Abstract
Background
Inconsistent associations between egg consumption and cardiovascular disease (CVD) risk have been observed in previous studies. This study aims to longitudinally investigate the association between egg consumption and altered risk of arterial stiffness, a major pre-clinical pathogenic change of CVD, which was assessed by brachial-ankle pulse wave velocity (baPWV).
Methods
A total of 7315 Chinese participants from the Kailuan Study, free of CVD and cancer were included in this study. Egg consumption was assessed by a semi-quantitative validated food frequency questionnaire in 2014. baPWV was repeatedly measured at baseline and during follow-up (mean follow-up: 3.41 years). General linear regression was used to calculate means of baPWV change rate across different egg consumption groups, adjusting for age, sex, baseline baPWV, healthy eating index, total energy, social-economic status, blood pressure, obesity, smoking, lipid profiles, and fasting glucose concentrations.
Results
Compared to the annual baPWV change rate in participants with 0–1.9 eggs/wk. (adjusted mean: 35.9 ± 11.2 cm/s/y), those consuming 3–3.9 eggs/wk. (adjusted mean: 0.2 ± 11.4 cm/s/y) had the lowest increase in baPWV during follow-up (P-difference = 0.002). Individuals with low (0–1.9 eggs/wk) vs. high (5+ eggs /wk) egg intake showed similar changes in baPWV.
Conclusions
In this large-scale longitudinal analysis, we did not find a significant difference in arterial stiffness, as assessed by baPWV level, between low and high egg consumption groups. However, moderate egg consumption (3–3.9 eggs/wk) appeared to have beneficial effects on arterial stiffness.
Similar content being viewed by others
Background
Eggs are a type of inexpensive, nutrient-dense food, an excellent source of protein, and a good source of lutein/zeaxanthin, vitamins, and minerals [1]. Eggs are also high in other biologically active compounds with antimicrobial, immunomodulatory, antioxidant, anti-cancer properties. Besides, egg protein has the highest biological value for providing essential amino acids that stimulate skeletal muscle synthesis [2]. Eggs are also one of the major sources of dietary cholesterol in the human diet [3]. A meta-analysis with 55 studies reported that high dietary cholesterol intake was associated with elevated serum cholesterol [4]. A recent Chinese study also reported that high dietary cholesterol intake was associated with hypercholesterolemia [5]. However, inconsistent associations between egg consumption and CVD risk have been observed in previous studies, and no clear association between egg consumption and cardiovascular disease (CVD) risk has been established. Several recent systematic reviews and meta-analyses showed no significant association between egg consumption and CVD mortality [6, 7] or altered status of CVD risk factors [8, 9]. In contrast, a recent pooled analysis of prospective study reported that each additional 0.5 egg/day consumption was associated with a 6% higher risk of CVD and 8% higher risk of all-cause mortality [10].
With the purpose of better understanding the relation between egg consumption and CVD, it is important to understand whether egg intake is associated with altered risk of major pre-clinical pathogenic progressions of CVD. Arterial stiffness is recognized as an important consequence of aging that has been shown to provoke deleterious vascular phenotypes in diseases such as diabetes [11], atherosclerosis [12], kidney dysfunction [13], and cognitive impairment [14]. Pulse wave velocity (PWV) is currently considered the gold standard in the evaluation of arterial stiffness [15]. PWV assesses the velocity of the blood pressure wave as it travels a known distance between two anatomic sites within the arterial system, and indicates the elasticity and other properties of the artery [16]. Arterial stiffness, as assessed by Brachial-ankle pulse wave velocity (baPWV), has been shown to be associated with subsequent CVD risk and having lower PWV at mid-life was associated with a lower risk of developing age-related CVD risk [17]. We, thus, conducted analysis with data from a large-scale longitudinal study, to examine whether egg intake was associated with the change in PWV during 3 years of follow-up, in 7315 adults without CVD.
Methods
Study population
The data utilized are from the Kailuan Study, a population-based prospective cohort launched in 2006 in Tangshan, China (The Chinese Clinical Trial Registry #: ChiCTR-TNRC-1101489). Participants recruited in the study were followed via biennial face-to-face physical examination, anthropometry, laboratory assessment, and annual comprehensive surveillance of medical records and death certificates, as detailed previously [12, 18, 19].
