Abstract
Hypervirulent Klebsiella pneumoniae (hvKp) has emerged as a pathogen of global concern. In this study, both phenotypic and genotypic tests were used to detect hvKp. Antimicrobial resistance profiles and clonal relatedness of clinical isolates were also determined. We found that 34.2% (163/477) of the isolates were tellurite resistant, and among them 102 hvKp isolates detected with iucA or iutA or peg-344 as molecular markers. The blaSHV (80.4%), followed by blaCTX-M-15 (76.5%) and blaTEM (67.6%), blaOXA-48 (53.9%), and blaNDM-1 (32.3%) were detected, while blaKPC-1 was not present in any hvKp isolates. It was found that the majority of hvKp isolates belonged to capsular serotype K20 and ompK36 group C, which is related to clonal group (CG) 23 (e.g. ST23). A high percentage of multidrug-resistant hvKp (76.6%) and high resistance to imipenem (67%) indicated a serious problem that should be addressed in the clinical setting.
Similar content being viewed by others
Introduction
Hypervirulent Klebsiella pneumoniae (hvKp), an emerging pathotype of K. pneumoniae was first reported from Taiwan. It was identified as an important cause of pyogenic liver abscess [1, 2]. In hvKp isolates, pLVPK-like plasmids (Large Virulence Plasmid of K. pneumoniae) encoding virulence factor genes including capsular polysaccharide synthesis regulators (rmpA and rmpA2) and iron acquisition systems (iucA, iutA, and iro siderophore gene cluster), a metabolic transporter (peg-344) and also heavy metal resistance genes (copper, silver, lead, and tellurite), have been identified [3, 4]. Therefore, most hvKp isolates are able to reduce tellurite and form a black colony due to the presence of the major virulence plasmids containing a tellurite resistance gene [5]. The pLVPK-like plasmids may carry all virulence factor genes or have lost some of them [6, 7]. On the other hand, the acquisition of antibiotic resistance plasmids or insertion of resistant mobile genetic elements into the hvKp plasmid turns them into superbugs that can be termed hyper-resistant hvKp strains [8,9,10]. Some K. pneumoniae clones are characterized as high-risk clones that play an important role in the spread of antibiotic-resistant strains [11, 12]. The association of the porin ompK36 with clonal relatedness of K. pneumoniae isolates has been described in several studies [13, 14]. This typing method can be considered as a rapid method for characterizing the clonal relatedness of K. pneumoniae isolates. Four different genotypes for ompK36 porin (A to D) in K. pneumoniae were defined and the correlation of different variants of ompK36 with specific sequence types (STs) was illustrated [13,14,15].
It is important to distinguish hvKps from classical K. pneumoniae (cKp) isolates. To date, several methods have been used to identify hvKp isolates. Detection of hypermucoviscous phenotype on agar (string test), use of Galleria mellonella infection model, serum killing assay and mouse infection models are some of the methods used for phenotypic identification of these strains [16, 17]. However, there is no consensus phenotypic test for the early diagnosis of hvKps, and it appears that more accurate phenotypic tests are needed to rapidly identify these pathotypes of K. pneumoniae. In addition to phenotypic methods, the presence of different virulence genes has been studied to increase the sensitivity and accuracy of hvKps identification. Among these, the genes of iucA, iutA, and peg-344 have been introduced as the best genetic diagnostic markers with the highest accuracy [18].
Therefore, the aim of this study was to develop a rapid identification method for hypervirulent K. pneumoniae. We also investigated the genotypic characteristics, prevalence of virulence factors and antibiotic resistance of hvKps in clinical samples isolated from Iran.
Materials and methods
Bacterial isolation and identification
In this cross-sectional study, we collected a total of 477 non-repetitive K. pneumoniae as clinical isolates from two educational hospitals in Tehran over a period of time from June 2019 to December 2020. All bacterial isolates were identified using standard biochemical laboratory methods and then the isolates were stored in a freezer at −70 °C in nutrient broth containing 20% glycerol until further studies.
HvKp phenotypic identification
Tellurite resistance
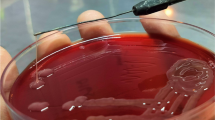
We used tellurite agar culture as a rapid screening test in this study. The isolates that formed black colonies on this tellurite-containing selective medium were considered as presumptive hypervirulent strains for further study. For this purpose, 0.1 g of potassium tellurite powder was first dissolved in 10 ml of sterile distilled water and filtered using membrane filters of pore size 0.45 µm. Then we added 300 μl of the potassium tellurite solution to 100 ml of Mueller–Hinton agar medium, which was autoclaved and cooled to 45–50 °C. Finally, we dispensed into sterile plates. Colonies were examined after overnight incubation at 37 °C.
