Abstract
Background
To investigate the relationship between oxysterols and mild cognitive impairment (MCI) in a matched case–control study.
Methods
The plasma levels of four oxysterols, 27–hydroxycholesterol (27–OHC), 24S–hydroxycholesterol (24S–OHC), 7α–hydroxycholesterol (7α–OHC) and 7β–hydroxycholesterol (7β–OHC), were analyzed by High Performance Liquid Chromatography–Mass Spectrometry (HPLC–MS) and compared between 70 MCI patients and 140 matched controls with normal cognition. The odds ratio (OR) was calculated using logistic analyses to assess the association between oxysterols and MCI.
Results
Compared with controls with normal cognition, plasma level of 27–OHC was significantly higher in MCI patients. Logistic analyses suggested high plasma level of 27–OHC was significantly associated with MCI even after multivariate adjustment (OR = 2.86, 95 % CI: 1.52 ~ 5.37).
Conclusions
Our findings suggested that the increased plasma level of 27-OHC was associated with MCI, suggesting high plasma levels of 27-OHC may pay an important role in the development of MCI.
Similar content being viewed by others
Background
Alzheimer’s disease (AD) is the most commonly recognized cause of dementia by memory loss and other intellectual symptoms serious enough to affect daily life in the elderly [1]. It contributes to premature death of elders after being diagnosed for 3 to 9 years [2]. MCI is the pre–clinical stage of AD with gradual cognitive decline but no influence on daily life activities. It is accepted that early intervention in MCI including decreasing the risk factors is useful and therefore many studies have focused on this stage [3].
Substantial epidemiological and molecular evidence has indicated that hypercholesterolemia is an important risk factor for neurodegenerative diseases [4]. However, clinical studies by using statins to lower the cholesterol for preventive and therapeutic management of neurodegeneration did not show the effects [5]. In addition, cholesterol in the blood cannot pass the blood brain barrier into central nervous system (CNS) [6]. The above facts cannot support the role of high plasma level of cholesterol in AD or MCI.
Oxysterols including 27–OHC, 24S–OHC, 7α–OHC and 7β–OHC are the oxidized derivatives of cholesterol, which can not only pass the blood brain barrier [7] but also have cytotoxic and pro-apoptotic properties [8, 9]. 27–OHC is the most abundant circulating oxysterol mainly produced in the liver [10]. Previous studies have also demonstrated an influx of the 27-OHC from the circulation into the brain [11]. Despite the fact that cholesterol cannot pass the blood–brain barrier, hypercholesterolemia is linked to an increased risk of neurodegenerative conditions including AD [12, 13], in particular in midlife [14]. Since there is a close correlation between circulating cholesterol and 27-OHC [15], hypercholesterolemia seems to result in an increased uptake of 27-OHC. Meanwhile, Heverin et al. [16] has demonstrated that treatment of mice with dietary cholesterol causes significant memory impairment and 27-OHC mediates the negative effects of dietary cholesterol on cognition. Therefore, there is possibility that 27-OHC is linking the excessive diet cholesterol or hypercholesterolemia and neurodegenerative conditions. A recent study showed a significant accumulation of 27–OHC in the brain of patients with AD [17]. In addition, one animal study showed the level of 27–OHC in 12–month–old rats is higher than that in 8–month–old rats, suggesting the accumulation of 27–OHC in the brain with age [18].
Despite the accumulated evidence about the relationship of oxysterols with neurodegenerative diseases such as AD, there are no direct data from humans to evaluate the relationship between oxysterols and MCI. The aim of this study was to evaluate plasma levels of 27–OHC, 24S–OHC, 7α–OHC and 7β–OHC in the elderly with and without MCI and attempt to establish potential relationships between these oxysterols and cognitive function.
