Abstract
Introduction
Social-economic factors have an important role in shaping inequality in congenital heart diseases. The current study aimed to assess and decompose the socio-economic inequality in Congenital Heart Diseases (CHDs) in Iran.
Methods
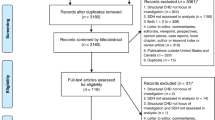
This is a cross-sectional research conducted at Shahid Rajaie Cardiovascular Medical and Research Center in Tehran, Iran, as one of the largest referral heart hospitals in Asia. Data were collected primarily from 600 mothers who attended in pediatric cardiology department in 2020. The polychoric principal component analysis (PCA) and Errygers corrected CI (ECI) were used to construct household socioeconomic status and to assess inequality in CHDs, respectively. A regression-based decomposition analysis was also applied to explain socioeconomic-related inequalities. To select the explanatory social, medical/biological, and lifestyle variables, the chi-square test was first used.
Results
There was a significant pro-rich inequality in CHDs (ECI = -0.65, 95% CI, − 0.72 to − 0.58). The social, medical/biological, and lifestyle variables accounted for 51.47, 43.25, and 3.92% of inequality in CHDs, respectively. Among the social variables, family SES (about 50%) and mother’s occupation (21.05%) contributed the most to CHDs’ inequality. Besides, in the medical/biological group, receiving pregnancy care (22.06%) and using acid folic (15.70%) had the highest contribution.
Conclusion
We concluded that Iran suffers from substantial socioeconomic inequality in CHDs that can be predominantly explained by social and medical/biological variables. It seems that distributional policies aim to reduce income inequality while increasing access of prenatal care and folic acid for disadvantaged mothers could address this inequality much more strongly in Iran.
Similar content being viewed by others
Background
Congenital Heart Diseases (CHDs) are structural or functional anomalies that occur during pregnancy. These disorders, also known as birth defects, congenital abnormalities, or congenital malformations, develop during pregnancy and can be discovered before, during, or after birth, as well as later in life. CHDs affect approximately 0.8 to 1.2% of live births [1, 2] with a global incidence rate of 17.9/1000 [3].
CHDs occur during fetal development and affect the infant from birth; they are among the most common birth defects, leading to childhood and infancy mortality [4]. The estimated prevalence of CHDs ranges from 4 to 50 per 1000 live births, and the difference in prevalence is primarily due to the age of diagnosis, the concept of CHDs, and the screening methods used [5].
Socioeconomic inequalities that disproportionately impact people of lower socioeconomic status (SES) over those of higher SES, have long been a cause of concern in cardiovascular health [6]. According to a cohort study from Eastern Europe in Russia, Poland and the Czech Republic, low socioeconomic status (SES) is a strong predictor of the high prevalence, morbidity, and mortality associated with cardiovascular diseases (CVD) and its main risk factors [7].
Health inequalities are more likely to be affected by socioeconomic factors than by medical and healthcare differences [8]. A minority of CHDs may be related to heritable or unintended genetic causes such as chromosomal abnormalities or pathogenic copy number variants (about 20%) [9]. Therefore, the vast majority of CHD incidents are believed to be caused by multifactorial causes, including various genetic, social and environmental factors [10, 11]. It has recently been shown that social determinants of health contribute to diseases and health outcomes and can lead to an increase in congenital anomalies [12, 13], including the formation of congenital heart disease [14]. In general, CHDs are related to serious difficulties such as cognitive impairment [15] and often affect parents and individuals disproportionately [16] in terms of mental health [17], quality of life and economic aspects [18].
It has been shown that different environmental and socioeconomic risk factors, as well as inequalities in social determinants of health, may play a significant role in the distribution and regional variations in the prevalence of CHDs. Few studies have looked at the importance of socioeconomic variables such as parental education/occupation and income as key outcome predictors in non-communicable diseases, which are considered to have a substantial effect on health and health inequalities [7], especially in the field of congenital heart disease [19]. In this regard, a study conducted in children born in Ontario, Canada (with access to public care) found that children born in families and neighborhoods with lower incomes and social status had significantly higher rates of congenital heart defects [20]. Thus, it has been shown that socioeconomic factors may be responsible for inequalities in the live-birth of children with CHDs [21]. Given that the prevalence of congenital heart diseases in Iran is between 9.7 and 17.5 per 1000 live births [22, 23], it remains uncertain if such socioeconomic factors among various groups are at proportionately higher risk of getting a child with congenital heart disease, especially in the Iranian context.
