Abstract
Background
Conventional indicators used to access the nutritional status of children tend to underestimate the overall undernutrition in the presence of multiple anthropometric failures. Further, factors contributing to the rich-poor gap in the composite index of anthropometric failure (CIAF) have not been explored. This study aims to estimate the prevalence of CIAF and quantify the contribution of factors that explain the rich-poor gap in CIAF.
Methods
The present study used data of 38,060 children under the age of five years and their biological mothers, drawn from the nationally representative Comprehensive National Nutrition Survey of children and adolescents aged 0–19 years in India. The CIAF outcome variable in this study provide an overall prevalence of undernutrition, with six mutually exclusive anthropometric measurements of height-for-age, height-for-weight, and weight-for-age, calculated using the World Health Organization (WHO) Multicenter Growth Reference Study. Multivariate regression and decomposition analysis were used to examine the association between covariates with CIAF and to estimate the contribution of different covariates in the existing rich-poor gap.
Results
An overall CIAF prevalence of 48.2% among children aged aged under 5 years of age was found in this study. 6.0% children had all three forms of anthropometric failures. The odds of CIAF were more likely among children belonging to poorest households (AOR: 2.41, 95% CI: 2.12–2.75) and those residing in urban area (AOR: 1.06, 95% CI 1.00–1.11). Children of underweight mothers and those with high parity were at higher risk of CIAF (AOR: 1.51, 95% CI: 1.42–1.61) and (AOR: 1.15, 95% CI: 1.08–1.22), respectively. Children of mother exposed to mass media were at lower risk of CIAF (AOR: 0.87, 95% CI: 0.81–0.93).
Conclusion
This study estimated a composite index to assess the overall anthropometric failure, which also provides a broader understanding of the extent and pattern of undernutrition among children. Findings show that maternal covariates contribute the most to the rich-poor gap. As well, the findings suggest that intervention programs with a targeted approach are crucial to reach the most vulnerable groups and to reduce the overall burden of undernutrition.
Similar content being viewed by others
Background
Worldwide, 1 in 3 children under the age of 5 years are malnourished [1]. Undernutrition in the form of stunting or wasting affected almost 200 million children below the age of 5 years globally in 2018 [1]. Moreover, it is considered to play a major role in the premature deaths of millions of children in developing countries [2]. Those who survive are rendered vulnerable to infections and diseases, devastating the lives of hundreds of millions of children [3, 4]. The complexity of undernutrition in developing countries is amplified due to its proximate association with poverty and inequality. Evidence of socio-economic differences in maternal and child morbidity and mortality rates is well documented [5,6,7,8,9,10,11,12,13]. Studies have identified poverty as the leading cause of malnutrition in developing countries that leads to poor nutritional status, intergenerationally and prevent social improvement and equity [5, 8].
To evaluate the nutritional status, three conventional anthropometric indices of stunting (low height-for-age), wasting (low weight-for-height) and underweight (low weight-for-age) were calculated [9, 14]. According to the World Health Organization (WHO), these anthropometric indices reflect distinct biological processes and are necessary for determining appropriate nutritional interventions [14]. Previous studies in Asian countries have found a concurrent relationship between stunting and wasting when compared to a reference population [15]. Underweight children may experience stunting and/or wasting and some of them may experience all three forms of anthropometric failures [16]. None of the three conventional nutritional indicators can estimate the true overall burden of undernutrition in children under the age of 5 years.
Subsequently, an aggregated single anthropometric measure providing an overall estimate of under-nourished children has been proposed and known as the Composite Index of Anthropometric Failure (CIAF) [9, 17]. The original model [17] consisted of six sub-groups of anthropometric failure (Groups A–F); A: No failure, B: Only wasting, C: Wasting and underweight, D: Stunting, wasting and underweight, E: Stunting and underweight, F: Stunting only. Further, Nandy [9] stressed on an additional sub-group, Group Y, as Underweight only. The CIAF included those children experiencing stunting, underweight, wasting, and multiple failures (Groups B–Y) and excluded those children who did not exhibit any anthropometric failure (Group A). The combination of wasted and stunted was not included in the CIAF classification as it was physically impossible for a child to simultaneously experience stunting and wasting and not be underweight [9].
