Abstract
Background
People with prediabetes can postpone or even reverse progression to type 2 diabetes (T2D) by making dietary changes. This study aimed to examine the association of changes in consumption of total and specific types of dairy products with the subsequent risk of incident T2D among individuals with prediabetes.
Method
This cohort study included 639 individuals (50% female, mean age 47.3 years) of the Tehran Lipid and Glucose Study (TLGS) who had prediabetes at baseline. We assessed 3-year changes in the consumption of dairy products using a food frequency questionnaire. Using multivariable logistic regression, odds ratios (OR) and 95% confidence intervals (CI) were calculated for the association of changes in intake of total and subtypes of dairy products during a 3-year interval with the risk of incident T2D in the subsequent 3 years.
Results
After almost 9 years of follow-up, the incidence of T2D was 25.2%. Compared with individuals whose intake remained relatively stable over 3 years, those who decreased consumption of total dairy (> 0.5 servings/day) had a higher T2D risk (OR = 1.56; 95% CI: 1.02 to 2.41). Increasing low-fat dairy consumption by 0.50 serving/d was associated with a lower risk of T2D (OR = 0.56; 95% CI: 0.35 to 0.90) compared with stable consumption. Those who increased consumption of low-fat milk (OR = 0.59; 95% CI: 0.37 to 0.92) and low-fat yogurt (OR = 0.55; 95% CI: 0.33 to 0.93) had a lower risk of T2D than those who were relatively stable in their consumption. Replacing low-fat milk and yogurt with regular cheese was associated with 66 and 47% higher risk of T2D, respectively.
Conclusion
In individuals with prediabetes, increasing consumption of low-fat dairy, low-fat milk, and low-fat yogurt had reduced risk of subsequent T2D. These data suggest a role of low-fat dairy products in the prevention of T2D among prediabetes patients.
Similar content being viewed by others
Introduction
Prediabetes is a health condition characterized by dysregulation of glucose homeostasis that temporarily presents between the normal metabolic state and the progression to overt type 2 diabetes (T2D) [1]. Individuals with prediabetes are highly prone to developing cardiovascular disease [2] and the possibility of lifetime conversion to T2D is up to 70% [3]. The prevalence and incidence of prediabetes are rising worldwide [4, 5] and, by 2035, the International Diabetes Federation estimates a prevalence of prediabetes of 471 million people globally [6]. Diet modification is recommended as an effective strategy in patients with prediabetes to prevent or delay the onset of T2D and other complications [3, 7]; however, the literature on the association of dietary intake with incident T2D among individuals with prediabetes is limited.
Foods classified as dairy products are widely consumed in many parts of the world and supply protein and minerals necessary for human health [8]. However, dairy products also contain factors conferring health risks, including cholesterol and saturated fatty acids (SFAs), though the mixture of SFA found in dairy does not raise the cardio-metabolic risk to the same extent as other foods [9, 10]. Likely because of the interplay of various nutrients and processing characteristics, association studies of the amount and type of dairy foods with T2D risk demonstrate mixed results [11,12,13]. A possible mediating effect of baseline glycemic status on risk conferred by intake of various types of dairy foods and incident diabetes has been proposed in a new prospective study of the Framingham Heart Study Offspring Cohort [14]. Thus, the contradictory results observed among previous studies may be accounted for by the lack of attention to the baseline glycemic status of participants [14]. The study showed that high-fat dairy and cheese intake had inverse, dose-dependent associations with hazard ratios of incident T2D of 0.70 and 0.63, respectively, in patients with prediabetes when adjusted for baseline glycemia whereas other dairy products, including low-fat dairy, skimmed milk, whole milk, and yogurt, had no association [14]. However, whether dynamic within-person changes over time in the total and subtypes of dairy product consumption are associated with a subsequent risk of T2D among prediabetes patients has not been reported. Evaluating changes in dairy food consumption rather than relying on the baseline intake of individuals is a more robust analytical approach because it can imitate dietary interventions in clinical trials [15]. Thus, in the present analyses, we aim to evaluate the association of changes in total consumption of dairy and subtypes of dairy foods (high-fat milk, low-fat milk, low-fat yogurt, high-fat yogurt, regular cheese, and cream cheese), with subsequent risk of incident T2D. We also used these changes in dairy exposures to estimate the association of replacing specific dairy foods with others on subsequent risk of T2D.