Furthermore, According to international organizations such as the World Bank [24] and UNICEF [25], inequalities in the distribution of external inputs such as education, income, wealth, and place of residence, which are beyond the control of children, contribute to inequality inopportunity for disadvantaged children [26, 27]. This form of socio-economic inequality is a major problem in developing countries, like Iran, where unfair socio-economic inequalities in early childhood lead to inequality in the health outcomes later in life [28, 29]. In other words, according to research, the prevalence of inequalities in access to health care to prevent physical and mental illnesses is dependent on the socio-economic situation of households [30, 31], and this type of unjust inequality would have negative consequences for the health and well-being of the children in these families. As a result, the central questions of this research are whether, in the area of congenital heart disease, the presence of socioeconomic inequality, which is a type of unfair inequality in parents’ health opportunities, would affect the prevalence of congenital heart disease in children, and what proportion of these inequalities in the birth of a child with congenital heart disease can be due to various socio-economic factors of the parents?
Methods
Setting
This is a cross-sectional study conducted at Shahid Rajaie Cardiovascular Medical and Research Center in Tehran, Iran, during March 2020 to September 2020. The hospital is one of the largest referral heart hospitals in Asia founded in 1976. It currently has over 600 active beds, and 1000 patients are admitted daily from various parts of Iran. This well-known, specialized and referral hospital welcomes a wide variety of clientele from different socioeconomic groups across Iran’s provinces One of the most important clinical services provided by this hospital is pediatric cardiac care. The pediatric cardiology department is a pioneer in educational, treatment, and research services, as well as the country’s most well-known clinic for heart diseases in children and adolescents. The department has provided 138 patient beds. This center is the largest and best-equipped hospital in the Middle East for treating the children with heart diseases. About 1400 congenital heart surgeries are performed in the pediatric cardiology department each year [32].
Data collection
The data were collected primarily from the mothers who attended the pediatric cardiology department during April 2020 to June 2020. The mothers were chosen through convenience random sampling. They were asked to complete a research administrated check list including three types of variables: social, medical/biological, and lifestyle. The social and life style variables were selected based on the WHO framework of social determinants of health presented by Solar and Irwin [33]. The medical/biological variables were selected according to the previous studies, as well [10, 11, 34].
Definition of variables
In this study, congenital heart diseases (CHDs) was chosen as a dichotomous outcome variable (mothers have had a child with CHDs or not).
Household socio-economic status, mother’s and father’s education levels, mother’s and father’s occupations, nationality, place of residence, number of children, and history of family marriage were all explanatory social variables. Explanatory medical/biological variables included mother’s age at delivery time, father’s age (as biological variables), parity number, receiving pregnancy care, mother’s history of abortion, chronic disease, and using folic acid (as medical variables). In addition, life style variables were as follows: doing physical activity, using alcohol, and smoking.
In the absence of direct data on income and expenditures, a common and widely used method for assessing the socioeconomic status of a household is to use an asset index (as a proxy of socio-economic status) from data on household ownership of durable assets and characteristics of the house [35]. The polychoric principal component analysis (PCA) was used to construct household socioeconomic status [36]. One of the assumptions underlying the classic PCA is that the input variables are normal. As our data included in household socio-economic status were discrete (including binary and ordinal variables), this assumption was clearly violated. As a result, polychoric PCA was used. The following variables were used in polychoric PCA model: mother’s education level, father’s education level, father’s occupation, house ownership, owning a personal computer, and having a kitchen, a bathroom, a vacuum cleaner, a washing machine, and a freezer. Accordingly, five socioeconomic quintiles including the poorest, poorer, middle, richer, and the richest were made and applied in the subsequent analyses. Mother’s age at delivery was also classified into four age categories [37] (≤17, 18–28, 29–39, and ≥ 40 years old).
Inequality measurement and decomposition
Socioeconomic inequality in CHDs was measured using the Concentration Index (CI) [38]. The CI proposed by Wagstaff et al. (2003) has been widely applied to assess socio-economic inequality in health outcomes. Furthermore, the decomposition potential of CI has led to its widespread adoption as a reliable measure of health inequality rather than other measures of inequality [39].