In India, the national prevalence of stunting and wasting in children under the age of 5 years is 37.0 and 20.8% [18], respectively, which is greater than the average of stunting and wasting from developing countries. Few recent studies confirm the existence of socio-economic inequality in prevalence of undernutrition at district level in India [19] and among the urban population [20]. However, previous studies have documented the socio-economic gap in child undernutrition based on conventional indicators of undernutrition [7, 10, 17, 19, 20]. Whereas, only few studies have documented the socio-economic gap considering CIAF as an outcome of interest, but are limited to specific geography [21]. This study utilizes data from Comprehensive National Nutrition survey to examine the socio-economic gap in child malnutrition using a single anthropometric measure—CIAF—in India. More specifically, the study aimed to identify the maternal, child and household level factors responsible for the rich-poor gap in child malnutrition and quantify their contribution to this gap by using the multivariate decomposition technique.
Methods
Dataset and sample covered
This study used nationally representative data from the Comprehensive National Nutrition Survey (CNNS) in India, which adopted a multi-stage sampling design using probability proportional to size (PPS) sampling procedure, after geographical stratification of urban and rural areas, to select the primary sampling units. For smaller Primary sampling units (PSUs), the sampling design was conducted in two stages; in the first stage, PSUs were selected using PPS sampling and in the second stage, a systematic random selection of households was done within each PSU. In large PSUs, the sampling design involved three stages, with the addition of a segmentation procedure to reduce enumeration areas to manageable sizes. This cross-sectional household survey was designed to provide nationally representative and comprehensive nutritional profiling of preschoolers (0–4 years), children of school-going age (5–9 years) and adolescents (10–19 years). Children who had a chronic illness, physical deformity, mental illness, cognitive disability, or an ongoing current illness (high fever, infection) were not included in the study. Analyses for this study was conducted by utilizing anthropometric data of 38,060 children aged under 5 years and their biological mothers, along with other socio-economic indicators that were collected across all 30 states of India between February 24, 2016 and October 26, 2018. The procedure of arriving at a final analytical sample size is described in Table 1.
Outcome variable
Weight was recorded in kilograms and height in centimeters, using a digital SECA scale and three-piece wooden height/length board, respectively. Before measurements were taken, the instrument was set up on a portable wooden square surface and a spirit level was used to ensure an even measurement surface. Recumbent length was measured in children who were either less than 2 years of age or 85 cm in length and for the remaining children, their standing height was measured [20]. WHO Anthro-Plus software was used to calculate children’s Z-scores standard deviation (SD) scores for height-for-age (HAZ), weight-for-age (WAZ) and weight-for-height (WHZ) [22,23,24]. Wasting was defined as weight-for-height (Z-Score [WHZ] < −2SD); stunting was defined as height-for-age (Z-Score [HAZ] < −2SD) and underweight was defined as weight-for-age (Z-Score [WAZ] < −2SD). CIAF subgroups are presented in Table 2. The sum of the children in groups B to Y provided the CIAF. Group A was excluded from the final estimates as children in this category had no anthropometric failure.
Covariates
Based on the available literature [25,26,27], maternal, child and household characteristics associated with malnutrition were included in the analysis. Maternal covariates included age, education, employment status, mass media exposure and parity. Child covariates included age, sex, and morbidity in the past 2 weeks (diarrhea, respiratory infection, or fever). The wealth index was computed using data on the household’s ownership of specific assets, such as televisions and bicycles, materials used for housing construction, access to and type of water and sanitation facilities and the number and kind of other consumer goods they owned. The index was included as a household-level covariate. Households were given scores derived at using the principal component analysis adjusted for national and state-level weights. Wealth quintiles were computed by dividing the weighted distribution into five equal categories, each with 20% of the sample population. Other household-level covariates included caste and place of residence. The list of selected covariates and construction plan are provided in Table 2.
Statistical analysis
Descriptive statistics were used to describe variables for the study. The association of CIAF with socio-economic characteristics was verified by Pearson’s χ2 test. Logistic regression was used to examine the association of CIAF with socio-demographic covariates. Results were presented as unadjusted odds ratios (UOR) and adjusted odds ratios (AOR) with 95% confidence intervals (CI). The estimates of CIAF prevalence in the population and all regression models were adjusted to consider the complex sampling design of the CNNS, 2016–18 by including primary sampling units, sampling weights and strata in the models.