Methods
Subjects and cognitive assessment
Seventy hospitalized subjects diagnosed as MCI and 140 controls with normal cognition were recruited from Xuan Wu Hospital in Beijing, China. The study design was ethically approved by the Ethics Committee of Capital Medical University (2013SY35). The process was explained for all subjects before the written informed consent was obtained. Controls were age- (±5 years), sex- and education- matched with MCI patients. The subjects with the history of a cerebrovascular event, malignant tumor and psychiatric illness or other neurological disease and statin or hypnotic sedative drugs abuse were excluded from the study. Cognitive function was evaluated by professional interviewers using the Mini–Mental State Examination (MMSE) [19] and Montreal Cognitive Assessment (MoCA) [20]. MMSE is commonly used to screen for dementia but insensitive to MCI while the MoCA was specially developed for detection of MCI [20]. All MCI patients should primarily satisfy the criteria of MCI including the following: (1) normal general cognitive function and absence of dementia that is sufficient to satisfy MMSE score of >19 for illiterate individuals, >22 for individuals with 1 to 6 years of education and >26 for individuals with 7 or more years of education; (2) mild impairment of cognitive functioning evaluated by MoCA score of ≤14 for illiterate individuals, ≤19 for individuals with 1 to 6 years of education and ≤24 for individuals with 7 or more years of education. If the subjects meet the above MCI criteria, they will visit a neurologist to make the final diagnosis.
Demographic, clinical and anthropometric assessment
Demographics (age, gender, education, weight and height), lifestyle habits (current smoking status and drinking status), history of hypertension, coronary heart disease, diabetes and cerebrovascular disease were collected by self–reported questionnaire. Body mass index (BMI) was calculated as weight (kg)/height2 (m2). Current smoking status and drinking status were binary variables. Subjects were classified as smokers if they reported smoking three or more cigarettes a week for more than six months before enrollment and non-smokers if their cigarettes consumption was lower than this. Drinkers were identified by reporting alcohol consumption three or more times a week for more than six months before enrollment and non-drinkers lower than this.
Laboratory measurements
The 0.6 mL tubes containing EDTA anticoagulant were used to collect fasting venous blood samples. The plasma samples were harvested after centrifugation at 3000 rpm for 10 min at 4 °C and stored frozen at −80 °C until measurement. The levels of plasma triglycerides (TG), total cholesterol (TC), high–density lipoprotein cholesterol (HDL–C), low-density lipoprotein cholesterol (LDL–C) and fasting blood glucose (FBG) were measured on a HITACHI 7600 analyzer. Aβ1-40 and Aβ1-42 plasma levels were evaluated by ELISA kit.
Plasma levels of oxysterols were measured using High Performance Liquid Chromatography–Mass Spectrometry (HPLC–MS) as described by Ines Burkard, et al. [21] with slight modifications. Briefly, 0.1 mL of plasma sample was transferred to a screw–capped vial and 100 ng of 19–hydroxycholesterol (19–OHC) was also added to the vial serving as internal standard. Alkaline hydrolysis was performed at 50 °C water bath for 2 h after adding 1.5 mL of 1 M ethanolic sodium hydroxide. Phosphoric acid (50 %) and 1 mL of phosphate buffer were added to the samples to adjust pH to 7. Supernatant was harvested after the centrifugation at 1000 g for 5 min and then applied to the C18 cartridges for solid–phase extraction. The eluted substances were dried at 30 °C and dissolved in 100 mL of methanol for future test. HPLC with an Angilent G1312B HPLC Pump and an Angilent C18 column (0.35 μm bead size; 4.6 × 250 mm) were used for the measurement of oxysterols. Quantification of oxysterols was performed using the multiple reaction monitoring (MRM) mode.
