Abstract
Objective
Familial hypercholesterolemia (FH) is an important cause of premature coronary artery disease (CAD). Prognosis data are lacking in patients with FH and coronary artery disease particularly in the era of widespread statin use. We compared long-term prognosis between patients with and without FH after a coronary event.
Methods
In this retrospective study, 865 patients younger than 40 years of age with CAD were enrolled. FH was diagnosed based on the Dutch Lipid Clinic Network algorithm. Baseline characteristics, coronary angiographic findings and prognosis during median follow-up of 5 (3–8) years were compared between patients with or without FH.
Results
Definite or probable FH was detected in 37 patients (4.3%) and possible FH in 259 patients (29.9%). FH was associated with significantly higher prevalence of multi-vessel lesions (p < 0.001) and higher Gensini score (p = 0.008). In the subset of 706 patients for whom follow-up data were available, 127 (18.0%) suffered major adverse cardiovascular and cerebrovascular events (MACCE). FH was associated with increased risk of MACCE, independently of age, sex, smoking, body mass index, hypertension or diabetes mellitus (HR = 2.30, 95%CI = 1.09 to 4.84, p = 0.028).
Conclusions
FH is an independent risk factor for MACCE in young patients after a coronary event during long-term follow-up. It is necessary to optimize lipid treatment of patients with FH after a coronary event.
Similar content being viewed by others
Introduction
Familial hypercholesterolemia (FH; MIM 143890) is an autosomal dominant genetic disease characterized by high levels of low-density lipoprotein cholesterol (LDL-C), cutaneous xanthomas and premature coronary artery disease (pCAD), which has recently become a major health concern around the world [1]. Data suggest that 1 in 200 of Caucasians are heterozygous for FH and that 1 in 160,000–300,000 are homozygous [2], which are much higher prevalences than those estimated a decade earlier [3]. A study in China has suggested a prevalence of probable or definite FH of 0.28% (1.4/500) based on the modified Dutch Lipid Clinic Network (DLCN) definition [4]. These studies suggest that nearly 36 million people around the world have potential FH, including 3.8 million in China. FH remains largely underdiagnosed and undertreated. Fewer than 1% of FH cases are diagnosed in most countries, except in some countries of western Europe [2].
Timely detection of FH is important because the presence of definite or probable FH increases 13-fold (95%CI = 10–17) risk of CAD compared to the general population [5]. In Europe, FH occurs in up to 8% of patients admitted for acute coronary syndromes, a frequency that is 10 times higher than in the general population [6]. For patients with acute coronary syndromes, the diagnosis of FH during hospitalization helps to ensure the use of high-dose statins and the management of blood lipids after discharge [7].
Whether FH in CAD alters the clinical manifestations of the disease and the prognosis of patients is unclear. We compared the long-term prognosis of young patients with and without FH after a coronary event.
Methods
Study population
Patients with both gender (≥18 years and < 40 years of age) with the following first or recurrent clinical diagnoses or procedures at Beijing Anzhen Hospital from January 2004 to January 2015 were consecutively enrolled in this retrospective study, including those with elective or primary PCI, elective or emergency CABG, acute myocardial infarction (AMI: ICD-10 I21), and acute myocardial ischemia (ICD-10 I20) [8]. The diagnosis of every participate enrolled in this study was confirmed by two experienced cardiologists.
Patients were excluded if blood lipid data were missing or if the patients had infectious or systematic inflammatory disease, significant hematologic disorders, thyroid dysfunction, severe liver and/or renal dysfunction, or malignant tumors. The study was approved by the Institutional Ethics Committee of Beijing Anzhen Hospital. The Ethics Committee waived the requirement for informed consent because of the retrospective nature of the study.
Patients enrolled in the study were diagnosed with FH based on the DLCN criteria (Table 1), which are endorsed by ESC/EAS guidelines [9]. Patients were classified as having possible FH if their DLCN score was 3–5, “definite” FH was > 8, “probable” FH was 6~8 [10]. In our study, we combined the categories “definite” FH and “probable” FH into one category (definite/probable FH). Family history of elevated LDL-C was not available for our study sample, so this information was counted as ‘0’ in the DLCN algorithm. Similarly, genetic tests of FH were not conducted and were counted as ‘0’.