String test
Hypermucoviscous phenotype of the hvKp isolates was examined by the string test, and the positive result was confirmed via the formation of a 5-mm viscous filament by stretching of bacterial colonies on a blood agar after 24 h of incubation at 37 °C [19].
Molecular characteristics
DNA extraction and identification
Plasmid DNA extraction Mini Kit (FAVORGEN Biotech Corporation, Taiwan) has been used for the detection of genes carried on plasmids. In addition, the boiling method was used for isolation of genomic DNA [20]. All amplification reactions for PCR assays were prepared in a total volume of 25 μl. The list of primer sequences, PCR product sizes, and PCR conditions is shown in Table 1. Finally, all PCR amplification products were sequenced and then searched in the GenBank database using BLAST tool (http://www.ncbi.nlm.nih.gov/blast/).
HvKp molecular identification
All tellurite-resistant K. pneumoniae were screened for the presence of the aerobactin (iucA), its receptor (iutA) genes and peg-344. The isolates containing the iucA or iutA or peg-344 genes were considered as hvKps [18].
Antimicrobial susceptibility testing for hvKp
Antimicrobial susceptibility testing was performed using the disc diffusion method according to the clinical and laboratory standards institute (CLSI) guidelines (CLSI 2018-M100-S28) by the following antibiotic discs including amikacin (AK), gentamicin (GN), cefotaxime (CTX), ceftazidime (CAZ), ceftriaxone (CRO), imipenem (IMI), meropenem (MRP), cefepime (FEP), ciprofloxacin (CIP), ampicillin (AMP) and aztreonam (AZM). Minimum inhibitory concentrations (MICs) of imipenem and ceftazidime were determined by broth dilution method. Escherichia coli ATCC 25922 was used as the quality control strain for antimicrobial susceptibility testing.
Capsular genotyping and detection of virulence, and antimicrobial resistance genes
The hvKp capsular serotypes K1, K2, K5, K20, K54, and K57 were identified using PCR method [21]. The hvKp virulence genes including salmochelin siderophore (iroB), mucoviscosity-associated gene (magA), Klebsiella ferric uptake (kfu), yersiniabactin (ybt), allantoin metabolism gene (allS), and rmpA were detected by specific primers listed in Table 1. In addition, PCR assays were carried out for detection of blaTEM, blaSHV, and blaCTX-M-15, blaKPC-1, blaNDM-1, and blaOXA-48 genes in all hvKp isolates.
Determination of clonal relatedness using ompK36 typing
All hvKp isolates were subjected to ompK36 typing by the PCR-based method described by Yan et al., using four pairs of primers [13].
Statistical analysis
The statistical analyses of data were performed using SPSS software, version 16.0 (IBM, Armonk, NY, USA) and Chi-square tests (2 × 2 contingency table) were used to compare the data associated with hvKp and cKp strains. Finally, the P values < 0.05 was considered statistically significant.
Nucleotide accession numbers
The accession numbers of blaOXA-48, blaNDM-1, iutA, iucA and peg-344 are MZ245618, MZ245619, MZ245620, MZ245621 and MZ245622, respectively in GenBank database.
Results
Phenotypic tests
In this study, 163 (34.2%) out of 477K. pneumoniae isolates were able to grow on tellurite-containing MH medium and were considered tellurite-resistant strains, so they were selected for the molecular identification test. In addition, 62 out of 477K. pneumoniae isolates (13%) were reported with positive string test and hypermucoviscous phenotype.
Molecular identification of hvKp
Based on molecular identification, we found the iucA or iutA or peg-344 as hvKp molecular markers in 21.4% (102/477) of total K. pneumoniae and 62.6% (102/163) of tellurite-resistant isolates. Therefor, 45 isolates had only the iucA, 6 isolates had only the iutA, and 48 strains had both the iucA and iutA genes, all three genes (iucA, iutA and peg-344) were detected simultaneously in only three hvKp isolates. Also, 48% (49/102) hvKp isolates were string positive. See Table 2.
Demographic data of hvKp isolates
In this collection, 61.7% (63/102) and 38.2% (39/102) of hvKp strains were isolated from hospital A and B, respectively. Most of hvKp isolates were obtained from urine (33.3%, 34/102), followed by tracheal aspiration (27.5%, 28/102), blood (9.8%, 10/102) and abscess (7.8%, 8/102) specimens. Also among hospital wards, most hvKps were obtained from patients admitted to intensive care unit (ICU) (51%), internal (12.7%), surgical (10.8%) and emergency (8.8%) wards. Sixty-two patients (60.8%) were male. Most of patients were over 60 years of age (45.1%). See Table 2.
