Abstract
Background
Arsenic exposure through drinking water is an established lung carcinogen. Evidence on non-malignant lung outcomes is less conclusive and suggests arsenic is associated with lower lung function. Studies examining low-moderate arsenic (< 50 μg/L), the level relevant for most populations, are limited. We evaluated the association of arsenic exposure with respiratory health in American Indians from the Northern Plains, the Southern Plains and the Southwest United States, communities with environmental exposure to inorganic arsenic through drinking water.
Methods
The Strong Heart Study is a prospective study of American Indian adults. This analysis used urinary arsenic measurements at baseline (1989–1991) and spirometry at Visit 2 (1993–1995) from 2132 participants to evaluate associations of arsenic exposure with airflow obstruction, restrictive pattern, self-reported respiratory disease, and symptoms.
Results
Airflow obstruction was present in 21.5% and restrictive pattern was present in 14.4%. The odds ratio (95% confidence interval) for obstruction and restrictive patterns, based on the fixed ratio definition, comparing the 75th to 25th percentile of arsenic, was 1.17 (0.99, 1.38) and 1.27 (1.01, 1.60), respectively, after adjustments, and 1.28 (1.02, 1.60) and 1.33 (0.90, 1.50), respectively, based on the lower limit of normal definition. Arsenic was associated with lower percent predicted FEV1 and FVC, self-reported emphysema and stopping for breath.
Conclusion
Low-moderate arsenic exposure was positively associated with restrictive pattern, airflow obstruction, lower lung function, self-reported emphysema and stopping for breath, independent of smoking and other lung disease risk factors. Findings suggest that low-moderate arsenic exposure may contribute to restrictive lung disease.
Similar content being viewed by others
Introduction
Arsenic exposure via drinking water is a well-established lung carcinogen [1,2,3]. More recently, water arsenic > 100 μg/L has been associated with non-malignant respiratory effects, including respiratory symptoms and worse lung function tests. A recent meta-analysis identified an association between arsenic exposure and reduced forced vital capacity (FVC) and forced expiratory volume in 1 s (FEV1) with a preserved ratio (in subset of 3 studies reporting FEV1/FVC), indicating a possible association with restrictive lung disease [4]. The studies in the meta-analysis included a wide range of exposure levels, with arsenic often 10 times higher than the World Health Organization guideline/United States Environmental Protection Agency standard of 10 μg/L in drinking water. More evidence is needed at low-moderate levels of arsenic exposure (< 50 μg/L), and levels common in the US and other countries (< 10 μg/L). A recent systematic review showed strong evidence of an association between high levels of arsenic exposure with respiratory symptoms, non-malignant respiratory illness, and reduced lung function [5]. One study from the US found no association between low-moderate arsenic exposure and self-reported diagnosis or symptoms of obstructive lung disease but lacked spirometry data [6]. We examined the association of low-moderate arsenic exposure with respiratory health in American Indians from the Northern Plains, the Southern Plains and the Southwest United States, communities with environmental exposure to inorganic arsenic through drinking water.
Methods
Study population
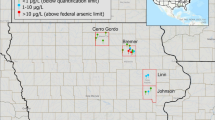
The Strong Heart Study (SHS) is an ongoing population-based, prospective study of cardiovascular disease and its risk factors in American Indian adults. The SHS recruited 4549 residents of Tribal Nations from study sites located in Arizona (AZ), Oklahoma (OK), and North Dakota and South Dakota (ND/SD) in the US. Study enrollment rates were 71.8% in AZ, 61.5% in OK, and 55.3% in ND/SD [7]. All men and women aged 45 to 74 years at the baseline visit in 1989–1991 were invited to participate, with subsequent clinical visits [8]. In 2016, one community in Arizona withdrew their consent, reducing the cohort to 3516 participants. To account for the unintended withdrawal of a Tribal Nation, all analyses were weighted using inverse probability weighting. As study site proportion is known from the original cohort, the withdrawal of the Tribal Nation was adjusted for by weighting the remaining participants, with approximately 1/3 of weight for each center (33.0% AZ, 33.6% OK, 33.4% ND/SD); the use of the statistical weight is to reduce bias introduced by drop-out [9].
This study uses urinary arsenic data from the baseline examination and spirometry from Visit 2 (1993–1995), both available in 2271 participants. We excluded 94 participants missing baseline data on smoking status and cigarette pack-years, 11 missing diabetes status, education, or body mass index (BMI), and 34 missing tuberculosis data, leaving 2132 participants.
Data collection
Visits included biospecimen collection, physical exam, and an interviewer-administered standardized questionnaire. Visits were performed by trained and certified examiners. Details have been described previously [8].
