Abstract
Background
Associations between ambient particulate matter < 2.5 μm (PM2.5) and asthma morbidity have been suggested in previous epidemiologic studies but results are inconsistent for areas with lower PM2.5 levels. We estimated the associations between early-life short-term PM2.5 exposure and the risk of asthma or wheeze clinical encounters among Massachusetts children in the innovative Pregnancy to Early Life Longitudinal (PELL) cohort data linkage system.
Methods
We used a semi-bidirectional case-crossover study design with short-term exposure lags for asthma exacerbation using data from the PELL system. Cases included children up to 9 years of age who had a hospitalization, observational stay, or emergency department visit for asthma or wheeze between January 2001 and September 2009 (n = 33,387). Daily PM2.5 concentrations were estimated at a 4-km resolution using satellite remote sensing, land use, and meteorological data. We applied conditional logistic regression models to estimate adjusted odds ratios (ORs) and 95% confidence intervals (CI). We also stratified by potential effect modifiers.
Results
The median PM2.5 concentration among participants was 7.8 μg/m3 with an interquartile range of 5.9 μg/m3. Overall, associations between PM2.5 exposure and asthma clinical encounters among children at lags 0, 1 and 2 were close to the null value of OR = 1.0. Evidence of effect modification was observed by birthweight for lags 0, 1 and 2 (p < 0.05), and season of clinical encounter for lags 0 and 1 (p < 0.05). Children with low birthweight (LBW) (< 2500 g) had increased odds of having an asthma clinical encounter due to higher PM2.5 exposure for lag 1 (OR: 1.08 per interquartile range (IQR) increase in PM2.5; 95% CI: 1.01, 1.15).
Conclusion
Asthma or wheeze exacerbations among LBW children were associated with short-term increases in PM2.5 concentrations at low levels in Massachusetts.
Similar content being viewed by others
Background
Asthma is a common chronic lung disease in which the airways become inflamed and produce increased mucus, making air flow in and out of the lungs difficult. The prevalence of asthma is higher among children 0–17 years of age compared to adults 18 years of age or older [1, 2]. Asthma is typically diagnosed starting at age 5; however symptoms may appear at younger ages. Children under the age of 5 may be more likely to have asthma if they have airborne allergies, wheeze without a cold, and if the parents have been diagnosed with asthma [2]. In addition to family history, children who had previously acquired respiratory syncytial virus (RSV), the virus primarily detected among infants diagnosed with viral bronchiolitis, were more likely to develop wheeze or asthma throughout both childhood and adulthood [3,4,5].
Several environmental exposures have suggested to increase the risk of asthma exacerbation, including both indoor and outdoor air quality [6,7,8,9,10,11]. Ambient air pollutants, including fine particulate matter (PM2.5), have been shown to play a role in adverse respiratory outcomes among children with asthma [12]. PM2.5 represents a combination of small particles and liquid droplets from vehicular exhaust, coal and wood burning, and industrial activities.
Measurements of residential distance to major roads and traffic density have been used as indirect estimates of traffic-related air pollutants due to the difficulty of measuring the mixture of traffic-related pollutants [13, 14]. Adverse respiratory outcomes have also been associated with exposure to areas of high traffic density or near major roadways [15,16,17,18,19]. Concentrations of vehicular pollutants have shown to decline to background levels after 150–300 m (m), while asthma prevalence has been reported to be higher among children who live closer to major roads [16, 17, 20]. The effects of air pollution in both warm and cool seasons have been associated with pediatric asthma attacks [21,22,23,24].
Although adverse health effects of ambient PM2.5 exposure have been shown across all populations, infants and young children are sensitive subgroups. The small size of PM2.5 makes the particles easy to inhale and penetrate deep into the airways [25]. In children, the immune and respiratory systems are not fully developed and their time spent outdoors is greater than adults. Young children also breathe more air per body weight than adults which in turn makes them more susceptible to ambient air pollutant exposures [26].
