Abstract
Background
COVID-19 has been characterised by its global and rapid spread, with high infection, hospitalisation, and mortality rates worldwide. However, the course of the pandemic showed differences in chronology and intensity in different geographical areas and countries, probably due to a multitude of factors. Among these, socio-economic deprivation has been supposed to play a substantial role, although available evidence is not fully in agreement. Our study aimed to assess incidence and fatality rates of COVID-19 across the levels of socio-economic deprivation during the first epidemic wave (March–May 2020) in the Italian Province of Foggia, Apulia Region.
Methods
Based on the data of the regional active surveillance platform, we performed a retrospective epidemiological study among all COVID-19 confirmed cases that occurred in the Apulian District of Foggia, Italy, from March 1st to May 5th, 2020. Geocoded addresses were linked to the individual Census Tract (CT) of residence. Effects of socio-economic condition were calculated by means of the Socio-Economic and Health-related Deprivation Index (SEHDI) on COVID-19 incidence and fatality.
Results
Of the 1054 confirmed COVID-19 cases, 537 (50.9%) were men, 682 (64.7%) were 0–64 years old, and 338 (32.1%) had pre-existing comorbidities. COVID-19 incidence was higher in the less deprived areas (p < 0.05), independently on age. The level of socio-economic deprivation did not show a significant impact on the vital status, while a higher fatality was observed in male cases (p < 0.001), cases > 65 years (p < 0.001), cases having a connection with a nursing home (p < 0.05) or having at least 1 comorbidity (p < 0.001). On the other hand, a significant protection for healthcare workers was apparent (p < 0.001).
Conclusions
Our findings show that deprivation alone does not affect COVID-19 incidence and fatality burden, suggesting that the burden of disease is driven by a complexity of factors not yet fully understood. Better knowledge is needed to identify subgroups at higher risk and implement effective preventive strategies.
Similar content being viewed by others
Background
The Coronavirus Disease 2019 (COVID-19) pandemic has caused substantial morbidity and mortality worldwide. As of June 1st 2020, 233,607 cases of confirmed Severe Acute Respiratory Syndrome coronavirus 2 (SARS-COV-2) infection were reported in Italy with a case fatality rate of 13.8% [1].
Despite the widespread opinion that the novel coronavirus has not discriminated, SARS-CoV-2 infection, like many other infectious diseases, seems to have affected predominantly the portion of the population in socio-economic disadvantage. Indeed, many studies have demonstrated disproportionate morbidity and mortality among socioeconomically disadvantaged population groups with higher hospitalisation and death rates among neighbourhoods with the highest proportion of ethnic minorities and individuals living in poverty [2,3,4,5,6,7,8,9,10,11,12,13,14]. On the other hand, a minority of studies did not show these associations or even reported conflicting results [15,16,17,18,19,20].
Several factors may have contributed to the observed inequality including the level of education, the overrepresentation of minorities in public-facing occupations, overcrowded living and working conditions, inappropriate information, and prevalence of pro-inflammatory unhealthy lifestyle [21,22,23,24]. All these factors negatively affect the overall health conditions and are correlated with an increased risk of several diseases such as cardiovascular diseases, diabetes, chronic respiratory diseases, and some cancers, which in turn may have increased COVID-19 incidence and mortality risk [25, 26]. The extent to which these disparities have been related to socio-economic versus biological factors still needs further understanding [4, 27]. Indeed, the knowledge gathered during the course of the pandemic investigated the complexity of the factors involved and distinguished four potential pathways: vulnerability (the burden of pre-existing health conditions), susceptibility (the status of the immune function), level of exposure (e.g., working or travelling conditions), and risk of transmission (e.g., due to crowded housing) [28].
The analysis of the Italian National Institute of Statistics (Istat) on the effect of socio-economic disparities in COVID-19 mortality demonstrated that during the first quarter of 2020, alongside an overall increase of the crude mortality rate, a more pronounced increase in mortality rate was observed among the most disadvantaged groups [25]. Istat data collected during the successive waves confirm the amplification effect of inequalities ascribable to the pandemic and its negative impact on mortality [26, 29]. A study conducted in the Emilia Romagna Region confirmed that people living in the most disadvantaged census block were exposed to an increased risk of both overall and COVID-19-related mortality during the first epidemic peak [30].
In such context, collection and analysis of socio-economic data appeared necessary to examine a potential disproportionate burden of COVID-19 across the different population subgroups. Deprivation indexes are useful measures for health inequalities analysis by identifying and evaluating the relationships between socio-economic status (SES) and health conditions. These indexes usually refer to geographical aggregations and are used as a proxy of the individual’s conditions according to the area of residence [31, 32].
By using deprivation indexes, our study aimed to assess the impact of socio-economic deprivation on the incidence and fatality of COVID-19 during the first epidemic wave (March–May 2020) in the Italian Province of Foggia, Apulia Region.
Methods
This study involved all the 1054 cases laboratory confirmed as SARS-CoV-2 positive by real-time RT-PCR, regardless of the presence of symptoms or patient management (hospitalised or managed at home), that were recorded in the Foggia province (Apulia region, Southern Italy) from March 1st to May 5th, 2020. The cases were selected and followed-up for the same period, as previously described [33, 34].