Urine arsenic
Morning spot urine samples were collected at baseline [8]. For arsenic analyses, urine concentrations of inorganic arsenic (iAs), methylarsonate (MMA), and dimethylarsinate (DMA) were measured using high performance liquid chromatography/inductively coupled plasma-mass spectrometry. The metabolism of inorganic arsenic in the human body results in MMA and DMA which are excreted in urine together with unchanged inorganic arsenic. Quality control and assurance methods and laboratory procedures for urine analysis have been described [10]. We used the sum of inorganic and methylated arsenic species (iAs + MMA + DMA) as the biomarker of exposure to inorganic arsenic in drinking water and food. Arsenobetaine levels are low in the population (median (10th, 90th percentiles): 0.5 μg/g (< 0.6–6.10) creatinine], confirming that seafood intake is rare [11]. Urine arsenic concentrations (μg/L) were divided by urine creatinine concentrations (g/L) to account for urine dilution in spot urine samples and expressed as concentrations of total urine arsenic and its species in μg/g creatinine.
Spirometry for identification of airflow obstruction and restrictive pattern
Spirometry was performed by trained and certified nurses and technicians [12]. Pre-bronchodilator testing was conducted while sitting, except for participants with BMI > 27 kg/m2 who stood. Maneuvers were considered acceptable to then-current American Thoracic Society recommendations [12, 13].
Spirometry metrics FEV1, FVC, and FEV1/FVC were used in analyses. Reference values for SHS participants were derived previously [12] yielding FVC %predicted and FEV1%predicted. The prevalence of airflow obstruction was defined by a fixed ratio of FEV1/FVC < 0.70 using crude values [14]. A low FVC (< 80%predicted) together with a preserved ratio (FEV1/FVC ≥ 0.70) was defined as restrictive pattern [15]. Healthy individuals (controls) were those with no-obstruction and no-restriction (FEV1/FVC > 0.70 and FVC > 80%predicted). We conducted secondary analyses with the lower limit of normal (LLN = 5th percentile of the frequency distribution of reference values; obstruction: FEV1/FVC < LLN; restriction: FEV1/FVC > LLN and FVC < LLN; healthy: FEV1/FVC > LLN and FVC > LLN).
Symptoms and lung disease
At Visit 2, participants were asked to report respiratory symptoms including cough (“Do you usually have a cough?”, frequent cough (“Do you usually cough as much as 4-6 times/day, 4 or more days/week?”), cough with phlegm (“Do you usually bring up phlegm when you cough?”), shortness of breath (“Are you troubled by shortness of breath when hurrying on the level or walking up a slight hill?”), and stopping for breath while walking (“Do you ever have to stop for breath while walking about 100 yards or a few minutes on the level?”). Participants self-reported if a medical person ever told them they had emphysema, asthma, or chronic bronchitis diagnoses, which was recorded at Visit 2.
Other variables
At the baseline visit, sociodemographic (age, sex, education, and study site) and life-style (smoking status and smoking pack-years) variables were ascertained through a standardized questionnaire by trained and certified interviewers [8]. Smoking status was categorized as never, former, or current. Former: smoked ≥100 cigarettes but no longer smoking; Never: smoked < 100 cigarettes in lifetime; and Current: smoking at then-present day. Height and weight measurements for BMI calculation (weight in kilograms divided by height in meters squared) were conducted during the physical exam. Chronic kidney disease was defined as estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73m2 based on serum creatinine using the Modification of Diet in Renal Disease equation [16]. Diabetes was defined as a fasting glucose level of ≥126 mg/dL, a 2-h post-load plasma glucose level of ≥200 mg/dL, an HbA1c level of ≥6.5%, or use of an oral hypoglycemic agent or insulin [17].
At Visit 2, a medical record review for a history of active and treated tuberculosis (class III tuberculosis) was performed. Case definition for class III tuberculosis involved having a positive culture for Mycobacterium tuberculosis from a body fluid or tissue or having a clinical picture suggestive of tuberculosis that responded to treatment with antitubercular medications. If the individual had active tuberculosis listed on a discharge diagnosis or on a problem list, they were considered to have a history of tuberculosis.
Statistical analysis
We conducted descriptive statistics to evaluate differences in participant demographic and lifestyle variables by obstruction and restrictive pattern and by urinary arsenic tertile. We used logistic regression to estimate the odds ratio [OR] for presence of obstruction/restrictive pattern, respiratory symptoms and disease by urinary arsenic concentrations, and linear regression to assess the mean difference of spirometric measurements. We modelled arsenic exposure using three approaches: a categorical variable, comparing tertiles of arsenic exposure; a continuous variable to compare an interquartile (IQR) increase of log urinary arsenic; and a continuous variable with splines with knots at the 10th, 50th, and 90th percentiles (3.8, 10.2, and 25.8 μg/g creatinine, respectively) to allow for a flexible dose-response relationship. P values for trend were obtained from modelling log-arsenic as continuous. Models were progressively adjusted (see footnotes of Tables 3, 4, 6).