Notwithstanding some studies associating air pollution exposure and childhood asthma development and exacerbation, it is unclear whether lower levels of PM2.5 trigger the same responses [27,28,29]. In addition, many large population-based studies have not studied effect modification between asthma exacerbations and short-term changes in PM2.5 among potentially susceptible subgroups due to the lack of data. The aims of the study were to investigate the associations between early-life short-term PM2.5 exposure and the risk of asthma or wheeze exacerbation, and to determine if there was any effect modification. To do this, we employed a case-crossover study design with short-term exposure lags using data on clinical encounters among all children 0–9 years of age in Massachusetts (MA) obtained from the innovative pregnancy to Early Life Longitudinal (PELL_ cohort record linkage system.
Methods
Study population
The PELL linkage system links all MA births to administrative databases including hospitalizations, emergency department visits, and observational stays. Pediatric emergency department, hospitalizations, and observational stay data were combined and included in a single analysis because of the similarity of cases. The case definition for asthma or wheeze included the first clinical encounter for children from 0 to 9 years of age using all International Classification of Diseases, Ninth Revision (ICD-9) diagnosis fields (ICD-9 code 493 or 786.07) between January 2001 and September 2009. Our data included street-level birth addresses and zip codes at time of clinical encounter. We excluded children who did not have the same zip code at the time of their clinical encounter and at birth because the PM2.5 concentration at their residence at birth was unlikely to be representative of their PM2.5 exposure at the time of their clinical encounter. We also excluded any children whose birth address was unable to be geocoded and children with birth defects. The final number of participants included in our analysis was 33,387 (see Fig. 1). After PM2.5 exposures were assigned, approximately 10% of our study population had missing PM2.5 estimates and were not included in the analysis. A secondary analysis using only primary and secondary ICD-9 fields was performed to account for any diagnosis misclassification that may result from using all ICD-9 fields (n = 30,301). Because asthma is typically best diagnosed at age 5 or older, a sensitivity analysis was conducted with cases age 5 and older (n = 6195).
Exposure assessment
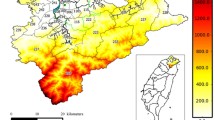
PM2.5 concentrations were modeled spatiotemporally using satellite remote sensing, meteorological and land use data for the same duration as the study period. Daily PM2.5 concentrations in MA were estimated for a 4-km (km) spatial grid from a three-stage statistical model using aerosol optical depth (AOD) data from the Geostationary Operational Environmental Satellite (GOES). The first stage included a linear mixed effects (LME) model accounting for temporal variation between PM2.5 and satellite based AOD by using day-specific random intercepts and slopes for AOD and meteorological data [30, 31]. The second stage accounted for spatial variability between PM2.5 and AOD using a geographically weighted regression (GWR) [32, 33]. Lastly, the third stage used the previously predicted PM2.5 concentrations across the study area from stages 1 and 2 to model areas in the study grid with missing AOD data [34]. However, if AOD data was completely missing for one day then no predictions were made from any stage of the model.
Distance to road (in meters) was estimated using geographic information systems (GIS) for all geocoded births. Road segments were obtained from the MA Department of transportation (MassDOT) roads. Major Roads (CLASS = 1–4) were used in the analysis and include limited access highways, multi-lane highways, numbered routes, and major roads.
Statistical analysis
Odds ratios (OR) and 95% confidence intervals (CI) for asthma clinical encounters were estimated using a conditional logistic regression model per interquartile range (IQR) increase in short-term PM2.5 exposure in a case-crossover study design. Each child served as their own control allowing implicit control for any confounders that do not temporally vary over the short term, including possible indoor air pollutant exposures such as secondhand cigarette smoke and exposures from indoor wood burning. The ‘index date’ was the day each child was considered to be a case based on having an asthma clinical encounter, and the ‘referent date’ was when the child was not considered a case, and served as a self-matched control. We used a semi-symmetric bidirectional referent design minimizing seasonal confounding bias by using narrow referent time periods [35, 36]. Referent dates were the same day of the week as the index date to allow for more accurate exposure assignments since there are differences in PM2.5 emissions depending on the day of the week. To avoid overlap bias, referent days were randomly selected 7 days before or after the clinical event. For any observation where one of the possible referent days did not fall within our study period, we assigned an offset term of log (2) [37]. The analysis used short exposure lags of 0, 1, and 2 days before both the index date and the referent date to analyze asthma symptom exacerbation with exposure to PM2.5.