In particular, the following case characteristics were considered: sex, age, health status at the end of the follow-up, and presence/absence of at least one comorbidity (specifically: cancer, diabetes, cardiovascular diseases, HIV infection, chronic lung diseases, kidney diseases, other metabolic diseases, obesity two subgroups: BMI between 30 and 40 kg/m2 or BMI > 40 kg/m2, liver diseases, neurological diseases, other diseases).
Additionally, the belonging to the healthcare personnel of public or private healthcare system and/or the connection with a nursing home (both as a patient or a care worker) were also recorded.
In order to attribute to every case his/her Census Tract (CT) of residence (referred to the 2011 Population and Housing National Census [35]), the individual complete residence address and X&Y Cartesian coordinates were collected and checked by the Geographic information system (GIS) procedure [32, 36, 37] (Fig. 1).
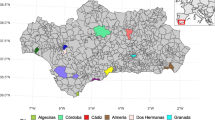
Information on the socio-economic condition of the cases was computed at CT level for the Foggia province and the Socio-Economic and Health-related Deprivation Index (SEHDI) was calculated as previously described [32, 38]. In particular, the SEHDI is able to highlight the relevance of the social aspects of deprivation (e.g., older age, availability of familial network and social support, etc.) when considering how a population cope with the disease spreading, prevention, or patient care, considering the peculiarities of the local area where it is calculated. We set the older age threshold at age 65 based on socioeconomic considerations (e.g., health status, retirement age) in line with previous published studies [32, 38]. Factors and variables composing the SEHDI 2011 are presented in Table 1 and Fig. 2. Due to some errors in the geographical data of 10 cases, the SEHDI score and classification were attributed to 1,044 cases (99.1% of all cases).
The SEHDI was computed as a score from 0 (lowest deprivation) to 100 (highest deprivation) attributed to all population and re-classified in 5 groups (from 1 = High deprivation to 5 = Low deprivation), in which the population has been normally distributed across the groups, according to the Agnelli-Cadeiras algorithm [32, 39].
The incidence of COVID-19 was examined by Standardised Incidence Ratio (SIR; SIRs were standardised on the 2011 overall provincial population [40]). The effects of the socio-economic deprivation on the incidence were analysed by Analysis of Variance (ANOVA) of the SIRs trend through the 5 deprivation groups (F test with statistical significance threshold at p < 0.05) [41].
The vital status (alive/dead at the end of follow-up) by personal characteristics and comorbidities was examined by two-way tables, considering the percentage by row and computing the χ2 as connection index (statistical significance at p < 0.05) [41]. The potential effects of the individual characteristics and classification by SEHDI on the vital status at the end of follow-up were analysed by multilevel mixed-effects logistic regression model (vital status as dependent variable, personal characteristics as individual fixed-effects covariates, SEHDI groups as the area random-effects covariates). The reliability and statistical significance of the model were tested by log likelihood ratio and comparison with χ2 (statistical significance at p < 0.05) [41]. All the procedures (GIS and statistical analyses) were performed by QGIS 3.10 and Stata 14.0 software.
Results
Table 1 reports the census variables composing the SEHDI factors, the variance explained by each factor, and the total explained variance. The distribution of old-age index and the distribution by age groups, sex and deprivation clusters individuated by the SEHDI 2011 are also reported. The SEHDI factors pertained to the domains which are classically recognised as linked to the socio-economic status of a population: the family structure, the household characteristics, and the education level. In terms of family structure (factor 1), it was included variables highlighting the difficulties of single-person households, particularly if composed by an elderly individual living alone. Furthermore, factor 2 described the dwelling conditions (i.e., the percentage of houses with a bath or a shower), factor 3 emphasised the association between deprivation and low educational level, while factor 4 considered the percentage of separated and divorced persons. The analysed population of Foggia province (n = 626,072) was quite young (the 81.2% was younger than 65 years). Among the elderly, the percentage of women was slightly prevalent than that of men (n = 66,946, 10.7% vs. n = 50,887, 8.1%). The population distribution by deprivation groups differed in age and sex: lower deprivation was associated with younger age while higher deprivation was more frequently observed in the elderly, mostly in women. The old-age index distribution showed a statistically significant positive linear trend (values increased as deprivation grew).
Figure 2 represents the distribution of CTs by SEHDI groups in the Foggia province and in the capital city (Foggia municipality). The presence of high and medium–high deprivation groups was higher within the Foggia municipality and in the proximity of the other main municipalities of the province (Cerignola, Lucera, and San Severo). In Foggia municipality, the proximity and the higher concentration of the most deprived groups were evident, mainly in the Southern part of the city centre.
Table 2 shows the characteristics of COVID-19 cases, along with the distribution by sex, age, and deprivation groups, as a descriptive comparison with the overall province population. Both case distribution and population distribution by sex were well-balanced in the province. On the contrary, the case distribution by age differed from the overall population distribution: the percentage of elderly (≥ 65 years old) among COVID-19 cases was 35.3% compared with 18.6% among the provincial population.