Effect modification of the association was evaluated depending on confounding variables by including interaction terms for log-transformed urinary arsenic concentrations with indicator variables for sex, age, smoking status, BMI, and diabetes. P values for interactions were obtained using Wald test for multiple coefficients. To evaluate arsenic metabolism, we examined the association between the relative proportions of arsenic species in urine per 5% change and presence of obstruction/restrictive pattern.
Results
Obstruction was present in 21.5% (458/2132) and restrictive pattern present in 14.4% (307/2132). Obstruction and restrictive pattern demographics are described in Table 1. Obstruction was present in 31.0% vs. 20.7% of participants in the highest vs. lowest arsenic exposure tertiles (p = 0.02); restrictive pattern was present in 23.8% vs. 17.2% of participants in corresponding tertiles (p < 0.001) (Table 2).
After full adjustment (age, sex, education, site, smoking status, smoking pack-year, eGFR, tuberculosis, and BMI) (Table 3, model 3), the odds ratio [95% CI] comparing the highest to lowest arsenic tertile (≥14.0 vs. ≤7.0 μg/g creatinine) was 1.33 [0.99, 1.77] for obstruction and 1.34 [0.92, 1.96] for restrictive pattern. The corresponding OR [95%CI] for an interquartile range (IQR) increase of arsenic was 1.17 [0.99, 1.38] (P for trend 0.07) for obstruction and 1.27 [1.01, 1.60] (P for trend 0.04) for restrictive pattern (Table 3, model 3). Modelling urinary arsenic using flexible splines, showed positive and linear associations with restrictive pattern and airflow obstruction that were suggestive but nonsignificant in the complete sample (Fig. 1). Results were unchanged in analyses excluding 5 participants above the 99th percentile of %predicted FEV1 and FVC (results not shown). In a sensitivity analysis with further adjustment for diabetes, the OR for obstruction per change in arsenic IQR remained similar (1.17 [0.99, 1.40] (P for trend 0.07)), and for restrictive pattern the OR was attenuated (1.18 [0.93, 1.50] (P for trend 0.18)) (Table 3).
Dose-Response Relationship of Fixed Airflow Obstruction and Restrictive Pattern with Urinary Arsenic Concentrations. Solid lines and shaded areas surrounding the lines represent the weighted odds ratio and 95% confidence intervals of airflow obstruction (upper panels) and restrictive pattern (lower panels). Models were conducted in the total study sample (left panels), stratified by sex (middle panels), and stratified by smoking status (right panels). These models were adjusted for age, sex (except models stratified by sex), education, study site, smoking status (except models stratified by smoking status), smoking pack-year, eGFR, tuberculosis and BMI. Histograms in the background and right Y axis represent the distribution of urinary arsenic. The histograms were truncated by excluding 10 participants with urine arsenic concentrations above 65 μg/g of creatinine
Using the LLN definition, obstruction was present in 7.1% (151/2132) and restrictive pattern in 6.9% (147/2132). The ORs for the association based on the LLN were stronger compared to the fixed ratio and were significant for obstruction (OR [95%CI] per IQR) (1.28 [1.02, 1.60] (P for trend 0.03) but non-significant for restriction (1.33 [0.90, 1.50] (P for trend 0.06) (Table 4).
The mean difference [95% CI] for FEV1%predicted for an IQR change in urinary arsenic was − 1.39 [− 2.51, − 0.25] (P for trend 0.02), although the trend was non-linear by tertile (Table 5) and flexible splines (Fig. 2). The %predicted association remained significant after further adjustment for diabetes in the sensitivity analyses (Additional file 1: Table S1). For FVC %predicted, the mean difference [95% CI] per IQR change in arsenic was − 1.13 [− 2.21, − 0.05] (P for trend 0.04). Among the healthy group, the mean difference for FEV1%predicted and FVC %predicted both became non-significant (Table 5) and remained non-significant in the sensitivity analysis (Additional file 1: Table S1). Wald test results for non-linear components of the spline model were p = < 0.001 for FEV1%predicted and p = 0.005 for FVC %predicted. No association was found between arsenic and FEV1/FVC. Using crude FEV1 and FVC measures (mL) the mean differences were significant (Table 5).