Changes in residency between clinical encounter and referent date were unlikely to be problematic because the index date and the referent date were only 7 days apart. For this same reason, differences in traffic characteristics on the same day-of-the-week were not controlled for as they were unlikely to change during that time. Variables that were controlled for, and included in the fully adjusted model, were those that had short-term changes including temperature, humidity, barometric pressure and whether a referent or index date occurred on a holiday (Memorial Day, Labor Day, Christmas Day, New Year’s Day, and Independence Day). Daily mean PM2.5 concentrations, temperature, humidity and barometric pressure were assigned to each study participant using ArcGIS. We assessed effect modification by stratifying on the following PELL data variables: season of clinical encounter, hospitalization frequency, insurance type, maternal education, previous bronchiolitis encounter, residential distance to major roadway, gestational age, birthweight, median income, breastfeeding status, cigarette use during pregnancy, maternal language preference and child’s gender. We present p-values for the interaction term added to the fully adjusted model between PM2.5 and each variable.
Results
Among the 33,387 asthma cases 0–9 years of age, the majority were male (63.2%), had a gestational age ≥ 37 weeks (86.4%), normal birthweight (89.9%) and were not previously admitted for a bronchiolitis encounter (71.7%). For most mothers of asthma cases, this was not their first child (58.9%), the majority were non-smokers during pregnancy (88.2%), white (59.3%), English-speaking (87.5%), lived within 150 m of a roadway (53.2%), had a household income between $20,000–$70,000 (55.5%), did not use government paid health insurance (55.7%), had more than a high school education (51.1%), had initiated breastfeeding at the hospital following the birth of their child (72.3), and did not report drinking during their pregnancy (98.3%) Relatively few participants had missing characteristic data (0.1%–0.5%). (Table 1).
Approximately 10% of our study sample had missing PM2.5 concentrations due to possible cloud or snow cover when the satellite based model was unable to provide estimates for a given day. For lag 0, the IQR for PM2.5 was 5.9 μg/m3. The mean PM2.5 concentration was 8.8 μg/m3 and the median concentration was 7.8 μg/m3. Similar distributions were observed for lags 1 and 2.
No statistically significant associations were found between PM2.5 exposures and asthma clinical encounters for lags 0, 1, and 2 regardless of whether only primary and secondary diagnosis fields were used (Table 2).
Effect modification was investigated for lags 0, 1 and 2 by stratifying to identify potentially susceptible subgroups (Table 3). Differences in odds ratios were observed when stratifying on birthweight. The association between PM2.5 exposure and having an asthma clinical encounter was significantly different among children with birthweight less than 2500 g (g) compared to those greater than or equal to 2500 g across all lags (p < 0.05), with the strongest association observed among low birthweight (LBW) children for lag 1 (OR: 1.08; 95% CI: 1.01, 1.15) compared to normal birthweight (OR: 0.99; 95% CI: 0.97, 1.01) per IQR increase in PM2.5.
Per IQR increase in PM2.5, non-significant increases in the odds of having an asthma clinical encounter were observed for preterm children for lag 1 (OR: 1.03; 95% CI: 0.97, 1.09) and lag 2 (OR: 1.02; 95% CI: 0.97, 1.08) compared to full-term children (lag 1 OR: 0.99; 95% CI: 0.97, 1.02; lag 2 OR: 0.98; 95% CI: 0.96, 1.00). The odds of an asthma clinical encounter were significantly higher (p < 0.05) among children who experienced a clinical encounter in the cold season (OR: 1.02; 95% CI: 0.99, 1.05) compared to the warm season (OR: 0.97, 95% CI: 0.94, 0.99) per IQR increase in PM2.5 for lag 0 with similar results for lag 1. Among children whose insurance type was not paid through the government a protective effect was observed for lag 2 (OR: 0.97; 95% CI: 0.94, 0.99) compared to those who had government paid insurance (OR: 1.00; 95% CI: 0.98, 1.04) per IQR increase in PM2.5. Similar results were observed for lags 0 and 1, although not significant (Table 3).