Method
Study population
The Tehran Lipid and Glucose Study (TLGS) is a community-based, longitudinal study initiated in 1998 to determine the risk factors for non-communicable diseases in a representative urban population of Tehran. Follow-up visits happened at approximately 3-year intervals. A detailed description of the study design has previously been published [16]. In the fourth examination cycle (2009–2011) of the TLGS, among 12,823 participants who completed questionnaires and a standard medical examination as well as laboratory and anthropometric measurements, a representative sample of participants of 7956 individuals was randomly selected for dietary assessment. Follow-up surveys were conducted in the fifth (2011–2014) and sixth (2015–2018) examinations. We used changes in total dairy consumption and its subtypes from the fourth (2009–2011) to fifth (2011–2014) examination cycles to predict the incidence of T2D risk in the sixth (2015–2018) examination cycle of TLGS. The fourth examination cycle was used as the baseline (initial) for the current analysis.
Among participants, 1401 men and women, aged ≥18 years who had prediabetes (impaired fasting glucose (IFG) [fasting plasma glucose (FPG) levels ≥100 to < 126 mg/dL (≥5.6 to < 7.0 mmol/L), or 2-h plasma glucose (2-hPG) of ≥140 to < 200 mg/dL (≥7.8 to < 11.1 mmol/L) in the fourth examination cycle were selected.
Participants were excluded if they reported a history of myocardial infarction, stroke, or cancer at the baseline examination (n = 23), if they were missing necessary covariates (n = 12), or if they had missing dietary data over follow-up (n = 462). We further excluded 92 participants with extreme and implausible energy intake at baseline or in the next examination cycle (defined as < 600 or > 3500 kcal/d for women and < 800 or > 4200 kcal/d for men). Participants were also excluded if they had diagnosed T2D in the fifth cycle (n = 43), or they missed the final follow-up examination (n = 253). Some participants fell into more than one exclusion category. The final sample size for analysis was 639 participants with prediabetes (Fig. 1). There were no significant differences between participants with follow-up measurements and those lost to follow-up (supplementary Table 1).
All participants signed a written informed consent form. The protocol was approved by the ethics committee of the Research Institute for Endocrine Sciences (IR.SBMU.ENDOCRINE.REC.1399.057), in compliance with the principles of the Declaration of Helsinki.
Assessment of diet
A semi-quantitative food frequency questionnaire (FFQ) was used to obtain information on the habitual consumption of food items at baseline (fourth cycle) and the fifth examination cycle of TLGS. Trained dietitians determined participants’ intake frequency of food items consumed through the previous year on a daily, weekly, or monthly basis via face-to-face interviews. Portion sizes of consumed foods were reported in household measures, which were then converted to grams.
The exposures of interest in the current analysis, all dairy products, were defined according to the USDA MyPlate (https://www.choosemyplate.gov/dairy) as “foods made from milk that retain their calcium content, including milk, yogurt, cheese, and ice cream.” Total dairy consumption (servings/d) was calculated as the sum of each of the dairy food items in the FFQ, including high-fat milk, low-fat milk, low-fat yogurt, high-fat yogurt, and regular cheese. Low-fat dairy was generated as the sum of low-fat milk plus low-fat yogurt, and high-fat dairy was calculated as the sum of high-fat milk, high-fat yogurt, and regular cheese. One serving of each dairy food item was converted as follows: 240 g for low-fat milk and high-fat milk, 227 g for low-fat yogurt and high-fat yogurt; 28 g for cream cheese and regular cheese; and 120 g for ice cream.
The reproducibility and validity of the FFQ was reported in a previous study [17, 18]. Energy-adjusted correlation coefficients of total dairy consumption based on the FFQ and those based on twelve 24-h dietary recalls among subsamples of men and women were 0.61 and 0.59, respectively. The energy-adjusted intraclass correlation coefficients for the reproducibility of two collected FFQ with a 14-month interval for men and women were 0.48 and 0.66 for total dairy consumption, respectively [18].
Assessment of outcome and definitions
At baseline and all subsequent examinations, fasting plasma glucose (FPG) was measured in overnight fasting plasma samples with an enzymatic colorimetric method using glucose oxidase (Pars Azmoon, Tehran, Iran). A standard 2-h plasma glucose (2-hPG) test was performed for all participants following oral glucose administration of 82.5 g glucose monohydrate solution [equivalent to 75 g anhydrous glucose; Cerestar EP, Spain]. Participants were classified as having T2D if they reported the use of an oral antidiabetic drug or insulin or had FPG ≥ 126 mg/dL (7 mmol/L) or 2-h PG ≥ 200 mg/dL (11.1 mmol/L).