To quantify the contribution of selected predictors in explaining the rich-poor gap in the prevalence of CIAF, multivariate decomposition analysis was used. Multivariate decomposition technique uses the output from regression models to partition the components of a group difference in a statistic, such as a mean or proportion, into a component attributable to compositional differences between groups, i.e., differences in characteristics or endowments, and a component attributable to differences in the effects of characteristics, i.e., differences in the returns, coefficients or behavioral responses. The mean difference in Y between groups A and B can be decomposed as,
where Y denotes the N × 1 dependent variable vector, X is an N × K matrix of independent variables, and β is a K × 1 vector of the coefficient.
The component labeled E refers to the part of the differential attributable to differences in endowments or characteristics usually called the explained component or characteristics effects. C refers to the part of the differential attributable to differences in coefficients or effects usually known as the unexplained component or coefficient effects; where A is the richest children (comparison group) and B is the poorest children (reference group). Therefore, E reflects a counterfactual comparison of the difference in outcomes from the richest children’s perspective and C reflects a counterfactual comparison of outcomes from the poorest children’s perspective. STATA 16.0 software was used for data analysis.
Ethical review
The CNNS received ethical clearance from the Ethical Review Board of the Post Graduate Institute for Medical Education and Research (PGIMER) and the Institutional Review Board of the Population Council in New York. All aspects of the survey were informed, following which written consent was obtained from caregivers of children aged under 5 years.
Results
The findings of this study show an overall CIAF prevalence of 48.2% among children aged under 5 years. 19.1% of children suffered from only one form of anthropometric failure (groups B, F and G), which include wasting only (4.6%), stunting only (11.5%) and underweight only (3.0%). 6.5% of the children suffered from both wasting & underweight (group C) and 16.6% were stunted as well as underweight (group E), constituting 22.1% of children with two simultaneous failure groups (group C and E). As shown in Table 3, 6.0% of children had all three forms of anthropometric failures. The distribution of covariates among poorest and richest socio-economic groups is presented in supplementary Table 1.
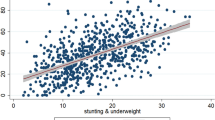
Table 4 presents the percentage of children under the age of 5 years who had anthropometric failure based on maternal, birth and socio-demographic characteristics. CIAF was found in 63.1% children from poorest households, whereas only 31.5% children from richest household experienced CIAF. 50.5% children from rural areas and those with morbidity in the 2 weeks prior to survey had CIAF. CIAF was found in 59.1% and 32.1% of children with underweight and overweight/obese mother respectively and in 60% of children with mothers who had no formal schooling, 46% whose mothers were not working and more than half with mothers who were not exposed to mass media.
Table 5 presents the factors associated with CIAF. In the multivariate analysis of socio-demographic factors, the odds of CIAF were more likely among children belonging to poorest households (AOR: 2.41, 95% CI: 2.12–2.75), Scheduled Caste/Scheduled Tribes (SC/ST) households (AOR: 1.06, 95% CI: 1.01–1.12) and those residing in urban area (AOR: 1.06, 95% CI 1.00–1.11). Children of mothers who were underweight and had high parity were at higher risk of CIAF (AOR: 1.51, 95% CI: 1.42–1.61 and AOR: 1.15, 95% CI: 1.08–1.22) respectively. Children with mothers who were exposed to mass media were at a lower risk of CIAF (AOR: 0.87, 95% CI: 0.81–0.93). Elder children in age group 2–4 years (AOR: 1.07, 95% CI: 1.02–1.12), male children (AOR: 1.07, 95% CI: 1.02–1.12) and those with morbidity in the 2 weeks prior to survey (AOR: 1.07, 95% CI: 1.02–1.13) were at a higher risk of CIAF.
