Abstract
Background
Elevated monocyte-to-high-density lipoprotein-cholesterol ratio (MHR) is relevant to higher all-cause and cardiovascular mortality in patients with coronary artery disease and other comorbidities. However, the predictive values of MHR for mortality in the general population have been underutilized. This study investigated the association of MHR with all-cause and cardiovascular mortality in the adult population of the United States.
Methods
This study included 34,335 participants (≥20 years) from the National Health and Nutrition Examination Survey 1999–2014 that were grouped according to MHR tertiles. Kaplan-Meier plots and long-rank tests were employed to investigate differences in survival among the groups. Moreover, the relationship of MHR with all-cause and cardiovascular mortality was further explored using multivariate Cox regression and restricted cubic spline analysis.
Results
During the average follow-up of 93.5 ± 56 months, 4310 (12.6%) participants died, with 754 (2.2%) deaths attributed to cardiovascular diseases. Kaplan-Meier analysis revealed statistically obvious differences in all-cause and cardiovascular mortality among the MHR tertiles (log-rank test: all P < 0.001). In multi-adjusted models, participants in the highest tertile of MHR had an increased risk of all-cause (hazard ratio [HR] = 1.19, 95% confidence interval [CI] 1.10–1.29) and cardiovascular mortality (HR = 1.44, 95% CI 1.17–1.77), compared to those in the lowest tertile. Furthermore, the restricted cubic spline curve indicated that MHR had a non-linear association with all-cause mortality (P < 0.001), and the inflection point of MHR was 0.006. Each 2-fold change in MHR exhibited a 32% decrease (HR = 0.68, 95%CI 0.58–0.82) and a 20% increase (HR = 1.20, 95%CI 1.13–1.27) in the risk of all-cause mortality on the left and right flanks of the inflection point, respectively. Additionally, the risk of cardiovascular mortality increased by 21% per 2-fold change in MHR (HR = 1.21, 95%CI 1.07–1.36) in a linear manner.
Conclusions
MHR was significantly related to all-cause and cardiovascular mortality in the general population independent of established risk factors.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the overriding cause of death worldwide, which contributes to a substantial burden on individuals and the society [1]. By 2035, the number of CVD patients is projected to be more than 130 million in the United States (US), and the total cost of CVD-related expenses is estimated to reach 1.1 trillion US dollars [2]. Therefore, efficient mortality prediction tools are essential for timely prevention and effective treatment [3]. Low-density lipoprotein cholesterol (LDL-C) is a well-known prognostic marker for all-cause and CVD mortality [4]. However, some studies found that people with lower LDL-C had an even shorter expectancy compared to those with a high LDL-C value [5]. Thus, more clinical markers are required to accurately identify the risk factors affecting survival.
Monocytes have significant functions in the formation and development of atherosclerotic plaques [6]. Monocytes can produce reactive oxygen species and differentiate into foamy macrophages that can release pro-inflammatory cytokines, driving circulating monocytes to lesion sites, leading to vulnerable atherosclerotic plaques, ultimately resulting in thrombosis and poor clinical outcomes [7, 8]. Epidemiological evidence has shown that monocyte count is associated with all-cause and cardiovascular mortality [8, 9]. In contrast, other researches have demonstrated high-density lipoprotein cholesterol (HDL-C) could suppress atherosclerotic plaque formation and exert anti-inflammatory, antithrombotic, and antioxidant effects on CVD patients [10]. In addition, HDL-C could attenuate and reverse monocyte activation through apoA-I– mediated CD11b inhibition [11].
Monocyte-to-HDL-C ratio (MHR) is a novel and composite predictor that can reflect the balance between the inflammatory and oxidative stress of monocytes and HDL-C. The predictive ability of MHR for clinical outcomes might even be better than independent monocyte count and HDL-C concentration [12]. Kanbay and co-workers first reported that MHR could predict cardiovascular events in individuals with chronic kidney disease [13]. Lots of research were subsequently conducted to evaluate the relations between MHR and prognosis among specific diseases [14,15,16,17,18,19,20], especially acute coronary syndrome (ACS) [12, 21]. Nonetheless, there is no available data concerning the prognostic value of MHR for long-term mortality in the general population to date.
This study aimed to investigate the clinical significance of MHR in predicting all-cause and cardiovascular mortality in the adult US population based on the available data from the National Health and Nutrition Examination Survey (NHANES) 1999–2014.