Antimicrobial susceptibility testing
In this study, we investigated the antimicrobial susceptibility profile in 90 hvKp isolates. Susceptibility profiles against antimicrobials agents are shown in Table 2. The highest rate of antibiotic resistance was related to ampicillin (100%), followed by cefotaxime and ceftazidime (91%). The lowest rate of resistance was found in amikacin (27.8%). The resistance rates to other antibiotics including ceftriaxone, cefepime, ciprofloxacin, gentamicin, meropenem, imipenem and aztreonam were 87.7%, 86.6%, 84.4%, 78.8%, 67.7%, 67.7% and 58.8%, respectively. In addition, 76.6% of the isolates (69/90) were resistant to at least three classes of antibiotics and were defined as multidrug resistant (MDR) [21]. Finally, the MIC of some resistant hvKp (resistant in disk diffusion) to the antibiotics ceftazidime and imipenem was determined by broth dilution method. In accordance with the facilities and funding, 23 isolates resistant to imipenem and ceftazidime were selected for the MIC test. All 23 isolates selected for ceftazidime had MIC ≥ 16: for 6 isolates MIC ˃ 16, 2 isolates MIC = 16, 3 isolates MIC = 32, 11 isolates MIC = 64, one isolate MIC = 128. Of the 39 resistant hvKp isolates, 79.5% had a MIC above the CLSI resistance criteria for imipenem (MIC ≥ 4): for 16 isolates MIC ˃ 4, 6 isolates MIC = 4, 5 isolates MIC = 8, 3 isolates MIC = 16, one isolate MIC = 256. 4 isolates (10.2%) were classified as intermediate resistant (MIC = 2) and 4 isolates (7.8%) were classified as susceptible (MIC < 2).
Capsular genotyping and detection of virulence genes, and antimicrobial resistance genes
Capsular genotyping (K genotyping) of hvKp isolates showed that capsular serotype K20 was detected in more than half of the hvKp strains (54.9%). K2 and K1 were identified in only 3 (2.9%) and one isolate (1%), respectively, while K5, K54 and K57 were not detected in any of the hvKp isolates. In addition, 42 isolates (41.2%) did not belong to serotypes K1, K2, K5, K20, K54 and K57 as shown in Table 2.
PCR for virulence-associated genes revealed that ybt (77.5%) was the most common virulence factor gene after iucA. The other virulence factor genes including rmpA, iroB, magA, kfu and allS were detected in 48%, 3.9%, 0.98, 21.6% and 1.96% hvKp isolates, respectively. See Table 2.
The distribution of ESBLs and carbapenemase genes among hvKp isolates are shown in Table 2. The results showed that 92.2% (94/102) of hvKp isolates carried at least one antibiotic resistance gene and only 7.8% (8/102) had no resistance gene. The blaSHV was the most common Beta-lactamase gene (80.4%), followed by blaCTX-M-15 (76.5%) and blaTEM (67.6%). Also, PCR amplification of carbapenemase genes showed that blaOXA-48 (53.9%) was the dominant genotype of carbapenem-resistant strains, followed by blaNDM-1 (32.3%), while blaKPC-1 was not detected in any hvKp isolate. Thus, 56.8% (58/102) of the hvKp isolates that co-carried blaTEM, blaSHV, blaCTX-M-15, blaOXA-48 and blaNDM-1 genes was the predominant MDR-hvKp genotype. On the other hand, as shown in Table 2, more than 2 virulence factor genes were detected simultaneously in the majority of resistant hvKp strains and virulence profiles including: iucA, iutA, ybt and rmpA genes have been reported in 40.4% (38/94) resistant hvKp isolates.
ompK36 typing
PCR-based ompK36 typing revealed that ompK36 group C was the most common type with 70.6% (72/102) frequency. The prevalence of the other types, including ompK36 groups A, B, and C, was (14/102) 13.7%, (5/102) 4.9%, and 10.8% (11/102), respectively. See Table 2.
Comparison between cKps and hvKps
In this study, 78 cKps and 102 hvKps isolates were examined. Demographic data and antimicrobial resistance profile were compared using chi-square tests. The data showed that there were no significant differences in demographic data between two groups. However, significant differences were found in antimicrobial resistance (e.g. amikacin, cefotaxime and gentamicin) and the presence of carbapenemases (blaOXA-48, blaNDM-1). See Table 3.