BaPWV measurement was introduced into the testing routine in 2010 and repeatedly measured in later rounds for a sub-cohort of the Kailuan study, as described previously [12, 20]. BaPWV was measured for each participant at least twice between 2010 and 2016 and the interval between two measurements was more than 3 months. (mean difference between two assessments = 3.41 years). Dietary data were collected in 2014 (baseline for the current analysis), and 8638 participants aged 22 years or older (mean age: 48.6 ± 10.8 years) had completed dietary information and two baPWV assessments at and after the baseline. We further excluded 336 participants with CVD or cancer and 987 participants with energy intake out of range (for men, < 800 kcal/d or > 4000 kcal/d; for women < 500 kcal/d or > 3500 kcal/d; Fig. 1), leaving a total of 7315 participants in the current analysis. The primary outcome variable was the longitudinal change in baPWV (mean follow-up: 3.41 years; interquartile range:1.99–5.13 years). In the secondary analysis for incident arterial stiffness, 3865 participants without arterial stiffness (baPWV< 1400 cm/s) at baseline were included. The study was performed according to the guidelines of the Helsinki Declaration and was approved by the Ethics Committee of the Kailuan General Hospital.
Assessment of egg consumption and other dietary components
In 2014, a 40-item (33 food items and 7 condiments) semi-quantitative food frequency questionnaire was used to collect possible food items participants consumed, which was validated in the Chinese population previously [21]. The food frequency questionnaire was administered along with other assessments during the face-to-face interview [14]. For each food item, participants were asked to provide information regarding the frequency (never, daily, weekly, or monthly) and quantity (liangs, 1 liang =50 g) of their consumption.
Specifically, a question regarding egg consumption was included in this food frequency questionnaire: “Based on your recent 1-year diet, do you usually eat egg including chicken egg, duck egg, etc.?” Participants answered this question by selecting the following options, “very often, __times/day”, “often, __times/week”, “sometimes, __times/month”, “never” and participants were then asked to provide how many eggs they consumed each time, on average. Based on self-reported egg consumption, we grouped the participants into 5 categories (0–1.9, 2–2.9, 3–3.9, 4–4.9, or ≥ 5 eggs/wk).
Overall diet quality, a potential confounder that might be associated with both egg consumption and arterial stiffness status, was evaluated via the dietary approaches to stop hypertension (DASH) score. The DASH score was focused on food and nutrients emphasized or minimized in the DASH diet, including nine components: vegetables, fruit, dairy, beans, whole grains, meat, fat, sodium, and sweetened beverage. Component scores were assigned to each participant quintile according to their intake ranking. As for vegetables, fruits, dairy, beans, and whole grains, the highest intake ranking quintile was assigned five points and the lowest intake ranking quintile was assigned one point. For sodium, meat, fat, and beverage, the lowest quintile was given a score of five points and the highest quintile was considered as one point. We then summed up the component scores to obtain an overall DASH score ranging from 9 to 45 [22, 23].
Measurement of arterial stiffness
Arterial stiffness status was assessed at baseline and follow-up (mean 3.41y) using baPWV, which has been used in Asian populations [12, 24] and has previously been described [12, 20]. Briefly, participants were asked to refrain from smoking and to rest for at least 5 min before the measurement of baPWV. Cuffs were placed on both the brachial area of the arm and the ankle to assess the pulse transit time which is defined as the travel time of the pulse wave from brachia to ankle. In our study, baPWV was measured with a BP-203RPEIII networked arteriosclerosis detection device (OMRON Healthcare (China) Co., LTD.). The measurement was repeated twice at each visit to ensure accuracy, and the baPWV value was read by trained health professionals. Therefore, in this study, arterial stiffness was noted using a cut-off point of baPWV ≥1400 cm/s [17].
Assessment of covariates
Baseline information was assessed with a validated questionnaire, administered in a face-to-face interview. The questionnaire included basic information (e.g. age, sex, marriage status, education level, smoking status, and occupation). Physical activity was assessed with the International Physical Activity Questionnaire (IPAQ) short form, which assesses the duration and frequency of sitting, walking, moderate-intensity activities, and vigorous-intensity activities, and has been validated in the Chinese population [25, 26].
Height, weight, and blood pressure were measured by trained health professionals, as detailed previously [12]. Body Mass Index was calculated as weight, in kilograms, divided by height, in meters, squared. Blood samples were collected the morning after a minimum of 8 h of fasting. Fasting blood glucose (FBG), high-density lipoprotein cholesterol (HDL-c), and low-density lipoprotein cholesterol (LDL-c) were measured in the central lab, Kailuan General Hospital, as previously described [12].
Statistical analysis
All statistical analyses were performed in SAS version 9.4 (SAS Institute Inc., USA), and all tests were two-sided. ANOVA was used to calculate continuous variables and Chi-square was used to calculate categorical variables for baseline characteristics among participants. In the primary analysis, we compared the rate of longitudinal change in baPWV across egg consumption groups. Change in baPWV was calculated as the difference of baPWV measurements (cm/s) between two visits divided by the time interval (years). General linear model regression was used to calculate the adjusted means of baPWV change rate in each group. Model 1 adjusted for age, sex, baseline baPWV, total energy intake, and DASH score; model 2 further adjusted for physical activity, marriage, employment, education level, alcohol use, smoking status, and heart rate; and model 3 further adjusted for systolic blood pressure, FBG, LDL-c, HDL-c. The same model was used to calculate adjusted means of baPWV change rate in each group after further adjusted for other blood pressure indices, DBP, MAP, and PP.