The CI is defined using a Concentration Curve (CC) (1). The CC plots the cumulative percentage of the health outcome (Y axis) against the cumulative percentage of individuals, ranked by their socioeconomic status from the poorest to the richest (X axis). If everyone, irrespective of his/her socioeconomic status, has exactly the same value as the health outcome, the CC will form a 45-degree line called equality line. But if the health outcome takes lower (or higher) values than the individuals with lower socioeconomic status, the CC will lie below (or over) the equality line. The CI is measured as twice the covariance of a health outcome and fractional rank of socioeconomic status divided by the mean health outcome, as follows:
Where Yi is the health outcome (CHDs) of the i th child, \(\overline{Y}\) denotes CHDs mean, and Ri indicates the fractional rank of the i th child in terms of the index of their household’s socioeconomic status. The negative and positive values of CI indicate that CHDs’ inequality is unevenly concentrated in the worse-off and better-off children, respectively. Given that CHDs was considered as a binary variable in the current study, Errygers corrected CI (ECI) was applied to assess CHDs’ inequality more precisely [40].
In which Ymax and Ymin are the maximum and minimum of CHDs, respectively, and CI is obtained from eq. 1.
To decompose, the chi-square test was first used to select the explanatory variables to be included in the decomposition model. In other words, we conducted the chi-square test on CHDs and each social, medical/biological, and life style variables, and then the significant values were entered in the decomposition model. Then, to examine the contribution of each social, medical/biological, and life style variables to CHDs’ inequality, a regression-based decomposition analysis was used as well. The CHDs were first explained using a Generalized Linear Model (GLM) (eq. 3) and then decomposed using eq. 4 as follows:
Where \({\mathrm{x}}_{{\mathrm{k}}_{\mathrm{i}}}\) is the set of k determinants (in binary form) of CHDs βk indicates the coefficient obtained through GLM, εi is an error term, and GCε is the generalized CI for εi. Equation (4) comprised of explained (or deterministic) and unexplained (or probabilistic) components. The absolute contribution of an explanatory social, medical/biological, and life style variable could be taken by estimating the explained component. The analysis was conducted using STATA/SE (version 14; Stata Corporation, College Station, TX, USA).
Results
In this study, 600 mothers completed the survey, of whom 200 (33.33%) had a child suffering from CHDs. As shown in Table 1, most of the mothers were in the middle SES group, had a middle school education level, were 29–39 years of age, were housewives, Iranian, resided in urban areas, got pregnancy care, and used acid folic. Fortunately, most of the mothers did not have family marriage, a history of abortion, alcohol use and smoking. The results showed that 43.83 and 43.50% of the studied mothers had two pregnancies and had two children, respectively. Regarding fathers, the data indicated that most of them had higher education levels, were aged 36–40, and worked in non-clerical jobs. CHDs were more prevalent among the families with the poorest SES, illiterate mothers, mothers aged 18–28 years at delivery who had chronic diseases, fathers with high school education levels, fathers with non-clerical jobs, and fathers of 31–35 years of age.
The ECI of CHDs was −0.65 (95% CI, − 0.72 to − 0.58), implying that CHDs were more concentrated among the families with low SES levels, and it was not equally distributed among the people with different SES levels.
Figure 1 shows the concentration curve of CHDs. As it depicts, the concentration curve of CHDs lays above the equality line. This implies that CHDs were more concentrated among relatively lower SES families.