Results for the analysis of children 5–9 years of age are presented in Additional file 1: Tables S1-S3. Characteristics among the 6195 children and mothers in the 5–9 years of age group were consistent with those 0–9 years of age (Additional file 1: Table S1). Again, asthma clinical encounters were not associated with PM2.5 exposures for lags 0, 1, and 2 regardless of whether only primary and secondary diagnosis fields were used (Additional file 1: Table S2). We observed negative associations for lag 0 when stratifying on gestational age, maternal race, residential distance to roadway, median income, breastfeeding initiation at hospital, and child’s gender. Per IQR increase in PM2.5, preterm children (< 37 weeks) had significantly lower odds of having an asthma clinical encounter (OR: 0.81; 95% CI: 0.71, 0.92) compared to those were born full-term (> = 37 weeks) (OR: 0.98; 95% CI: 0.94, 1.03). Children who were born to mothers whose race was other than white had significantly decreased odds of having an asthma clinical encounter (OR: 0.91; 95% CI: 0.84, 0.98) per IQR increase in PM2.5 compared to those born to white mothers (OR: 0.99; 95% CI: 0.93, 1.05). Among children who lived within 150 m from a roadway we did not observe any association per IQR increase in PM2.5 (OR: 1.00; 95% CI: 0.94, 1.06), whereas a protective effect was observed among those who lived greater than 150 m from a roadway (OR: 0.92; 95% CI: 0.86, 0.98). Similar results were observed across lags 1 and 2, although not significant. Per IQR increase in PM2.5, those with an annual household median income between $20,000–$70,000 had decreased odds of an asthma clinical encounter (OR: 0.92; 95% CI: 0.86, 0.98) compared to those whose median income was greater than $70,000 (OR: 1.01; 95% CI: 0.94, 1.09) and those who were less than $20,000 (OR: 1.02; 95% CI: 0.87, 1.19). Odds of having a clinical encounter per IQR increase in PM2.5 were lower for female children (OR: 0.92; 95% CI: 0.85, 0.99) compared to male children (OR: 0.98; 95% CI: 0.93, 1.04). Lastly, children of mothers who initiated breastfeeding at the hospital following delivery were observed to have a protective effect against asthma clinical encounters per IQR increase in PM2.5 (OR: 0.93; 95% CI: 0.88, 0.98) compared to those who did not initiate breast feeding (OR: 1.03; 95% CI: 0.95, 1.12) (Additional file 1: Table S3).
Discussion
Several studies have suggested increased asthma exacerbation with short-term PM2.5 exposure [25] but little has been reported on the subgroups of children with asthmatic symptoms that may be most susceptible to the effects of PM2.5. Further, a broad range of PM2.5 concentrations in the various study locations have been reported [27]. In our study area, we report lower levels of PM2.5 with a median value of 7.8 μg/m3, however it has been suggested that asthma exacerbations may begin to increase at PM2.5 levels as low as 4.00–7.06 μg/m3 [38]. Our study identified sensitive subgroups that may be more vulnerable to low levels of PM2.5-induced asthma exacerbation resulting in a clinical encounter. LBW has been associated with a range of health effects in children including respiratory infections, lowered lung function and asthma [39,40,41]. LBW children have also displayed increased asthma symptoms related to air pollutants [42, 43]. When stratifying on birthweight, we saw increased odds of having an asthma clinical encounter across all lags, and statistically significant differences in the effect of PM2.5 on asthma clinical encounters for LBW children compared to normal birthweight. This demonstrates that birthweight may play a role in immune development and subsequent asthma development.
In addition to LBW, the effect of PM2.5 on asthma clinical encounters was significantly different in the cold season compared to the warm season (p < 0.05). Previous studies have identified the effects of air pollution in both warm and cool seasons to be associated with pediatric asthma attacks [21,22,23,24].
In this study we did not find smoking during pregnancy to be a significant effect modifier; however, we did observe increased odds ratios among women who smoked during pregnancy compared to those who did not across lags 1 and 2. Several studies have shown that maternal smoking during pregnancy is a modifiable risk factor for asthma [44]. The lack of effect modification by smoking in our analyses may be due to the relatively small number of women who reported smoking during pregnancy (n = 3922) and the under-reporting of smoking by pregnant women, causing misclassification of that variable.
