 28.8, 79.5 and 55.3% of all patients reached the treatment goal among each group, and after 3 months, 40.6, 29.3, 80.0 and 43.8% of all patients reached the treatment goal, respectively (Table 1). Despite higher LDL levels at admission, AMI patients achieved a promising control rate in short-term PCSK9i treatment Fig. 2.
LDL level and compliance rate on admission and short-term follow-up among different lipid-lowering strategies in AMI patients. A. LDL level and compliance rate among different lipid-lowering strategies on admission and at the 1- and 3-month follow-ups. Each point represents one AMI patient’s lipid data. B LDL alterations among different lipid-lowering strategies on admission and at the 1st and 3rd month follow-ups. Data are shown as the mean ± SEM LDL Target Level = 1.4 mmol/L
Approximately 1.9% of AMI patients died with statin alone therapy, and 0.7, 0.8, and 0.0% died among the statin plus ezetimibe, evolocumab dual and triple groups, respectively, during the 3-month follow-up. The readmission rates were 4.0 and 5.3% with PCSK9i treatment and more than 10%, approximately 10.4% in statin users and 14.7% in statin plus ezetimibe users, respectively.
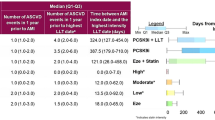
Statin plus evolocumab therapy (dual therapy)-based PSM analysis
Ninety-five statin plus evolocumab users, 190 statin users and 190 statin plus ezetimibe users were well matched for this PSM analysis. The mean age was 59.42 ± 11.66, 58.62 ± 12.73 and 58.53 ± 10.63 among each group, and the admission LDL was 3.11 ± 1.02, 3.24 ± 1.13, and 3.24 ± 0.98 mmol/L, respectively, after PSM adjustments.
On admission, 0.5, 2.1 and 3.2% of AMI patients reached target LDL levels among the statin, statin plus ezetimibe, and statin plus evolocumab groups, respectively. At the 1-month follow-up, the target rates were 31.0, 21.3, and 79.5% and 29.4, 21.4, and 80.0% after 3 months, respectively (Fig. 3A). The mean LDL level was significantly decreased in statin plus evolocumab users compared to the other two groups, with 0.92 ± 0.62, 1.58 ± 0.44, and 1.96 ± 0.82 mmol/L in the 1st month and 1.17 ± 0.73, 1.61 ± 0.49, and 2.10 ± 0.82 months in the 3rd month. (Table 2 and Fig. 3.B). Additionally, a similar trend was observed in the ApoB level, with 0.39 ± 0.20, 0.64 ± 0.16, and 0.70 ± 0.22 g/L in the 1st month and 0.46 ± 0.20, 0.59 ± 0.15, and 0.75 ± 0.22 g/L in the 3rd month follow-up, respectively. Approximately 4.0% of AMI patients were rehospitalized with statin plus evolocumab therapy, and 11.6 and 10.5% readmission rates were observed in the other two groups during the short-term follow-up.
Lipid profile alterations and short-term follow-up among statin plus evolocumab/statin/statin plus ezetimibe lipid-lowering strategies in AMI patients after PSM adjustment. A LDL level and compliance rate among different lipid-lowering strategies on admission and at the 1- and 3-month follow-ups. Each point represents one AMI patient’s lipid data after PSM adjustment. LDL (B) and ApoB (C) alterations among different lipid-lowering strategies on admission and at the 1- and 3-month follow-ups. Data are shown as the mean ± SEM. D Readmission rate among each group. Ninety-five statin plus evolocumab users, 190 statin plus ezetimibe users and 190 statin users were chosen after 1:2:2 propensity score matching. For statistical analysis, one-way ANOVA followed by Sidak’s multiple comparison test was applied, * P < 0.05, ***P < 0.001
Statin plus ezetimibe plus evolocumab therapy (triple therapy)-based PSM analysis
In the 7556 AMI patients, 75 patients received triple therapy (statin plus ezetimibe plus evolocumab) and were well matched with 150 statin users and 150 statin plus ezetimibe users. The mean age was 52.59 ± 11.92, 53.57 ± 11.29 and 53.67 ± 11.86 among the groups, and the admission LDL levels were 3.59 ± 0.95, 3.82 ± 1.20, and 3.90 ± 1.45 mmol/L, respectively, after PSM adjustments.