Table 6 shows the how the endowment and coefficient effects contribute to the gap in CIAF prevalence between children of poorest and richest households. A negative contribution indicates that the determinant narrowed the gap between poorest and richest households and vice-versa. Results showed that the differences due to coefficient accounted for 59.45% of the observed socio-economic differential in the prevalence of CIAF and the difference due to characteristics accounted for 40.55%. For instance, if the mothers from the poorest households were as educated to those from the richest households, then the prevalence of CIAF would reduce by 15.03%. Similarly, equalizing parity of mothers and their exposure to mass media in poorest and richest households could reduce the prevalence of CIAF by 5.38 and 4.91%, respectively. The difference in mothers’ body mass index (BMI) among the poorest and richest households contributed to a gap of 13.6%—underweight: 6.47% and overweight/obese: 7.13%)—in the prevalence of CIAF.
Discussion
This study attempted to estimate the overall burden of child undernutrition at the national level by calculating CIAF and the factors contributing to the rich-poor gap in the prevalence of CIAF. The overall prevalence of CIAF was reported as 48.1%, which was in line with the estimates reported by studies conducted in Assam and Bangladesh [28, 29]. However, studies conducted in states of Odisha, West Bengal and Chhattisgarh reported higher prevalence of CIAF [30,31,32]. Similarly, studies conducted in Ethiopia [33] and Nepal [31] reported higher prevalence, whereas studies from Zimbabwe and Peru reported lower prevalence of CIAF [34]. The findings of this study align with the findings of previous studies [26,27,28,29] and show that stunting is the most prevalent type of undernutrition. These findings suggest that 16.6% of children experienced both stunting and underweight, indicating the coexistence of both acute and chronic undernutrition and emphasizing the importance of a composite index to gauge the scale of undernutrition.
Several socio-demographic, maternal and child related factors were found to be associated with the prevalence of CIAF in this study. Children belonging to poor households were found to be at a higher risk of being undernourished as compared to children from rich households. Systematic review conducted in low- and middle-income countries, including India, reported that percent point difference between the poorest and richest households remains the same overtime [35]. This study further revealed that maternal nutrition, education, parity, and exposure to mass media were associated with child undernutrition and subsequently with the overall CIAF.
Maternal undernutrition in form of low stature or underweight is consequent to prevailing adverse social and economic circumstances. Mothers who are undernourished in their formative years are more likely to deliver small-for-gestational age (SGA) babies, who then are at a higher risk of undernutrition [36]. Findings of this study suggest that children of a mothers with no or lower education, no exposure to mass media and high parity were associated with CIAF. These results corroborate findings from other studies that illustrate how low education and no exposure to mass media limit a mother’s knowledge and consequently result in poor awareness for nutritional programs and child feeding practices, leading to child undernutrition [37, 38].
Male children in this study were found at a greater risk of being undernourished as per CIAF. This finding was contrary to other studies conducted in developing countries with the standalone undernutrition indicators [39]. However, a meta-analysis conducted in sub-Saharan Africa reported that more male children were stunted than females, suggesting males as more vulnerable to health inequalities than females [40]. Further research is needed to understand this anomaly. Findings of this study suggest that an increase in the child’s age was positively associated with undernutrition. These findings are in line with previous studies [41, 42]. One probable reason for this could be that a child’s nutritional needs are not fulfilled as per the demand with increasing age.
Another objective of this study was to disaggregate the effect of the determinants in explaining the gap in prevalence of CIAF between rich and poor households in India. The results revealed that 41% of the gap in prevalence of CIAF was attributed mainly to the distribution of determinants between poor and rich households. Maternal factors were found as main contributors to endowment effect, explaining most of the gap in the prevalence of CIAF. Low level of maternal education in poor households limit the practice of healthy behavior for reasons such as limited knowledge, poor nutritional practices, lack of resources, underutilization of health care services and depleted autonomy within the household. These limitations to the practice of healthy behavior are detrimental factors that affect child nutritional outcome [38]. The nutritional status of mothers among poor household is another important factor responsible for the poor nutritional status of children. Intrauterine growth retardation in malnourished mothers is known to be directly associated with premature deliveries and low birth-weight infants, leading to different morbidities along with undernutrition in early childhood [43]. Mother’s exposure to mass media plays a vital role in reducing the rich poor gap. Mothers with exposure to mass media are better informed on breastfeeding practices, government health initiatives and other programs that promote the health of children [44]. Caste was another contributor to the endowment effect. The significance of this may be attributed to the fact that deprived caste groups such as the SC/ST are clustered primarily in unhealthy living environments as compared to the remaining population. In contrast, other caste groups are characterized by a relatively better socioeconomic status and are thus at a lower risk of childhood undernutrition [45].