Methods
Study population
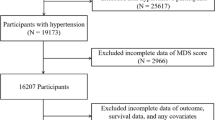
This study population was obtained from the NHANES survey, a continuous program performed by the National Center for Health Statistics (NCHS) with a multistage, complex, probability sampling design to represent the noninstitutionalized civilian population in the US. The protocol was approved by the ethics review board of NCHS research, and all participants provided signed informed consents. The 1999–2014 survey cycles included 82,091 participants in total. Exclusion criteria were as follows: (a) participants aged less than 20 years old (n = 26,053); (b) missing information on monocyte count or high-density lipoprotein cholesterol (n = 21,664); (c) missing mortality information (n = 59). After these exclusions, 34,335 participants were available for the final analysis. The study flowchart is represented in Fig. 1.
Exposure
All blood specimens were withdrawn in the morning after a 9-h fast under established procedures. The Beckman Coulter MAXM provided complete blood counts of the blood specimens. Monocytes were sorted from white blood cells using three simultaneous measurements of laser light scatter, high-frequency conductivity, and individual cell volume. The concentration of HDL-C was measured by direct precipitation or immunoassay [22]. MHR was obtained by dividing monocyte count (103cells/μL) by HDL-C (mg/dL).
Outcomes
Mortality status was ascertained by the NHANES-linked National Death Index record, and detailed information is available on the NCHS data linkage webpage [23]. The outcomes of this study, including all-cause and cardiovascular mortality, were defined referring to the International Classification of Diseases, 10th Revision (ICD-10) [24]. The follow-up time was recorded from the survey participation date until the 31st December 2015.
Covariates
The interview questionnaires provided demographic data, including age, gender, and ethnicity. Drinkers were defined as subjects who consumed at least 12 drinks in the past 12 months, and those smoking more than 100 cigarettes throughout their life were categorized as smokers [25]. The medical comorbidities such as diabetes mellitus (DM), heart failure (HF), hypertension, coronary heart disease (CHD), stroke, and cancer were ascertained by self-reported history in the questionnaires. Body mass index (BMI) was evaluated by body mass (kilograms) and body height (m2). Other covariates including hemoglobin, platelets, LDL-C, triglyceride, albumin, and serum creatinine were obtained from laboratory data. Estimated glomerular filtration rate (eGFR) was measured based on the Modification of Diet in Renal Disease (MDRD) formula [26].
Statistical analysis
Participants of this study were separated into 3 groups according to the tertiles of MHR: low (< 0.009), medium (0.009–0.013), and high (> 0.013) MHR groups. The results for categorical and continuous variables were expressed as frequencies with percentages and means with standard deviations. Chi-squared test and one-way ANOVA were utilized to analyze the differences in categorical or continuous variables among the MHR tertiles. The differential survival rates of all-cause and cardiovascular mortality according to MHR tertiles were determined by Kaplan–Meier plots and log-rank tests. The multivariate Cox regression models with hazard ratios (HRs) and 95% confidence intervals (CIs) were applied to examine the association of MHR with all-cause and cardiovascular mortality. Model 1 was adjusted for none. Model 2 was adjusted for age, gender, ethnicity, smoker, and drinker. Model 3 was further adjusted for DM, hypertension, HF, CHD, stroke, cancer, BMI, hemoglobin, platelets, LDL-C, triglyceride, albumin, and eGFR. Restricted cubic spline (RCS) regression models were applied to explore any non-linear relationship of MHR (per 2-fold change) with all-cause and cardiovascular mortality. Then a two-piecewise Cox regression model was utilized to determine the threshold point if the relationship was non-linear. Sex-stratified models were performed to further investigate the effect of MHR on the risk of death among male and female participants separately. Statistical tests involved the use of Empower(R) (X&Y solutions, Inc., MA, USA) and Stata v14.0 (StataCorp, TX, USA). The statistical significance was present if P-value < 0.05.
Results
Baseline participant characteristics
Table 1 shows the details and comparison of the baseline characteristics. Among the 34,335 participants included in the present study, the average age was 49.6 ± 18.2 years, and 48.4% were male. Across the average follow-up period of 93.5 ± 56 months, 4310 (12.6%) death occurred and 754 (2.2%) participants died of cardiovascular diseases. All baseline covariates had statistically significant differences among MHR groups (all P < 0.05).
Association of MHR with all-cause mortality.
Kaplan-Meier curves among tertiles for all-cause mortality showed worse outcomes as MHR increased (log-rank P < 0.001, Fig. 2A). In the fully adjusted Cox regression model (Table 2), the HRs (95% CI) of all-cause death for participants in the medium and highest tertiles were 1.02 (0.95, 1.11) and 1.19 (1.10, 1.29) compared with participants in the lowest tertile. The association of MHR and all-cause mortality was non-linear and U-shaped based on the RCS model (Fig. 3A), and the test for non-linearity was significant (P < 0.001).