Patient assessment
Data on clinical characteristics were collected based on review of medical records or patient interviews. All patients underwent clinical examination, blood testing and angiography. Peripheral blood samples were drawn from patients within 24 h after admission, and lipid profiles and other assays were performed using an automated biochemical analyzer. LDL-cholesterol concentrations were multiplied by 1.43 in individuals using cholesterol lowering medication before admission [11]. Hypertension was defined according to the 2010 Hypertension Prevention and Treatment Guidelines [12] as systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg or the taking of antihypertensive medication. Diabetes mellitus was defined according to the American Diabetes Association (ADA) Diabetes Diagnostic Criteria [13]. Data were collected on smoking status and body mass index (BMI). After release from hospital, patients were followed up through phone interviews, review of hospital records or outpatient visits.
The primary outcome was main adverse cardiovascular and cerebrovascular events (MACCE), which were defined as cardiac death, acute myocardial infarction, acute decompensated heart failure requiring hospitalization, cerebrovascular events or ischemia-driven revascularization. Ischemia-driven revascularization was defined as repeated PCI or CABG of lesions in the presence of acute myocardial infarction, unstable or stable angina, or documented silent ischemia.
Statistical analysis
Continuous variables were presented as the mean ± standard deviation (SD) if the data were normally distributed. Otherwise, the data were presented as median and interquartile range (IQR). Categorical variables were expressed as frequencies and percentages. Differences in clinical characteristics between patients with or without FH were assessed for significance using one-way ANOVA, χ2 tests or the Kruskal-Wallis rank test. Hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) were calculated using Cox proportional hazard models. Event-free survival was analyzed using the Kaplan-Meier method, and inter-group differences in survival were assessed for significance using the log-rank test. All statistical calculations were performed in SPSS 22 (IBM, Chicago, IL, USA), with p < 0.05 defined as indicating significance.
Results
Baseline characteristics
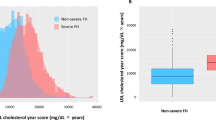
Among 865 participants, 37 (4.3%) had definite/probable FH and 259 (29.9%) had possible FH, respectively. The remaining 569 (65.8%) received DLCN scores of “unlikely FH” and so were classified as not having FH (Table 2). Unstable angina pectoris is the main cause of hospitalization in FH patients (56.8%), while ST-segment elevation myocardial infarction (STEMI) is a common cause of hospitalization in non-FH patients (57.3%). Compared with patients without FH, those with definite or probable FH were younger but showed higher prevalence of multi-vessel disease (75.7% vs 34.1%), chronic total occlusion (CTO) (45.9% vs 29.9%)and greater coronary severity based on Gensini score (50 vs 32). More patients with definite or probable FH received bypass grafting than those without FH (32.4% vs 10.7%) (Table 3). When discharge, 75.7% of patients with definite or probable FH were on statin therapy, 24.3% on a combination of statin and ezetimibe, and 5.4% on high-dose statin.
The association between FH and risk of MACCE
Follow-up data were available for 708 (81.8%) patients, while the remaining patients were lost to follow-up, such as because they moved or changed their telephone number. During follow-up, which lasted for a median of 5 (3–8) years, one patient without FH died of leukemia and one without FH died of a brain tumor. These two patients were excluded from the follow-up analysis. Among the remaining 706 follow-up patients, 127 (18.0% of all patients followed-up) experienced a cardiovascular event, which was myocardial infarction in 36 cases (5.1% of all patients followed-up) and cardiac deaths in 15 cases (2.1% of all patients followed-up), respectively. In an unadjusted model, patients with definite or probable FH were at 2.34-fold higher risk of MACCE than those without FH (HR = 2.34, 95%CI = 1.17–4.68, p = 0.016). In a multivariable model adjusted for age and sex, patients with definite or probable FH were at 2.39-fold higher risk of MACCE than patients without FH (HR = 2.39, 95%CI = 1.19–4.78, p = 0.014). These HR estimates did not decrease when the multivariable model also adjusted for BMI, smoking, hypertension, and diabetes mellitus (HR = 2.30, 95%CI = 1.09–4.84, p = 0.028) (Table 4).
Discussion
This study suggests that the prevalence of definite or probable FH among young patients after a coronary event was 4.3%, while that of possible FH was 29.9%, based on the DLCN algorithm. In our cohort, FH was associated with more serious coronary lesions and greater prevalence of multi-vessel disease, despite being associated with younger age. FH was independently associated with increased risk of MACCE during long-term follow-up. Our study suggests that timely diagnosis of FH may help stratify the risk of future MACCE in young patients after a coronary event, as well as identify patients whose close relatives should be screened.