The decomposition results of SES inequality in CHDs are presented in Table 2. The ECIs of the explanatory variables revealed that mothers’ and fathers’ low educational attainment, being a housewife, father’s non-clerical job, having a history of family marriage, younger maternal age (< 28 years) and fathers’ age (< 25 years), having a history of abortion and chronic disease, using alcohol, and smoking were more concentrated among families with lower SES. In contrast, mothers’ and fathers’ clerical jobs, living in urban areas, mother’s age of 29–39 at delivery time, using prenatal care and acid folic as well as doing enough physical activity were all more concentrated among higher SES families. As Table 2 shows, the observed component including social, medical/biological, and life style variables accounted for 51.47, 43.25, and 3.92% of inequality in CHDs, respectively. The observed component indicated that the determinants included in the current model were able to explain 98.64% of the measured inequality in CHDs. The rest of the inequality (1.36%) was due to the residual (unexplained) component. The main contributors to inequality in CHDs regarding social variables were devoted to family SES (about 50%), mother’s occupation (21.05%), and mother’s education (3.62%). Besides, in the medical/biological group, receiving pregnancy care (22.06%), using acid folic (15.70%), and a history of abortion (5.38%) were the most contributors to inequality in CHDs. In addition, regarding the life style variables, using alcohol and smoking accounted for 2.67 and 1.87% of inequality in CHDs, respectively. About the contributing variables, if the value of the contributor X was x and positive (or negative), the inequality in CHDs would decrease (or increase) by x% if the contributor was to become equally distributed among different socioeconomic groups. The largest contribution to inequality in CHDs was attributed to family SES (about 50%), i.e. if income and wealth were equally distributed in the society, the inequality in CHDs would decrease by 50%. Also, if employment opportunities and access to pregnancy care were equally distributed among different mothers, the inequality in CHDs would decrease by 21 and 22%, respectively.
Discussion
Previous studies have shown that disadvantaged groups have a higher rate of CHDs' morbidity and mortality [19]. The current research was carried out in order to provide some evidence regarding social inequalities in CHDs and the factors that played crucial roles in shaping such unwanted inequality. To the knowledge of the researchers, the present study is the first research that measured such inequality through concentration index and explained it via regression-based decomposition analysis in the globe. We found substantial socioeconomic inequality in CHDs which was in favor of the better-offs. Although there were no related studies, other studies showed that other negative outcomes such as preterm birth and still birth [41] were concentrated among the disadvantaged groups. Unfortunately, it seems that socioeconomic inequality in mortality due to CHDs increased across the world over time [42]. As children have no choices about their health status, our findings implicitly indicated huge inequality of opportunities for CHDs’ patients within the health system of Iran and probably other low- and middle-income countries. Furthermore, it seems that survived children with congenital anomalies such as heart disease will have less opportunities to improve their health resources [43].
The explanation of socioeconomic inequalities has an intrinsic value and could assist policy makers to address these inequalities much effectively [44]. The decomposition analysis revealed that socioeconomic factors solely explained about 51% of the observed inequality in CHDs. A study conducted through mediation analysis in the US also found that socioeconomic factors such as education and health insurance accounted for a significant portion of racial and ethnic disparities in CHDs [45]. Surprisingly, income status contributed somewhat further to socioeconomic inequality in our analysis and could be considered as a key contributor. Previous research [21, 46, 47], found that lower socioeconomic status was substantially correlated to the risk of CHDs, which is consistent with our findings, but those studies failed to trace the impact of this predictor on socioeconomic inequality in CHDs. However, other studies showed that economic status was the main contributor to socioeconomic inequality in infants and children mortality [48, 49]. Furthermore there is some evidence that shows income inequality has negative effects on cardiovascular disease in the US [50] and globally on heart failure [51]. Parents with higher incomes are able to make more investments in their health capital through purchasing medical care services, nutritious food, and other health-related products, as well as providing safer environments. Hence, children of these parents are likely to be healthier comparing to those of lower-income parents [52]. Alongside socio-economic status, the effect of parental characteristics on CHDs’ inequality was also studied. We observed that although mother’s occupation positively contributed to CHDs’ inequality, father’s occupation was negatively contributed to this outcome. Housewives accounted for the greatest share of CHDs’ inequality within mother’s occupation category (16.52%).It seems that housewife mothers do not have enough affordability to experience safe pregnancy and this could increase CHDs among their children [53].
Although, clerical and non-clerical employed father approximately neutralized each other effects on CHDs’ inequality, but given to the positive contribution of father’s non-clerical occupation in CHDs’ inequality, it seems that non-clerical occupation groups suffer from insufficient income, job insecurity, lack of medical insurance and access to healthcare [54]. Besides, Occupation status could also associate with CHDs through occupational exposure to chemicals [55] and this could be increased among parents with non-clerical jobs which seemed to be more prevalent among disadvantaged households. So, it could be said that more attention should be paid to the households that their fathers have non-clerical jobs.
In the current study, the father’s age had only a small contribution to CHDs’ inequality but, it might work as a social factor from the point of view of occupation, income (e.g. mean to pay) and/or knowledge and experiences.
