Abstract
Background
Meningitis with a negative cerebrospinal (CSF) Gram stain represents a diagnostic and therapeutic challenge. The purpose of our study was to evaluate the performance of the BioFire FilmArray® Meningitis/Encephalitis (FA ME) panel in patients presenting with community-acquired meningitis with a negative Gram stain.
Methods
CSF from 48 patients with community-acquired meningitis with a negative Gram stain admitted to four hospitals in Houston, TX underwent additional testing by the FA ME. FA ME results were compared to results obtained as part of routine evaluation.
Results
The panel detected pathogens not previously identified in 11 (22.9 %) of 48, but did not detect pathogens identified by standard technique (West Nile virus, Histoplasma) in 5 (15.2 %) patients.
Conclusions
Rapid testing for the most common pathogens causing meningitis will aid in the diagnosis and treatment of patients with meningitis.
Similar content being viewed by others
Background
Meningitis with a negative cerebrospinal fluid (CSF) Gram stain represents a diagnostic and therapeutic challenge, as the majority of the causative organisms are unknown [1]. Clinicians on the front lines are faced with multiple diagnostic dilemmas in an effort to ensure bacterial or other treatable infections are not missed. A variety of strategies have been employed to assist physicians including the use of advanced molecular techniques. Such advanced strategies are not widely accessible, tandem agent testing requires lengthy turn-around time at a distal reference laboratory and definitive results are complicated by specimen contamination and limited available volume [2]. Identifying the specific etiology of meningitis with a negative CSF Gram stain has important clinical, public health and antibiotic use implications. We evaluated the performance of the BioFire FilmArray Meningitis/Encephalitis (FA ME) panel in patients presenting with community-acquired meningitis with a negative Gram stain. CSF samples were obtained from patients admitted to four hospitals in Houston, TX comparing the BioFire FA to routine laboratory evaluation.
Methods
Patients admitted between November 2008 and March 2014 with community-acquired meningitis or encephalitis (fever, headache, vomiting, photophobia, stiff neck, focal neurological symptoms), CSF cell count >5 cells/mm [3] and a negative CSF Gram stain were eligible. Residual patient CSF underwent additional testing by a research use only version of the FilmArray Meningitis/Encephalitis panel (FA ME, BioFire Diagnostics, LLC) according to the manufacturer’s instructions [3]. Briefly residual CSF sample was combined with FilmArray Sample Buffer in a 1:4 ratio and then injected into a FilmArray pouch. The panel requires 200 µL of CSF and simultaneously tests for six bacteria (S. pneumoniae, N. meningitidis, S. agalactiae, H. influenzae, L. monocytogenes, E. coli K1), eight viruses [Herpes simplex types (HSV) 1 and 2, Human herpesvirus 6, Cytomegalovirus, Epstein-Barr virus (EBV), Enterovirus, Parechovirus, Varicella zoster virus (VZV)] and two fungi (Cryptococcus gattii/neoformans). Two minutes of user hands-on time are required and comprehensive results are returned in approximately 1 h. The University of Texas Institutional Review Board approved the study and results were not used in patient management.
Results
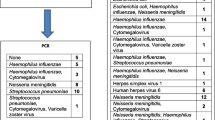
Of 149 patients with community-acquired meningitis, 48 (32.2 %) had residual CSF (38 adults, 10 children < age 18) available for FA ME testing. Median age of patients was 38.3 months (range 3 months–82 years) and 21 (43.7 %) were male. Twenty-five (52 %) were diagnosed with meningitis at discharge and 23 with encephalitis (47.9 %). Pathogens were identified in 14 (29.2 %) of 48 samples by routine evaluation and 15 (31.2 %) by FA ME (see Table 1). Among FA ME results, viral pathogens were most commonly detected [EBV (8), HSV2 (3), VZV (3), HSV1 (1), Enterovirus (1)], followed by bacterial [S. pneumoniae (2)] and fungal [C. gattii/neoformans (1)]. Co-detections were present in six patients (12.5 %); EBV was present in all (6) along with VZV (2), HSV1 (1), HSV2 (1), C. gattii/neoformans (1), and S. pneumoniae (1). In 11 (22.9 %) patients, FA ME identified pathogens not previously identified. Routine evaluation evaluations identified pathogens in 5 (15.2 %) of 33 FA ME negative samples [West Nile virus (WNV) (4), Histoplasma capsulatum (1)].