Due to lack of national data, we cannot compare our measured prevalence of 4.3% for definite or probable FH in our cohort with statistics for the population of CAD patients or the general population in China. A single-center study in China reported a prevalence of 3.9% for definite or probable FH in patients with acute myocardial infarction and 7.1% in patients with premature myocardial infarction [14]. A European multi-country study involving 1451 patients with premature acute coronary syndrome and younger than 55 years (men) or 60 years (women) reported prevalence of 4.8% for definite or probable FH and 47.1% for possible FH [6].
As a hereditary disease, the clinical diagnostic criteria of FH can identify FH rapidly and costly. We found that patients with definite or probable FH, despite their younger age, exhibited more severe coronary atherosclerosis and higher prevalence (75.7%) of multi-vessel lesions than patients without FH (34.1%). Patients with FH tend to receive lipid-lowering treatment relatively late, when severe atherosclerosis has developed, and the efficacy of lipid-lowering therapy may be reduced. In addition, we found that few of patients with FH in this study were discharged on high-dose statin therapy. Instead, our clinicians preferred to use moderate doses of statins on their own or combined with ezetimibe or bile acid sequestrants in order to enhance lipid-lowering therapy while minimizing the statin-associated risk of elevated liver enzymes and creatine kinase. Statin monotherapy fails to achieve optimal LDL-C levels in most patients with FH [15]. More effective lipid-lowering strategies include high-dose statin in combination with evolocumab [16, 17] or ezetimibe. Bile acid sequestrants are rarely used because of their adverse gastrointestinal side effects and poor patient compliance. Colesevelam has stronger ability to bind bile acid. Monotherapy with colesevelam reduced LDL cholesterol by 13–19% and additional 18% in combination with statins [18]. While treatment for CAD patients with FH remains to be optimized, statins can substantially improve prognosis: modest doses of statins can reduce risk of CAD by about 80% in patients with FH [19], and a prospective registry study involving 3382 patients with FH showed that statins can reduce coronary mortality by 30% [20].
With regard to clinical outcomes, we found that definite or probable FH had a > 2-fold increase MACCE during a long-term follow-up comparing with the patients without FH. This association between FH clinical diagnosis and MACCE was independent of conventional risk factors. Since the lipid-lowering therapy in patients with FH is generally quite late, the coronary artery lesions in patients with FH are more serious. This may be one of the reasons for the adverse outcomes in these patients. In addition, even after a coronary event, the rate of high-dose statin therapy in FH patients was fairly inadequate in this cohort. These patients were still exposed to high levels of LDL-C. Furthermore, though some patients with FH were treated with high-dose statin combined with ezetimibe, part of them still could not attain the desirable targets of LDL-C levels. For these patients, novel lipid-lowering drugs such as proprotein convertase subtilisin kexin 9 inhibitors are expected to further decrease the LDL-C levels and improve cardiovascular outcomes [21, 22].
In conclusion, early diagnosis and treatment are crucial for improving the outcomes of FH patients. Screening for FH may allow timelier and therefore more effective lipid management in CAD patients with FH. It may also identify patients whose close family members should be screened for FH in order to ensure timely intervention to prevent cardiovascular events.
Limitations
The results of this study should be interpreted with caution in light of several limitations. One is the retrospective design, although all patients were followed up prospectively. Secondly, we did not perform genetic molecular analysis to identify heterozygous FH patients. In addition, not all patients received similar treatment. Finally, family history of elevated LDL-C was not available for the presents study, which might underestimate the prevalence of FH in this population.
Conclusions
It is necessary to optimize lipid treatment of patients with FH after a coronary event. This study provides evidence that FH is an independent risk factor for long-term MACCE in young patients after a coronary event.
Availability of data and materials
The datasets used and/or analyzed during the current study will be available from the corresponding author on reasonable requests after study completion.
Abbreviations
- ACEI/ARB:
-
angiotensin converting enzyme inhibitors/angiotensin receptor blocker
- BMI:
-
body mass index
- CABG:
-
coronary artery bypass grafting
- CAD:
-
Coronary artery disease
- CTO:
-
chronic total occlusion
- FH:
-
Familial hypercholesterolemia
- HDL-C:
-
High density lipoprotein cholesterol
- LDL-C:
-
low-density lipoprotein cholesterol
- MACCE:
-
major adverse cardiovascular and cerebrovascular events
- NONSTEMI:
-
Non-ST-segment elevation myocardial infarction
- pCAD:
-
Premature coronary artery disease
- PCI:
-
percutaneous coronary intervention
- PTCA:
-
percutaneous transluminal coronary angioplast
- SAP:
-
Stable angina pectoris
- STEMI:
-
ST-segment elevation myocardial infarction
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- UAP:
-
Unstable angina pectoris
References
Watts GF, Gidding S, Wierzbicki AS, Toth PP, Alonso R, Brown WV, Bruckert E, Defesche J, Lin KK, Livingston M, Mata P, Parhofer KG, Raal FJ, Santos RD, Sijbrands EJ, Simpson WG, Sullivan DR, Susekov AV, Tomlinson B, Wiegman A, Yamashita S, Kastelein JJ. Integrated guidance on the care of familial hypercholesterolaemia from the international FH Foundation. Int J Cardiol. 2014;171(3):309–25. 24418289.