Restricted cubic spline curves of relations between MHR with all-cause (A) and cardiovascular mortality (B). Analysis was adjusted for age, gender, ethnicity, smoker, drinker, DM, hypertension, HF, CHD, stroke, cancer, BMI, hemoglobin, platelets, LDL-C, triglyceride, albumin, and eGFR. The solid and dashed lines symbolize the hazard ratios and corresponding 95% confidence intervals, respectively
Table 3 shows the result of the two-piecewise Cox regression model. Because of skewed distribution, MHR was log2-transformed for fitting the models. The one-line Cox regression model and the two-piecewise regression model were compared, and P-value for the logarithmic likelihood ratio test was < 0.001. The inflection point of MHR was 0.006. Each 2-fold change in MHR exhibited a 32% decrease (HR = 0.68, 95%CI 0.58–0.82) and a 20% increase (HR = 1.20, 95%CI 1.13–1.27) in the risk of all-cause mortality on the left and right flanks of the inflection point, respectively.
Association of MHR with cardiovascular mortality
As displayed in the Kaplan-Meier plot (Fig. 2B), increased MHR value was also related to reduced survival in cardiovascular disease (log-rank P < 0.001). After full adjustment for all covariates (Table 2), compared to individuals in the lowest tertile, the HR and 95% CIs of cardiovascular mortality for those in the medium and highest tertile were 1.28 (1.05, 1.57) and 1.44 (1.17, 1.77), respectively. The RCS curve indicated that MHR was linearly associated with cardiovascular mortality (P for non-linearity = 0.595, Fig. 3B). The risk for cardiovascular mortality increased by a 21% per 1-fold increase in MHR (HR = 1.21, 95%CI 1.07–1.36, Table 3).
Subgroup analysis.
As shown in Table 4, there was a significant interaction between sex and MHR on all-cause and cardiovascular mortality (P for interaction =0.019 and 0.040, respectively). The non-linear relationship between MHR and all-cause mortality persisted in women (P for nonlinearity< 0.001, Fig. 4A) and men (P for nonlinearity = 0.012, Fig. 4C). And a higher MHR was linearly associated with an increased risk of cardiovascular mortality in women (P for nonlinearity = 0.425, Fig. 4B) and men (P for nonlinearity = 0.532, Fig. 4D).
Restricted cubic spline curves of relations between MHR and mortality in different sex groups. (A) Female: all-cause mortality; (B) Female: cardiovascular mortality; (C) Male: all-cause mortality; (D) Male: cardiovascular mortality. Analysis was adjusted for age, ethnicity, smoker, drinker, DM, hypertension, HF, CHD, stroke, cancer, BMI, hemoglobin, platelets, LDL-C, triglyceride, albumin, and eGFR. The solid and dashed lines symbolize the hazard ratios and corresponding 95% confidence intervals, respectively
Discussion
The present study firstly assessed the predictive values of MHR for long-term outcomes in the general population. The results suggested that elevated MHR was remarkably associated with increased susceptibility to cardiovascular mortality while MHR had a non-linear association with all-cause mortality. The lowest risk was found at a threshold value of 0.006. Similar patterns of associations between MHR and the risk of death were found in women and men separately. The association with all-cause mortality was stronger in women, while the association with cardiovascular mortality was stronger in men.
Comparisons with other studies and what does the current work add to the existing knowledge.
Recently, many studies have demonstrated that MHR is a strong index of cardiovascular mortality in individuals with specific diseases, especially coronary artery disease (CAD) [27,28,29]. For instance, Zhang and colleagues found that an increase in MHR was independently related to cardiac mortality in CAD patients after percutaneous coronary intervention [27]. A Turkish study also reported that the highest MHR was related to a 1.8-fold and 1.5-fold risk of in-hospital and long-term cardiovascular mortality, respectively [28]. Additionally, this relationship was confirmed in patients diagnosed with renal insufficiency [18, 30] and type 2 diabetes [19]. However, cardiovascular mortality did not differ between the low-MHR and high-MHR groups in a study of patients commencing dialysis [31]. A large number of patients lost to follow-up might explain the above-unexpected result. Consistent with the above studies, this study investigated a positive relationship between MHR and cardiovascular mortality in the general population. Moreover, this study revealed that each 1-fold increase of MHR led to a 21% increase in the risk of cardiovascular mortality in the quantitative analysis.