Discussion
Novel and fast molecular techniques are critical in identifying etiologies and starting appropriate therapy quickly in patients with meningitis. PCR assays to diagnose viral central nervous system infections have now become standard and have largely replaced viral culture [1, 4]. PCR, however, continues to be underutilized [1]. Reasons for underutilization are multiple and include variable approaches to diagnosis and variable access to such testing. The BioFire FA ME addresses such diagnostic underutilization by providing a comprehensive panel testing for 15 CNS pathogens simultaneously using a minimal amount of CSF with rapid turn-around time (1 h). Shown to be an effective alternative for other infections such as gastroenteritis [3], and bacteremia [5–8] BioFire’s FA ME was approved by the Federal Drug Administration on October 8, 2015 with promising results both in the US [9] and internationally [10, 11]. This is the second report [12] of the FA ME’s performance in the US, highlighting the importance of additional WNV and Histoplasmosis testing.
The FA ME resulted in pathogen detections not previously recognized and for which treatment is recommended [13], including VZV (n = 2), HSV (n = 2) and S. pneumoniae (n = 1) In one patient with VZV identified by FA ME, the routine evaluation did not include VZV testing (CSF VZV PCR or VZV IgM/IgG). Similarly, one patient with HSV identified by FA ME did not have HSV testing included in routine evaluation. In both patients, no rash was present. Appropriate laboratory studies for VZV and HSV should be ordered in any patient with unexplained meningoencephalitis, even if cutaneous manifestations are absent [14, 15]. In the patient with S. pneumoniae identified by FA ME but not routine evaluation, IV antibiotics were administered prior the LP, reducing the likelihood of the rapid antigen testing (RAT) and CSF culture being positive.
EBV was the most common virus identified by FA ME (n = 8), as the sole organism (n = 2) or in co-infection (n = 6). Of the patients with EBV identified by FA ME, 3 had meningitis and 5 encephalitis. The most common pathogens identified in aseptic meningitis (Enteroviruses) [1] and encephalitis (HSV, WNV and Enterovirus) [13] do not include EBV so it’s not surprising routine evaluation did not include EBV testing (EBV CSF PCR or EBV IgM, IgG) for any patient. Complications of EBV infection are diverse and include a number of neurologic manifestations such as meningitis, meningoencephalitis, cerebellitis, cranial neuritis and others. Children with EBV encephalitis rarely present with infectious mononucleosis symptoms so this particular virus should be considered in any child with acute childhood encephalitis, irrespective of associated symptoms. In a review of 21 children with EBV encephalitis, >50 % had other pathogens identified either by CSF PCR or serology. Additional reports of EBV CNS coinfections have been published [16, 17]. The role of EBV in meningoencephalitis is unclear, so it is not surprising that conventional testing did not include EBV for any patient in this study. Furthermore, the recently FDA cleared FA ME does not include EBV due to the difficulty in interpretation.
The FA ME panel was not capable of detecting organisms, such as WNV and Histoplasma, which are not included in the panel. Despite WNV being prevalent in Texas (the location of 4 enrolling hospitals) [18], only 19 (39.6 %) were tested for WNV with serology. Similarly, in a review of 323 patients with aseptic meningoencephalitis, <50 % had WNV serology performed [1]. The addition of arboviral serology to routine evaluation [1] (CSF WNV IgM, serum WNV IgM/IgG) during peak summer months would improve yield of diagnostic evaluation. Histoplasmosis is similarly common in Texas [19], often presenting in immunocompromised patients with chronic meningitis [13]. Only one patient in our study was identified to have Histoplasmosis (positive urinary Histoplasma antigen test) and was immunocompromised (AIDS). Special stains of sputum, blood, CSF as well as CSF antigen, CSF Ab test, and fungal culture, none of which were used, can also identify H. capsulatum. A fungal stain was not done in our patient, only a fungal culture.