Assessment of covariates
Detailed measurements of variables in the TLGS have been reported elsewhere [16]. Briefly, participants were invited to the TLGS center, and trained interviewers collected and updated information at 3-y follow-up intervals regarding the familial history of non-communicable diseases, cigarette smoking, medication usage, and assessment of physical activity. Body height and weight were measured, and BMI was calculated as weight in kg divided by height in meters squared (kg/m2). The mean of two measurements of systolic (SBP) and diastolic blood pressure (DBP) after a 15-min rest in the sitting position was recorded as the participant’s blood pressure. Hypertension was defined as an SBP ≥ 140 mmHg or a DBP ≥ 90 mmHg or taking antihypertensive drugs. A valid and reliable Persian version of the Modifiable Activity Questionnaire (MAQ) was applied to measure physical activity and metabolic equivalent (MET) values (MET-min/wk) was calculated.
Statistical analyses
For total dairy consumption, low-fat, or high-fat dairy products or subtypes of dairy products as the main exposure, categories of change were performed based on the mean and distribution of change of the dairy variables. For instance, individuals were categorized into 3 groups based on changes in total dairy product intake: 1) relatively stable consumption (±0.5 serving/d), 2) increased consumption of > 0.5 serving/d, and 3) decreased consumption of > 0.5 serving/d.
We illustrated the participants’ baseline characteristics and 3-year changes in lifestyle and dietary factors according to the changes in total dairy product consumption using descriptive statistics. The reported means (SD) were adjusted for age, and dietary factors further adjusted for total energy intake. Tests for linear trend across decreasing-stable-increasing categories of changes in total dairy product consumption were performed by assigning the median value of consumption within each category and treating these as continuous variables.
Odds ratio (ORs) and 95% confidence intervals (CIs) across categories of dairy exposures were estimated from multivariable binary logistic regression models by considering incidence of T2D as the dependent variable. Individuals with relatively stable consumption were assigned as the reference group. Model 1 was adjusted for age, sex, physical activity, change in body mass index, family history of diabetes, and total energy intake. Model 2 was further adjusted for dietary factors, including whole-grain intake and energy from protein and carbohydrate. P-trend values were estimated using the median value in each intake category. We further estimated the association of incident of T2D with changes in intakes of dairy products and its subtypes while modeled as continuous variables of 0.5 servings/d.
Lastly, applying cross-product terms, we checked for statistical interaction of changes in total dairy, low- and high- fat dairy with baseline age, sex, and BMI in the final model on the outcome. There were no interactions between those variables and total dairy intake on the incidence of T2D.
We applied substitution modeling to estimate the effect on diabetes risk of increasing the consumption of a subtype of dairy product and simultaneously decreasing consumption of another specific subgroup of dairy product. All type of dairy products were included in the same multivariate model, and OR were calculated from the difference in β coefficients of changes in intakes of different dairy exposure and the 95% CI from the corresponding variances and covariance [19].
We conducted a series of sensitivity analyses to test the robustness of our results: 1) to minimize the influence of outliers, we performed final analysis after excluding participants for whom dairy exposures were lower than the 0.5th percentile or higher than the 99.5th percentile; 2) we additionally adjusted other dietary factors including changes in fruit as well as legumes intakes to measure the impact of these dietary items on the relationship; 3) we further adjusted the final model for 3-year changes in body weight to estimate the extent to which weight change mediates the association between changes in dairy intake with risk of incident T2D; and 4) we added smoking status as a further covariate in final model. All analyses were performed using SPSS software, version 16, and a two-tailed P value of 0.05 was considered statistically significant.
Results
The mean ± SD age of the prediabetes population at baseline was 47.3 ± 11.d y, 50% were women, and 13.8% had a family history of diabetes. We identified 161 cases (25.2%) of incident T2D at the sixth cycle follow-up.