The prognostic utility of MHR for short-term and long-term all-cause mortality has been well-established among ACS patients with or without percutaneous coronary intervention by meta-analysis involving relative studies with a follow-up time of up to 60 months [12, 21]. Additionally, the relationship between MHR and all-cause mortality was found to be significant in several specific clinical settings, including transcatheter aortic valve replacement [17], infective endocarditis [16], cerebrovascular disease [14, 20], renal insufficiency [18], type 2 diabetes [19], pulmonary embolism [32], and hepatitis B virus-related decompensated cirrhosis [15]. Nevertheless, some studies did not obtain a significant result [31, 33,34,35]. Herein, the findings of this study showed that a higher MHR was significantly related to increased risk of all-cause mortality in the general population over an average follow-up period of 93.5 months. Furthermore, the RCS model illustrated a nonlinear relation between MHR and all-cause mortality, represented by the U-shaped relationship between HDL-C levels and all-cause mortality [36, 37]. Experimental evidence has found that HDL-C has potentially harmful effects at high concentrations [38]. This adverse effect may be partly attributed to genetic variants, which could lead to the dysfunction of HDL particles [39, 40]. Besides, very high concentrations of plasma HDL-C have been reported to be associated with infection, cognitive decline, and cancer death [41,42,43]. Hence, a higher HDL-C level might be a causal factor for the higher risk of all-cause deaths among individuals with lower MHR.
For the part of the curve (MHR > 0.006) in which the incidences of all-cause mortality increases with increasing MHR and a strong positive association between MHR and cardiovascular mortality, several possible explanations exist. Traditionally, monocytes were deemed to play a crucial role in the innate immunity in response to inflammation [44, 45]. Recent evidence suggests that monocytes are important mediators in the process of vascular inflammation and atherosclerosis [46, 47]. In the early stage, vascular endothelial function is impaired due to various factors leading to the subsequent release of chemokines such as CC-chemokine ligand 2 into the blood circulation [48]. Through the action of these chemokines, monocytes could then adhere firmly to the endothelium allowing their transmigration into the subendothelial space and differentiation into macrophages and foam cells [49], resulting in smooth muscle proliferation [50]. Besides, human monocytes and their subpopulations are observed in various pathological states, such as in infectious diseases [51], cancers [52], neurological disorders [53], and macrovascular diseases [54].
Several epidemiological studies such as the one by Framingham and co-workers have reported that HDL-C is a ‘good cholesterol’ since a lower serum level of HDL-C is indicative of increased susceptibility to CVD despite their non-linear relationship [39, 55]. HDL has been proven to mediate reverse cholesterol transport and has shown an anti-atherosclerosis effect. Moreover, HDL can also suppress inflammatory responses and inhibit the oxidation of native LDL [10]. Some studies reported interactions between HDL-C and monocytes [56, 57]. Dyslipidemia might change the behavior of monocytes as well as macrophages, and HDL-C can suppress the expression of endothelial adhesion cytokines, which in turn reduces the aggregation of monocytes [58]. Concurrently, the proliferation and activation of monocyte progenitor cells are also modulated by HDL-C [59]. All in all, both the increase in monocyte counts and the decrease in HDL-C concentrations lead to elevated MHR and decreased survival rates.
Study strength and limitations
Given the larger study population and longer follow-up period, the present study offered a deeper insight into the relation between MHR and the incidences of all-cause and cardiovascular mortality among the general population. Additionally, this study applied RCS models to assess a nonlinear relationship, which allowed an in-depth analysis of the correlations between MHR and all-cause mortality. Nevertheless, this study has several limitations. Firstly, the complications and living habits were obtained from self-reported data that were not validated, which could lead to recall bias. Secondly, this study only collected baseline MHR values which might not reflect the changes in MHR during the follow-up period. Thirdly, although the results were adjusted for many confounders, some nonincluded variables may contribute to other inevitable biases. Lastly, this study could not compare MHR with other inflammatory markers such as high-sensitivity C-reactive protein because these inflammatory markers had more than 10% missing values or were unavailable for analysis.
Conclusions
In summary, this study showed that MHR value was independently related to all-cause and cardiovascular mortality in the general population, suggesting that MHR might be a promising predictor for identifying individuals with a higher risk of poor clinical outcomes. Since MHR can be easily and inexpensively acquired, it might serve as a convenient clinical tool for risk stratification and guide preventative and treatment strategies for clinicians in routine clinical care.
Availability of data and materials
The data analyzed during the current study are available in the NHANES study (https://www.cdc.gov/nchs/nhanes/index.htm).