Additionally, differences were observed in the distributions across deprivation groups: the majority of COVID-19 cases were resident in the least deprived areas, while the provincial population was distributed on a Gaussian basis by methodological definition. Moreover, among COVID-19 cases the percentage of individuals having a connection with nursing facilities was low (16.8%) while the percentage of healthcare system employees was slightly higher (27.9%). Lastly, the case fatality rate was 12.3%.
Table 3 provides a more complete description of the COVID-19 case group: 338 of 1054 cases (32.1%) had pre-existing comorbidities, most of which were significantly linked to ageing (p < 0.05; cancer, diabetes, cardiovascular disease, chronic lung diseases, kidney diseases, other metabolic diseases, liver diseases, neurological diseases, other diseases), while obesity and HIV infection were not related to ageing. No direct correlation between deprivation and comorbidities was observed.
The effects of socio-economic deprivation on the incidence of COVID-19 are presented in Table 4. The distribution of SIRs in the overall population and by sex, age groups, and age by sex were analysed across the five SEHDI clusters. It was confirmed that COVID-19 incidence was higher in the least deprived individuals with a statistically significant negative linear trend (p < 0.05). Similar trends were observed when two different age groups were considered (<65 or ≥65 years old). When comparing each sex with the age by sex, the same trend was maintained in men regardless of the age group while in the female population the same trend was maintained only in the younger group (0–64 years old) (p < 0.05).
The effects of individual characteristics and socio-economic deprivation on the vital status of cases at the end of the follow-up period are shown in Tables 5 and 6. A higher fatality was observed in male cases (15.6% males vs. 8.9% females), elderly cases (31.2% in over-65s vs. 2.1% in under-65s), cases having a connection with a nursing home as guests or staff members (17.5% with connection vs. 11.8% without connection), and cases affected by at least one comorbidity (24% with comorbidities vs. 6.8% without comorbidities) (p < 0.05). No statistically significant effect was associated with the socio-economic status. Significant protection was observed for healthcare workers (16.8% of deaths in non-healthcare workers vs. 0.7% in healthcare workers; p < 0.001).
The model in Table 6 enables a better evaluation of the impact of every covariate on the risk of death. Age was the main determinant of the risk of death (OR = 14.6; p < 0.001); moreover, being male or having at least one comorbidity significantly increased the risk of death (OR = 2.3 and 2.2, respectively; p < 0.01). On the contrary, having a connection with a nursing home was not statistically significant with regard to the risk of mortality, while being employed in the healthcare system showed a significant association with the alive status (p = 0.004).
The socio-economic status was analysed as a random effect attributed by the SEHDI of the CT of residence to each corresponding case: a statistically significant effect was found, with an increase in the probability of death with increasing deprivation. Finally, a weak statistically significant stochastic effect, expressed by the constant, was found, which increased the chances of death. The model was stable, as stated by the log-likelihood ratio and its tests (p = 0.000).
Discussion
COVID-19 is widespread diffused, but many studies and reports worldwide have demonstrated that risk of infection and outcomes are socially patterned with the most deprived population groups usually experiencing the worst outcomes [2,3,4,5,6,7,8,9,10,11,12,13,14]. A narrative review of 42 studies, all focused on the first pandemic wave, found an association between socio-economic deprivation and an increased likelihood of contracting COVID-19; the strongest evidence was arisen from three large observational studies. The other compelling association was observed with regard to race or ethnicity [42]. On the other hand, a minority of studies, a number of which incidentally were conducted in Italy, did not show such association or even reported opposing results [15,16,17,18,19,20].
By using the SEHDI, our study allowed us to validly and reliably identify the main factors related to socio-economic deprivation, as demonstrated by the high total explained variance value (74.2%), and to study their impact on COVID-19 incidence and fatality.
The factors and census variables composing the SEHDI included in this analysis were the family structure, the characteristics of the house and the education level, which are known to be associated with the socio-economic status of the population [43]. In particular, the main determinants of socio-economic status considered in our study were: single-member household composition, older age, housing conditions and lower education level.
In agreement with the literature [44], most of the census variables considered in our study highlighted the discomfort of single-member families, especially those composed by an elderly individual due to their greater need for both domestic and personal care.
Regarding the housing conditions, it is well known that adequate housing and hygiene conditions are essential for preventing or limiting the spread of respiratory infections [45]. Indeed, overcrowding living conditions and poor-quality housing challenge social distancing increasing the risk of COVID-19 transmission [2, 3, 8, 22].
In terms of education level, it is well known that low education level negatively impacts health and is correlated with a higher incidence of chronical non-communicable diseases (e.g., cardiovascular diseases, diabetes, respiratory chronic diseases, cancer), which in turn may increase the susceptibility to COVID-19 infection and related mortality [25, 26, 46]. Additionally, low education is often associated with elementary occupations, which have been demonstrated to be correlated with a particularly high rate of mortality from COVID-19 [22]. Furthermore, education is recognised as a strong factor influencing health literacy and correct health behaviours both overall and in the specific COVID-19 context [47,48,49]. During the first epidemic wave in Italy, the already existing mortality gap between the high and low education level population groups further increased and individuals with lower education level were more exposed to those factors increasing COVID-19 mortality risk [50].