The decomposition analysis in this study was not limited to socioeconomic factors; the effects of other variables such as medical/biological and lifestyle variables were also investigated. Second to socioeconomic variables, medical/biological variables played a crucial role in shaping socioeconomic inequality in CHDs through their positive contribution to inequality. Among the variables of this category, using pregnancy care and folic acid collectively explained 38% of the observed inequality. There are well-established evidence about the protecting effect of pregnancy care such as prenatal screening and the use of folic acid against CHDs [56, 57]. It is believed that the misuse of pregnancy services and supplements by disadvantaged mothers could be an important justification of the association between lower socioeconomic status and the risk of CHDs [58]. These factors in our analysis had negative concentration index indicating that disadvantaged households had undesirable access to pregnancy care and folic acid. Iran has been subject to international sanctions over the years, which are believed to have negatively affected food security and access to the required healthcare services [59]. Hence it seems that Iranian healthcare authorities could be able to address remarkable of CHDs inequality through facilitating the access of disadvantaged mothers to the pregnancy care and folic acid this could be done through providing subsidized prenatal care and including accessing to the folic acid in national food fortification strategy. Life style factors also had positive contribution on the CHDs’ inequality in our research that was in line with former studies [54]. We observed that the dangerous life style behaviors such as using alcohol and smoking were concentrated among the poor. Hence, health promotion interventions among disadvantaged groups could decrease the CHDs’ inequality to some extent. The children with CHDs have higher hospitalization rates with expensive healthcare services [56]. According to our findings, the disadvantaged households that have children with CHDs were in a higher risk of experiencing financial hardship [60]. As a result, it is strongly recommended that healthcare authorities place these households at the core of their policy-making.
Strengths and limitations
Although our study was the first research that simultaneously measured and explained socioeconomic inequality in the area of CHDs through gathering primary data, several limitations need to be acknowledged. First, the results of the present research are based on cross-sectional data and hence, could not bring strong causality between the studied variables and CHDs’ inequality. Second, despite the fact that this analysis examined the CHDs’ inequality using a broad variety of variables, the majority of those variables were social in nature; however, there are some others that we did not address in this report, including parental occupational exposure to chemicals or clinical variables. Third, there are concerns about sample bias with this study, as this study conducted at Shahid Rajaie Cardiovascular Medical and Research Center. It is possible that a number of families and mothers whose children might have CHDs but for various reasons did not have access to diagnosis/care. Accordingly, neglected patients might suffer and/or lose their lives and could not be included in this study.
Conclusion
This research tried to firstly investigate determinants of socioeconomic inequality in CHDs. We showed that Iran suffers from remarkable pro-rich inequality in CHDs. Considering that social variables including socioeconomic status and mother’s occupation are the main contributor to the CHDs’ inequality, policy makers must pay special attention to these social conditions in which children are born and grow. They can try to provide equal opportunities to decrease the occurrence of CHDs, its inequality, and other related unjustified outcomes. The first policy entry point to tackle CHDs’ inequality is to promote an equitable distribution of income across various SES groups. Second, it is recommended to develop a comprehensive social program and provide special health services for housewife mothers. Third, in terms of medical contributors to the CHDs’ inequality, it seems that providing subsidized prenatal care and national food fortification strategy can address the CHDs’ inequality among disadvantaged households and the burden in the health system in general. Moreover, it seems that addressing the social and medical factors contributing to the CHDs’ inequality, simultaneously, can further improve the equality in the CHDs’ status quo.
Availability of data and materials
Data are available on reasonable request. The data that support the findings of this study are available from the corresponding author.
Change history
16 March 2022
After publication of the original article, it was noted that in the affiliation of the second author, ‘Jundishapur’ was incorrectly written as ‘Jundishapour’. This has been corrected.
References
Bouma BJ, Mulder BJ. Changing landscape of congenital heart disease. Circ Res. 2017;120(6):908–22.
Van Der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58:2241–7.
Wu W, He J, Shao X. Incidence and mortality trend of congenital heart disease at the global, regional, and national level, 1990-2017. Medicine (Baltimore). 2020;99:e20593
Zimmerman MS, Smith AGC, Sable CA, Echko MM, Wilner LB, Olsen HE, et al. Global, regional, and national burden of congenital heart disease, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Child Adolescent Health. 2020;4:185–200.