Abbreviations
- CVD:
-
Cardiovascular disease
- US:
-
United States
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- MHR:
-
Monocyte to HDL-C ratio
- ACS:
-
Acute coronary syndrome
- NHANES:
-
National Health and Nutrition Examination Survey
- NCHS:
-
National Center for Health Statistics
- ICD:
-
International Classification of Diseases
- DM:
-
Diabetes mellitus
- HF:
-
Heart failure
- CHD:
-
Coronary heart disease
- BMI:
-
Body mass index
- MDRD:
-
Modification of Diet in Renal Disease
- eGFR:
-
Estimated glomerular filtration rate
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- RCS:
-
Restricted cubic spline
- CAD:
-
Coronary artery disease
References
Authors/Task Force Members, ESC Committee for Practice Guidelines (CPG), ESC National Cardiac Societies. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019;290:140–205.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke Statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492. https://doi.org/10.1161/CIR.0000000000000558.
Ekroos K, Lavrynenko O, Titz B, Pater C, Hoeng J, Ivanov NV. Lipid-based biomarkers for CVD, COPD, and aging - a translational perspective. Prog Lipid Res. 2020;78:101030. https://doi.org/10.1016/j.plipres.2020.101030.
Johannesen CDL, Langsted A, Mortensen MB, Nordestgaard BG. Association between low density lipoprotein and all-cause and cause specific mortality in Denmark: prospective cohort study. BMJ. 2020;371:m4266. https://doi.org/10.1136/bmj.m4266.
Ravnskov U, de Lorgeril M, Diamond DM, Hama R, Hamazaki T, Hammarskjold B, et al. LDL-C does not cause cardiovascular disease: a comprehensive review of the current literature. Expert Rev Clin Pharmacol. 2018;11(10):959–70. https://doi.org/10.1080/17512433.2018.1519391.
Pardali E, Waltenberger J. Monocyte function and trafficking in cardiovascular disease. Thromb Haemost. 2012;108(5):804–11. https://doi.org/10.1160/TH12-04-0276.
Groh L, Keating ST, Joosten LAB, Netea MG, Riksen NP. Monocyte and macrophage immunometabolism in atherosclerosis. Semin Immunopathol. 2018;40(2):203–14. https://doi.org/10.1007/s00281-017-0656-7.
Choi SH, Kim JH, Lim S, Lim JY, Kim KW, Park KS, et al. Monocyte count as a predictor of cardiovascular mortality in older Korean people. Age Ageing. 2017;46(3):433–8. https://doi.org/10.1093/ageing/afw226.
Kreuter M, Lee JS, Tzouvelekis A, Oldham JM, Molyneaux PL, Weycker D, et al. Monocyte count as a prognostic biomarker in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2021;204(1):74–81. https://doi.org/10.1164/rccm.202003-0669OC.
Soran H, Hama S, Yadav R, Durrington PN. HDL functionality. Curr Opin Lipidol. 2012;23(4):353–66. https://doi.org/10.1097/MOL.0b013e328355ca25.
Murphy AJ, Woollard KJ, Hoang A, Mukhamedova N, Stirzaker RA, McCormick SP, et al. High-density lipoprotein reduces the human monocyte inflammatory response. Arterioscler Thromb Vasc Biol. 2008;28(11):2071–7. https://doi.org/10.1161/ATVBAHA.108.168690.
Villanueva DLE, Tiongson MD, Ramos JD, Llanes EJ. Monocyte to high-density lipoprotein ratio (MHR) as a predictor of mortality and major adverse cardiovascular events (MACE) among ST elevation myocardial infarction (STEMI) patients undergoing primary percutaneous coronary intervention: a meta-analysis. Lipids Health Dis. 2020;19(1):55. https://doi.org/10.1186/s12944-020-01242-6.
Kanbay M, Solak Y, Unal HU, Kurt YG, Gok M, Cetinkaya H, et al. Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease. Int Urol Nephrol. 2014;46(8):1619–25. https://doi.org/10.1007/s11255-014-0730-1.
You S, Zhong C, Zheng D, Xu J, Zhang X, Liu H, et al. Monocyte to HDL cholesterol ratio is associated with discharge and 3-month outcome in patients with acute intracerebral hemorrhage. J Neurol Sci. 2017;372:157–61. https://doi.org/10.1016/j.jns.2016.11.022.
Wu Q, Mao W. New prognostic factor for hepatitis B virus-related decompensated cirrhosis: Ratio of monocytes to HDL-cholesterol. J Clin Lab Anal. 2021:e24007. https://doi.org/10.1002/jcla.24007.