Discussion
In this study, to identify these K. pneumoniae superbugs, we used a combination of phenotypic and genotypic methods including tellurite resistance, and preferential gene markers. Previously, only the string test was used as a phenotypic method to identify hvKp isolates, but the string test is not a reliable rapid test for hvKp detection [1, 22, 23]. MacConkey inositol potassium tellurite agar (MCIK) has been used as a selective medium for the detection of K. pneumoniae from environmental sources or animal and human fecal samples [24]. This study showed that the trait of tellurite resistance is strongly associated with CG23, CG65 and CG86, which are mostly invasive community-acquired strains of K. pneumoniae. It appears that the large virulence plasmids of hvKp harbor tellurium resistance genes [24]. In silico analysis revealed that the tellurium gene cluster is highly prevalent among hypervirulent plasmids which is present in different sequence types (data not yet published). This prompted us to use Mueller–Hinton agar containing potassium tellurite as a selective medium for the rapid detection of hypervirulent K. pneumoniae strains. In this study, out of 163 tellurite-resistant isolates, 102 strains were genetically confirmed as hypervirulent K. pneumoniae, so making this method superior than string test for rapid phenotypic hvKp identification.
We also used three key virulence genes as molecular biomarkers previously introduced by Russo et al. to increase the accuracy and sensitivity of hvKp detection [18]. In addition, all hvKp isolates were examined for the presence of other virulence factor genes. In general, the frequencies of virulence factor genes, from highest to lowest, iucA, ybt, iutA, rmpA, kfu, iroB, peg-344, allS, and magA, respectively, were reported. Other studies have also shown that the aerobactin is produced by more than 90% of hvKp, whereas only 6% of cKp strains can express it [18, 25]. In a study by XU et al. the prevalence of iucA, iutA, rmpA and iro was reported to be 56.8%, 56.8%, 43.2% and 40.9%, respectively. The prevalence of iutA and rmpA was similar to our study, but in the present study, the prevalence of iucA was higher and iro was lower than the results of the study by Xu et al. [26]. The ybt was the second most prevalent virulence factor gene among hvKp isolates in this study. The yersiniabactin gene and its receptor, which is an important virulence factor for the survival of Klebsiella strains under severe conditions, can transmit both an integrative conjugative element (ICEKp) and a plasmid (recently reported) [27]. Some studies have described the correlation between yersiniabactin-producing hvKps and pulmonary infectious diseases [28, 29]. In Iran, a study conducted by Tabrizi et al. reported that 5 of 53 K. pneumoniae strains isolated from ventilator-associated pneumonia were hvKp [30]. In the current study, of 33 hvKps isolated from lung-related samples, 27 isolates were ybt-positive, confirming the results of previous studies. The rmpA was identified as the fourth most virulence factor. Because rmpA increases the expression of capsular polysaccharide (CPS), we expected that the rmpA-producing hvKp that were isolated would be string test-positive, but this hypothesis was refuted by our results, such that only 36.7% of the rmpA-positive isolates were reported as hypercystic phenotype. Studies have shown that other genes besides rmpA are involved in capsular gene expression, such as regulation of capsular synthesis B (rcsB). Both rmpA and rcsB genes have been shown to co-occur [31]. In addition, the data show that the co-presence of four genes (iucA, ybt, iutA and rmpA) was more frequent in hvKp. In addition, other plasmid-born genes such as iro, peg-344 were less frequent and were reported only sporadically.
Sequencing and analysis of large virulence plasmids from hvKp strains revealed that virulence-associated genes were mainly found in two regions. The rmpA2, iucABCD and iutA genes are located close to each other, followed by the rmpA, peg-344 and iroBCDN genes in the second region. Some virulence plasmids carry all virulence genes (e.g. pLVPK, GenBank accession number: AY378100), but others have lost one or more virulence-associated loci, confirming our result (e.g. pVir, GenBank accession number: CP029383.2) [6, 32]. Despite most Asian countries having introduced K1 and K2 as the most common capsular serotypes [21, 33,34,35], we identified K20 as the most common capsular type in Iran. This phenomenon suggests that the prevalence of the different serotypes may vary depending on the geographical area. Although there has been no comprehensive study on the hvKp isolates in Iran and little information is available on them, no K1 and K2 were found among the K. pneumoniae isolates in the study conducted by Aghamohammad et al. [36]. Also, in another study, one K1 and 15 K2 were identified among 122 K. pneumoniae isolates from Semnan, Iran, which are in agreement with our results (we detected only one K1 and three K2) [37]. Another study from Iran conducted by Solgi et al. reported that the prevalence of K1 and K2 was 45.9% and 13.5% respectively, which was more than the present study [38].
Also, in the present study, according to the Table 3, in terms of frequency in the type of sample, and the hospital wards did not show a significant difference between these two variants. In both groups, almost half of the samples were isolated from the ICU. However, patients admitted to the ICU due to prolonged hospitalization were more susceptible to hvKp infection. In addition, it may increase the probability of horizontal gene transfer in clinical settings [39, 40]. In this study, it was also found that in-hospital B, most hvKps had the same genotypic characteristics such as capsular serotype K20, ompK36 type C, and similar antibiotic resistance profiles. Therefore, the hvKp regional expansion hypothesis seems reasonable.