Approximately 1.3, 0 and 1.3% of AMI patients reached target LDL levels among the statin, statin plus ezetimibe, and triple therapy groups during admission. At the 1-month follow-up, the achieved rates were 10.7, 28.6, and 55.3% and 0.0, 17.9, and 43.8% after 3 months, respectively (Fig. 4A). Additionally, the mean LDL level was significantly decreased in triple therapy patients compared to the other two groups, with 1.43 ± 1.06, 1.96 ± 0.49, and 2.04 ± 0.81 mmol/L in the 1st month and 1.40 ± 0.50, 2.06 ± 0.42, and 2.37 ± 1.13 mmol/L after the 3-month follow-up (Table 3 and Fig. 4.B). Additionally, a similar decrease was observed in ApoB levels, and triple medication users reached 0.59 ± 0.29 0.61 ± 0.20 g/L in the 1st month and 3rd month, compared to 0.75 ± 0.17 and 0.80 ± 0.13 g/L in the statin group and 0.76 ± 0.20 and 0.83 ± 0.29 g/L in the statin plus ezetimibe group. A total of 5.3% of AMI patients were rehospitalized with triple therapy, which was 6.7 and 6.0% lower than those in statin and statin plus ezetimibe users, respectively.
Lipid profile alterations and short-term follow-up among statin plus ezetimibe plus evolocumab/statin/statin plus ezetimibe lipid-lowering strategies in AMI patients after PSM adjustment. A LDL level and compliance rate among different lipid-lowering strategies on admission and at the 1- and 3-month follow-ups. Each point represents one AMI patient’s lipid data after PSM adjustment. LDL (B) and ApoB (C) alterations among different lipid-lowering strategies on admission and at the 1- and 3-month follow-ups. Data are shown as the mean ± SEM. D Readmission rate among each group. Seventy-five statin plus ezetimibe plus evolocumab users, 150 statin plus ezetimibe users and 150 statin users were chosen after 1:2:2 propensity score matching. For statistical analysis, one-way ANOVA followed by Sidak’s multiple comparison test was applied, * P < 0.05, ** P < 0.01, *** P < 0.001
Discussion
In this single-center, retrospective, population-based study, we found that in-hospital initiation of PCSK9 was effective in short-term lipid control among AMI patients. In both the PCSK9i plus statin therapy with or without ezetimibe cohort, the mean LDL levels decreased by more than 60%. In addition, more than 50% of patients in the above two groups reached the target LDL-C level after 1 month of treatment. PCSK9i plus statin therapy with or without ezetimibe exhibits a better lipid-lowering effect than statin or statin plus ezetimibe therapy.
Previously, PCSK9 inhibitors have been shown to reduce major cardiovascular events in secondary prevention and improve adherence and quality of life in high-risk patients with coronary artery disease [12, 13]. The EVOPACS study confirmed that compared with a high-intensity statin alone, the very early application of evolocumab brings a very significant reduction in LDL-C levels in ACS patients [14]. Additionally, the ODYSSEY study demonstrated that alirocumab added to intensive statin therapy reduced the occurrence of both Type 1 and Type 2 MI among patients after a recent ACS [15]. To the best of our knowledge, our study is the first to investigate lipid profile alterations as well as the short-term outcomes of PCSK9i initiated together with statins among AMI patients, focusing on real-world evidence. Similar to the EVOPACS study [14], our results show that LDL is significantly decreased via PCSK9i treatment after 1-month and 3-month follow-up when added to either statin or statin plus ezetimibe therapy. It is also noteworthy that ApoB, the primary apolipoprotein of LDL particles, exhibited the same trend as LDL among each treatment group, further proving the efficiency of PCSK9i in the lipid-lowering strategy.
In addition, our study shows a decreased readmission rate in the short-term follow-up via PCSK9i therapy. Mechanistically, previous studies have proven that after adjusting for ACSVD risk factors (including LDL level), serum PCSK9 levels were linearly associated with the fraction and amount of necrotic core tissue in coronary atherosclerosis [16]. Compared with healthy volunteers, a significantly higher concentration of PCSK9 was observed in patients with ACS [17]. Additionally, increased PCSK9 levels were associated with higher platelet reactivity and might be a possible predictor of ischemic events in ACS patients undergoing PCI [18]. Taken together, based on a 3-month follow-up, our results have provided further clinical benefits that PCSK9i might exert lasting cardiovascular benefits on AMI patients apart from lipid control. Long-term follow-up data are warranted to further validate the efficacy of the in-hospital initiation of PCSK9i [19].