Dose-Response Relationship of Lung Function at Visit 2 (1993–1995) with Urinary Arsenic Concentrations. Solid lines and shaded areas surrounding the lines represent the weighted mean differences and 95% confidence intervals of FEV1% predicted (right panels), FVC % predicted (middle panels), and FEV1/FVC (right panels Models were conducted in the total study sample (upper panels) and stratified by sex (lower panels). These models were adjusted for age, sex (except models stratified by sex), education, study site, smoking status, smoking pack-year, eGFR, tuberculosis and BMI. Histograms in the background and right Y axis represent the distribution of urinary arsenic. The histograms were truncated by excluding 10 participants with urine arsenic concentrations above 65 μg/g of creatinine
We found no effect modification for the association of arsenic with obstruction/restrictive pattern by age, BMI, or diabetes (Additional file 1: Table S2). By sex, effect modification was significant for obstruction (P = 0.003), with an association found in men (OR [95%CI]) (1.47 [1.07, 2.06]) but not significant in women (1.07 [0.82, 1.33]). By smoking status, the association with arsenic was strongest in former smokers both for obstruction (1.74 [1.20, 2.55]) and restrictive pattern (1.34 [0.82, 2.17]) compared to never or current smokers, but confidence intervals overlapped in both analyses. Urinary relative proportions of iAs, MMA, and DMA were not associated with obstruction/restrictive pattern (Additional file 1: Table S4).
Urinary arsenic was inversely associated with cough (OR [95%CI] per IQR) (0.78 [0.65, 0.93]), but not with frequent cough (4–6x/day) or production of phlegm (Table 6). There was no association between arsenic and shortness of breath, but arsenic was positively associated with stopping for breath while walking (1.41 [1.19, 1.69]) (Table 6). Urinary arsenic was positively associated with emphysema (OR [95%CI] per IQR) (1.66 [1.29, 2.15]); inversely associated with asthma (0.76 [0.61, 0.96]) and not associated with chronic bronchitis (Additional file 1: Table S3).
Discussion
Exposure to low-moderate levels of inorganic arsenic was associated with increased odds of fixed ratio restrictive lung pattern, lower FEV1 and lower FVC, borderline associated with fixed ratio obstruction, and not associated with FEV1/FVC. The associations based on the LLN became stronger and significant for obstruction and stronger but non-significant for restrictive pattern. Arsenic was also associated with stopping for breath while walking and with higher self-reported emphysema. The association with restrictive pattern is consistent with recent meta-analysis findings that suggested low-level arsenic exposure is a restrictive lung disease risk factor [4]. There is debate over using the fixed ratio definition of obstruction, which can potentially lead to over-diagnoses in older individuals [18, 19]. However, there are also limitations with LLN-defined obstruction, which can underestimate airflow obstruction [20]. The stronger but non-significant effect estimates we see for the association between arsenic and LLN-defined restrictive pattern may be due to a more specific definition and exclusion of less severe cases.
Restrictive pattern findings remained significant after adjustment for smoking (status and pack-years), a major risk factor for reduced pulmonary function [21, 22]. In a sensitivity analysis (results not shown), we adjusted for additional adiposity factors (% body fat, waist circumference) to account for mechanical constraints of obesity-related lung restriction [23] with consistent findings. Adjustment for diabetes, however, attenuated the association, which became non-significant. The definitive direction as well as the exact pathophysiological mechanism to explain the association between diabetes and lung function is not known [24]; in the Strong Heart Study, impaired lung function presented before the development of diabetes [25]. Previous similar studies have not adjusted for diabetes, but there is a large body of evidence suggesting that chronic arsenic exposure can contribute to diabetes development [26], and diabetes could be in the causal pathway between arsenic and restrictive lung pattern. Lung restriction in diabetes can result from chronic low-grade inflammation of the lung tissue; lung volume has been found to inversely correlate with the level of systemic inflammation, [24] with a restrictive pattern of lung function loss associated with systemic inflammation [27].
There is consistent evidence that increasing arsenic exposure is associated with reports of coughing and breathing problems [5]. However, we only found a positive association between arsenic and with the need to stop for breath and a reduced odds of cough. One study in the US also found lower odds of chronic cough in participants with greater than the 80th (< 17.23 μg/L) arsenic percentile compared to those with less than the 20th (< 3.52 μg/L) percentile [6]. The same study reported greater odds of self-reported emphysema, similar to our findings, among those with the highest quartile of urinary arsenic compared to the lowest, but results were non-significant [6]. Four studies have examined arsenic and chronic bronchitis; three found a greater odds [28,29,30] and one found reduced odds [6].
Despite epidemiologic evidence, little is known regarding arsenic-induced effects on airway physiology [31, 32]. Rather than a direct toxic effect of arsenic on the lung, an inflammation-mediated immunologic basis is suggested [33], as arsenic is known to alter key functions of the innate and adaptive immune system [34,35,36,37]. One possible mechanism is aberrant airway remodeling targeted by arsenic following activation of inflammatory mediators. Airway remodeling has been linked to the equilibrium between proteases matrix metalloproteinase-9 (MMP-9) and its inhibitors, receptor for advanced glycation end products (RAGE) [38]. Loss of the soluble form of RAGE, sRAGE, is related to functional changes of pulmonary cell types, with consequences of fibrotic disease. Arsenic may change RAGE gene expression by altering the promoter region methylation or by affecting transcriptional regulators of RAGE. In humans, sputum sRAGE levels were negatively correlated with urinary arsenic levels, similar to animal models [39]. In vitro models have shown arsenic exposure increases activity and expression of MMP-9 in airway epithelial cells [40].