Most hvKps are sensitive to most antibiotics except for intrinsic resistance to ampicillin, similarly in this study all hvKp isolates were ampicillin resistant [40]. Studies have shown that hvKps are unlikely to take up DNA from other resistant bacteria due to the large size of the capsule and increased expression of capsule-related genes, therefore antibiotic resistance is less common in hvKps than in cKp isolates [41]. But contrary to expectations, the rate of resistance was not much different between the two variants hvKps and cKps. Our results are consistent with other studies that have shown that the rate of hvKp resistance is increasing worldwide [42, 43]. The current study revealed the high prevalence of MDR-hvKp and high resistance to imipenem (66%). Moreover, the presence of blaTEM, blaSHV, blaCTX-M-15, blaOXA-48 and blaNDM-1 was detected simultaneously in 56.8% of hvKp isolates. There was a significant difference between hvKps and cKps about carbapenem-resistance genes so that blaOXA-48 was more frequent in carbapenem-resistant hvKps, and in contrast, blaNDM-1 was more detected in carbapenem-resistant cKp isolates. The reason for this difference is not clear.
However, two pathways have been introduced for the emergence of MDR-hvKp strains, the horizontal acquisition of resistance genes by plasmids and mobile genetic elements (MGEs) by hvKp isolates (type I), and another pathway is the acquisition of the virulence-associated plasmid (e.g., pLVPK and pVir) by MDR-cKp (type II) [42, 44]. Ultimately, both mechanisms lead to the development of MDR-hvKp strains that are resistant to antibiotic treatment in addition to having a very high pathogenicity that poses a serious threat to public health.
The correlation of ompK36 porin variants with specific sequence types (STs) of K. pneumoniae was first described by Papagiannitsis et al. K. pneumoniae isolates can be classified into four groups (designated groups A to D) by ompK36 genotyping [13, 45]. There is a relationship between ompK36 type and clonal group (CG). Also, some STs were reported to be associated with hvKp isolates, e.g. ST11 and ST23, that ST11 (CG258) belonged to ompK36 group A and ST23 (CG23) belonged to ompK36 group C [13, 46]. In this study, clonal relatedness by ompK36 typing revealed that group C (70.6%) was the most common ompK36 porin type among hvKp isolates. A study in Taiwan showed that ompK36 group C was significantly more abundant among K. pneumoniae isolates [46]. This study was in agreement with our study in Iran.
Conclusion
This study presented a new rapid screening method based on the resistance of hvKp to tellurite, which was superior than string test in phenotypic identification of hvKp isolates. The consideration of phenotypic detection along with genotyping of hvKp render a reliable identification of hypervirulent strains. In this study, a high prevalence of MDR-hvKp and a high level of resistance to imipenem (66%) were detected. In addition, co-existence of blaTEM, blaSHV, blaCTX-M-15, blaOXA-48 and blaNDM-1 was identified in 56.8% of hvKp isolates. Using the PCR-based ompK36 typing method, which was simpler and less expensive than MLST, we were also able to investigate the clonal relatedness of the strains. It was found that the majority of hvKp isolates belonged to capsular serotype K20 and ompK36 group C, which is related to CG23 (e.g. ST23). It seems that the expansion of MDR-hvKp in clinical settings is an inevitable event and this needs an urgent infection control program in the healthcare setting. The plasmids harboring virulence and antimicrobial resistance factors will change the clinical face of K. pneumoniae soon.
Abbreviations
- K. pneumoniae :
-
Klebsiella pneumoniae
- hvKp:
-
Hypervirulent Klebsiella pneumoniae
- rmpA :
-
Regulator of mucoid phenotype
- magA :
-
Mucoviscosity-associated gene
- kfu :
-
Klebsiella Ferric uptake
- iroB :
-
Salmochelin iron uptake systems
- ybt :
-
Yersiniabactin
- allS :
-
Allantoin metabolism gene
- AK:
-
Amikacin
- GN:
-
Gentamicin
- CTX:
-
Cefotaxime
- CAZ:
-
Ceftazidime
- CRO:
-
Ceftriaxone
- IMI:
-
Imipenem
- MRP:
-
Meropenem
- FEP:
-
Cefepime
- CIP:
-
Ciprofloxacin
- AMP:
-
Ampicillin
- AZM:
-
Aztreonam
- MIC:
-
Minimum inhibitory concentration
- ICU:
-
Intensive care unit
- ESBL:
-
Extended spectrum beta-lactamases
- pLVPK:
-
Large Virulence Plasmid of K. pneumoniae
- MDR:
-
Multidrug resistant
- MDR-cKp:
-
Classical MDR-K. pneumoniae
- ST:
-
Sequence types
- BAL:
-
Bronchoalveolar lavage
- CSF:
-
Cerebrospinal fluid
References
Liu C, Guo J. Hypervirulent Klebsiella pneumoniae (hypermucoviscous and aerobactin positive) infection over 6 years in the elderly in China: antimicrobial resistance patterns, molecular epidemiology and risk factor. Ann clin microbiol. 2019;18(1):1–11.