Notably, in terms of lipid-lowering effects, we found that triple therapy with PCSK9i, statin and ezetimibe was not superior to statin plus evolocumab treatment before PSM adjustment. Several potential mechanisms may account for this phenomenon. First, most patients with triple treatment have extremely high LDL levels on admission, which was even 20% higher than that of the dual therapy group. Second, different lipid-lowering mechanisms also influence the effect. Ezetimibe inhibits the absorption of cholesterol from the small intestine and decreases the amount of cholesterol normally available to liver cells; the lower levels of cholesterol in the liver cells lead them to absorb more cholesterol from circulation and thus “indirectly” lower the levels of circulating cholesterol. On the other hand, evolocumab inhibits PCSK9 from binding to LDL receptors on the liver surface, and there are more LDL receptors on the surface of liver cells to remove LDL-C from the blood directly. Finally, limited therapy users were included in this study, and reduced compliance may also affect the results.
Via a 3-month follow-up, the strength of our study is to demonstrate that PCSK9i based therapy exhibits a better lipid-lowering effect, as well as a further clinical benefit on AMI patients apart from lipid control. However, there are several limitations in the current work. First, this study is limited in its single-center, retrospective and observational nature. Future multicenter studies based on longer follow-up are needed. Additionally, although the dosage and frequency of statins (20 mg atorvastatin or 10 mg rosuvastatin per day) are fixed, the data on whether statin therapy was started during or before hospital admission and whether statins were not allowed due to their side effects are inaccessible so that it is not possible to match this situation in the four groups. However, the initiation, dosage and frequency of evolocumab were fixed among all the groups in this study. Third, as alirocumab was not prescribed in this study, the results may not apply to patients on alirocumab treatment.
Conclusions
In conclusion, through this retrospective, PSM-adjusted cohort study, we have further proved the efficiency and safety outcomes of PCSK9i during the short-term follow-up based on real-world analysis among AMI patients. The long-term effectiveness, as well as the specific mechanism of PCSK9i for reducing major cardiovascular events, remain to be explored.
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Seidah NG, Awan Z, Chretien M, Mbikay M. PCSK9: a key modulator of cardiovascular health. Circ Res. 2014;114:1022–36.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2019;2020(41):111–88.
Cannon CP, de Lemos JA, Rosenson RS, Ballantyne CM, Liu Y, Gao Q, et al. Use of lipid-lowering therapies over 2 years in GOULD, a registry of patients with atherosclerotic cardiovascular disease in the US. JAMA Cardiol. 2021;6(9):1–9.
Santos RD, Ruzza A, Hovingh GK, Wiegman A, Mach F, Kurtz CE, et al. Evolocumab in pediatric heterozygous familial hypercholesterolemia. N Engl J Med. 2020;383:1317–27.
Burnett JR, Hooper AJ. PCSK9 - a journey to cardiovascular outcomes. N Engl J Med. 2018;379:2161–2.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Committees OO and Investigators. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379:2097–107.
Raygor V, Khera A. New recommendations and revised concepts in recent guidelines on the Management of Dyslipidemias to prevent cardiovascular disease: the 2018 ACC/AHA and 2019 ESC/EAS guidelines. Curr Cardiol Rep. 2020;22:87.
Dykun I, Mahabadi AA, Rassaf T. A clinical perspective on the 2019 ESC/EAS guidelines for the management of dyslipidaemias: PCSK-9 inhibitors for all? Eur Heart J. 2020;41:2331.
Atherosclerosis, Coronary heart disease working Group of Chinese Society of C and editorial Board of Chinese Journal of C. Chinese expert consensus on lipid management of very high-risk atherosclerotic cardiovascular disease patients. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:280–6.
DeFilippis AP, Chapman AR, Mills NL, de Lemos JA, Arbab-Zadeh A, Newby LK, et al. Assessment and treatment of patients with type 2 myocardial infarction and acute nonischemic myocardial injury. Circulation. 2019;140:1661–78.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2017;2018(39):119–77.