Higher rates of asthma have been reported along major roadways [17] and exposure to traffic-related air pollutants have been associated with an increased risk of asthma hospitalizations [45, 46]. We found non-significant and inconsistent results within our data among children who lived within 150 m of roadways. In our analysis with children 5 and older, we found non-significant increases in odds ratios among children who lived within 150 m of a major roadway compared to those who lived greater than 150 m for lag 2 per IQR increase in PM2.5, and a statistically significant protective effect among those who lived greater than 150 m per IQR increase in PM2.5 for lag 0 (Additional file 1: Table S3). In our study, we specifically determined distance to major roadway from the household residence. However, studies have identified near roadway exposures at school may play a role in asthma outcomes as well [47].
Because asthma is best diagnosed at age 5 or older, we performed a secondary analysis restricting our cases those who had a clinical encounter at 5 years of age and older. We chose not to use these cases as our primary analysis because our case definition for asthma or wheeze included children who had the most severe symptoms leading them to seek care in the emergency department, and the majority of our cases were under the age of 5. Among those children who had a clinical encounter at age 5 or older, the association between PM2.5 exposure and having an asthma clinical encounter was significantly different among preterm children compared to the full-term children for lag 0 (p < 0.05). We observed significantly decreased odds of asthma clinical encounters among pre-term children (OR: 0.81; 95% CI: 0.71, 0.92) compared to full-term children (OR: 0.98; 95% CI: 0.94, 1.03) per IQR increase in PM2.5 (Additional file 1: Table S3). Preterm children may have other health issues that are typically treated more often in outpatient clinical settings, and therefore may have their asthma well-controlled and are seen less often in the emergency department. In addition, older children may have already been diagnosed with asthma in an outpatient clinical setting, or may have been seen in the emergency department for asthma or wheeze prior to age 5.
Our study tested several susceptible subgroups, and although we did not formally test for multiple comparisons, our significant findings exceeded the 5% type 1 error rate, or false positive rate, that we would have expected under the null hypothesis of no associations. Of the 42 tests between effect modifiers and PM2.5 exposure among children 0–9 years of age, there were 5 (11.9%) significant interactions found (Table 3). In the analysis with children 5–9 years of age, there was only 1 significant interaction found between PM2.5 and gestational age and therefore was within the 5% type 1 error rate and may have been an expected finding due to chance (Additional file 1: Table S3).
Our study design allowed our cases to serve as self-matched controls which provided several strengths. We did not need to control for modifiable asthma risk factors such as secondhand smoke. We were able to adjust for short-term meteorological changes that affect PM2.5 concentrations. Another major strength of this study was our ability to use satellite-based measurements to obtain estimates of PM2.5 at a 4-km resolution instead of relying on data from a relatively small number of fixed monitoring stations. Using short-term lags was reasonable since we would expect parents to seek medical attention for poorly controlled asthma or exacerbation of asthma or wheeze within the same day, or a day or two after symptoms begin. Another strength of this study was that the PELL data afforded both the large sample size and the record linkage necessary to exclude children who moved between their time of birth and clinical encounter. Exposure was assigned based on residential address so using the street-level birth address and matching that to the zip code at the time of their clinical encounter reduced exposure misclassification. Demographic characteristics among the subgroup that moved (including race, income, and maternal education) were consistent with the characteristics of those that did not move.
Although one advantage of using a case-crossover design is that there is no confounding by time invariant factors, one limitation is that the study design doesn’t allow for independent estimation of the effects for time invariant characteristics. Another limitation of this study was that our cases included only children who had more severe or poorly controlled asthma with severe enough symptoms to seek clinical care, and did not include children who are seen in outpatient clinical settings. Our study strictly focused on PM2.5 exposure, however there has been accumulating literature focusing on traffic-related air pollutants (TRAP) as a whole instead of the independent effects of individual air pollutants [48]. Although we used distance to major roadway measurements to account for traffic-related air pollutants, further investigation of other air pollution components may be warranted.
Conclusions
Our study identified susceptible subgroups of children that may have increased risk for asthma clinical encounters resulting from lower-level PM2.5 exposure. We found that LBW children had increased odds of an asthma or wheeze clinical encounter across all lags. Birthweight was a significant effect modifier at α = 0.05. We also found the season of clinical encounter to be a significant effect modifier for lags 0 and 1. This study suggests LBW children may be more susceptible to the effects of PM2.5. We did not find strong evidence of PM2.5 exposure and increased risk of asthma or wheeze clinical encounters among other subgroups.