Our study had several limitations. First, our study was observational so routine evaluation was driven by independent physicians (versus a standardized diagnostic workup). The variability in diagnostic evaluation resulted in incomplete data and hence inability to perform complete analysis of the FA ME panel dynamics including sensitivity and specificity. Secondly, the study involved 4 different institutions each with independent laboratories among which assays differing in sensitivity could have affected patient results. Furthermore, the use of residual CSF might lead to a selection bias. And finally, FA ME testing was only performed on those patients with additional CSF available, which could have resulted in a selection bias.
In conclusion, we compared the performance of standard evaluation to the BioFire Film Array Meningitis/Encephalitis panel in 48 patients. The BioFire FA ME panel detected organisms that were missed by conventional laboratory studies. The BioFire ME panel cannot replace some conventional laboratory studies, because it does not test for all organisms responsible for meningitis and encephalitis. FA ME offered comprehensive, standard, rapid testing with minimal use of CSF volume. Rapid, comprehensive testing for the most common pathogens causing meningitis will aid in the diagnosis and treatment of patients with central nervous system infections.
References
Nesher L, Hadi CM, Salazar L, Wootton SH, Garey K, Luce AM, Hasbun R. Epidemiology of meningitis with a negative CSF Gram stain: under-utilization of available diagnostic tests. Epidemiol Infect Jan. 2015;144(1):189–97.
Xu J, Moore JE, Millar BC, Webb H, Shields MD, Goldsmith CE. Employment of broad range 16S r DNA PCR and sequencing in the detection of aetiological agents of meningitis. New Microbiol. 2005;28:135–43.
Buss SN, Leber A, Chapin K, Fey PD, Bankosky MJ, Jones MK, Rogatcheva M, Kanack KJ, Bourzac KM. Multicenter evaluation of the BioFire FilmArray gastrointestinal panel for etiologic diagnosis of infectious gastroenteritis. J Clin Microbiol. 2015;53(3):915–25.
Debiasi RL, Tyler KL. Molecular methods for diagnosis of viral encephalitis. Clin Microbiol Rev. 2004;17:903–25.
Southern TR, VanSchooneveld TC, Bannister DL, Brown TL, Crismon AS, Buss SN, Iwen PC, Fey PD. Implementation and performance of the BioFire FilmArray ®blood culture identification panel with antimicrobial treatment recommendations for bloodstream infections at a Midwestern academic tertiary hospital. Diagn Microbiol Infect Dis. 2015;81(20):96–101.
Blaschke AJ, Heyrend C, Byington CL, Fisher MA, Barker E, Garrone NF, Thatcher SA, Pavia AT, Barney T, Alger GD, Daly JA, Ririe KM, Ota I, Poritz MA. Rapid identification of pathogens from positive blood cultures by multiplex polymerase chain reaction using the FilmArray system. Diagn Microbiol Infect Dis. 2012;74(4):349–55.
Poritz MA, Blaschke AJ, Byington CL, Meyers L, Nilsson K, Jones DE, Thatcher SA, Robbins T, Lingenfelter B, Amiott E, Herbener A, Daly J, Dobrowolski SF, Teng DH, Ririe KM. FilmArray, an automated nested multiplex pcr stystem for multi-pathogen detection: development and application to respiratory tract infection. PLoS ONE. 2011;6(10):e26047.
Babedy NE. The FilmArray respiratory panel: an automated, broadly multiplexed molecular test for the rapid and accurate detection of respiratory pathogens. Expert Rev Mol Diagn. 2013;13(8):779–88.
Hanson, KE. Slechta ES, Killpact JA et al. Preclinical assessment of a fully automated multiplex PCR panel for the detection of central nervous system pathogens. J Clin Microbiol. 2015 [Epub ahead of print] PMID: 26719439.