Wei XB, Chen F, Huang JL, He PC, Wei YX, Tan N, et al. Novel risk biomarker for infective endocarditis patients with Normal left ventricular ejection fraction- monocyte to high-density lipoprotein cholesterol ratio. Circ J. 2017;82(1):283–8. https://doi.org/10.1253/circj.CJ-17-0427.
Karahan S, Okuyan E. Monocyte-to-high density lipoprotein cholesterol ratio as a predictor of mortality in patients with transcatheter aortic valve replacement. Eur Rev Med Pharmaco. 2021;25(16):5153–62.
Chen J, Zhong Z, Shi D, Li J, Li B, Zhang R, et al. Association between monocyte count to high-density lipoprotein cholesterol ratio and mortality in patients undergoing peritoneal dialysis. Nutr Metab Cardiovasc Dis. 2021;31(7):2081–8. https://doi.org/10.1016/j.numecd.2021.03.014.
Cardoso CRL, Leite NC, Salles GF. Importance of hematological parameters for micro- and macrovascular outcomes in patients with type 2 diabetes: the Rio de Janeiro type 2 diabetes cohort study. Cardiovasc Diabetol. 2021;20(1):133. https://doi.org/10.1186/s12933-021-01324-4.
Bolayir A, Gokce SF, Cigdem B, Bolayir HA, Yildiz OK, Bolayir E, et al. Monocyte/high-density lipoprotein ratio predicts the mortality in ischemic stroke patients. Neurol Neurochir Pol. 2018;52(2):150–5. https://doi.org/10.1016/j.pjnns.2017.08.011.
Sun M, Zhao D, Zhang Y, Zhai Y, Ye M, Wang X, et al. Prognostic utility of monocyte to high-density lipoprotein ratio in patients with acute coronary syndrome: a Meta-analysis. Am J Med Sci. 2020;359(5):281–6. https://doi.org/10.1016/j.amjms.2020.01.018.
Liu XC, He GD, Lo K, Huang YQ, Feng YQ. The triglyceride-glucose index, an insulin resistance marker, Was Non-linear Associated With All-Cause and Cardiovascular Mortality in the General Population. Front Cardiovasc Med. 2020;7:628109. https://doi.org/10.3389/fcvm.2020.628109.
National Center for Health Statistics, Centers for Disease Control and Prevention. The Linkage of National Center for Health Statistics Survey Data to the National Death Index – 2015 Linked Mortality File (LMF): Methodology Overview and Analytic Considerations. Accessed 11 Apr 2019.
Li J, Covassin N, Bock JM, Mohamed EA, Pappoppula LP, Shafi C, et al. Excessive daytime sleepiness and cardiovascular mortality in US adults: a NHANES 2005-2008 follow-up study. Nat Sci Sleep. 2021;13:1049–59. https://doi.org/10.2147/NSS.S319675.
Liao S, Wu N, Gong D, Tang X, Yin T, Zhang H, et al. Association of aldehydes exposure with obesity in adults. Ecotoxicol Environ Saf. 2020;201:110785. https://doi.org/10.1016/j.ecoenv.2020.110785.
Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145(4):247–54. https://doi.org/10.7326/0003-4819-145-4-200608150-00004.
Zhang DP, Baituola G, Wu TT, Chen Y, Hou XG, Yang Y, et al. An elevated monocyte-to-high-density lipoprotein-cholesterol ratio is associated with mortality in patients with coronary artery disease who have undergone PCI. Biosci Rep. 2020;40(8)
Cetin MS, Ozcan Cetin EH, Kalender E, Aydin S, Topaloglu S, Kisacik HL, et al. Monocyte to HDL cholesterol ratio predicts coronary artery disease severity and future major cardiovascular adverse events in acute coronary syndrome. Heart Lung Circ. 2016;25(11):1077–86. https://doi.org/10.1016/j.hlc.2016.02.023.
Cicek G, Kundi H, Bozbay M, Yayla C, Uyarel H. The relationship between admission monocyte HDL-C ratio with short-term and long-term mortality among STEMI patients treated with successful primary PCI. Coron Artery Dis. 2016;27(3):176–84. https://doi.org/10.1097/MCA.0000000000000343.
Zhan X, Pan D, Wei X, Wen D, Yan C, Xiao J. Monocyte to high-density lipoprotein ratio and cardiovascular events in patients on peritoneal dialysis. Nutr Metab Cardiovasc Dis. 2020;30(7):1130–6. https://doi.org/10.1016/j.numecd.2020.03.011.
Kim D, Kim DW, Lee YH, Park SY, Song YW, Shin H, et al. Relationships between monocyte count to high-density lipoprotein cholesterol ratio and cardiovascular outcomes in patients commencing dialysis. J Int Med Res. 2021;49(11):3000605211058861. https://doi.org/10.1177/03000605211058861.