In our study, the most deprived groups lived in the capital city and the main municipalities of Foggia province, where the majority of the elderly population resided. Within the Foggia municipality, the most deprived area was the old part of the city (Southern part of the city centre), which is at a longer distance from healthcare services and has restricted availability of public transport [32]. The lower accessibility to healthcare facilities is known to influence health service utilisation and delay patients care affecting health outcomes [51, 52].
Our study showed that the majority of COVID-19 cases were aged 0–64 years, belonged to medium–low/low deprivation groups, were not employed in the healthcare system and did not have a connection with a nursing home. As for the lack of correlation between COVID-19 and high deprivation observed in our study, which is in disagreement with a part of the literature, a potential explanation behind the observed discrepancy may be the younger age of the population living in the least deprived areas of the Foggia province. Younger individuals may be more exposed to the virus due to occupational and recreational reasons. The younger age of COVID-19 cases was also confirmed by the low connection with nursing homes, the low number of resulting deaths and the low number of comorbidities in the COVID-19 case group.
Secondly, a lower ethnic heterogeneity of the Foggia population compared with most studies in the literature may have removed one of the main determinants of COVID-19 differential susceptibility (i.e., presence of racial minorities). Indeed, most studies in the literature have been conducted in the UK and US, countries with an extremely high ethnic heterogeneity [3,4,5,6, 8,9,10, 21]. Findings from a later phase of the pandemic confirm the different impact of deprivation and ethnicity [53].
Also the SIR distributions by sex, age and age by sex across the SEHDI groups confirmed that the incidence of COVID-19 increased with decreasing deprivation and was higher in the 0–64 year age group. Furthermore, a higher incidence of COVID-19 in men compared with women emerged from our study. Sex disparity in COVID-19 incidence and mortality has extensively been documented in the literature. Women seem to mount a stronger immune response to infections, being protected by oestrogens and being more inclined to preventive care, healthy lifestyle, and hand hygiene [54,55,56].
The lack of association between fatality and socio-economic status of COVID-19 cases observed in our study is in disagreement with some studies [2,3,4,5,6,7,8,9,10,11,12,13,14]. Compared with the other European countries, the Italian population is known to be less affected by mortality-related social inequalities thanks to the protection of the Mediterranean diet, family support and the universal character of the healthcare system [50, 57]. As opposed to our study, the similar Italian study conducted by Di Girolamo et al. in the Emilia Romagna region demonstrated a higher mortality burden in the most deprived areas of the region. [30]. This discrepancy could be explained by the different pattern of diffusion of COVID-19 and different COVID-19 case fatality rate during the first epidemic wave between the two Italian regions which prevent a meaningful comparison of the data. Based on the ISS-Istat report published on March 2021, 26,564 COVID-19 cases and 4238 COVID-19 deaths were reported in the Emilia Romagna region compared with 4804 cases and 537 deaths in the Apulia region during the first epidemic wave (March–May 2020) [25, 26]. During this period, the percentage of COVID-19 deaths observed in the Emilia Romagna region over the total of COVID-19-related deaths in Italy was nearly 8 times higher compared with the number reported in the Apulia region [50].
Knowledge gained as the epidemic progressed revealed that the impact of deprivation on COVID-19 outcomes has been different in the subsequent waves and varied from country to country. Studies conducted in Spain, Belgium, and Germany, observed, from the first to the last wave, an increasingly detrimental trend for the deprived subgroups or even a small advantage in terms of incidence from living in a disadvantaged area. [17, 20, 58]. These findings differ from what has been observed in the UK, where incidence during the second wave increased more in less deprived areas than in more deprived areas [59].
Multiple factors have been invoked to account for this variability, some of which, such as the diffusion of knowledge of the risk factors and the adoption of preventive behavior related to individual awareness, are inversely related to deprivation level [17, 30]. Furthermore, fake news and conspiracy theories rapidly spread online during the first wave of the COVID-19 pandemic generating confusion and insecurity among the population and potentially leading to serious implications for the individual and community [60,61,62,63]. Such misinformation regarded an exaggeration by the experts about the disease severity and the extent of virus spread, and the cause of the disease itself, among other factors [60, 61]. In such a context of misinformation, the education level appears to have contributed to health inequality as communities with lower education levels are more likely to believe in fake news leading to an increased risk of SARS-CoV-2 infection or worse disease outcome [64,65,66,67].
A study that followed the entire evolution of pandemic in the Apulia Region [19] suggests that deprivation has a greater impact the greater is the viral circulation and the fewer are the restrictions. In our study, the burden of deprivation may have been somewhat mitigated due to the fact that we addressed the first wave, when a total lockdown was imposed and when Apulia was a region with a low incidence compared to other Italian regions.
Furthermore, the lack of correlation between socio-economic status and COVID-19 fatality observed in our study may be explained with the higher incidence of COVID-19 among the least deprived population groups of the Foggia district, which may be more exposed to SARS-CoV-2 virus for occupational reasons (e.g. work-related travel to high risk areas) and lifestyle. This portion of the population resides in urban areas with prompt access to healthcare facilities and live in better conditions. Another explanation for the lack of association between fatality and socio-economic status could be the younger age of COVID-19 cases, that represents an enhancement in the survival probability.