Zhao Q-M, Liu F, Wu L, Ma X-J, Niu C, Huang G-Y. Prevalence of congenital heart disease at live birth in China. J Pediatr. 2019;204:53–8.
Downing NS, Wang C, Gupta A, Wang Y, Nuti SV, Ross JS, et al. Association of racial and socioeconomic disparities with outcomes among patients hospitalized with acute myocardial infarction, heart failure, and pneumonia: an analysis of within-and between-hospital variation. JAMA Netw Open. 2018;1:e182044.
Tillmann T, Pikhart H, Peasey A, Kubinova R, Pajak A, Tamosiunas A, et al. Psychosocial and socioeconomic determinants of cardiovascular mortality in Eastern Europe: a multicentre prospective cohort study. PLoS Med. 2017;14:e1002459.
Mazeikaite G, O’Donoghue C, Sologon DM. What drives cross-country health inequality in the EU? Unpacking the role of socio-economic factors. Soc Indic Res. 2021;155(1):117–55.
Blue GM, Kirk EP, Giannoulatou E, Sholler GF, Dunwoodie SL, Harvey RP, et al. Advances in the genetics of congenital heart disease: a clinician’s guide. J Am Coll Cardiol. 2017;69:859–70.
Lopes SAVA, Guimarães ICB, Costa SFO, Acosta AX, Sandes KA, Mendes CMC. Mortality for critical congenital heart diseases and associated risk factors in newborns. A cohort study. Arq Bras Cardiol. 2018;111:666–73.
Suluba E, Shuwei L, Xia Q, Mwanga A. Congenital heart diseases: genetics, non-inherited risk factors, and signaling pathways. Egypt J Med Hum Genetics. 2020;21:1–12.
Knowles RL, Ridout D, Crowe S, Bull C, Wray J, Tregay J, et al. Ethnic and socioeconomic variation in incidence of congenital heart defects. Arch Dis Child. 2017;102:496–502.
Bronberg R, Groisman B, Bidondo MP, Barbero P, Liascovich R. Birth prevalence of congenital anomalies in the City of Buenos Aires, Argentina, according to socioeconomic level. J Commun Genetics. 2020;11:303–11.
Wong P, Denburg A, Dave M, Levin L, Morinis JO, Suleman S, et al. Early life environment and social determinants of cardiac health in children with congenital heart disease. Paediatr Child Health. 2018;23:92–5.
Sanz JH, Berl MM, Armour AC, Wang J, Cheng YI, Donofrio MT. Prevalence and pattern of executive dysfunction in school age children with congenital heart disease. Congenit Heart Dis. 2017;12:202–9.
Lisanti AJ. Parental stress and resilience in CHD: a new frontier for health disparities research. Cardiol Young. 2018;28:1142–150.
Woolf-King SE, Anger A, Arnold EA, Weiss SJ, Teitel D. Mental Health Among Parents of Children With Critical Congenital Heart Defects: A Systematic Review. J Am Heart Assoc. 2017;6
Gregory MRB, Prouhet PM, Russell CL, Pfannenstiel BR. Quality of Life for Parents of Children With Congenital Heart Defect: A Systematic Review. J Cardiovasc Nurs. 2018;33:363–71.
Best KE, Vieira R, Glinianaia SV, Rankin J. Socio-economic inequalities in mortality in children with congenital heart disease: a systematic review and meta-analysis. Paediatr Perinat Epidemiol. 2019;33:291–309.
Agha MM, Glazier RH, Moineddin R, Moore AM, Guttmann A. Socioeconomic status and prevalence of congenital heart defects: does universal access to health care system eliminate the gap? Birth Defects Research Part A: Clinical and Molecular Teratology. 2011;91:1011–8.
Peyvandi S, Baer RJ, Chambers CD, Norton ME, Rajagopal S, Ryckman KK, et al. Environmental and socioeconomic factors influence the live-born incidence of congenital heart disease: a population-based study in California. J Am Heart Assoc. 2020;9:e015255.
Nazari P, Davoodi M, Faramarzi M, Bahadoram M, Dorestan N. Prevalence of congenital heart disease: a single center experience in southwestern of Iran. Global J Health Sci. 2016;8:56421.