Change history
06 March 2018
After publication of the article [1], it was brought to our attention that a number in Table 1 is incorrect.
Abbreviations
- CI:
-
Confidence interval
- g:
-
grams
- ICD-9:
-
International Classification of Diseases, Ninth Revision
- IQR:
-
interquartile range
- LBW:
-
Low birthweight
- MA:
-
Massachusetts
- OR:
-
Odds ratio
- PELL:
-
Pregnancy to Early Life Longitudinal
- PM2.5 :
-
Fine particulate matter less than 2.5 μm
References
Centers for Disease Control and Prevention. Asthma surveillance data. National Center for. Environ Health. 2016; http://www.cdc.gov/asthma/asthmadata.htm. Accessed 10 Nov 2016
National Institute of Health. Explore Asthma. National Heart, Lung, and Blood Institute. 2014. http://www.nhlbi.nih.gov/health/health-topics/topics/asthma. Accessed 12 Nov 2016.
Henderson J, Hilliard TN, Sherriff A, Stalker D, Al Shammari N, Thomas HM. Hospitalization for RSV bronchiolitis before 12 months of age and subsequent asthma, atopy and wheeze: a longitudinal birth cohort study. Pediatr Allergy Immunol. 2005;16(5):386–92.
James KM, Gebretsadik T, Escobar GJ, Wu P, Carroll KN, Li SX, Walsh EM, Mitchel EF, Sloan C, Hartert TV. Risk of childhood asthma following infant bronchiolitis during the respiratory syncytial virus season. J Allergy Clin Immunol. 2013;132(1):227–9.
Sigurs N, Aljassim F, Kjellman B, Robinson PD, Sigurbergsson F, Bjarnason R, Gustafsson PM. Asthma and allergy patterns over 18 years after severe RSV bronchiolitis in the first year of life. Thorax. 2010;65(12):1045–52.
Brunekreef B, Holgate ST. Air pollution and health. Lancet. 2002;360(9341):1233–42.
Etzel RA. How environmental exposures influence the development and exacerbation of asthma. Pediatrics. 2003;112:233–9.
Delamater PL, Finley AO, Banerjee S. An analysis of asthma hospitalizations, air pollution, and weather conditions in Los Angeles County, California. Sci Total Environ. 2012;425:110–8.
Iskandar A, Andersen ZJ, Bonnelykke K, Ellermann T, Andersen KK, Bisgaard H. Coarse and fine particles but not ultrafine particles in urban air trigger hospital admission for asthma in children. Thorax. 2012;67(3):252–7.
Mann JK, Balmes JR, Bruckner TA, Mortimer KM, Margolis HG, Pratt B, Hammond SK, Lurmann FW, Tager IB. Short-term effects of air pollution on wheeze in asthmatic children in Fresno, California. Environ Health Perspect. 2010;118(10):1497–502.
Meng YY, Rull RP, Wilhelm M, Lombardi C, Balmes J, Ritz B. Outdoor air pollution and uncontrolled asthma in the San Joaquin Valley, California. J Epidemiol Community Health. 2010;64(2):142–7.
Trasande L, Thurston GD. The role of air pollution in asthma and other pediatric morbidities. J Allergy Clin Immunol. 2005;115(4):689–99.
Boothe V, Shendell D. Potential health effects associated with residential proximity to freeways and primary roads: review of scientific literature 1999-2006. J Environ Health. 2008;70:44–1.
Brugge D, Durant JL, Rioux C. Near-highway pollutants in motor vehicle exhaust: a review of epidemiologic evidence of cardiac and pulmonary health risks. Environ Health. 2007;6:23.
Brauer M, Hoek G, Smit HA, de Jongste JC, Gerritsen J, Postma DS, Kerkhof M, Brunekreef B. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J. 2007;29(5):879–88.
Kim JJ, Huen K, Adams S, Smorodinsky S, Hoats A, Malig B, Lipsett M, Ostro B. Residential traffic and children's respiratory health. Environ Health Perspect. 2008;116(9):1274–9.
McConnell R, Berhane K, Yao L, Jerrett M, Lurmann F, Gilliland F, Künzli N, Gauderman J, Avol E, Thomas D, et al. Traffic, susceptibility, and childhood asthma. Environ Health Perspect. 2006;114(5):766–72.