This study had several limitations. We measured urinary arsenic levels in a single sample at baseline, while spirometric measurements were taken at Visit 2. However, the temporal stability of arsenic levels in drinking water and urine has been shown in this population [11]. Spirometry was originally performed for better prediction of cardiovascular disease [13]. We did not have total lung capacity measurements, often not available for large population screenings, and could not confirm restriction presence. We also could not confirm the presence of obstructive disease without post-bronchodilator spirometry. Thus, we cannot discard the possibility that the association we found may be due to mixed ventilatory defect. Outcome misclassification could have occurred from inaccurate recall of disease diagnosis. The reason we saw a significant relationship between arsenic and obstruction only in former smokers is unknown. A few studies have reported similar findings, with authors suggesting the toxic effects of smoking could be masking those of arsenic [28, 41]. A recent meta-analysis found the association between arsenic and FVC to be slightly stronger among non-smokers than smokers, also for reasons unknown [4]. This finding, too, is surprising, as generally the quickest benefit after quitting cigarette smoking is improvement in lung function. This further points to the possibility that active smoking’s toxic effects could be masking those of arsenic; however, this is speculative.
Strengths of this study include having American Indian reference values derived from the SHS cohort [12]. This is important as anthropomorphic differences vary between ethnic groups, and NHANES III, from which normative values are generated, did not include American Indians. The reference values allowed for results to be evaluated for abnormalities against predicted values for better interpretation of results. Other major strengths include the community-based sample, standardized spirometry, and extensive data on potential confounders.
Conclusions
Our study provides evidence of an association between low-moderate arsenic exposure and a spirometric restrictive pattern, airflow obstruction (especially based on the LLN), and higher self-reported emphysema and stopping for breath. No other study has evaluated the association between arsenic exposure and individual spirometric lung function in American Indians, US population, or population exposed to low-moderate arsenic levels. Research in additional populations is needed to confirm the association, including evaluation of relevant subclinical and pathophysiological outcomes. This could include repeated urinary arsenic measurement and diagnostic testing, like computed tomography scan, to better assess patterns of lung disease.
Availability of data and materials
Strong Heart Study data are shared with researchers following Resource and Data Sharing Policies, which include review and approval from the Strong Heart Study Steering Committee and Strong Heart Study participating tribes.
Change history
26 February 2020
The original version of this article [1], published on 28 November 2019, contained incorrect title. In this Correction the affected part of the article is shown.
Abbreviations
- BMI:
-
Body mass index
- DMA:
-
Dimethylarsinate
- FEV1:
-
Forced expiratory volume in one second
- FVC:
-
Reduced forced vital capacity
- iAs:
-
Inorganic arsenic
- IQR:
-
Interquartile range
- LLN:
-
Lower limit of normal, the 5th percentile of the frequency distribution of reference values
- MMA:
-
Methylarsonate
- OR:
-
Odds ratio
- SHS:
-
Strong Heart Study
References
Smith AH, Ercumen A, Yuan Y, Steinmaus CM. Increased lung cancer risks are similar whether arsenic is ingested or inhaled. J Expo Sci Environ Epidemiol. 2009;19(4):343–8. https://doi.org/10.1038/jes.2008.73 Epub 2009/02/05. PubMed PMID: 19190673; PMCID: Pmc2682945.
Smith AH, Marshall G, Yuan Y, Ferreccio C, Liaw J, von Ehrenstein O, Steinmaus C, Bates MN, Selvin S. Increased mortality from lung Cancer and bronchiectasis in young adults after exposure to arsenic in utero and in early childhood. Environ Health Perspect. 2006;114(8):1293–6. https://doi.org/10.1289/ehp.8832.
IARC. Arsenic and Arsenic Compounds: International Agency for Resarch on Cancer: World Health Organization; 2004. Available from: http://monographs.iarc.fr/ENG/Monographs/vol100C/mono100C-6.pdf. Accessed 12 Dec 2018.
Sanchez TR, Powers M, Perzanowski M, George CM, Graziano JH, Navas-Acien A. A meta-analysis of arsenic exposure and lung function: is there evidence of restrictive or obstructive lung disease? Curr Environ Health Rep. 2018. https://doi.org/10.1007/s40572-018-0192-1 Epub 2018/04/11. PubMed PMID: 29637476.
Sanchez TR, Perzanowski M, Graziano JH. Inorganic arsenic and respiratory health, from early life exposure to sex-specific effects: A systematic review. Environ Res. 2016;147:537–55. https://doi.org/10.1016/j.envres.2016.02.009 zPubMed PMID: 26891939; PMCID: PMC4821752.