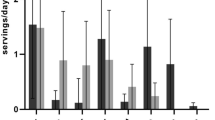
The changes in total, low- and high-fat dairy product consumption were − 0.12 ± 1.45 servings/d, 0.02 ± 1.21 and − 0.16 ± 0.87 serving/d, respectively. Age-adjusted baseline values and changes in physiological markers and lifestyle characteristics according to 3-y changes in total dairy consumption are presented in Table 1. Participants who increased ≥0.5 serving/d total dairy consumption over time had lower initial dairy consumption and total energy intake than those who maintained a stable consumption or decreased their consumption. Baseline percentage of energy from carbohydrate were higher, whereas the percentage of energy from protein, total fat, and SFA slightly decreased among participants who increased total dairy consumption by ≥0.5 serving/d compared with those who maintained a stable consumption. Furthermore, with increasing total dairy intake over time, intake of whole grains (p = 0.028) and legumes (p = 0.057) tended to be higher. Across all categories of changes in total dairy product consumption, low-fat yogurt and regular cheese were the most consumed dairy products (Supplemental Table 2).
The risk of incident T2D according to changes in total, low-fat, and high-fat dairy consumption are presented in Table 2. After controlling for age, sex, physical activity, change in body mass index, family history of diabetes, and total energy intake, compared with individuals who maintained a stable consumption (±0.50 serving/d), decreased dairy consumption of ≥0.50 servings/d was associated with 56% higher risk of diabetes at the subsequent 3-year follow-up (OR = 1.56; 95% CI: 1.02 to 2.39). This estimate remained similar after further adjusting for dietary factors, including whole grain intake and percentage of energy from protein and carbohydrate (OR = 1.56; 95% CI: 1.02 to 2.41). Increasing total dairy consumption was not associated with T2D risk compared with maintaining stable consumption. Increasing low-fat dairy consumption by 0.50 serving/d was associated with a 44% (OR = 0.56, 95% CI: 0.35 to 0.90) lower risk of T2D compared with maintaining stable consumption. Null associations between decreasing or increasing consumption of high-fat dairy with the risk of T2D were observed.
We further evaluated associations of changes in the consumption of subtypes of dairy products with the risk of T2D (Table 3). Increasing low-fat milk and yogurt consumption was associated with 41% (OR = 0.59, 95% CI: 0.37 to 0.92) and 45% (OR = 0.55, 95% CI 0.33 to 0.93) lower risk of T2D, respectively, than maintaining stable consumption. However, compared with maintaining stable yogurt or low-fat milk consumption, decreasing yogurt and low-fat milk consumption was not associated with T2D risk. Conversely, participants who decreased high-fat milk consumption by ≥0.10 servings/d had a higher risk of T2D (OR = 1.57; 95% CI: 1.02 to 2.41) when compared with individuals who maintained their high-fat milk consumption. Changes in consumption of high-fat yogurt, regular cheese, cream cheese, and ice cream were not associated with T2D risk.
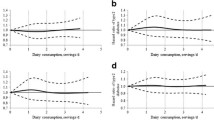
Each increase of 0.5 servings/d in total dairy and low-fat dairy consumption was associated with an 15% (OR = 0.85; 95% CI: 0.77 to 0.94) and 12% (OR = 0.78; 95% CI: 0.65 to 0.95) lower risk of T2D (Fig. 2). Increasing intakes of low-fat milk and yogurt per 0.5 servings/d were significantly associated with a lower risk of T2D. An increase in consumption of cream cheese (0.5 servings/d) was associated with a higher risk of T2D.
Odds ratios and 95% confidence intervals for incident type 2 diabetes, per 0.5-serving/d increase in consumption of various types of dairy during follow-up. The model was adjusted for age, sex, physical activity, change in body mass index, family history of diabetes, total energy intake, whole-grain intake, and energy from protein and carbohydrate
We estimated that replacing 0.5 daily servings of high-fat dairy with 0.5 daily servings of low-fat dairy was associated with 11% lower diabetes risk in the subsequent 3-year follow-up period (Fig. 3). Increasing low-fat yogurt intake by 0.5 servings/day with a simultaneous decrease in high-fat yogurt was associated with a 27% lower risk of T2D. Replacing low-fat milk and low-fat yogurt by 0.5 servings/d with 0.5 servings/d of regular cheese was associated with 66 and 47% higher risk of T2D, respectively. Substitutions of high-fat yogurt for low-fat milk and high-fat milk were associated with a 53 and 37% higher risk of T2D, respectively, per 0.5 serving/d substituted.