Nordestgaard BG,Chapman MJ, Humphries SE, Ginsberg HN, Masana L, Descamps OS, Wiklund O, Hegele RA, Raal FJ, Defesche JC, Wiegman A, Santos RD, Watts GF, Parhofer KG, Hovingh GK, Kovanen PT, Boileau C, Averna M, Borén J, Bruckert E, Catapano AL, Kuivenhoven JA, Pajukanta P, Ray K, Stalenhoef AF, Stroes E, Taskinen MR, Tybjærg-Hansen A; European Atherosclerosis Society Consensus Panel. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European atherosclerosis society. Eur Heart J 2013, 34: 3478-3490a. [PMID: 23956253].
Austin MA, Hutter CM, Zimmern RL, Humphries SE. Genetic causes of monogenic heterozygous familial hypercholesterolemia: a HuGE prevalence review. Am J Epidemiol 2004, 160(5): 407–420. [PMID: 15321837].
Shi Z, Yuan B, Zhao D, Taylor AW, Lin J, Watts GF. Familial hypercholesterolemia in China: prevalence and evidence of underdetection and undertreatment in a community population. Int J Cardiol. 2014;174:834–6. 24801084.
ScientificSteeringCommitteeonbehalfoftheSimonBroomeRegister Group. Mortality in treated heterozygous familial hypercholesterolaemia: implications for clinical management. Atherosclerosis. 1999;142(1):105–12. 9920511.
Nanchen D, Gencer B, Auer R, Räber L, Stefanini GG, Klingenberg R, Schmied CM, Cornuz J, Muller O, Vogt P, Jüni P, Matter CM, Windecker S, Lüscher TF, Mach F, Rodondi N. Prevalence and management of familial hypercholesterolaemia in patients with acute coronary syndromes. Eur Heart J. 2015;36(36):2438–45. 26142466.
Rerup SA, Bang LE, Mogensen UM, Engstrøm T, Jørgensen E, Pedersen F, Torp-Pedersen C, Gislason G, James S, Hagström E, Køber L, Fosbøl EL. The prevalence and prognostic importance of possible familial hypercholesterolemia in patients with myocardial infarction. Am Heart J. 2016;181:35–42. 27823691.
De Backer G, Besseling J, Chapman J, Hovingh GK, Kastelein JJ, Kotseva K, Ray K, Reiner Ž, Wood D, De Bacquer D, EUROASPIRE Investigators. Prevalence and management of familial hypercholesterolaemia in coronary patients: an analysis of EUROASPIRE IV, a study of the European Society of Cardiology. Atherosclerosis. 2015;241(1):169–75. 25997074.
European Association for Cardiovascular Prevention & Rehabilitation, Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P, Erdine S, Halcox J, Hobbs R, Kjekshus J, Filardi PP, Riccardi G, Storey RF, Wood D. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011, 32(14): 1769–1818. [PMID: 21712404].
Civeira F. International panel on Management of Familial Hypercholesterolemia. Guidelines for the diagnosis and management of heterozygous familial hypercholesterolemia. Atherosclerosis. 2004, 173 (1): 55–68. [PMID: 15177124].
Benn M, Watts GF, Tybjaerg-Hansen A, Nordestgaard BG. Familial hypercholesterolemia in the Danish general population: prevalence, coronary artery disease, and cholesterol-lowering medication. J Clin Endocrinol Metab. 2012;97:3956–64. 22893714.
Liu LS. Writing group of 2010 Chinese guidelines for the Management of Hypertension. 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi 2011, 39(7): 579–615. [PMID: 22088239].
American Diabetes Association. Introduction standards of medical care in diabetes-2018. Diabetes Care. 2018 Jan;41(Suppl 1):S13-S27. [PMID: 29222373].