One of the limitations in this study is non-availability of household level factors related to water, sanitation and hygiene and maternal nutrition like anemia and other factors like maternal autonomy, which might influence the status of child nutritional, have not been assessed in this study. Further research is needed to explore the role of these variables in anthropometric failure among under-five children.
With the launch of Poshan Abhiyaan, India is striving to achieve SDG-2, that aims to end all forms of malnutrition by 2030 [46]. While the importance of conventional standalone indicators to screen undernutrition is well documented, screening through them may lead to exclusion of those who demonstrate multiple manifestations. In addition, information from conventional indicators in the overall change in undernutrition is contradictory at times. The CIAF takes the differences between the three conventional indicators into account and provide an indicator that can be used to identify nutritionally vulnerable geographies as well as segments of the population. Findings from this study can be helpful to identify groups for targeted interventions that aim to reduce rich-poor inequity.
Conclusion
There were two key findings of this study. Firstly, a composite index to assess the overall anthropometric failure is essential as it provides a broader understanding of the extent and pattern of undernutrition among children. Secondly, findings suggest that intervention programs with a targeted approach are needed to reach the most vulnerable groups and should devise policy to strengthen the factors which will narrow the rich-poor gap and further reduce the overall burden of undernutrition.
Availability of data and materials
Reasonable request for data used in this article may be made to the corresponding author.
References
UNICEF. The state of the World’s children 2019. New York: Children, Food and Nutrition: Growing well in a changing world; 2019.
Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361(9376):2226–34. https://doi.org/10.1016/S0140-6736(03)13779-8.
World Bank. 1993. World Development Report 1993 : Investing in Health. New York: Oxford University Press. © World Bank. https://openknowledge.worldbank.org/handle/10986/5976 License: CC BY 3.0 IGO.
World Health Organization & World Bank. Better health for poor children: a special report. World Health Organization. 2001. https://apps.who.int/iris/handle/10665/69704.
Hong R, Banta JE, Betancourt JA. Relationship between household wealth inequality and chronic childhood under-nutrition in Bangladesh. Int J Equity Health. 2006;5(1):15. https://doi.org/10.1186/1475-9276-5-15.
Houweling TA, Ronsmans C, Campbell OM, Kunst AE. Huge poor-rich inequalities in maternity care: an international comparative study of maternity and child care in developing countries. Bull World Health Organ. 2007;85(10):745–54. https://doi.org/10.2471/BLT.06.038588.
Kanjilal B, Mazumdar PG, Mukherjee M, Rahman MH. Nutritional status of children in India: household socio-economic condition as the contextual determinant. Int J Equity Health. 2010;9(1):19. https://doi.org/10.1186/1475-9276-9-19.
Larrea C, Kawachi I. Does economic inequality affect child malnutrition? The case of Ecuador. Soc Sci Med. 2005;60(1):165–78. https://doi.org/10.1016/j.socscimed.2004.04.024.
Nandy S, Irving M, Gordon D, Subramanian SV, Smith GD. Poverty, child undernutrition and morbidity: new evidence from India. Bull World Health Organ. 2005;83(3):210–6 DOI: /S0042-96862005000300014.
Subramanyam MA, Kawachi I, Berkman LF, Subramanian SV. Socioeconomic inequalities in childhood undernutrition in India: analyzing trends between 1992 and 2005. PLoS One. 2010;5(6):e11392. https://doi.org/10.1371/journal.pone.0011392.
Van de Poel E, Hosseinpoor AR, Speybroeck N, Van Ourti T, Vega J. Socioeconomic inequality in malnutrition in developing countries. Bull World Health Organ. 2008;86(4):282–91. https://doi.org/10.2471/BLT.07.044800.
Wagstaff A. Socioeconomic inequalities in child mortality: comparisons across nine developing countries. Bull World Health Organ. 2000;78(1):19–29.
Kumar A, Kumari D. Decomposing the rural-urban differentials in childhood malnutrition in India, 1992–2006. Asian Popul Stud. 2014;10(2):144–62. https://doi.org/10.1080/17441730.2014.902161.