Odds ratios and 95% confidence intervals from substitution models for type 2 diabetes associated with increased consumption of a specific dairy product by 0.5 serving/d and concomitantly decreasing consumption of another dairy product by 0.5 serving/d during a 3-y period. The model was adjusted for age, sex, physical activity, change in body mass index, family history of diabetes, total energy intake, whole-grain intake, and energy from protein and carbohydrate
In all sensitivity analyses, excluding subjects with reported outliers, further adjustment for smoking status and concurrent 3-year changes in fruit, legumes intakes, and body weight had small or no impact on the ORs (95%CI) and did not alter the significance of the results (Supplemental Table 3).
Discussion
In this population-based study of individuals with prediabetes, we observed that increasing low-fat dairy consumption was associated with a 44% lower risk of T2D. Consistent inverse associations with the risk of T2D were observed with a 0.5 increase in the consumption of low-fat dairy. Further, we found that replacing 0.5 daily servings of high-fat dairy with low-fat dairy was associated with an 11% lower risk of diabetes. Also, increased low-fat milk and low-fat yogurt consumption were inversely associated with incident T2D. Thus, these findings suggest a potential role of the fat content of dairy foods concerning the development of T2D. This study benefits from a longitudinal design to imitate a large nutritional intervention investigating an aspect of changes in dairy products through a regular diet when individuals were living with prediabetes and in the diabetes development over a long-time period.
Compared with participants who had stable total dairy consumption, participants who decreased their total dairy intake had a 56% higher risk of subsequent incidence of T2D. Each 0.5 serving/d increased in total dairy consumption over 3-year was also associated with a 15% lower risk of subsequent diabetes. In a very recent study of 3 US cohorts of healthy participants, among those with normoglycemia at baseline, participants who decreased their total dairy consumption more than 1 serving/d through a 4-y period had 11% increased risk of T2D, compared with those who had a relatively stable intake [20]. Reducing the intake of total dairy products over time may increase the progression of T2D because dairy foods are being replaced by other, less healthy foods. For instance, those who decrease their dairy intakes may increase the consumption of sugar-sweetened beverages, which could result in a higher risk of T2D.
Although there are other studies supporting a favorable association of total dairy intake with risk of T2D [21,22,23], it seems that some inherent properties of dairy foods may influence their effects on T2D risk, including the type and fat content of the dairy products. Their overall benefit in specific populations may also relate to the general popularity in their consumption, which may differ according to ethnocultural considerations [24]. Regarding the fat content of dairy products, in accordance with previous studies associating low-fat dairy consumption with T2D incidence among apparently healthy individuals [23], we observed that long-term increases in low-fat dairy intake were associated with subsequent lower T2D risk in people with prediabetes. A meta-analysis done by pooling data from observational studies showed that both low-fat and high-fat dairy consumption had no association with the risk of T2D [25]. Although our finding showed a non-significant association between increased high-fat dairy consumption over time and subsequent risk of T2D, results from the Framingham Heart Study Offspring Cohort illustrated that higher consumption of high-fat dairy decreased the risk of incident T2D among prediabetes participants by 70% [14]. Current data from the international cohort of The Prospective Urban Rural Epidemiology (PURE) study has shown that higher consumption of whole-fat (but not low-fat) dairy is associated with a lower risk of T2D compared with no dairy intake [26]. Consistent with our findings, a US cohort study revealed that compared with those stable in their intake, participants who decreased their low-fat dairy intake by > 0.5 daily serving had a higher subsequent risk of T2D, and no significant relationship between high-fat dairy and diabetes was observed [20]. We also estimated that substituting low-fat dairy for high-fat dairy products was favorably associated with the incidence of T2D. Findings from previous study [20] and results from ours highlight the preventive association of low-fat dairy on T2D.
In our analysis, increasing low-fat milk consumption was associated with lower T2D risk relative to the reference category. Furthermore, an increase of 0.5 servings/d in low-fat milk consumption was inversely associated with the risk for T2D. However, there was no significant relationship between high-fat milk and the risk of T2D. Evidence for an association of milk consumption with the risk of T2D is inconsistent. The meta-analysis by Gijsbers et al. [12] indicated that total milk consumption was not associated with T2D risk. Null associations of the total, low- and high-fat milk consumption with incident T2D were also demonstrated in a study of participants with prediabetes [14]. However, a protective association of higher intake of low-fat milk was reported in some studies [27, 28]. A study investigating the association of changes in low-fat milk consumption with the incidence of T2D among normoglycemic subjects indicated that decreasing consumption of low-fat milk was associated with a higher risk of T2D [20].