Avci A, Biricik S, Avci BS, Yesiloglu O, Sumbul HE, Icme F, et al. The new prognostic factor for pulmonary embolism: the ratio of monocyte count to HDL cholesterol. Am J Emerg Med. 2021;46:212–6. https://doi.org/10.1016/j.ajem.2020.07.026.
Huang JB, Chen YS, Ji HY, Xie WM, Jiang J, Ran LS, et al. Neutrophil to high-density lipoprotein ratio has a superior prognostic value in elderly patients with acute myocardial infarction: a comparison study. Lipids Health Dis. 2020;19(1):59. https://doi.org/10.1186/s12944-020-01238-2.
Sun Y, Lu J, Zheng D, Qian J, Zhang H, Xing D, et al. Predictive value of monocyte to HDL cholesterol ratio for stroke-associated pneumonia in patients with acute ischemic stroke. Acta Neurol Belg. 2021;121(6):1575–81. https://doi.org/10.1007/s13760-020-01418-y.
Ulus T, Isgandarov K, Yilmaz AS, Vasi I, Moghanchizadeh SH, Mutlu F. Predictors of new-onset atrial fibrillation in elderly patients with acute coronary syndrome undergoing percutaneous coronary intervention. Aging Clin Exp Res. 2018;30(12):1475–82. https://doi.org/10.1007/s40520-018-0926-9.
Li ZH, Lv YB, Zhong WF, Gao X, Byers Kraus V, Zou MC, et al. High-density lipoprotein cholesterol and all-cause and cause-specific mortality among the elderly. J Clin Endocrinol Metab. 2019;104(8):3370–8. https://doi.org/10.1210/jc.2018-02511.
Chen CL, Liu XC, Liu L, Lo K, Yu YL, Huang JY, et al. U-shaped Association of High-Density Lipoprotein Cholesterol with all-cause and cardiovascular mortality in hypertensive population. Risk Manag Healthc Policy. 2020;13:2013–25. https://doi.org/10.2147/RMHP.S272624.
Huang CY, Lin FY, Shih CM, Au HK, Chang YJ, Nakagami H, et al. Moderate to high concentrations of high-density lipoprotein from healthy subjects paradoxically impair human endothelial progenitor cells and related angiogenesis by activating rho-associated kinase pathways. Arterioscler Thromb Vasc Biol. 2012;32(10):2405–17. https://doi.org/10.1161/ATVBAHA.112.248617.
Madsen CM, Varbo A, Nordestgaard BG. Extreme high high-density lipoprotein cholesterol is paradoxically associated with high mortality in men and women: two prospective cohort studies. Eur Heart J. 2017;38(32):2478–86. https://doi.org/10.1093/eurheartj/ehx163.
von Eckardstein A, Rohrer L. HDLs in crises. Curr Opin Lipidol. 2016;27(3):264–73. https://doi.org/10.1097/MOL.0000000000000294.
Madsen CM, Varbo A, Tybjaerg-Hansen A, Frikke-Schmidt R, Nordestgaard BG. U-shaped relationship of HDL and risk of infectious disease: two prospective population-based cohort studies. Eur Heart J. 2018;39(14):1181–90. https://doi.org/10.1093/eurheartj/ehx665.
Ko DT, Alter DA, Guo H, Koh M, Lau G, Austin PC, et al. High-density lipoprotein cholesterol and cause-specific mortality in individuals without previous cardiovascular conditions: the CANHEART study. J Am Coll Cardiol. 2016;68(19):2073–83. https://doi.org/10.1016/j.jacc.2016.08.038.
An Y, Zhang X, Wang Y, Wang Y, Liu W, Wang T, et al. Longitudinal and nonlinear relations of dietary and serum cholesterol in midlife with cognitive decline: results from EMCOA study. Mol Neurodegener. 2019;14(1):51. https://doi.org/10.1186/s13024-019-0353-1.
Kratofil RM, Kubes P, Deniset JF. Monocyte conversion during inflammation and injury. Arterioscler Thromb Vasc Biol. 2017;37(1):35–42. https://doi.org/10.1161/ATVBAHA.116.308198.
Ozanska A, Szymczak D, Rybka J. Pattern of human monocyte subpopulations in health and disease. Scand J Immunol. 2020;92(1):e12883. https://doi.org/10.1111/sji.12883.
Zawada AM, Rogacev KS, Schirmer SH, Sester M, Bohm M, Fliser D, et al. Monocyte heterogeneity in human cardiovascular disease. Immunobiology. 2012;217(12):1273–84. https://doi.org/10.1016/j.imbio.2012.07.001.