Amster ED, Cho JI, Christiani D. Urine arsenic concentration and obstructive pulmonary disease in the U.S. population. J Toxicol Environ Health A. 2011;74(11):716–27. https://doi.org/10.1080/15287394.2011.556060 PubMed PMID: 21480046; PMCID: PMC3655422.
Stoddart ML, Jarvis B, Blake B, Fabsitz RR, Howard BV, Lee ET, Welty TK. Recruitment of American Indians in epidemiologic research: the strong heart study. Am Indian Alsk Native Ment Health Res. 2000;9(3):20–37 Epub 2001/04/04. PubMed PMID: 11279560.
Lee ET, Welty TK, Fabsitz R, Cowan LD, Le NA, Oopik AJ, Cucchiara AJ, Savage PJ, Howard BV. The strong heart study. A study of cardiovascular disease in American Indians: design and methods. Am J Epidemiol. 1990;132(6):1141–55 Epub 1990/12/01. PubMed PMID: 2260546.
Hofler M, Pfister H, Lieb R, Wittchen HU. The use of weights to account for non-response and drop-out. Soc Psychiatry Psychiatr Epidemiol. 2005;40(4):291–9. https://doi.org/10.1007/s00127-005-0882-5 Epub 2005/04/19. PubMed PMID: 15834780.
Scheer J, Findenig S, Goessler W, Francesconi KA, Howard B, Umans JG, Pollak J, Tellez-Plaza M, Silbergeld EK, Guallar E, Navas-Acien A. Arsenic species and selected metals in human urine: validation of HPLC/ICPMS and ICPMS procedures for a long-term population-based epidemiological study. Anal Methods. 2012;4(2):406–13. https://doi.org/10.1039/c2ay05638k Epub 2012/06/12. PubMed PMID: 22685491; PMCID: Pmc3368501.
Navas-Acien A, Umans JG, Howard BV, Goessler W, Francesconi KA, Crainiceanu CM, Silbergeld EK, Guallar E. Urine arsenic concentrations and species excretion patterns in American Indian communities over a 10-year period: the Strong Heart Study. Environ Health Perspect. 2009;117(9):1428–33. https://doi.org/10.1289/ehp.0800509 PubMed PMID: 19750109; PMCID: PMC2737021.
Marion M, Leonardson G, Rhoades E, Welty T, Enright P. Spirometry reference values for American Indian adults: results from the strong heart study. Chest. 2001;120(2):489–95.
SHS. Strong Heart Study, Spirometry- Manual of Operations. In: Center SHSC. Oklahoma City: Strong Heart Study; 1993.
GOLD. Global Initiative for Chronic Obstructive Lung Disease (GOLD) Spirometry 2010. Available from: http://goldcopd.org/wpcontent/uploads/2016/04/GOLD_Spirometry_2010.pdf. Accessed 19 June 2017.
Crapo RO. Pulmonary-function testing. N Engl J Med. 1994;331(1):25–30. https://doi.org/10.1056/nejm199407073310107 Epub 1994/07/07. PubMed PMID: 8202099.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med. 1999;130(6):461–70 Epub 1999/03/13. PubMed PMID: 10075613.
Gribble MO, Howard BV, Umans JG, Shara NM, Francesconi KA, Goessler W, Crainiceanu CM, Silbergeld EK, Guallar E, Navas-Acien A. Arsenic exposure, diabetes prevalence, and diabetes control in the strong heart study. Am J Epidemiol. 2012;176(10):865–74 PubMed PMID: 23097256.
Stanojevic S, Wade A, Stocks J, Hankinson J, Coates AL, Pan H, Rosenthal M, Corey M, Lebecque P, Cole TJ. Reference ranges for spirometry across all ages: a new approach. Am J Respir Crit Care Med. 2008;177(3):253–60. https://doi.org/10.1164/rccm.200708-1248OC Epub 2007/11/17. PubMed PMID: 18006882; PMCID: Pmc2643211.
Hardie JA, Buist AS, Vollmer WM, Ellingsen I, Bakke PS, Morkve O. Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. Eur Respir J. 2002;20(5):1117–22 Epub 2002/11/27. PubMed PMID: 12449163.
Mohamed Hoesein FA, Zanen P, Lammers JW. Lower limit of normal or FEV1/FVC < 0.70 in diagnosing COPD: an evidence-based review. Respir Med. 2011;105(6):907–15. https://doi.org/10.1016/j.rmed.2011.01.008 Epub 2011/02/08. PubMed PMID: 21295958.
Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765–73. https://doi.org/10.1016/s0140-6736(07)61380-4 Epub 2007/09/04. PubMed PMID: 17765526.