Statistical analysis
The data were expressed by means ± standard deviations for normally distributed continuous variables, medians (interquartile ranges) for non–normally distributed continuous variables and frequencies (percentages) for categorical variables. Independent t–test and Mann Whitney U test were used for continuous variables and Chi–square test for categorical variables to compare differences between MCI and control groups. 27–OHC, 24S–OHC, 7α–OHC and 7β–OHC levels were classified into high and low levels by their medians. Univariate conditional logistic regression was used to evaluate the association between four oxysterols (treated as categorical variables) and MCI risk. Multivariate analysis was used to adjust demographic, clinical and anthropometric characteristics. Spearman rank correlation test was calculated to assess correlation coefficients. And P < 0.05 was considered statistically significant. All of the statistical analyses were performed using SPSS (version 18.0).
Results
This study included 70 MCI patients (35 men and 35 women) and 140 controls with normal cognitive state (70 men and 70 women). Demographic and clinical characteristics of all the subjects were summarized in Table 1. Drinkers (P = 0.03), MoCA scores (P < 0.01), Aβ1-40 (P < 0.01) and Aβ1-42 (P < 0.01) were observed with significant differences between MCI and control group.
The plasma levels of four oxysterols were present in Table 2. There was significant difference between the two groups regarding the plasma 27–OHC levels but no significant differences in 24S–OHC, 7α–OHC and 7β–OHC levels.
Table 3 using univariate analysis showed that only high plasma level of 27-OHC was associated with MCI (OR = 3.21, 95 % CI: 1.76 ~ 5.85). Four oxysterols were classified into high and low levels by their medians.
Table 4 showed the significant association between high plasma level of 27-OHC and MCI persisted even after adjustment (OR = 2.86, 95 % CI: 1.52 ~ 5.37).
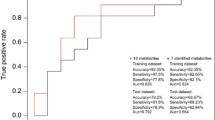
Spearman correlation analyses showed that the plasma level of 27-OHC was positively correlated with that of Aβ1-40 and Aβ1-42 and negatively correlated with MoCA scores (Fig. 1a–c).
Discussion
In these four oxysterols, 27–OHC is the major cholesterol metabolite in the circulation and mainly produced from cholesterol in periphery and synthesized in almost all cells by the cytochrome P-450 enzyme CYP27A1 located in the inner mitochondrial membranes. A significant association between high plasma level of 27-OHC and MCI was observed in this study. Our results were in accordance with the previous studies that described 27–OHC level in blood was negatively associated with cognitive performance in aging population and was significantly higher in AD patients [22, 23]. However, subjects with neurological diseases, such as AD or other types of dementia, were ruled out by exclusion criteria in our study for more reliable results prior to medication. There was also a negative correlation between plasma 27-OHC level and MoCA scores (r = − 0.269, P = 0.001). The negative correlation indicates that 27-OHC production in the blood is expected to increase with severity of cognitive impairment.
Previous research has indicated that subjects with high Aβ levels showed increased cognitive impairment [24]. Marwarhaet al [25] has found that 27-OHC induced 3-fold increase in Aβ1-42 and 1.5-fold increase in Aβ1-40 levels in the organotypic slices from rabbits. Moreover, Prasanthiet al [26] treated human neuroblastoma SH-SY5Y cells with 27-OHC and found a substantial increase in Aβ1-42 levels compared to untreated cells. Our study has also shown MCI patients had higher plasma Aβ1-40 and Aβ1-42 levels than controls with normal cognition (P <0.01). Simultaneously, a good positive correlation between plasma levels of Aβ1-42 and 27-OHC (r = 0.269, P = 0.005) and a weak but significant correlation of plasma 27-OHC with Aβ1-40 levels (r = 0.192, P = 0.048) were also observed, supporting the hypothesis that 27-OHC may enhance circulating amyloid production and increase the risk of cognitive impairment.