Franca CN, Izar MCO, Hortencio MNS, do Amaral JB, Ferreira CES, Tuleta ID, et al. Monocyte subtypes and the CCR2 chemokine receptor in cardiovascular disease. Clin Sci (Lond). 2017;131(12):1215–24. https://doi.org/10.1042/CS20170009.
Yang J, Park Y, Zhang H, Gao X, Wilson E, Zimmer W, et al. Role of MCP-1 in tumor necrosis factor-alpha-induced endothelial dysfunction in type 2 diabetic mice. Am J Physiol Heart Circ Physiol. 2009;297(4):H1208–16. https://doi.org/10.1152/ajpheart.00396.2009.
Vlacil AK, Schuett J, Schieffer B, Grote K. Variety matters: diverse functions of monocyte subtypes in vascular inflammation and atherogenesis. Vasc Pharmacol. 2019;113:9–19. https://doi.org/10.1016/j.vph.2018.12.002.
Moreno PR, Purushothaman KR, Fuster V, O'Connor WN. Intimomedial interface damage and adventitial inflammation is increased beneath disrupted atherosclerosis in the aorta: implications for plaque vulnerability. Circulation. 2002;105(21):2504–11. https://doi.org/10.1161/01.CIR.0000017265.52501.37.
Strauss-Ayali D, Conrad SM, Mosser DM. Monocyte subpopulations and their differentiation patterns during infection. J Leukoc Biol. 2007;82(2):244–52. https://doi.org/10.1189/jlb.0307191.
Olingy CE, Dinh HQ, Hedrick CC. Monocyte heterogeneity and functions in cancer. J Leukoc Biol. 2019;106(2):309–22. https://doi.org/10.1002/JLB.4RI0818-311R.
Zhao M, Tuo H, Wang S, Zhao L. The roles of monocyte and monocyte-derived macrophages in common brain disorders. Biomed Res Int. 2020;2020:9396021–11. https://doi.org/10.1155/2020/9396021.
Raffort J, Lareyre F, Clement M, Hassen-Khodja R, Chinetti G, Mallat Z. Monocytes and macrophages in abdominal aortic aneurysm. Nat Rev Cardiol. 2017;14(8):457–71. https://doi.org/10.1038/nrcardio.2017.52.
Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989;79(1):8–15. https://doi.org/10.1161/01.CIR.79.1.8.
Rahman MS, Murphy AJ, Woollard KJ. Effects of dyslipidaemia on monocyte production and function in cardiovascular disease. Nat Rev Cardiol. 2017;14(7):387–400. https://doi.org/10.1038/nrcardio.2017.34.
Yamamoto S, Narita I, Kotani K. The macrophage and its related cholesterol efflux as a HDL function index in atherosclerosis. Clin Chim Acta. 2016;457:117–22. https://doi.org/10.1016/j.cca.2016.04.012.
Açıkgöz SK, Açıkgöz E, Şensoy B, Topal S, Aydoğdu S. Monocyte to high-density lipoprotein cholesterol ratio is predictive of in-hospital and five-year mortality in ST-segment elevation myocardial infarction. Cardiol J. 2016;23(5):505–12. https://doi.org/10.5603/CJ.a2016.0026.
Yvan-Charvet L, Pagler T, Gautier EL, Avagyan S, Siry RL, Han S, et al. ATP-binding cassette transporters and HDL suppress hematopoietic stem cell proliferation. Science. 2010;328(5986):1689–93. https://doi.org/10.1126/science.1189731.
Acknowledgments
The authors would like to thank Dr. Chengzhong Chen (Dana-Farber Cancer Institute, Harvard Medical School, Boston, MA) for providing statistical guidance on Empower(R) and Home for Researchers (https://www.home-for-researchers.com) for editing this manuscript.
Funding
None.
Author information
Authors and Affiliations
Contributions
MJ: conceptualization, formal analysis, writing-review draft. JY: investigation and writing-original draft. HZ and ML: validation. WS: project administration. XK: conceptualization and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The survey protocol was approved by the Ethics Review Board of the National Center for Health Statistics. All participants have signed a written informed consent form.
Consent for publication
All participants in the NHANES study provided consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, M., Yang, J., Zou, H. et al. Monocyte-to-high-density lipoprotein-cholesterol ratio (MHR) and the risk of all-cause and cardiovascular mortality: a nationwide cohort study in the United States. Lipids Health Dis 21, 30 (2022). https://doi.org/10.1186/s12944-022-01638-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-022-01638-6