Similarly, Gadeyne et al. reported [15], during the first COVID-19 wave in Belgium, higher excess mortality among certain subgroups, specifically high-income men aged 25–64 years, middle- and high-income men and women aged 65–84 years, and non-resident men and women aged 85 years and over. These results were ascribed to an increased risk of infection through leisure and work-related travel for the younger, affluent, and active subgroup, and to the interfamilial exposure and transmission for the older subgroup.
On the other hand, a significantly lower case fatality rate among healthcare workers (0.7% in the healthcare worker group vs. 16.8% in the non-healthcare worker group) emerged from our study. This is in line with the overall Italian trend and may be explained by more frequent testing of healthcare workers compared with the general population enabling faster detection of asymptomatic or mildly symptomatic cases [1]. A low case fatality rate among healthcare workers has also been reported worldwide by a systematic review and meta-analysis including 594 records [68].
This work has some strengths and limitations. The robust model adopted providing an accurate picture of the Foggia population by SEHDI alongside a detailed analysis of the main socio-economic, demographic and clinical factors that could have an impact on COVID-19 incidence and fatality may be considered a strength. Furthermore, the low ethnic heterogeneity of the Foggia population may have limited the weight of a determinant which was not the subject of our analysis.
A major limitation is the unavailability of the number of people tested, rather than of positive cases. It has been reported that disadvantaged people are less likely to be tested and more likely to test positive, be hospitalised or die [12, 58]. This seems to have been particularly prevalent during the first wave due to the scarcity of testing, [13, 14, 17, 58] which was reserved to symptomatic or moderate-severe cases and could represent a bias masking/underestimating the actual incidence of COVID-19 cases among the most deprived population.
Another limitation, though shared with the most studies evaluating the relation between deprivation and COVID-19 dynamics, is the adoption of a composite measure of deprivation, with the intrinsic difficulty to discriminate the role of each factor contributing to the SEHDI score.
Conclusion
Our study did not support the hypothesis that the COVID-19 incidence and fatality burden are always heavier in the most deprived areas and provides a further contribution to the available literature whose findings are not fully consistent. Several reasons may support the reported discrepancy, including differences in population age distribution, population ethnic composition, estimation of viral circulation, COVID-19 incidence rates, and type of healthcare system. Furthermore, especially during the earlier phase of the pandemic, infection risk and outcome may be more strongly associated to behavioural aspects like social contacts and working conditions, both potentially correlated to low deprivation patterns. Further research is needed to better understand the correlation between COVID-19 incidence/mortality and socio-economic status and identify the underlying mechanisms. This better understanding could help adapt and tailor preventive strategies according to the vulnerability of certain population subgroups in order to reduce social and healthcare inequalities generated by the pandemic.
Availability of data and materials
The authors declare that the data supporting the findings of this study are available within the article and upon reasonable request and with permission of Apulian Public Health Authority.
Abbreviations
- ANOVA:
-
Analysis of variance
- COVID-19:
-
Coronavirus Disease 2019
- CS:
-
Census Tract
- GIS:
-
Geographic information system
- OR:
-
Odds ratio
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome coronavirus 2
- SES:
-
Socio-economic status
- SEHDI:
-
Socio-Economic and Health-related Deprivation Index
- SIR:
-
Standardised Incidence Ratio
References
Italian National Institute of Heath (Istituto Superiore di Sanità). COVID-19 integrated surveillance: key national data (Sorveglianza integrata COVID-19: archivio dei principali dati nazionali). https://www.epicentro.iss.it/coronavirus/sars-cov-2-sorveglianza-dati-archivio. Accessed 5 Oct 2022.
Das A, Ghosh S, Das K, Basu T, Dutta I, Das M. Living environment matters: unravelling the spatial clustering of COVID-19 hotspots in Kolkata megacity. India Sustain Cities Soc. 2021;65:102577.
Hatef E, Chang H-Y, Kitchen C, Weiner JP, Kharrazi H. Assessing the impact of neighborhood socioeconomic characteristics on COVID-19 prevalence across seven States in the United States. Front Public Health. 2020;8:571808.
Patel AP, Paranjpe MD, Kathiresan NP, Rivas MA, Khera AV. Race, socioeconomic deprivation, and hospitalization for COVID-19 in English participants of a National Biobank. Int J Equity Health. 2020. https://doi.org/10.1186/s12939-020-01227-y.
Hull SA, Williams C, Ashworth M, Carvalho C, Boomla K. Prevalence of suspected COVID-19 infection in patients from ethnic minority populations: a cross-sectional study in primary care. Br J Gen Pract. 2020;70:e696-704.
Ingraham NE, Purcell LN, Karam BS, Dudley RA, Usher MG, Warlick CA, et al. Racial and ethnic disparities in hospital admissions from COVID-19: determining the impact of neighborhood deprivation and primary language. J Gen Intern Med. 2021;36:3462–70.