Despite that, studies analyzing the associations between plasma 27–OHC level and cognitive decline yielded conflicting results. Timothy M. Hughes et al. [27] recently found that the increase of plasma 27–OHC levels was related to cerebrovascular disease prior to cognitive decline over many years of follow–up. However, it lacked MRI results for cerebrovascular disease when the volunteers were diagnosed of AD or MCI in follow–up. Thus, the question arises whether cerebrovascular disease is the injury factor for cognitive status. In addition, a case–control study has shown that the ratio of 27–OHC to total circulating cholesterol (27–OHC/Chol) level is lower in AD and MCI patients than that in controls [28]. There is possibility that oxysterols and cholesterol compete for space within the lipoproteins and they have different scales on space within the lipoprotein, absolute levels of plasma 27–OHC may be higher in MCI compared to controls despite of the decrease of 27–OHC/Chol.
On the other hand, in the brain, cholesterol is removed by conversion to 24S–OHC via CYP46A1 enzyme, which is primarily expressed in neurons. We found no significant difference in 24S–OHC level in plasma between MCI patients and control group. In contrast to the former research, they observed significantly elevated or declined plasma levels of 24S–OHC in AD, vascular disease (VaD) and MCI participants [29, 30]. These conflicting findings may result from study population with different time after being diagnosed with MCI. The late MCI patients with the loss of neuronal cells had decreased level of 24S–OHC whereas the early MCI patients were characterized by the increase of 24S–OHC probably as a consequence of the released cholesterol caused by the myelin disruption [31].
Unlike 27–OHC and 24S–OHC, 7β–OHC is generated by non–enzymatic oxidation whereas 7α–OHC is generated by both non–enzymatic and enzymatic oxidation that is catalyzed by CYP7A1 [32]. The effects of 7α–OHC and 7β–OHC on cognitive function are less known. MCI falls in between normal forgetfulness and AD. It is accepted that early intervention in MCI including decreasing the risk factors is useful. Our findings has offered some valid epidemiological evidence to reveal the role of 27-OHC in the pathogenesis of MCI, which may provide new insights into the prevention of AD. Some experiments in cell cultures and animals have suggested increased levels of 27-OHC may trigger or accelerate progression of AD or MCI through a variety of mechanisms. However, efforts to find out the role of 27-OHC in AD or MCI are still necessary by further human studies. The strengths of our study was a matched case–control study after adjustment for confounders and based on standardized epidemiological methods. Additionally, we enrolled MCI patients without medication as the target population in order to more directly investigate the relationship with risk factors than AD patients and take preventive measures in the preclinical stage of AD. However, it was a case–control study that can not establish the timeline of exposure to disease outcome, prospective cohort studies are also needed to further evaluate the role of oxysterols in AD or MCI.
Conclusions
In conclusion, our findings suggested plasma level of 27-OHC was significantly higher in MCI patients than controls with normal cognition and the increased plasma level of 27-OHC was significantly associated with MCI. Prospective cohort studies and experiments in vitro are needed to further evaluate the potential role of 27-OHC and other oxysterols in involvement in AD or MCI.
Abbreviations
- 24S–OHC:
-
24S–hydroxycholesterol
- 27–OHC:
-
27–hydroxycholesterol
- 7α–OHC:
-
7α–hydroxycholesterol
- 7β–OHC:
-
7β–hydroxycholesterol
- AD:
-
Alzheimer’s disease
- HPLC–MS:
-
High Performance Liquid Chromatography–Mass Spectrometry
- MCI:
-
Mild cognitive impairment
References
Swaminathan A, Jicha GA. Nutrition and prevention of Alzheimer’s dementia. Front Aging Neurosci. 2014;6:282.
Li X, Song D, Leng SX. Link between type 2 diabetes and Alzheimer’s disease: from epidemiology to mechanism and treatment. Clin Interv Aging. 2015;10:549–60.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, Gamst A, Holtzman DM, Jagust WJ, Petersen RC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9.
Zambon D, Quintana M, Mata P, Alonso R, Benavent J, Cruz-Sanchez F, Gich J, Pocovi M, Civeira F, Capurro S, et al. Higher incidence of mild cognitive impairment in familial hypercholesterolemia. Am J Med. 2010;123(3):267–74.