We further tested interactions between egg consumption and covariates in the fully adjusted model.
In the secondary analyses, we examined egg consumption and the risk of developing arterial stiffness during the follow-up among participants who were free of arterial stiffness at baseline. Cox proportional hazard models were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs), after adjusting for the aforementioned covariates.
Results
Compared to participants with low egg intake (< 2 eggs/ wk), participants with higher egg intake were more likely to be current smokers, have higher DASH scores and higher degree of education, but lower physical activity (Table 1). There were significant differences in age, total energy intake, and biomarkers crossing every group.
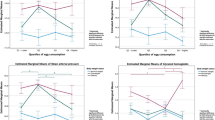
Compared to the participants consuming 0–1.9 eggs/wk., participants consuming 3–3.9 eggs/wk. had the lowest increment in baPWV during follow-up (Table 2). In the final model, the difference in baPWV change rate between this group (adjusted mean: 0.2 ± 11.4 cm/s per year) and the group with consumption of 0–1.9 eggs/wk. (35.9 ± 11.2 cm/s per year) was significant (P-difference = 0.002). Similar results were observed when restricting to participants without arterial stiffness at baseline (Table 2). Further adjustment for other blood pressure indices, such as diastolic blood pressure, mean arterial pressure, and pulse pressure, did not materially change observed results (supplementary Table 1). There was no significant association between egg consumption and the risk of developing arterial stiffness (Table 3). None of the interactions between egg consumption and age, sex, BMI, total energy intake, DASH score, smoking status, alcohol consumption, physical activity level, SBP, LDL, FBG, and heart rate in relation to baPWV change rate were significant (p for interaction≥0.05 for all).
Discussion
In this longitudinal community-based study, individuals with low (< 2 eggs/wk) vs. high (5+ eggs /wk) egg intake showed similar changes in baPWV and risk of developing arterial stiffness over a mean 3.41 y follow-up. Interestingly, those with egg consumption of 3–3.9/wk. experienced the slowest aging-related increment in baPWV during the follow-up, among all participants, independent of age, sex, overall diet quality, and health status. In this study, we showed an average lower increase in baPWV of 35.7 cm/s per year between the moderate and lowest egg consumption groups, which amounted to ~ 122 cm/s over 3.41 years of follow-up. The difference in accumulated change may be associated with ~ 8% higher risk of CVD, based on a recent meta-analysis [27].
To the best of our knowledge, this study is the first to examine the association between egg consumption and arterial stiffness in a community-based population without CVD. The non-significant difference in baPWV status between two extreme egg consumption categories is consistent with previous systematic reviews and meta-analyses regarding egg intake and mortality, CVD risk, and CVD biomarkers. A recent meta-analysis reported a non-significant difference, for high (7+/wk) vs low (< 1/wk) egg consumption, for death due to ischemic heart disease, ischemic stroke, and hemorrhagic stroke [7]. Similar results were reported in another meta-analysis of egg consumption and total and cause-specific mortality [6]. A systematic review concluded that high-quality intervention studies have found nonsignificant effects of increasing the consumption of eggs on risk markers for CVD and type 2 diabetes in healthy subjects and type 2 diabetic subjects [27]. Another two recent meta-analyses of randomized controlled trials also reported non-differential effects of egg consumption (> 4/wk) on inflammation [9], blood pressure [8], and lipid profiles [8] compared to egg consumption ≤4 eggs/week. In contrast, a recent pooled study based on 6 US cohorts reported that higher egg intake was associated with higher CVD incidence and all-cause mortality [10]. However, there was no significant difference when comparing individuals who consumed < 1 egg/d with those with no egg consumption [10].
We found that participants with modest egg consumption (3–3.9/wk) had a significantly lower age-related increment in baPWV across all egg consumption groups. Of note, when the binary variable of arterial stiffness was used as the outcome, a similar trend was observed, but it became non-significant. Several previous studies have reported a low risk of CVD and mortality being associated with modest egg consumption. For example, in a recent prospective study including 146,011 individuals from 21 countries, those who consumed 3–4.9 eggs/wk. had the lowest risk of mortality and CVD across all egg consumption groups [28]. In this study, compared to egg consumption < 1 egg/wk., 3–4.9 eggs/wk. had lower risks of mortality and CVD. In contrast, the difference in risk of mortality and/or CVD was not significant for 5 + eggs /wk. vs < 1 egg/wk. [28]. In a prospective study in Sweden, individuals consuming 3–6 eggs/wk. had the lowest risk for heart failure, myocardial infarction, and hemorrhagic stroke, but not ischemic stroke, across all egg consumption groups, although the difference was not significant [29]. A similar non-significant U-shaped trend was also observed for the association between eggs and total mortality [4, 5, 27, 30].