Fermented dairy products, including yogurt and cheese, may elicit different impacts on the metabolic status of individuals than non-fermented dairy products. Increasing low-fat yogurt over 3 years decreased the risk of T2D by 55% compared with those with relatively stable intake, whereas decreasing high-fat yogurt intake was also associated with benefits. Yogurt consumption, regardless of fat content, was associated with a lower risk of T2D expressed in meta-analyses of prospective cohort studies [12, 28]. A nonlinear association for yogurt consumption was observed with incident T2D among participants with prediabetes, and no additional protective relation was observed with greater than 1–3 servings/week [14]. It was recently illustrated in a pooled analysis of 3 US cohorts that participants decreasing yogurt consumption by > 1.0 serving/d over a 4-y period had an 11% higher risk of T2D when compared to those with stable yogurt consumption [20]. On the other hand, increasing cream cheese consumption over 3 years increased the risk of subsequent T2D in our population; however, increasing the consumption of regular cheeses was not associated with T2D risk. Regarding the association of cheese consumption and T2D, positive [20], inverse [14], and no [29] associations were reported in different cohort studies. These contradictory results between different observational studies might be accounted for by a lack of ability to differentiate among the various types of cheeses, which contain different amounts of fat and sodium. It should be noted that most cheeses, even those with low fat content, contain relatively high amounts of fat, which may increase the amount of SFAs in the diet.
Since increasing consumption over time of low-fat dairy products, including low-fat milk and low-fat yogurt, was associated with a lower risk of T2D, these results highlight the potentially favorable effect of moderate amounts of dairy fat intake on T2D. In this regard, when regular cheese (high-fat content) replaced 0.5 servings/d of low-fat milk or low-fat yogurt over the 3-year period, the the subsequent risk of diabetes increased by 66 and 47%, respectively. Similarly, replacing high-fat yogurt with low-fat milk or low-fat yogurt was associated with lower T2D risk. It should be noted that, except for cream cheese, all substitutions in other types of high-fat dairy had no association with the onset of T2D.
Physiologically, the association between an increase in low-fat dairy and a lower increase in body weight and BMI over time [30] may at least partially account for its association with reduced incident T2D. From a practical standpoint, replacing one type of dairy product for another may be more feasible than substituting for other food groups in a real-life setting. Thus, substituting high-fat dairy products such as cheese with low-fat dairy products such as low-fat milk or low-fat yogurt may be acceptable for patients with prediabetes to prevent the onset of diabetes. However, as dairy fat contains a complex mix of different SFAs with different biological effects and given the pre-existing metabolic states on differential response to the foods [31], further mechanistic studies and prospective studies with substitution models among participants with impaired glucose tolerance are needed to get a complete picture of dairy consumption and T2D risk.
Strengths of this study include that the TLGS cohort is population-based with reasonable representation of the urban population of Tehran [16], and the diagnosis of prediabetes and diabetes was defined based on a drawn fasting blood sample. In addition, we examined the temporality of exposures and outcomes. The FFQ was collected through a careful interview utilizing a photographic method to minimize the impact of recall bias. Furthermore, in this study, baseline characteristics of participants lost to follow-up compared to those followed did not have meaningful differences; thus selection bias is unlikely to have influenced the results.
Several limitations of this investigation need to be mentioned. First, using an FFQ cannot estimate the ‘actual’ intake of participants. For example, cheese is commonly consumed in mixed meals and prepared foods. Second, despite controlling for different covariates in our analysis, residual confounding due to unknown or unmeasured confounders cannot be excluded. Finally, this study was conducted on data from TLGS, which is a homogeneous urban population; thus, results may not be generalizable to other populations, such as rural dwelling or other those with other ethnocultural backgrounds.
Conclusion
In conclusion, in this prospective study of participants with prediabetes, decreasing total dairy consumption was positively associated with incident T2D. Increasing low-fat dairy consumption or replacing high-fat dairy with low-fat products was generally associated with a lower risk of diabetes. Our analysis also suggests that substituting regular cheese for low-fat milk or low-fat yogurt increased the risk of T2D in people with prediabetes.
Availability of data and materials
The data set is the property of Research Institute for Endocrine Sciences (RIES) and is made available upon approval of the research proposal by the research council and the ethics committee. The RIES ethics committee must issue an approval in case of a request for access to the de-identified dataset. Data request may be sent to the head of the RIES Ethics Committee Dr. Azita Zadeh-Vakili at email: azitavakili@endocrine.ac.ir.