Bhat TA, Panzica L, Kalathil SG, Thanavala Y. Immune Dysfunction in Patients with Chronic Obstructive Pulmonary Disease. Ann Am Thorac Soc. 2015;12(Suppl 2):S169–75. https://doi.org/10.1513/AnnalsATS.201503-126AW Epub 2015/11/26. PubMed PMID: 26595735; PMCID: Pmc4722840.
Zammit C, Liddicoat H, Moonsie I, Makker H. Obesity and respiratory diseases. Int J Gen Med. 2010;3:335–43 PubMed PMID: 21116339.
Klein OL, Krishnan JA, Glick S, Smith LJ. Systematic review of the association between lung function and type 2 diabetes mellitus. Diabet Med. 2010;27(9):977–87. https://doi.org/10.1111/j.1464-5491.2010.03073.x Epub 2010/08/21. PubMed PMID: 20722670.
Yeh F, Dixon AE, Marion S, Schaefer C, Zhang Y, Best LG, Calhoun D, Rhoades ER, Lee ET. Obesity in adults is associated with reduced lung function in metabolic syndrome and diabetes: the Strong Heart Study. Diabetes Care. 2011;34(10):2306–13. https://doi.org/10.2337/dc11-0682 Epub 2011/08/20. PubMed PMID: 21852681; PMCID: Pmc3177743.
Navas-Acien A, Silbergeld EK, Streeter RA, Clark JM, Burke TA, Guallar E. Arsenic exposure and type 2 diabetes: a systematic review of the experimental and epidemiological evidence. Environ Health Perspect. 2006;114(5):641–8 PubMed PMID: 16675414.
Thyagarajan B, Jacobs DR, Apostol GG, Smith LJ, Lewis CE, Williams OD. Plasma fibrinogen and lung function: the CARDIA study. Int J Epidemiol. 2006;35(4):1001–8. https://doi.org/10.1093/ije/dyl049 Epub 2006/03/24. PubMed PMID: 16554379.
Dauphine DC, Ferreccio C, Guntur S, Yuan Y, Hammond SK, Balmes J, Smith AH, Steinmaus C. Lung function in adults following in utero and childhood exposure to arsenic in drinking water: preliminary findings. Int Arch Occup Environ Health. 2011;84(6):591–600. https://doi.org/10.1007/s00420-010-0591-6 PubMed PMID: 20972800; PMCID: PMC3141825.
von Ehrenstein OS, Mazumder DN, Yuan Y, Samanta S, Balmes J, Sil A, Ghosh N, Hira-Smith M, Haque R, Purushothamam R, Lahiri S, Das S, Smith AH. Decrements in lung function related to arsenic in drinking water in West Bengal. India Am J Epidemiol. 2005;162(6):533–41. https://doi.org/10.1093/aje/kwi236 PubMed PMID: 16093295.
Milton AH, Rahman M. Respiratory effects and arsenic contaminated well water in Bangladesh. Int J Environ Health Res. 2002;12(2):175–9. https://doi.org/10.1080/09603120220129346 PubMed PMID: 12400554.
Sherwood CL, Liguori AE, Olsen CE, Lantz RC, Burgess JL, Boitano S. Arsenic compromises conducting airway epithelial barrier properties in primary mouse and immortalized human cell cultures. PLoS One. 2013;8(12):e82970. https://doi.org/10.1371/journal.pone.0082970 Epub 2013/12/19. PubMed PMID: 24349408; PMCID: Pmc3857810.
Andrew AS, Bernardo V, Warnke LA, Davey JC, Hampton T, Mason RA, Thorpe JE, Ihnat MA, Hamilton JW. Exposure to arsenic at levels found inU.S. drinking water modifies expression in the mouse lung. Toxicol Sci. 2007;100(1):75–87. https://doi.org/10.1093/toxsci/kfm200 Epub 2007/08/08. PubMed PMID: 17682005.
De BK, Majumdar D, Sen S, Guru S, Kundu S. Pulmonary involvement in chronic arsenic poisoning from drinking contaminated ground-water. J Assoc Physicians India. 2004;52:395–400 Epub 2005/01/20. PubMed PMID: 15656029.
Dangleben NL, Skibola CF, Smith MT. Arsenic immunotoxicity: a review. Environ Health. 2013;12(1):73. https://doi.org/10.1186/1476-069x-12-73 Epub 2013/09/06. 24004508; PMCID: Pmc3848751.
Attreed SE, Navas-Acien A, Heaney CD. Arsenic and Immune Response to Infection During Pregnancy and Early Life. Curr Environ Health Rep. 2017, 229;4(2):–43. https://doi.org/10.1007/s40572-017-0141-4 Epub 2017/05/11. PubMed PMID: 28488132; PMCID: Pmc5521214.