Rossi B, Gasperini ML, Leflon-Guibout V, Gioanni A, de Lastours V, Rossi G, et al. Hypervirulent Klebsiella pneumoniae in cryptogenic liver abscesses, Paris, France. Emerg Infect Dis. 2018;24(2):221.
Dong N, Yang X, Zhang R, Chan EW-C, Chen S. Tracking microevolution events among ST11 carbapenemase-producing hypervirulent Klebsiella pneumoniae outbreak strains. Emerg Microbes Infect. 2018;7(1):1–8.
Sanikhani R, Moeinirad M, Shahcheraghi F, Lari A, Fereshteh S, Sepehr A, et al. Molecular epidemiology of hypervirulent Klebsiella pneumoniae: a systematic review and meta-analysis. Iran J Microbiol. 2021;13(3):257–65.
Paterson DL, Siu K, Chang FY. Klebsiella species (K. pneumoniae, K. oxytoca, K. ozaenae and K. rhinoscleromatis). Antimicrobe. 2014;9:74–6.
Russo TA, Marr CM. Hypervirulent Klebsiella pneumoniae. Clin Microbiol Rev. 2019. https://doi.org/10.1128/CMR.00001-19.
Xie M, Dong N, Chen K, Yang X, Ye L, Chan EW-C, et al. A hybrid plasmid formed by recombination of a virulence plasmid and a resistance plasmid in Klebsiella pneumoniae. J Glob Antimicrob Resist. 2020;23:466–70.
Liao W, De Wang L, Li D, Du F-L, Long D, Liu Y, et al. High Prevalence of 16s rRNA methylase genes among carbapenem-resistant hypervirulent Klebsiella pneumoniae isolates in a Chinese Tertiary Hospital. Microb Drug Resist. 2021;27(1):44–52.
Wyres KL, Wick RR, Judd LM, Froumine R, Tokolyi A, Gorrie CL, et al. Distinct evolutionary dynamics of horizontal gene transfer in drug resistant and virulent clones of Klebsiella pneumoniae. PLoS Genet. 2019;15(4):e1008114.
Feng Y, Lu Y, Yao Z, Zong Z. Carbapenem-resistant hypervirulent Klebsiella pneumoniae of sequence type 36. Antimicrob Agents Chemother. 2018;62(7):e02644-e2717.
Peirano G, Chen L, Kreiswirth BN, Pitout JD. Emerging antimicrobial-resistant high-risk Klebsiella pneumoniae clones ST307 and ST147. Antimicrob Agents Chemother. 2020;64(10):e01148-e1220.
Astocondor-Salazar L. Betalactamasas: la evolución del problema. Rev peru investig salud. 2018;2(2):42–9.
Yan J, Wang M, Zheng P, Tsai L, Wu J. Associations of the major international high-risk resistant clones and virulent clones with specific ompK36 allele groups in Klebsiella pneumoniae in Taiwan. N Microbes New Infect. 2015;5:1–4.
Hamzaoui Z, Ocampo-Sosa A, Martinez MF, Landolsi S, Ferjani S, Maamar E, et al. Role of association of OmpK35 and OmpK36 alteration and blaESBL and/or blaampC genes in conferring carbapenem resistance among non-carbapenemase-producing Klebsiella pneumoniae. Int J Antimicrob Agents. 2018;52(6):898–905.
Woodford N, Turton JF, Livermore DM. Multiresistant Gram-negative bacteria: the role of high-risk clones in the dissemination of antibiotic resistance. FEMS Microbiol Rev. 2011;35(5):736–55.
Russo TA, MacDonald U. The Galleria mellonella infection model does not accurately differentiate between hypervirulent and classical Klebsiella pneumoniae. Msphere. 2020;5(1):e00850-e919.
Li G, Shi J, Zhao Y, Xie Y, Tang Y, Jiang X, et al. Identification of hypervirulent Klebsiella pneumoniae isolates using the string test in combination with Galleria mellonella infectivity. Eur J Clin Microbiol Infect Dis. 2020;39(9):1673–9.
Russo TA, Olson R, Fang C-T, Stoesser N, Miller M, MacDonald U, et al. Identification of biomarkers for differentiation of hypervirulent Klebsiella pneumoniae from classical K. pneumoniae. J Clin Microbiol. 2018;56(9):00776–18.
Yao B, Xiao X, Wang F, Zhou L, Zhang X, Zhang J. Clinical and molecular characteristics of multi-clone carbapenem-resistant hypervirulent (hypermucoviscous) Klebsiella pneumoniae isolates in a tertiary hospital in Beijing, China. Int J Infect Dis. 2015;37:107–12.