Kafian Atary S, Mirshahi A, Amouzeshi A, Ramazani AA, Soleimani Khomartash Z, Bahman B, et al. Epidemiologic study of congenital heart diseases and its related factors in children referred to the pediatric cardiac Clinic of Birjand University of medical sciences, Iran. Int J Pediatr. 2019;7:10455–63.
Pons-Duran C, Lucas A, Narayan A, Dabalen A, Menéndez C. Inequalities in sub-Saharan African women's and girls' health opportunities and outcomes: evidence from the Demographic and Health Surveys. J Glob Health. 2019;9(1):010410.
Lu C, Cuartas J, Fink G, McCoy D, Liu K, Li Z, Daelmans B, Richter L. Inequalities in early childhood care and development in low/middle-income countries: 2010–2018. 2020;5:e002314.
Elgar FJ, Gariépy G, Torsheim T, Currie C. Early-life income inequality and adolescent health and well-being. Soc Sci Med. 2017;174:197–208.
Hosseinkhani Z, Nedjat S, Aflatouni A, Mahram M, Majdzadeh R. Socioeconomic inequality and child maltreatment in Iranian schoolchildren. East Mediterr Health J. 2016;21:819–27.
Bricard D, Jusot F, Trannoy A, Tubeuf S. Inequality of opportunities in health and death: an investigation from birth to middle age in Great Britain. Int J Epidemiol. 2020;49:1739–48.
Galama TJ, Van Kippersluis H. A theory of socio-economic disparities in health over the life cycle. Econ J. 2019;129:338–74.
Saidi A, Hamdaoui M. On measuring and decomposing inequality of opportunity in access to health services among Tunisian children: a new approach for public policy. Health Qual Life Outcomes. 2017;15:1–29.
Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob Health. 2017;5:e277–89.
Rajaie Cardiovascular Medical and Research Center. Tehran: Iran University of Medical Sciences; 2021. Available from: http://rhc.ac.ir. [cited 2021 June 30]
Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Social determinants of health discussion paper 2 (policy and practice), 2010. Geneva: World Health Organization; 2018.
Naghavi-Behzad M, Alizadeh M, Azami S, Foroughifar S, Ghasempour-Dabbaghi K, Karzad N, et al. Risk factors of congenital heart diseases: a case-control study inNorthwest Iran. J Cardiovasc Thoracic Res. 2013;5:5.
Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan 2006;21:459–68.
Kolenikov S, Angeles G. Socioeconomic status measurement with discrete proxy variables: is principal component analysis a reliable answer? Rev Income Wealth. 2009;55:128–65.
Londero AP, Rossetti E, Pittini C, Cagnacci A, Driul L. Maternal age and the risk of adverse pregnancy outcomes: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19:1–10.
O’donnell O, Van Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data: a guide to techniques and their implementation: The World Bank; 2007.
Wagstaff A, Van Doorslaer E, Watanabe N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. J Econom. 2003;112:207–23.
Erreygers G. Correcting the concentration index. J Health Econ. 2009;28:504–15.
Almasi-Hashiani A, Sepidarkish M, Safiri S, Morasae EK, Shadi Y, Omani-Samani R. Understanding determinants of unequal distribution of stillbirth in Tehran, Iran: a concentration index decomposition approach. BMJ Open. 2017;7:e013644.
Cha S, Jin Y. Have inequalities in all-cause and cause-specific child mortality between countries declined across the world? Int J Equity Health. 2020;19:1–13.
Currie J. Healthy, wealthy, and wise: socioeconomic status, poor health in childhood, and human capital development. J Econ Lit. 2009;47:87–122.
Vahedi S, Yazdi-Feyzabadi V, Amini-Rarani M, Mohammadbeigi A, Khosravi A, Rezapour A. Tracking socio-economic inequalities in healthcare utilization in Iran: a repeated cross-sectional analysis. BMC Public Health. 2020;20:1–12.
Peyvandi S, Baer RJ, Moon-Grady AJ, Oltman SP, Chambers CD, Norton ME, et al. Socioeconomic mediators of racial and ethnic disparities in congenital heart disease outcomes: a population-based study in California. J Am Heart Assoc. 2018;7:e010342.