Wjst M, Reitmeir P, Dold S, Wulff A, Nicolai T, Loeffelholz-Colberg Ev ME. Road traffic and adverse effects on respiratory health in children. BMJ. 1993;307(6904):596–600.
Delfino RJ, Wu J, Tjoa T, Gullesserian SK, Nickerson B, Gillen DL. Asthma morbidity and ambient air pollution: effect modification by residential traffic-related air pollution. Epidemiology. 2014;25(1):48–57.
Zhu Y, Hinds W, Kim S, Sioutas C. Concentration and size distribution of ultrafine particles near a major highway. J Air Waste Manag Assoc. 2002;52(9):1032–42.
Silverman RA, Ito K. Age-related association of fine particles and ozone with severe acute asthma in new York City. J Allergy Clin Immunol. 2010;125(2):367–73. e365
Strickland MJ, Darrow LA, Klein M, Flanders WD, Sarnat JA, Waller LA, Sarnat SE, Mulholland JA, Tolbert PE. Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. Am J Respir Crit Care Med. 2010;182(3):307–16.
Tsai SS, Cheng MH, Chiu HF, Wu TN, Yang CY. Air pollution and hospital admissions for asthma in a tropical city: Kaohsiung, Taiwan. Inhal Toxicol. 2006;18(8):549–54.
Yang CY, Chen CC, Chen CY, Kuo HW. Air pollution and hospital admissions for asthma in a subtropical city: Taipei, Taiwan. J Toxicol Environ Health A. 2007;70(2):111–7.
Fan J, Li S, Fan C, Bai Z, Yang K. The impact of PM2.5 on asthma emergency department visits: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2015;23(1):843–50.
World Health Organization. Systematic Review of Air Pollution in Europe. Copenhagen; 2004.
EPA US. Integrated science assessment for particulate matter. Research Triangle Park: US EPA; 2009.
Anderson HR, Favarato G, Atkinson RW. Long-term exposure to outdoor air pollution and the prevalence of asthma: meta-analysis of multi-community prevalence studies. Air Qual Atmos Health. 2013;6:57–68.
Molter A, Simpson A, Berdel D, Brunekreef B, Custovic A, Cyrys J, de Jongste J, de Vocht F, Fuertes E, Gehring U, et al. A multicentre study of air pollution exposure and childhood asthma prevalence: the ESCAPE project. Eur Respir J. 2015;45(3):610–24.
Kloog I, Koutrakis P, Coull BA, Lee HJ, Schwartz J. Assessing temporally and spatially resolved PM2.5 exposures for epidemiological studies using satellite aerosol optical depth measurements. Atmos Environ. 2011;45(35):6267–75.
Lee HJ, Liu Y, Coull BA, Schwartz J, Koutrakis P. A novel calibration approach of MODIS AOD data to predict PM2.5 concentrations. Atmos Chem Phys. 2011;11(15):7991–8002.
Hu X, Waller LA, Al-Hamdan MZ, Crosson WL, Estes MG Jr, Estes SM, Quattrochi DA, Sarnat JA, Liu Y. Estimating ground-level PM2.5 concentrations in the southeastern U.S. using geographically weighted regression. Environ Res. 2013;121:1–10.
Hu X, Waller LA, Lyapustin A, Wang Y, Al-Hamdan MZ, Crosson WL, Estes MG, Estes SM, Quattrochi DA, Puttaswamy SJ, et al. Estimating ground-level PM2.5 concentrations in the southeastern United States using MAIAC AOD retrievals and a two-stage model. Remote Sens Environ. 2014;140:220–32.
Kloog I, Nordio F, Coull BA, Schwartz J. Incorporating local land use regression and satellite aerosol optical depth in a hybrid model of spatiotemporal PM2.5 exposures in the mid-Atlantic states. Environ Sci Technol. 2012;46:11913–21.
Levy D, Lumley T, Sheppard L, Kaufman J, Checkoway H. Referent selection in case-crossover analyses of acute health effects of air pollution. Epidemiology. 2001;12:186–92.
Navidi W, Weinhandl E. Risk set sampling for case-crossover designs. Epidemiology. 2002;13:100–5.
Janes H, Sheppard L, Lumley T. Overlap bias in the case-crossover design, with application to air pollution exposures. Stat Med. 2005;24:285–300.