Peymani A, Farivar TN, Sanikhani R, Javadi A, Najafipour R. Emergence of TEM, SHV, and CTX-M-extended spectrum β-lactamases and class 1 integron among Enterobacter cloacae isolates collected from hospitals of Tehran and Qazvin, Iran. Microb Drug Resist. 2014;20(5):424–30.
Fang C-T, Lai S-Y, Yi W-C, Hsueh P-R, Liu K-L, Chang S-C. Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clin Infect Dis. 2007;45(3):284–93.
Catalán-Nájera JC, Garza-Ramos U, Barrios-Camacho H. Hypervirulence and hypermucoviscosity: two different but complementary Klebsiella spp. phenotypes? Virulence. 2017;8(7):1111–23.
Parrott A, Shi J, Aaron J, Green D, Whittier S, Wu F. Detection of multiple hypervirulent Klebsiella pneumoniae strains in a New York City hospital through screening of virulence genes. Clin Microbiol Infect. 2021;27(4):583–9.
Passet V, Brisse S. Association of tellurite resistance with hypervirulent clonal groups of Klebsiella pneumoniae. J Clin Microbiol. 2015;53(4):1380–2.
Paczosa MK, Mecsas J. Klebsiella pneumoniae: going on the offense with a strong defense. Microbiol Mol Biol Rev. 2016;80(3):629–61.
Xu M, Fu Y, Fang Y, Xu H, Kong H, Liu Y, et al. High prevalence of KPC-2-producing hypervirulent Klebsiella pneumoniae causing meningitis in Eastern China. Infect Drug Resist. 2019;12:641.
Lam MM, Wyres KL, Judd LM, Wick RR, Jenney A, Brisse S, et al. Tracking key virulence loci encoding aerobactin and salmochelin siderophore synthesis in Klebsiella pneumoniae. Genome Med. 2018;10(1):1–15.
Bachman MA, Oyler JE, Burns SH, Caza M, Lépine F, Dozois CM, et al. Klebsiella pneumoniae yersiniabactin promotes respiratory tract infection through evasion of lipocalin 2. Infect Immun. 2011;79(8):3309–16.
Lawlor MS, O’connor C, Miller VL. Yersiniabactin is a virulence factor for Klebsiella pneumoniae during pulmonary infection. Infect Immun. 2007;75(3):1463–72.
Tabrizi AMA, Badmasti F, Shahcheraghi F, Azizi O. Outbreak of hypervirulent Klebsiella pneumoniae harbouring blaVIM-2 among mechanically-ventilated drug-poisoning patients with high mortality rate in Iran. J Glob Antimicrob Resist. 2018;15:93–8.
Cheng H, Chen Y, Wu C, Chang H, Lai Y, Peng H-L. RmpA regulation of capsular polysaccharide biosynthesis in Klebsiella pneumoniae CG43. J Bacteriol. 2010;192(12):3144–58.
Struve C, Roe CC, Stegger M, Stahlhut SG, Hansen DS, Engelthaler DM, et al. Mapping the evolution of hypervirulent Klebsiella pneumoniae. MBio. 2015;6(4):e00630-e715.
Victor LY, Hansen DS, Ko WC, Sagnimeni A, Klugman KP, Von Gottberg A, et al. Virulence characteristics of Klebsiella and clinical manifestations of K. pneumoniae bloodstream infections. Emerg Infect Dis. 2007;13(7):986.
Liu YM, Li BB, Zhang YY, Zhang W, Shen H, Li H, et al. Clinical and molecular characteristics of emerging hypervirulent Klebsiella pneumoniae bloodstream infections in mainland China. Antimicrob Agents Chemother. 2014;58(9):5379–85.
Yeh K-M, Kurup A, Siu L, Koh Y, Fung C-P, Lin J-C, et al. Capsular serotype K1 or K2, rather than magA and rmpA, is a major virulence determinant for Klebsiella pneumoniae liver abscess in Singapore and Taiwan. J Clin Microbiol. 2007;45(2):466–71.
Aghamohammad S, Badmasti F, Solgi H, Aminzadeh Z, Khodabandelo Z, Shahcheraghi F. First report of extended-spectrum betalactamase-producing Klebsiella pneumoniae among fecal carriage in Iran: high diversity of clonal relatedness and virulence factor profiles. Microb Drug Resist. 2020;26(3):261–9.
Pajand O, Darabi N, Arab M, Ghorbani R, Bameri Z, Ebrahimi A, et al. The emergence of the hypervirulent Klebsiella pneumoniae (hvKp) strains among circulating clonal complex 147 (CC147) harbouring blaNDM/OXA-48 carbapenemases in a tertiary care center of Iran. Ann clin microbiol. 2020;19:1–9.