Miao Q, Dunn S, Wen SW, Lougheed J, Reszel J, Venegas CL, et al. Neighbourhood maternal socioeconomic status indicators and risk of congenital heart disease. BMC Pregnancy Childbirth. 2021;21:1–21.
Xiang L, Su Z, Liu Y, Zhang X, Li S, Hu S, et al. Effect of family socioeconomic status on the prognosis of complex congenital heart disease in children: an observational cohort study from China. Lancet Child Adolescent Health. 2018;2:430–9.
Rarani MA, Rashidian A, Khosravi A, Arab M, Abbasian E, Morasae EK. Changes in socio-economic inequality in neonatal mortality in Iran between 1995-2000 and 2005-2010: an Oaxaca decomposition analysis. Int J Health Policy Manag. 2017;6:219.
Hosseinpoor AR, Van Doorslaer E, Speybroeck N, Naghavi M, Mohammad K, Majdzadeh R, et al. Decomposing socioeconomic inequality in infant mortality in Iran. Int J Epidemiol. 2006;35:1211–9.
Pabayo R, Kawachi I, Gilman SE. US state-level income inequality and risks of heart attack and coronary risk behaviors: longitudinal findings. Int J Public Health. 2015;60:573–88.
Dewan P, Rørth R, Jhund PS, Ferreira JP, Zannad F, Shen L, et al. Income inequality and outcomes in heart failure: a global between-country analysis. JACC Heart Failure. 2019;7:336–46.
Vukojević M, Zovko A, Talić I, Tanović M, Rešić B, Vrdoljak I, et al. Parental socioeconomic status as a predictor of physical and mental health outcomes in children—literature review. Acta Clin Croat. 2017;56:742–8.
Larson CP. Poverty during pregnancy: its effects on child health outcomes. Paediatr Child Health. 2007;12:673–7.
Zhang S, Wang L, Yang T, Chen L, Zhao L, Wang T, Chen L, Ye Z, Zheng Z, Qin J. Parental alcohol consumption and the risk of congenital heart diseases in offspring: An updated systematic review and meta-analysis. Eur J Prev Cardiol. 2020;27:410–21.
Snijder CA, Vlot IJ, Burdorf A, Obermann-Borst SA, Helbing WA, Wildhagen MF, et al. Congenital heart defects and parental occupational exposure to chemicals. Hum Reprod. 2012;27:1510–7.
Obeid R, Holzgreve W, Pietrzik K. Folate supplementation for prevention of congenital heart defects and low birth weight: an update. Cardiovasc Diagnosis Ther. 2019;9:S424.
Hunter LE, Simpson JM. Prenatal screening for structural congenital heart disease. Nat Rev Cardiol. 2014;11:323.
Qu Y, Lin S, Bloom MS, Wang X, Ye B, Nie Z, et al. Maternal folic acid supplementation mediates the associations between maternal socioeconomic status and congenital heart diseases in offspring. Prev Med. 2021;143:106319.
Yazdi-Feyzabadi V, Amini-Rarani M, Delavari S. The Health Consequences of Economic Sanctions: Call for Health Diplomacy and International Collaboration. Arch Iran Med. 2020;23:S51–s53.
Sadoh W, Nwaneri D, Owobu A. The cost of out-patient management of chronic heart failure in children with congenital heart disease. Niger J Clin Pract. 2011;14:65.
Acknowledgements
The authors would like to thank all of the mothers who participated in this study.
Funding
The study was funded by Isfahan University of Medical Sciences, Isfahan, Iran with research code No. 298204.
Author information
Authors and Affiliations
Contributions
MN and MA-R contributed to conception. All authors contributed to the acquisition, analysis, or interpretation of data for the work. All authors gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study received the required ethics approval from Isfahan University of Medical Sciences Research Ethics Committee, Isfahan, Iran, with ethics code No. IR.MUI.RESEARCH.REC.1399.118. Informed consent has been obtained from subjects of the current study. Besides, Participants sign a written informed consent in which they have been assured that their identities and responses will be anonymous and that participants’ data will be kept confidential as possible.
Consent for publication
Not applicable.
Competing interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Amini-Rarani, M., Vahedi, S., Borjali, M. et al. Socioeconomic inequality in congenital heart diseases in Iran. Int J Equity Health 20, 251 (2021). https://doi.org/10.1186/s12939-021-01591-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12939-021-01591-3