Ferrario D, Gribaldo L, Hartung T. Arsenic exposure and Immunotoxicity: a review including the possible influence of age and sex. Curr Environ Health Rep. 2016;3(1):1–12. https://doi.org/10.1007/s40572-016-0082-3 Epub 2016/02/15. PubMed PMID: 26875182.
Heaney CD, Kmush B, Navas-Acien A, Francesconi K, Gossler W, Schulze K, Fairweather D, Mehra S, Nelson KE, Klein SL, Li W, Ali H, Shaikh S, Merrill RD, Wu L, West KP Jr, Christian P, Labrique AB. Arsenic exposure and hepatitis E virus infection during pregnancy. Environ Res. 2015;142:273–80. https://doi.org/10.1016/j.envres.2015.07.004 Epub 2015/07/18. PubMed PMID: 26186135; PMCID: Pmc4609253.
Olivas-Calderon E, Recio-Vega R, Gandolfi AJ, Lantz RC, Gonzalez-Cortes T, Gonzalez-De Alba C, Froines JR, Espinosa-Fematt JA. Lung inflammation biomarkers and lung function in children chronically exposed to arsenic. Toxicol Appl Pharmacol. 2015;287(2):161–7. https://doi.org/10.1016/j.taap.2015.06.001 Epub 2015/06/07. PubMed PMID: 26048584; PMCID: Pmc4751871.
Lantz RC, Lynch BJ, Boitano S, Poplin GS, Littau S, Tsaprailis G, Burgess JL. Pulmonary biomarkers based on alterations in protein expression after exposure to arsenic. Environ Health Perspect. 2007;115(4):586–91 PubMed PMID: 17450228.
Olsen CE, Liguori AE, Zong Y, Lantz RC, Burgess JL, Boitano S. Arsenic upregulates MMP-9 and inhibits wound repair in human airway epithelial cells. Am J Phys Lung Cell Mol Phys 2008;295(2):L293–L302. Epub 2008/06/10. doi: https://doi.org/10.1152/ajplung.00134.2007. PubMed PMID: 18539681; PMCID: Pmc2519851.
Steinmaus C, Ferreccio C, Acevedo J, Balmes JR, Liaw J, Troncoso P, Dauphine DC, Nardone A, Smith AH. High risks of lung disease associated with early-life and moderate lifetime arsenic exposure in northern Chile. Toxicol Appl Pharmacol. 2016;313:10–5. https://doi.org/10.1016/j.taap.2016.10.006 Epub 2016/11/05. PubMed PMID: 27725189; PMCID: Pmc5247272.
Acknowledgements
We thank the SHS participants, Indian Health Service facilities, and participating tribal communities for their extraordinary cooperation and involvement, which has contributed to the success of the Strong Heart Study. The views expressed in this paper are those of the authors and do not necessarily reflect those of the Indian Health Service.
Funding
This study was supported by research grants R01ES021367, R01ES025216, and P42ES010349, R01HL109315, R01HL109301, R01HL109284, R01HL109282 and R01HL109319 and R01HL090863 cooperative agreement grants U01-HL41642, U01-HL41652, U01-HL41654, U01-HL65520, and U01-HL65521; training grant 5T32ES007141–32 and F31ES028597.
Author information
Authors and Affiliations
Contributions
MP, AN-A had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. MP, TRS, MG-P, KAF, WG, CMG, CH, LGB, JGU, RHB, AN-A, contributed substantially to the study design, data analysis and data interpretation. MP, TRS, AN-A contributed substantially to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional and Tribal Review Boards approved all study procedures and all participants provided written, informed consent.
Consent for publication
This paper complies with the Strong Heart Study publication policy and was approved for publication after review by the Strong Heart Study Publications and Presentations Committee.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
Sensitivity Analysis: adjustment for diabetes. Weighted Mean Difference (95% Confidence Interval) of Lung Function at Visit 2 (1993-1995) by Urinary Arsenic Concentration* at Baseline (1989-1991). Table S2. Weighted Odds Ratios (95% Confidence Interval) for Airflow Obstruction and Restrictive Pattern, Defined Based on Fixed Ratios, when an Interquartile Range* of Urinary Arsenic Concentration is Compared, by Participant Characteristics at Baseline. Table S3. Weighted Odds Ratio (95% Confidence Interval) of Self-reported Emphysema, Chronic Bronchitis, or Asthma by Urine Arsenic Tertile Concentration. Table S4. Weighted Odds Ratio (95% Confidence Interval) of Airflow Obstruction and Restrictive Pattern, Defined Based on Fixed Ratios, by 5% Change in Urinary Arsenic Metabolites*.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Powers, M., Sanchez, T.R., Grau-Perez, M. et al. Low-moderate arsenic exposure and respiratory in American Indian communities in the Strong Heart Study. Environ Health 18, 104 (2019). https://doi.org/10.1186/s12940-019-0539-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-019-0539-6