Change history
22 December 2021
A Correction to this paper has been published: https://doi.org/10.1186/s12937-021-00754-w
Abbreviations
- FBS:
-
Fasting plasma glucose
- T2D:
-
Type 2 diabetes
- TLGS:
-
Tehran Lipid and Glucose Study
- OR:
-
Odds ratio
- IFG:
-
Impaired fasting glucose
- 2-hPG:
-
2-h plasma glucose
- FFQ:
-
Food frequency questionnaire
References
Ferrannini E, Gastaldelli A, Iozzo P. Pathophysiology of prediabetes. Med Clin. 2011;95(2):327–39.
Grundy SM. Pre-diabetes, metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol. 2012;59(7):635–43.
Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR, Pratley R, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30(3):753–9.
Hostalek U. Global epidemiology of prediabetes - present and future perspectives. Clin Diabetes Endocrinol. 2019;5:5.
Hadaegh F, Derakhshan A, Zafari N, Khalili D, Mirbolouk M, Saadat N, et al. Pre-diabetes tsunami: incidence rates and risk factors of pre-diabetes and its different phenotypes over 9 years of follow-up. Diabet Med. 2017;34(1):69–78.
Aguiree F, Brown A, Cho NH, Dahlquist G, Dodd S, Dunning T, et al. IDF diabetes atlas. 2013.
Roncero-Ramos I, Alcala-Diaz JF, Rangel-Zuniga OA, Gomez-Delgado F, Jimenez-Lucena R, Garcia-Rios A, et al. Prediabetes diagnosis criteria, type 2 diabetes risk and dietary modulation: the CORDIOPREV study. Clin Nutr (Edinburgh, Scotland). 2020;39(2):492–500.
Heaney RP. Dairy intake, dietary adequacy, and lactose intolerance. Adv Nutr. 2013;4(2):151–6.
Mozaffarian D, Wu JH. Flavonoids, dairy foods, and cardiovascular and metabolic health: a review of emerging biologic pathways. Circ Res. 2018;122(2):369–84.
Yakoob MY, Shi P, Willett WC, Rexrode KM, Campos H, Orav EJ, et al. Circulating biomarkers of dairy fat and risk of incident diabetes mellitus among men and women in the United States in two large prospective cohorts. Circulation. 2016;133(17):1645–54.
Alvarez-Bueno C, Cavero-Redondo I, Martinez-Vizcaino V, Sotos-Prieto M, Ruiz JR, Gil A. Effects of milk and dairy product consumption on type 2 diabetes: overview of systematic reviews and meta-analyses. Adv Nutr. 2019;10(suppl_2):S154–S63.
Gijsbers L, Ding EL, Malik VS, De Goede J, Geleijnse JM, Soedamah-Muthu SS. Consumption of dairy foods and diabetes incidence: a dose-response meta-analysis of observational studies. Am J Clin Nutr. 2016;103(4):1111–24.
Moslehi N, Shab-Bidar S, Mirmiran P, Sadeghi M, Azizi F. Associations between dairy products consumption and risk of type 2 diabetes: Tehran lipid and glucose study. Int J Food Sci Nutr. 2015;66(6):692–9.
Hruby A, Ma J, Rogers G, Meigs JB, Jacques PF. Associations of dairy intake with incident prediabetes or diabetes in middle-aged adults vary by both dairy type and glycemic status. J Nutr. 2017;147(9):1764–75.
Slurink IAL, Soedamah-Muthu SS. Dairy consumption and cardiometabolic risk: advocating change on change analyses. Am J Clin Nutr. 2020;111(5):944–5.
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid And Glucose Study phase II. Trials. 2009;10(1):5.
Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 2010;13(5):654–62.
Esfahani FH, Asghari G, Mirmiran P, Azizi F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran Lipid and Glucose Study. J Epidemiol. 2010;20(2):150–8.
Laursen ASD, Sluijs I, Boer JM, Verschuren WM, Van Der Schouw YT, Jakobsen MU. Substitutions between dairy products and risk of stroke: results from the European investigation into cancer and nutrition-Netherlands (EPIC-NL) cohort. Br J Nutr. 2019;121(12):1398–404.
Drouin-Chartier JP, Li Y, Ardisson Korat AV, Ding M, Lamarche B, Manson JE, et al. Changes in dairy product consumption and risk of type 2 diabetes: results from 3 large prospective cohorts of US men and women. Am J Clin Nutr. 2019;110(5):1201–12.