Gragnano F, Natale F, Concilio C, Fimiani F, Cesaro A, Sperlongano S, et al. Adherence to proprotein convertase subtilisin/kexin 9 inhibitors in high cardiovascular risk patients: an Italian single-center experience. J Cardiovasc Med (Hagerstown). 2018;19:75–7.
Cesaro A, Gragnano F, Fimiani F, Moscarella E, Diana V, Pariggiano I, et al. Impact of PCSK9 inhibitors on the quality of life of patients at high cardiovascular risk. Eur J Prev Cardiol. 2020;27:556–8.
Koskinas KC, Windecker S, Pedrazzini G, Mueller C, Cook S, Matter CM, et al. Evolocumab for early reduction of LDL cholesterol levels in patients with acute coronary syndromes (EVOPACS). J Am Coll Cardiol. 2019;74:2452–62.
White HD, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Effects of alirocumab on types of myocardial infarction: insights from the ODYSSEY OUTCOMES trial. Eur Heart J. 2019;40:2801–9.
Cheng JM, Oemrawsingh RM, Garcia-Garcia HM, Boersma E, van Geuns RJ, Serruys PW, et al. PCSK9 in relation to coronary plaque inflammation: results of the ATHEROREMO-IVUS study. Atherosclerosis. 2016;248:117–22.
Burchardt P, Rzezniczak J, Dudziak J, Dzumak A, Marchlewski T, Ganowicz-Kaatz T, et al. Evaluation of plasma PCSK9 concentrations, transcript of LDL receptor, as well as the total number of monocyte LDL receptors in acute coronary syndrome patients. Cardiol J. 2016;23:604–9.
Navarese EP, Kolodziejczak M, Winter MP, Alimohammadi A, Lang IM, Buffon A, et al. Association of PCSK9 with platelet reactivity in patients with acute coronary syndrome treated with prasugrel or ticagrelor: the PCSK9-REACT study. Int J Cardiol. 2017;227:644–9.
Ibrahim NE, Pina IL, Camacho A, Bapat D, Felker GM, Maisel AS, et al. Prospective study of biomarkers SI and ventricular remodeling during Entresto therapy for heart failure study I. sex-based differences in biomarkers, health status, and reverse cardiac remodelling in patients with heart failure with reduced ejection fraction treated with sacubitril/valsartan. Eur J Heart Fail. 2020;22:2018–25.
Acknowledgments
The authors wish to acknowledge the assistance of Biobank from the First Affiliated Hospital of Xi’an Jiaotong University with the data extraction and preparation of the manuscript.
Funding
This study was supported by National Natural Science Foundation of China (No. 81800390, 82170464, 81822005, 81970351, 81941005, 82100477, 92049203), National Key R&D Program of China (2019YFA0802300, 2018YFC1311505), Key Research and Development Program of Shaanxi (No. 2020KW-049, No.2020SF-253, 2021KWZ-25, S2020-YF-GHMS-0014, 2017SF-085, 2020GXLH-Y-015), Central University Basic Science Foundation of China (119132971000056); and the Clinical Research Award of the First Affiliated Hospital of Xi’an Jiaotong University, China (No. XJTU1AF-CRF-2018-025, XJTU1AF-CRF-2017-006).
Author information
Authors and Affiliations
Contributions
JS, BL and ZY participated in the design of the study. JL, BL and HL collected the patients’ data and performed the follow-up. HL, YL and GTJ performed the statistical analysis. YL, HW, YW and CW finished the patients’ follow-up. JS, JL and BL drafted the manuscript. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from all study participants, with ethics committee approval at the First Affiliated Hospital of Xi’an Jiaotong University.
Consent for publication
All authors have reviewed the final version of the manuscript and approved it for publication.
Competing interests
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Fig. S1.
Jitter and hist plots (statin plus evolocumab-based PSM).
Additional file 2: Fig. S2.
Jitter and hist plots (triple therapy-based PSM).
Additional file 3: Table. S1.
Summary of statin plus evolocumab therapy-based PSM.
Additional file 4: Table. S2.
Summary of triple therapy-based PSM.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lou, B., Liu, H., Luo, Y. et al. In-hospital initiation of PCSK9 inhibitor and short-term lipid control in patients with acute myocardial infarction. Lipids Health Dis 21, 105 (2022). https://doi.org/10.1186/s12944-022-01724-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-022-01724-9