Lewis NM, Friedrichs M, Wagstaff S, Sage K, LaCross N, Bui D, et al. Disparities in COVID-19 incidence, hospitalizations, and testing, by area-level deprivation—Utah, March 3–July 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1369–73.
Madhav KC, Oral E, Straif-Bourgeois S, Rung AL, Peters ES. The effect of area deprivation on COVID-19 risk in Louisiana. PLoS ONE. 2020;15:e0243028.
Mourad A, Turner NA, Baker AW, Okeke NL, Narayanasamy S, Rolfe R, et al. Social disadvantage, politics, and severe acute respiratory syndrome coronavirus 2 trends: a county-level analysis of United States data. Clin Infect Dis. 2021;72:e604–7.
Nicodemo C, Barzin S, Cavalli N, Lasserson D, Moscone F, Redding S, et al. Measuring geographical disparities in England at the time of COVID-19: results using a composite indicator of population vulnerability. BMJ Open. 2020;10:e039749.
Woodward M, Peters SAE, Harris K. Social deprivation as a risk factor for COVID-19 mortality among women and men in the UK Biobank: nature of risk and context suggests that social interventions are essential to mitigate the effects of future pandemics. J Epidemiol Community Health. 2021;75:1050–5.
Riou J, Panczak R, Althaus CL, Junker C, Perisa D, Schneider K, et al. Socioeconomic position and the COVID-19 care cascade from testing to mortality in Switzerland: a population-based analysis. Lancet Public Health. 2021;6(9):e683–91.
Politi J, Martín-Sánchez M, Mercuriali L, Borras-Bermejo B, Lopez-Contreras J, Vilella A, et al. Epidemiological characteristics and outcomes of COVID-19 cases: mortality inequalities by socio-economic status, Barcelona, Spain, 24 February to 4 May 2020. Euro Surveill. 2021;26:2001138.
Vandentorren S, Smaïli S, Chatignoux E, Maurel M, Alleaume C, Neufcourt L, et al. The effect of social deprivation on the dynamic of SARS-CoV-2 infection in France: a population-based analysis. Lancet Public Health. 2022;7:e240–9.
Gadeyne S, Rodriguez-Loureiro L, Surkyn J, Van Hemelrijck W, Nusselder W, Lusyne P, Vanthomme K. Are we really all in this together? The social patterning of mortality during the first wave of the COVID-19 pandemic in Belgium. Int J Equity Health. 2021;20:258.
Abedi V, Olulana O, Avula V, et al. Racial, economic, and health inequality and COVID-19 infection in the United States. J Racial Ethn Health Disparities. 2021;8(3):732–42.
Meurisse M, Lajot A, Devleesschauwer B, Van Cauteren D, Van Oyen H, Van den Borre L, Brondeel R. The association between area deprivation and COVID-19 incidence: a municipality-level spatio-temporal study in Belgium, 2020–2021. Arch Public Health. 2022;80:109.
Mateo-Urdiales A, Fabiani M, Rosano A, Rosano A, Vescio MF, Del Manso M, et al. Socioeconomic patterns and COVID-19 outcomes before, during and after the lockdown in Italy (2020). Health Place. 2021;71:102642.
Bartolomeo N, Giotta M, Tafuri S, Trerotoli P. Impact of socioeconomic deprivation on the local spread of COVID-19 cases mediated by the effect of seasons and restrictive public health measures: a retrospective observational study in Apulia Region, Italy. Int J Environ Res Public Health. 2022;19:11410.
Wachtler B, Michalski N, Nowossadeck E, Diercke M, Wahrendorf M, Santos-Hövener C, et al. Socioeconomic inequalities in the risk of SARS-CoV-2 infection—first results from an analysis of surveillance data from Germany. J Health Monit. 2020;5(Suppl 7):18–29.
Lassale C, Gaye B, Hamer M, Gale CR, Batty GD. Ethnic disparities in hospitalisation for COVID-19 in England: the role of socioeconomic factors, mental health, and inflammatory and pro-inflammatory factors in a community-based cohort study. Brain Behav Immun. 2020;88:44–9.
Marmot M, Allen J, Goldblatt P, Herd E, Morrison J. Build back fairer: The COVID-19 Marmot review. The pandemic, socioeconomic and health inequalities in England. London: Institute of Health Equity. 2020. https://www.health.org.uk/sites/default/files/upload/publications/2020/Build-back-fairer-the-COVID-19-Marmot-review.pdf. Accessed 5 Oct 2022.
Kelly-Irving M. Health inequalities & Covid-19: The situation in France. 2020. https://www.who.int/docs/default-source/documents/social-determinants-of-health/health-inequalities-covid-19---the-situation-in-france-(michelle-kelly-irving).pdf. Accessed 5 Oct 2022.
Valentine N. Extent, scope and impacts of COVID-19 on health inequalities: the evidence. World Health Organization (WHO). 2020. https://www.who.int/docs/default-source/documents/social-determinants-of-health/overview---covid-19-impacts-(nicole-valentine).pdf. Accessed 5 Oct 2022.