McGuinness B, Craig D, Bullock R, Malouf R, Passmore P. Statins for the treatment of dementia. Cochrane Database Syst Rev. 2014;7:D7514.
Bjorkhem I, Meaney S. Brain cholesterol: long secret life behind a barrier. Arterioscler Thromb Vasc Biol. 2004;24(5):806–15.
Bjorkhem I, Cedazo-Minguez A, Leoni V, Meaney S. Oxysterols and neurodegenerative diseases. Mol Aspects Med. 2009;30(3):171–9.
Daugvilaite V, Arfelt KN, Benned-Jensen T, Sailer AW, Rosenkilde MM. Oxysterol-EBI2 signaling in immune regulation and viral infection. Eur J Immunol. 2014;44(7):1904–12.
Olkkonen VM, Beaslas O, Nissila E. Oxysterols and their cellular effectors. Biomolecules. 2012;2(1):76–103.
Lee WR, Ishikawa T, Umetani M. The interaction between metabolism, cancer and cardiovascular disease, connected by 27-hydroxycholesterol. Clin Lipidol. 2014;9(6):617–24.
Bjorkhem I. Crossing the barrier: oxysterols as cholesterol transporters and metabolic modulators in the brain. J Intern Med. 2006;260(6):493–508.
Launer LJ, White LR, Petrovitch H, Ross GW, Curb JD. Cholesterol and neuropathologic markers of AD: a population-based autopsy study. Neurology. 2001;57(8):1447–52.
Pappolla MA, Bryant-Thomas TK, Herbert D, Pacheco J, Fabra GM, Manjon M, Girones X, Henry TL, Matsubara E, Zambon D, et al. Mild hypercholesterolemia is an early risk factor for the development of Alzheimer amyloid pathology. Neurology. 2003;61(2):199–205.
Kivipelto M, Helkala EL, Laakso MP, Hanninen T, Hallikainen M, Alhainen K, Soininen H, Tuomilehto J, Nissinen A. Midlife vascular risk factors and Alzheimer’s disease in later life: longitudinal, population based study. BMJ. 2001;322(7300):1447–51.
Mateos L, Ismail MA, Gil-Bea FJ, Leoni V, Winblad B, Bjorkhem I, Cedazo-Minguez A. Upregulation of brain renin angiotensin system by 27-hydroxycholesterol in Alzheimer’s disease. J Alzheimers Dis. 2011;24(4):669–79.
Heverin M, Maioli S, Pham T, Mateos L, Camporesi E, Ali Z, Winblad B, Cedazo-Minguez A, Bjorkhem I. 27-hydroxycholesterol mediates negative effects of dietary cholesterol on cognition in mice. Behav Brain Res. 2015;278:356–9.
Shafaati M, Marutle A, Pettersson H, Lovgren-Sandblom A, Olin M, Pikuleva I, Winblad B, Nordberg A, Bjorkhem I. Marked accumulation of 27-hydroxycholesterol in the brains of Alzheimer’s patients with the Swedish APP 670/671 mutation. J Lipid Res. 2011;52(5):1004–10.
Jenner AM, Lim WL, Ng MP, Wenk MR, Shui G, Sharman MJ, Gandy SE, Martins RN. The effect of APOE genotype on brain levels of oxysterols in young and old human APOE epsilon2, epsilon3 and epsilon4 knock-in mice. Neuroscience. 2010;169(1):109–15.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Lu J, Li D, Li F, Zhou A, Wang F, Zuo X, Jia XF, Song H, Jia J. Montreal cognitive assessment in detecting cognitive impairment in Chinese elderly individuals: a population-based study. J Geriatr Psychiatry Neurol. 2011;24(4):184–90.
Burkard I, Rentsch KM, von Eckardstein A. Determination of 24S- and 27-hydroxycholesterol in plasma by high-performance liquid chromatography-mass spectrometry. J Lipid Res. 2004;45(4):776–81.
van den Kommer TN, Dik MG, Comijs HC, Lutjohann D, Lips P, Jonker C, Deeg DJ. The role of extracerebral cholesterol homeostasis and ApoE e4 in cognitive decline. Neurobiol Aging. 2012;33(3):617–22.