Li S, Zhang Y, Zhu CG, Guo YL, Wu NQ, Gao Y, Qing P, Li XL, Sun J, Liu G, Dong Q, Xu RX, Cui CJ, Li JJ. Identification of familial hypercholesterolemia in patients with myocardial infarction: a Chinese cohort study. J Clin Lipidol. 2016;10(6):1344–52. 27919351.
Polychronopoulos G, Tziomalos K. Novel treatment options for the management of heterozygous familial hypercholesterolemia. Expert Rev Clin Pharmacol. 2017;10(12):1375–81. 28884604.
Robinson JG, Nedergaard BS, Rogers WJ, Fialkow J, Neutel JM, Ramstad D, Somaratne R, Legg JC, Nelson P, Scott R, Wasserman SM, Weiss R, LAPLACE-2 Investigators. Effect of evolocumab or ezetimibe added to moderate- or high-intensity statin therapy on LDL-C lowering in patients with hypercholesterolemia: the LAPLACE-2 randomized clinical trial. JAMA. 2014;311(18):1870–82. 24825642. https://doi.org/10.1001/jama.2014.4030.
Wilson PWF, Polonsky TS, Miedema MD, Khera A, Kosinski AS, Kuvin JT. Systematic Review for the 2018. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018. Doi https://doi.org/10.1016/j.jacc.2018.11.004. [Epub ahead of print] [PMID: 30423394].
Alonso R, Perez de Isla L, Muñiz-Grijalvo O, Diaz-Diaz JL, Mata P. Familial Hypercholesterolaemia diagnosis and management. Eur Cardiol 2018, 13(1):14–20. [PMID: 30310464].
Versmissen J, Oosterveer DM, Yazdanpanah M, Defesche JC, Basart DC, Liem AH, Heeringa J, Witteman JC, Lansberg PJ, Kastelein JJ, Sijbrands EJ. Efficacy of statins in familial hypercholesterolaemia: a long term cohort study. BMJ. 2008;337:a2423. 19001495.
Neil A, Cooper J, Betteridge J, Capps N, McDowell I, Durrington P, Seed M, Humphries SE. Reductions in all-cause, cancer, and coronary mortality in statin-treated patients with heterozygous familial hypercholesterolaemia: a prospective registry study. Eur Heart J. 2008;29(23):2625–33. 18840879.
Santos RD, Watts GF. Familial hypercholesterolaemia: PCSK9 inhibitors are coming. Lancet. 2015;385:307–10. 25282517. https://doi.org/10.1016/S0140-6736(14)61702-5.
Raal FJ, Stein EA, Dufour R, Turner T, Civeira F, Burgess L, Langslet G, Scott R, Olsson AG, Sullivan D, Hovingh GK, Cariou B, Gouni-Berthold I, Somaratne R, Bridges I, Scott R, Wasserman SM, Gaudet D, RUTHERFORD-2 Investigators. PCSK9 inhibition with evolocumab (AMG 145) in heterozygous familial hypercholesterolaemia (RUTHERFORD-2): a randomised, double-blind, placebo-controlled trial. Lancet. 2015;385:331–40. 25282519. https://doi.org/10.1016/S0140-6736(14)61399-4.
Acknowledgements
We thank all our colleagues at the Emergency & Critical Care Center and the department of Cardiology, Beijing Anzhen Hospital, Capital Medical University.
Funding
This work was supported by the grant from Chinese Cardiovascular Association-Access found (2017-CCA-AF-002), Chinese Cardiovascular Association-V.G found (2017-CCA-VG-003), Beijing Municipal Science and Technology Commission (Z161100000116073), National Key Research and Development Program of China (2017YFC0908800), Beijing Municipal Administration of Hospitals’ Ascent Plan (DFL20150601) and Mission plan (SML20180601), Beijing Municipal Health Commission “Project of Science and Technology Innovation Center”(PXM2019_026272_000006)(PXM2019_026272_000005).
Author information
Authors and Affiliations
Contributions
Study conception and design: WL, YJZ. Literature search: XW, GJC. Data collection and analysis: XW, GJC, YYW, RL, ZWX, GXL, WHW, YW, CGW, QWJ, XGW, QZ, YJZ, LYW. Data interpretation: XW, GJC, Writing: XW, GJC. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was complied with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Beijing Anzhen Hospital. Written informed consent was not obtained from the participants, because of the data retrospectively obtained from electronic medical records.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wang, X., Cai, G., Wang, Y. et al. Comparison of long-term outcomes of young patients after a coronary event associated with familial hypercholesterolemia. Lipids Health Dis 18, 131 (2019). https://doi.org/10.1186/s12944-019-1074-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-019-1074-8