WHO Expert Committee on Physical Status : the Use and Interpretation of Anthropometry ( 1993 : Geneva, Switzerland) & World Health Organization. ( 1995) .https://apps.who.int/iris/handle/10665/37003
Richard SA, Black RE, Gilman RH, Guerrant RL, Kang G, Lanata CF, et al. Wasting is associated with stunting in early childhood. J Nutr. 2012;142(7):1291–6. https://doi.org/10.3945/jn.111.154922.
(IFPRI) IFPRI. Global Nutrition Report 2016: From Promise to Impact: Ending Malnutrition by 2030″: International Food Policy Research Institute (IFPRI), 2016.
P S. Poverty and Undernutrition: Theory, Measurement, and Policy. New Delhi: Oxford India Paperback; 2000.
IIPS. National Family Health Survey (NFHS-4), 2015–16: India. Mumbai: IIPS; 2017.
Singh S, Srivastava S, Upadhyay AK. Socio-economic inequality in malnutrition among children in India: an analysis of 640 districts from National Family Health Survey (2015-16). Int J Equity Health. 2019;18(1):203. https://doi.org/10.1186/s12939-019-1093-0.
Singh SK, Srivastava S, Chauhan S. Inequality in child undernutrition among urban population in India: a decomposition analysis. BMC Public Health. 2020;20(1):1852. https://doi.org/10.1186/s12889-020-09864-2.
Sabu KU, Sundari Ravindran TK, Srinivas PN. Factors associated with inequality in composite index of anthropometric failure between the Paniya and kurichiya tribal communities in wayanad district of Kerala. Indian J Public Health. 2020;64(3):258–65. https://doi.org/10.4103/ijph.IJPH_340_19.
(WHO) WHO. Multicenter Growth Reference Study Group. WHO child growth standards: length/height-for-age, weight-for-length, weight-for-height and body mass index-forage: methods and development. Geneva: World Health Organization; 2006.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–7. https://doi.org/10.2471/BLT.07.043497.
WHO. WHO AnthroPlus for personal computers Manual: Software for assessing growth of the world's children and adolescents. Geneva: WHO; 2009.
Akombi BJ, Agho KE, Merom D, Hall JJ, Renzaho AM. Multilevel Analysis of Factors Associated with Wasting and Underweight among Children Under-Five Years in Nigeria. Nutrients. 2017;9(1):44.
Das S, Gulshan J. Different forms of malnutrition among under five children in Bangladesh: a cross sectional study on prevalence and determinants. BMC Nutrition. 2017;3(1):1. https://doi.org/10.1186/s40795-016-0122-2.
Sen J, Mondal N. Socio-economic and demographic factors affecting the composite index of anthropometric failure (CIAF). Ann Hum Biol. 2012;39(2):129–36. https://doi.org/10.3109/03014460.2012.655777.
Bharali N, Singh K, Nitish M. Composite index of anthropometric failure (CIAF) among Sonowal Kachari tribal preschool children of flood effected region of Assam, India. Anthropol Rev. 2019;82(2):163–76. https://doi.org/10.2478/anre-2019-0012.
Islam MS, Biswas T. Prevalence and correlates of the composite index of anthropometric failure among children under 5 years old in Bangladesh. Matern Child Nutr. 2020;16(2):e12930. https://doi.org/10.1111/mcn.12930.
Boregowda GS, Soni GP, Jain K, Agrawal S. Assessment of under nutrition using composite index of anthropometric failure (CIAF) amongst toddlers residing in urban slums of Raipur City, Chhattisgarh, India. J Clin Diagn Res. 2015;9(7):LC04–6. https://doi.org/10.7860/JCDR/2015/12822.6197.
Goswami M. Prevalence of under-nutrition measured by composite index of anthropometric failure (CIAF) among the Bhumij children of northern Odisha, India. J Nepal Paediatr Soc. 2016;36(1):61–7. https://doi.org/10.3126/jnps.v36i1.14390.
Shit S, Taraphdar P, Mukhopadhyay DK, Sinhababu A, Biswas AB. Assessment of nutritional status by composite index for anthropometric failure: a study among slum children in Bankura, West Bengal. Indian J Public Health. 2012;56(4):305–7. https://doi.org/10.4103/0019-557X.106421.