Rhein J, Cloud J, Hemmert A, Bahr N, Bellamkonda S, Oswald C, Lo E, Nabeta H, Kiggundu R, Akampuria A, Williams D, Meya D, Boulware D. Diagnostic performance of a multiplex PCR assay for meningitis in an HIV-infected population in Uganda. Poster Presentation (#1432), ID Week 2014 Meeting, Philadelphia. 2014.
Rhein J, Bahr NC, Hemmert AC, et al. Diagnostic performance of a multiplex PCR assay for meningitis in an HIV infected population in Uganda. Diagn Microbiol Infect Dis. 2016;84(3):266–73.
Wootton SH, Aguilera EA, Salazar L, Hemmert, AC. Enhancing pathogen identification using a comprehensive PCR system in adult and pediatric patients with meningitis and a negative gram stain. Poster presentation (#843), ID Week 2014 Meeting, Philadelphia. 2014.
Tunkel AR, Glaser CA, Block KC, Sejvar JJ, Marra CM, Roos KL, Hartman BJ, Kaplan SL, Scheld WM, Whitley RJ. The management of encephalitis: clinical practice guidelines by the infectious diseases society of america. Clin Infect Dis. 2008;47(3):303–27.
Sullivan CE, Aksamit AJ, Harrington JR, Harmsen WS, Mitchell PS, Patel R. Clinical spectrum and laboratory characteristics associated with detection of herpes simplex virus DNA in cerebrospinal fluid. Mayo Clin Proc. 2003;78(11):1347–52.
Becerra JCL, Seiber R, Martinetti G, Costa ST, Meylan P, Bernasconi E. Infection of the central nervous system caused by varicella zoster virus reactivation: a retrospective case series study. Int J Infect Dis. 2013;17(7):e529–34.
Weinberg A, Bloch KC, Shaobing L, Tang YW, Palmer M, Tyler KL. Dual infections of the nervous system with Epstein-Barr virus. J Infect Dis. 2005;191:234–7.
Tang YW, Espy MJ, Persing DH, Smith TF. Molecular evidence and clinical significance of herpesvirus coinfection in the central nervous system. J Clin Microbiol. 1997;35:869–72.
Murray KO, Ruktanonchai D, Hesalroad D, Fonken E, Nolan MS. West Nile virus, Texas, USA, 2012. Emerg Infect Dis. 2013;19(11):1836–8.
Chu JH, Feudtner C, Heydon K, Walsh TJ, Zaoutis TE. Hospitalizations for endemic mycoses: a population-based national study. Clin Infect Dis. 2006;42(6):822–5.
Authors’ contributions
SW conceptualized and designed the study, designed the data collection instruments, supervised the data collectionand drafted the initial manuscript. RH conceptualized and designed the study, designed the data collection instruments, supervised the data collection and reviewed the final mansucript. EA and LS did the data extraction and reviewed the final manuscript. EA and SW created the Table. AH performed the Film Array analysis of the samples and reviewed the final manuscript. All authors read and approved the final manuscript.
Acknowledgements
We want to thank Mr. and Mrs. Starr for their continuous support of our studies through their Grant A Starr Foundation.
Funding
Financial support for this project included funding from the Grant-A-Starr Foundation (SW) and the NIH 1 K23 RR01892901A2 (RH). The funding organizations did not play a role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests
Andrew Hammert, Ph.D. is employed by BioFire and Rodrigo Hasbun, MD is a consultant for Biofire. Biofire performed the Film Array panel for the study but had no role in the study design, data collection or preparation of manuscript. All other authors have verified that they do not have commercial or other associations that might pose a competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wootton, S.H., Aguilera, E., Salazar, L. et al. Enhancing pathogen identification in patients with meningitis and a negative Gram stain using the BioFire FilmArray® Meningitis/Encephalitis panel. Ann Clin Microbiol Antimicrob 15, 26 (2016). https://doi.org/10.1186/s12941-016-0137-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-016-0137-1