Mirabelli MC, Vaidyanathan A, Flanders WD, Qin X, Garbe P. Outdoor PM2.5, ambient air temperature, and asthma symptoms in the past 14 days among adults with active asthma. Environ Health Perspect. 2016;124(12):1882–90.
Barker DJP, Godfrey KM, Fall C, Osmond C, Winter PD, Shaheen S. Relation of birth weight and childhood respiratory infection to adult lung function and death from chronic obstructive airways disease. BMJ. 1991;303:5.
Steffensen FH, Sørensen HT, Gillman MW, Rothman KJ, Sabroe S, Fischer P, Olsen J. Low birth weight and preterm delivery as risk factors for asthma and atopic dermatitis in young adult males. Epidemiology. 2000;11(2):4.
Pei L, Chen G, Mi J, Zhang T, Song X, Chen J, Ji Y, Li C, Zheng X. Low birth weight and lung function in adulthood: retrospective cohort study in China, 1948-1996. Pediatrics. 2010;125(4):e899–905.
Mortimer KM, Tager IB, Dockery DW, Neas LM, Redline S. The effect of ozone on Inner-City children with asthma. Am J Respir Crit Care Med. 2000;162:1838–45.
Sbihi H, Tamburic L, Koehoorn M, Brauer M. Perinatal air pollution exposure and development of asthma from birth to age 10 years. Eur Respir J. 2016;47:1062–71.
Burke H, Leonardi-Bee J, Hashim A, Pine-Abata H, Chen Y, Cook DG, Britton JR, McKeever TM. Prenatal and passive smoke exposure and incidence of asthma and wheeze: systematic review and meta-analysis. Pediatrics. 2012;129(4):735–44.
Chang J, Delfino RJ, Gillen D, Tjoa T, Nickerson B, Cooper D. Repeated respiratory hospital encounters among children with asthma and residential proximity to traffic. Occup Environ Med. 2009;66(2):90–8.
Delfino RJ, Chang J, Wu J, Ren C, Tjoa T, Nickerson B, Cooper D, Gillen D. Repeated hospital encounters for asthma in children and exposure to traffic-related air pollution near the home. Annals of Allergy Asthma and Immunology. 2009;102:138–44.
McConnell R, Islam T, Shankardass K, Jerrett M, Lurmann F, Gilliland F, Gauderman J, Avol E, Kunzli N, Yao L, et al. Childhood incident asthma and traffic-related air pollution at home and school. Environ Health Perspect. 2010;118(7):1021–6.
Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383(9928):1581–92.
Acknowledgements
Health data was provided by the Massachusetts Department of Public Health and should not be considered an endorsement of this study or its conclusions.
Funding
This work was supported by grant number R01ES019897 from the National Institute of Environmental Health Sciences (NIEHS). Its contents are solely the responsibility of the authors and do not necessarily represent the views of NIH. YL and XH were partially supported by NASA Applied Sciences Program (grant no. NNX11AI53G).
Availability of data and materials
The health data obtained from the PELL data system are not publicly available due to patient confidentiality reasons but may be requested from the Massachusetts Department of Public Health.
Author information
Authors and Affiliations
Contributions
RK performed the analyses and drafted the initial manuscript with contribution from all authors. VMV, SMB, HC, CB, and MJS provided technical input to the analysis and manuscript preparation. XH and YL developed the exposure model. VMV conceived the study and its design. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board (IRB) (Reference number: UCI IRB HS# 2012–8784).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional information
A correction to this article is available online at https://doi.org/10.1186/s12940-018-0371-4.
Additional file
Additional file 1:
Table S1. Selected demographic characteristics among children 5–9 years of age with asthma clinical encounters. Table S2. Odds ratios for a 5 μg/m3 increase in PM2.5 and asthma clinical encounters. Table S3. Odds ratios for a 5 μg/m3 increase in PM2.5 and asthma clinical encounters with stratified analysis. (DOCX 43 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Khalili, R., Bartell, S.M., Hu, X. et al. Early-life exposure to PM2.5 and risk of acute asthma clinical encounters among children in Massachusetts: a case-crossover analysis. Environ Health 17, 20 (2018). https://doi.org/10.1186/s12940-018-0361-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-018-0361-6