Endris N, Asefa H, Dube L. Prevalence of malnutrition and associated factors among children in rural Ethiopia. Biomed Res Int. 2017;2017:6587853.
Nandy S, Miranda JJ. Overlooking undernutrition? Using a composite index of anthropometric failure to assess how underweight misses and misleads the assessment of undernutrition in young children. Soc Sci Med. 2008;66(9):1963–6. https://doi.org/10.1016/j.socscimed.2008.01.021.
Vollmer S, Harttgen K, Kupka R, Subramanian SV. Levels and trends of childhood undernutrition by wealth and education according to a composite index of anthropometric failure: evidence from 146 demographic and health surveys from 39 countries. BMJ Glob Health. 2017;2(2):e000206. https://doi.org/10.1136/bmjgh-2016-000206.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51. https://doi.org/10.1016/S0140-6736(13)60937-X.
Miller J, Rodgers Y. Mother's education and children’s nutritional status: new evidence from Cambodia. Asian Dev Rev. 2009;26:131–65.
Mukherjee R, Chaturvedi S, Bhalwar R. Determinants of nutritional status of school children. Med J Armed Forces India. 2008;64(3):227–31. https://doi.org/10.1016/S0377-1237(08)80099-8.
Sen A, Sunil S. Malnutrition of rural children and the sex bias. Econ Polit Wkly. 1983;18(19/21):855–64.
Wamani H, Astrom AN, Peterson S, Tumwine JK, Tylleskar T. Boys are more stunted than girls in sub-Saharan Africa: a meta-analysis of 16 demographic and health surveys. BMC Pediatr. 2007;7(1):17. https://doi.org/10.1186/1471-2431-7-17.
Rahman A, Chowdhury S. Determinants of chronic malnutrition among preschool children in Bangladesh. J Biosoc Sci. 2007;39(2):161–73. https://doi.org/10.1017/S0021932006001295.
Wamani H, Tylleskar T, Astrom AN, Tumwine JK, Peterson S. Mothers’ education but not fathers’ education, household assets or land ownership is the best predictor of child health inequalities in rural Uganda. Int J Equity Health. 2004;3(1):9. https://doi.org/10.1186/1475-9276-3-9.
Vitolo MR, Gama CM, Bortolini GA, Campagnolo PD, Drachler ML. Some risk factors associated with overweight, stunting and wasting among children under 5 years old. J Pediatr. 2008;84(3):251–7. https://doi.org/10.2223/JPED.1776.
Dangura D, Gebremedhin S. Dietary diversity and associated factors among children 6–23 months of age in Gorche district, Southern Ethiopia: Cross-sectional study. BMC Pediatr. 2017;17(1):6.
Van de Poel E, Speybroeck N. Decomposing malnutrition inequalities between scheduled castes and tribes and the remaining Indian population. Ethn Health. 2009;14(3):271–87. https://doi.org/10.1080/13557850802609931.
United Nations, 2015. Transforming Our World: The 2030 Agenda for Sustainable Development. New York: UN Publishing.
Acknowledgements
Not applicable.
Funding
This study was funded by UNICEF.
Author information
Authors and Affiliations
Contributions
AP, RA, and SA conceptualized the manuscript. PKA designed the survey, NK conducted data quality control and computed sampling weights. AP led the statistical analyses and SA contributed to analyses. RA guided the analysis and AP, RA and AS interpreted the results. AP led the writing of the manuscript with inputs from RA and SA. RA, AS, SR, NK, RJ and PKA reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The CNNS received ethical clearance from the Ethical Review Board of the Post Graduate Institute for Medical Education and Research (PGIMER) and the Institutional Review Board of the Population Council in New York. All aspects of the survey were informed, following which written consent was obtained from caregivers of children aged under 5 years.
Consent for publication
All authors reviewed the manuscript and gave consent for publication.
Competing interests
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Percentage of the children under-five by their maternal, birth and socio-demographic characteristics between the richest and the poorest socioeconomic groups.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Porwal, A., Acharya, R., Ashraf, S. et al. Socio-economic inequality in anthropometric failure among children aged under 5 years in India: evidence from the Comprehensive National Nutrition Survey 2016–18. Int J Equity Health 20, 176 (2021). https://doi.org/10.1186/s12939-021-01512-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12939-021-01512-4