Leoni V, Masterman T, Mousavi FS, Wretlind B, Wahlund LO, Diczfalusy U, Hillert J, Bjorkhem I. Diagnostic use of cerebral and extracerebral oxysterols. Clin Chem Lab Med. 2004;42(2):186–91.
Llado-Saz S, Atienza M, Cantero JL. Increased levels of plasma amyloid-beta are related to cortical thinning and cognitive decline in cognitively normal elderly subjects. Neurobiol Aging. 2015;36(10):2791–7.
Marwarha G, Dasari B, Prasanthi JR, Schommer J, Ghribi O. Leptin reduces the accumulation of Abeta and phosphorylated tau induced by 27-hydroxycholesterol in rabbit organotypic slices. J Alzheimers Dis. 2010;19(3):1007–19.
Prasanthi JR, Huls A, Thomasson S, Thompson A, Schommer E, Ghribi O. Differential effects of 24-hydroxycholesterol and 27-hydroxycholesterol on beta-amyloid precursor protein levels and processing in human neuroblastoma SH-SY5Y cells. Mol Neurodegener. 2009;4:1.
Hughes TM, Kuller LH, Lopez OL, Becker JT, Evans RW, Sutton-Tyrrell K, Rosano C. Markers of cholesterol metabolism in the brain show stronger associations with cerebrovascular disease than Alzheimer’s disease. J Alzheimers Dis. 2012;30(1):53–61.
Kolsch H, Heun R, Kerksiek A, Bergmann KV, Maier W, Lutjohann D. Altered levels of plasma 24S- and 27-hydroxycholesterol in demented patients. Neurosci Lett. 2004;368(3):303–8.
Papassotiropoulos A, Lutjohann D, Bagli M, Locatelli S, Jessen F, Rao ML, Maier W, Bjorkhem I, von Bergmann K, Heun R. Plasma 24S-hydroxycholesterol: a peripheral indicator of neuronal degeneration and potential state marker for Alzheimer’s disease. Neuroreport. 2000;11(9):1959–62.
Lutjohann D, Papassotiropoulos A, Bjorkhem I, Locatelli S, Bagli M, Oehring RD, Schlegel U, Jessen F, Rao ML, von Bergmann K, et al. Plasma 24S-hydroxycholesterol (cerebrosterol) is increased in Alzheimer and vascular demented patients. J Lipid Res. 2000;41(2):195–8.
Hughes TM, Rosano C, Evans RW, Kuller LH. Brain cholesterol metabolism, oxysterols, and dementia. J Alzheimers Dis. 2013;33(4):891–911.
Saito Y, Noguchi N. 7-Hydroxycholestrol as a possible biomarker of cellular lipid peroxidation: difference between cellular and plasma lipid peroxidation. Biochem Biophys Res Commun. 2014;446(3):741–4.
Acknowledgements
Not applicable.
Funding
The research was supported by the State Key Program of the National Natural Science Foundation of China (Grant No. 81330065).
Availability of data and materials
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Authors’ contributions
RX: conceived and designed the study; QL, YA and HY: measured the oxysterols, analyzed experimental results and wrote the manuscript; YL, CW and LF: assessed cognitive function of all the subjects. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
All the co-authors and participants have gave their consent for publication in Lipids in Health and Disease.
Ethics approval and consent to participate
The study design was ethically approved by the Ethics Committee of Capital Medical University (2013SY35). All participants were provided written informed consent at the beginning of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Liu, Q., An, Y., Yu, H. et al. Relationship between oxysterols and mild cognitive impairment in the elderly: a case–control study. Lipids Health Dis 15, 177 (2016). https://doi.org/10.1186/s12944-016-0344-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-016-0344-y