Italian Central Statistics Institute (Istituto Nazionale di Statistica). Istat Rapporto Annuale 2020. Sanità e salute di fronte all’emergenza COVID-19. https://www.istat.it/storage/rapporto-annuale/2020/capitolo2.pdf. Accessed 5 Oct 2022.
Italian Central Statistics Institute (Istituto Nazionale di Statistica). Istat Rapporto Annuale 2021. La situazione del Paese. https://www.istat.it/storage/rapporto-annuale/2021/Rapporto_Annuale_2021.pdf. Accessed 5 Oct 2022.
Moissl AP, Lorkowski S, März W. Socio-economic deprivation and COVID-19 in Germany. Scand J Public Health. 2022;50:668–70.
Hoebel J, Michalski N, Diercke M, Hamouda O, Wahrendorf M, Dragano N, Nowossadeck E. Emerging socio-economic disparities in COVID-19-related deaths during the second pandemic wave in Germany. Int J Infect Dis. 2021;113:344–6.
Italian Central Statistics Institute (Istituto Nazionale di Statistica). Istat Rapporto Annuale 2022. La situazione del Paese. https://www.istat.it/storage/rapporto-annuale/2022/Rapporto_Annuale_2022.pdf. Accessed 5 Oct 2022.
Di Girolamo C, Bertolini L, Caranci N, Moro ML. Socioeconomic inequalities in overall and COVID-19 mortality during the first outbreak peak in Emilia-Romagna Region (Northern Italy). Epidemiol Prev. 2020;44(Suppl 2):288–96.
Cabrera-Barona P, Murphy T, Kienberger S, Blaschke T. A multi-criteria spatial deprivation index to support health inequality analyses. Int J Health Geogr. 2015;14:11.
Fortunato F, Iannelli G, Cozza A, Del Prete M, Pollidoro FV, Cocciardi S, et al. Local deprivation status and seasonal influenza vaccination coverage in adults ≥ 65 years residing in the Foggia municipality, Italy, 2009–2016. J Prev Med Hyg. 2019;59(4 Suppl 2):E51-64.
Fortunato F, Martinelli D, Iannelli G, Milazzo M, Farina U, Di Matteo G, et al. Self-reported olfactory and gustatory dysfunctions in COVID-19 patients: a 1-year follow-up study in Foggia district. Italy BMC Infect Dis. 2022;22:77.
Fortunato F, Martinelli D, Lo Caputo S, Santantonio T, Dattoli V, Lopalco PL, Prat R. Sex and gender differences in COVID-19: an Italian local register-based study. BMJ Open. 2021;11:e051506.
Italian Central Statistics Institute (Istituto Nazionale di Statistica. Basi territoriali e variabili censuarie. https://www.istat.it/it/archivio/104317#accordions. Accessed 5 July 2020.
Lee J. GIS-based geocoding methods for area-based addresses and 3D addresses in urban areas. Environ Plann B Plann Des. 2009;36:86–106.
Baldovin T, Zangrando D, Casale P, Ferrarese F, Bertoncello C, Buja A, et al. Geocoding health data with geographic Information systems: a pilot study in northeast Italy for developing a standardized data-acquiring format. J Prev Med Hyg. 2015;56:E88-94.
Lillini R, Vercelli M. The local socio-economic health deprivation index: methods and results. J Prev Med Hyg. 2019;59(4 Suppl 2):E3–10.
Agnelli JP, Cadeiras M, Tabak EG, Turner CV, Vanden-Eijnden E. Clustering and classification through normalizing flows in feature space. Multiscale Model Simul. 2010;8:1784–802.
Sahai H, Khurshid A. Statistics in epidemiology: methods, techniques, and applications. Boca Raton FL: CRC Press Inc; 1996.
Tacq J. Multivariate analysis techniques in social science research: from problem to analysis. London, UK: SAGE Publications Ltd; 1997.
Upshaw TL, Brown C, Smith R, Perri M, Ziegler C, Pinto AD. Social determinants of COVID-19 incidence and outcomes: a rapid review. PLoS ONE. 2021;16:e0248336.
Blakely T, Hunt D, Woodward A. Confounding by socioeconomic position remains after adjusting for neighbourhood deprivation: an example using smoking and mortality. J Epidemiol Community Health. 2004;58:1030–1.
Artazcoz L, Rueda S. Social inequalities in health among the elderly: a challenge for public health research. J Epidemiol Community Health. 2007;61:466–7.
Krieger J, Higgins DL. Housing and health: time again for public health action. Am J Public Health. 2002;92:758–68.
Petrelli A, Di Napoli A, Sebastiani G, et al. Italian atlas of mortality inequalities by education level. Epidemiol Prev. 2019;43(Suppl 1):1–120.
Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19:1228–39.
Zhong BL, Luo W, Li HM, Zhang QQ, Liu XG, Li WT, Li Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16:1745–52.
Clements JM. Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic: Cross-sectional online questionnaire. J Med Internet Res. 2020;22:1–11.
Italian Central Statistics Institute (Istituto Nazionale di Statistica). Rapporto BES 2020: Il Benessere Equo e Sostenibile in Italia. 2021. https://www.istat.it/it/archivio/254761. Accessed 5 Oct 2022.