Solgi H, Shahcheraghi F, Bolourchi N, Ahmadi A. Molecular characterization of carbapenem-resistant serotype K1 hypervirulent Klebsiella pneumoniae ST11 harbouring blaNDM-1 and blaOXA-48 carbapenemases in Iran. Microb Pathog. 2020;149:104507.
Zhao Y, Zhang X, Torres VVL, Liu H, Rocker A, Zhang Y, et al. An outbreak of carbapenem-resistant and hypervirulent Klebsiella pneumoniae in an intensive care unit of a major teaching hospital in Wenzhou, China. Public Health Front. 2019;7:229.
Tang M, Kong X, Hao J, Liu J. Epidemiological characteristics and formation mechanisms of multidrug-resistant hypervirulent Klebsiella pneumoniae. Front microbiol. 2020;11:2774.
Zhu J, Wang T, Chen L, Du H. Virulence factors in hypervirulent Klebsiella pneumoniae. Front microbiol. 2021;12:734.
Gu D, Dong N, Zheng Z, Lin D, Huang M, Wang L, et al. A fatal outbreak of ST11 carbapenem-resistant hypervirulent Klebsiella pneumoniae in a Chinese hospital: a molecular epidemiological study. Lancet Infect Dis. 2018;18(1):37–46.
Li W, Sun G, Yu Y, Li N, Chen M, Jin R, et al. Increasing occurrence of antimicrobial-resistant hypervirulent (hypermucoviscous) Klebsiella pneumoniae isolates in China. Clin Infect Dis. 2014;58(2):225–32.
Liu Y, Long D, Xiang T-X, Du F-L, Wei DD, Wan L-G, et al. Whole genome assembly and functional portrait of hypervirulent extensively drug-resistant NDM-1 and KPC-2 co-producing Klebsiella pneumoniae of capsular serotype K2 and ST86. J Antimicrob Chemother. 2019;74(5):1233–40.
Papagiannitsis CC, Giakkoupi P, Kotsakis SD, Tzelepi E, Tzouvelekis LS, Vatopoulos AC, et al. OmpK35 and OmpK36 porin variants associated with specific sequence types of Klebsiella pneumoniae. J Chemother. 2013;25(4):250–4.
Yan J-J, Zheng P-X, Wang M-C, Tsai S-H, Wang L-R, Wu J-J. Allocation of Klebsiella pneumoniae bloodstream isolates into four distinct groups by ompK36 typing in a Taiwanese university hospital. J Clin Microbiol. 2015;53(10):3256–63.
Compain F, Babosan A, Brisse S, Genel N, Audo J, Ailloud F, et al. Multiplex PCR for detection of seven virulence factors and K1/K2 capsular serotypes of Klebsiella pneumoniae. J Clin Microbiol. 2014;52(12):4377–80.
Yu W-L, Ko W-C, Cheng K-C, Lee C-C, Lai C-C, Chuang Y-C. Comparison of prevalence of virulence factors for Klebsiella pneumoniae liver abscesses between isolates with capsular K1/K2 and non-K1/K2 serotypes. Diagn Microbiol Infect Di. 2008;62(1):1–6.
Ahmed SF, Ali MMM, Mohamed ZK, Moussa TA, Klena JD. Fecal carriage of extended-spectrum β-lactamases and AmpC-producing Escherichia coli in a Libyan community. Ann clin microbiol. 2014;13(1):1–8.
Abhari SS, Badmasti F, Modiri L, Aslani MM, Asmar M. Circulation of imipenem-resistant Acinetobacter baumannii ST10, ST2 and ST3 in a university teaching hospital from Tehran. Iran J Med Microbiol. 2019;68(6):860–5.
Acknowledgements
The authors would like to thank the personnel in the bacteriology department of the Pasteur Institute of Iran for their help. This research was supported by the Pasteur Institute of Iran.
Funding
The funding source was Granted to Rahimeh Sanikhani as Ph.D. student from Pasteur Institute of Iran (Project No.: B-9427).
Author information
Authors and Affiliations
Contributions
HS & MM, collected the samples and their data; RS & FS, carried out other phenotypic and genotypic tests; RS, MM and FB, wrote the manuscript and analyzed the data; FB, supervised the project and write and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This project was done based on ethical guidelines as previously approved by the Pasteur Institute of Iran (IR. B-9427).
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sanikhani, R., Moeinirad, M., Solgi, H. et al. The face of hypervirulent Klebsiella pneumoniae isolated from clinical samples of two Iranian teaching hospitals. Ann Clin Microbiol Antimicrob 20, 58 (2021). https://doi.org/10.1186/s12941-021-00467-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-021-00467-2