Mishali M, Prizant-Passal S, Avrech T, Shoenfeld Y. Association between dairy intake and the risk of contracting type 2 diabetes and cardiovascular diseases: a systematic review and meta-analysis with subgroup analysis of men versus women. Nutr Rev. 2019;77(6):417–29.
Tong X, Dong JY, Wu ZW, Li W, Qin LQ. Dairy consumption and risk of type 2 diabetes mellitus: a meta-analysis of cohort studies. Eur J Clin Nutr. 2011;65(9):1027–31.
Liu S, Choi HK, Ford E, Song Y, Klevak A, Buring JE, et al. A prospective study of dairy intake and the risk of type 2 diabetes in women. Diabetes Care. 2006;29(7):1579–84.
Wang Y, Li S. Worldwide trends in dairy production and consumption and calcium intake: is promoting consumption of dairy products a sustainable solution for inadequate calcium intake? Food Nutr Bull. 2008;29(3):172–85.
Chen M, Sun Q, Giovannucci E, Mozaffarian D, Manson JE, Willett WC, et al. Dairy consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. BMC Med. 2014;12(1):215.
Bhavadharini B, Dehghan M, Mente A, Rangarajan S, Sheridan P, Mohan V, et al. Association of dairy consumption with metabolic syndrome, hypertension and diabetes in 147 812 individuals from 21 countries. BMJ Open Diabetes Res Care. 2020;8(1):e000826.
Gao D, Ning N, Wang C, Wang Y, Li Q, Meng Z, et al. Dairy products consumption and risk of type 2 diabetes: systematic review and dose-response meta-analysis. PLoS One. 2013;8(9):e73965.
Aune D, Norat T, Romundstad P, Vatten LJ. Dairy products and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Am J Clin Nutr. 2013;98(4):1066–83.
Díaz-López A, Bulló M, Martínez-González MA, Corella D, Estruch R, Fitó M, et al. Dairy product consumption and risk of type 2 diabetes in an elderly Spanish Mediterranean population at high cardiovascular risk. Eur J Nutr. 2016;55(1):349–60.
Trichia E, Luben R, Khaw KT, Wareham NJ, Imamura F, Forouhi NG. The associations of longitudinal changes in consumption of total and types of dairy products and markers of metabolic risk and adiposity: findings from the European Investigation into Cancer and Nutrition (EPIC)-Norfolk study, United Kingdom. Am J Clin Nutr. 2020;111(5):1018–26.
Kim Y, Keogh JB, Clifton PM. Differential effects of red meat/refined grain diet and dairy/chicken/nuts/whole grain diet on glucose, insulin and triglyceride in a randomized crossover study. Nutrients. 2016;8(11):687.
Acknowledgements
We express our appreciation to the participants of the study for their enthusiastic support and to the staff of the involved hospitals for their valuable help.
Funding
This work was funded by a Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. There was no additional external funding received for this study.
Author information
Authors and Affiliations
Contributions
E.Y. conceptualized and designed the study, analyzed and interpreted the data, prepared the manuscript and approved the final manuscript as submitted. G.A. designed the study and drafted the initial manuscript, and approved the final manuscript as submitted. C.C. interpreted the data and critically revised the manuscript and approved the final manuscript as submitted. P.M. supervised the project, drafted the initial manuscript, and approved the final manuscript as submitted. F.A. supervised the project, critically revised the manuscript and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants signed a written, informed consent form. The protocol was approved by the ethics committee of the Research Institute for Endocrine Sciences (IR.SBMU.ENDOCRINE.REC.1399.057), in compliance with the principles of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
On behalf of all authors, the corresponding author hereby declares that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table 1. A comparison of baseline characteristics between participants followed and those lost to follow-up.
Additional file 2:
Supplementary Table 2. Initial intake and changes in consumption of subtypes of dairy products over a 3-year follow-up.
Additional file 3:
Supplementary Table 3. Sensitivity analysis: Multivariable adjusted odds ratios (95% confidence intervals) for incident type 2 diabetes according to categories changes in total, low-fat, and high-fat dairy consumption.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yuzbashian, E., Asghari, G., Mirmiran, P. et al. Changes in dairy product consumption and subsequent type 2 diabetes among individuals with prediabetes: Tehran Lipid and Glucose Study. Nutr J 20, 88 (2021). https://doi.org/10.1186/s12937-021-00745-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-021-00745-x