Paez A, Mercado RG, Farber S, Morency C, Roorda M. Accessibility to health care facilities in Montreal Island: an application of relative accessibility indicators from the perspective of senior and non-senior residents. Int J Health Geogr. 2010;9:52.
Salze P, Banos A, Oppert J-M, Charreire H, Casey R, Simon C, et al. Estimating spatial accessibility to facilities on the regional scale: an extended commuting-based interaction potential model. Int J Health Geogr. 2011;10:2.
Padellini T, Jersakova R, Diggle PJ, Holmes C, King RE, Lehmann BCL, et al. Time varying association between deprivation, ethnicity and SARS-CoV-2 infections in England: a population-based ecological study. Lancet Reg Health Eur. 2022;15:100322.
Scully EP, Haverfield J, Ursin RL, Tannenbaum C, Klein SL. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol. 2020;20:442–7.
Sharma G, Volgman AS, Michos ED. Sex differences in mortality from COVID-19 pandemic: are men vulnerable and women protected? JACC Case Rep. 2020;2:1407–10.
Cataldo C, Masella R. Gender-related sociocultural differences and COVID-19: what influence on the effects of the pandemic? Epidemiol Prev. 2020;44(Suppl 2):398–9.
Martini D. Health benefits of mediterranean diet. Nutrients. 2019;5(11):1802.
Gullón P, Cuesta-Lozano D, Cuevas-Castillo C, Fontán-Vela M, Franco M. Temporal trends in within-city inequities in COVID-19 incidence rate by area-level deprivation in Madrid. Spain Health Place. 2022;76: 102830.
UK Office for National Statistics. Coronavirus (COVID-19) Infection Survey. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19infectionsinthecommunityinengland/characteristicsofpeopletestingpositiveforcovid19inenglandseptember2020. Accessed 5 Oct 2022.
Scales D, Gorman J, Jamieson KH. The Covid-19 infodemic—applying the epidemiologic model to counter misinformation. N Engl J Med. 2021;385:678–81.
Islam MS, Sarkar T, Khan SH, Mostofa Kamal AH, Hasan SMM, Kabir A, et al. COVID-19-related infodemic and Its Impact on Public Health: A Global Social Media Analysis. Am J Trop Med Hyg. 2020;103:1621–9.
Tentolouris A, Ntanasis-Stathopoulos I, Vlachakis PK, Tsilimigras DI, Gavriatopoulou M, Dimopoulos MA. COVID-19: time to flatten the infodemic curve. Clin Exp Med. 2021;21:161–5.
Mheidly N, Fares J. Leveraging media and health communication strategies to overcome the COVID-19 infodemic. J Public Health Policy. 2020;41:410–20.
Allington D, McAndrew S, Moxham-Hall V, Duffy B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol Med. 2021;53:236–47.
Pickles K, Cvejic E, Nickel B, Copp T, Bonner C, Leask J, et al. COVID-19 misinformation trends in Australia: prospective longitudinal national survey. J Med Internet Res. 2021;23:e23805.
Masoud AT, Zaazouee MS, Elsayed SM, Ragab KM, Kamal EM, Alnasser YT, et al. KAP-COVIDGLOBAL: a multinational survey of the levels and determinants of public knowledge, attitudes and practices towards COVID-19. BMJ Open. 2021;11:e043971.
Li GHY, Lam SKK, Wong ICK, Chu JKP, Cheung CL. Education attainment, intelligence and covid-19: a mendelian randomization study. J Clin Med. 2021;10:4870.
Bandyopadhyay S, Baticulon RE, Kadhum M, Alser M, Ojuka DK, Badereddin Y, et al. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ Glob Health. 2020;5:e003097.
Acknowledgements
The Authors would like to thank Lucia Massi, Maria Rosa Valetto, and Pietro Dri (Zadig Scientific Publisher, Milan, Italy) for editorial assistance and writing support.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization FF, RL and RP; methodology FF, RL and DM; validation RP and PLL; formal analysis FF, RL and GC; investigation GI, LA; data curation FF, DM, GI, LA and GC; writing-original draft preparation FF, RL and RP; writing-review and editing RP and PLL; supervision RP and PLL. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted within the public health surveillance program established by the Apulia region; ethical approval was not required. All procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Moreover, according to the Italian regulation (DETERMINAZIONE AIFA—20 marzo 2008, GU n. 76 del 31-3-2008), a retrospective epidemiological study only required notification to the Regional Public Health Authority (IRB) due to the nature of the study itself. Moreover, according to the Italian Data Protection Authority in the context of the COVID-19 health emergency, it is indicated that, in the event of the impossibility of obtaining the consent of the interested parties, observational studies take advantage of a derogation regime for the duration of the COVID-19 emergency (art. 110 of the Code regarding the protection of personal data).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fortunato, F., Lillini, R., Martinelli, D. et al. Association of socio-economic deprivation with COVID-19 incidence and fatality during the first wave of the pandemic in Italy: lessons learned from a local register-based study. Int J Health Geogr 22, 10 (2023). https://doi.org/10.1186/s12942-023-00332-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12942-023-00332-9