Arterial stiffness is the stiffening of the blood vessel wall. When the blood vessel loses its elasticity, its ability to control the blood flow is compromised. The blood vessel needs more force to push blood through, which increases the pulse pressure and may introduce damage to the blood vessels [31]. Eggs, as a type of nutrient-dense food, are an accessible source of L-arginine, vitamin D, vitamin K, choline, and xanthophyll carotenoids, specifically lutein and zeaxanthin [3], which have been shown to be protective against arterial stiffness. The amino acid, L-arginine, is a precursor of nitric oxide. Nitric oxide inhibits the expression of adhesion and further improves endothelial function [32, 33]. Endothelial dysfunction is a risk factor for arterial stiffness [34, 35]. Therefore, modest egg consumption might be potentially protective from endothelial dysfunction and arterial stiffness. Xanthophyll carotenoids, lutein and zeaxanthin, and choline have been shown to decrease inflammation [36,37,38]. However, choline is also a source for trimethylamine-N-oxide, which has been shown to be associated with a high risk of atherosclerosis and other cardiovascular events [39, 40]. On the other hand, eggs are a major source of dietary cholesterol and saturated fat [3]. A previous meta-analysis showed that high egg consumption was associated with elevated serum cholesterol, [4] a potential risk factor for arterial stiffness [41, 42]. High saturated fat intake has also been associated with high aortic pulse wave velocity [43]. Given both positive and negative nutritional components in eggs, it is not surprising that our result, and others, appears to be non-linear, with modest, but not low, egg consumption associated with the desired health outcome. However, further studies are needed to confirm this association.
However, given the lack of consistency in findings, more research is needed. As a majority of existing studies were conducted in western countries, more investigations at various geographic areas are necessary. This will be beneficial for future meta-analyses.
This study has some limitations. Egg consumption was assessed with a single self-reported question, which may introduce measurement error (misclassification) or recall bias. Undifferentiated misclassification could bias toward the null. In this study, total energy intake was likely to be underestimated due to the small number of food items in the food frequency questionnaire, which might miss some important foods. Thus, total energy intake was adjusted as a covariate in all multiple regression models in order to reduce the influence of this systematic error. Because this study is a preliminary study, the follow-up (mean 3.41 years) is relatively short, which is another limitation. Because the majority of participants were in the 4–4.9 eggs/wk. group, the sample size in the extreme categories was small, which may limit the statistical power to detect small-to-moderate effects. The study population is localized, and the observed results may not generalize to other ethnic groups with different eating habits and social economic backgrounds. Only 2406 women were included in the analysis and the menopausal status was not assessed in our questionnaire, which is also one of the major limitations.
Conclusions
In conclusion, in this large-scale longitudinal analysis, we did not find a significant difference in arterial stiffness, as assessed by baPWV level, between low and high egg consumption groups (0–1.9/wk. vs. ≥ 5/wk). However, moderate egg consumption (3–3.9 eggs/wk) appeared to have beneficial effects on arterial stiffness. Further studies, investigating the association between egg consumption and arterial stiffness with longer follow-up years and more women participants, are warranted to replicate our findings.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CVD:
-
Cardiovascular diseases
- PWV:
-
Pulse wave velocity
- baPWV:
-
Brachial-ankle pulse wave velocity
- mHEI-2015:
-
Modified healthy eating index 2015
- IPAQ:
-
International physical activity questionnaire
- FBG:
-
Fasting blood glucose
- HDL-c:
-
High-density lipoprotein cholesterol
- LDL-c:
-
Low-density lipoprotein cholesterol
- HRs:
-
Hazard ratios
- CIs:
-
Confidence intervals
- T2D:
-
Type 2 diabetes
- DBP:
-
Diastolic blood pressure
- MAP:
-
Mean arterial pressure
- PP:
-
Pulse pressure
References
U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020. Available at DietaryGuidelines.gov.
Miranda JM, Anton X, Redondo-Valbuena C, Roca-Saavedra P, Rodriguez JA, Lamas A, Franco CM, Cepeda A. Egg and egg-derived foods: effects on human health and use as functional foods. Nutrients. 2015;7(1):706–29. https://doi.org/10.3390/nu7010706.
US Department of Agriculture. Agricultural Research Service, Nutrient Data Laboratory. USDA National Nutrient Database for Standard Reference, Release 28; 2015. https://ndb.nal.usda.gov/ndb/; 2015 [accessed 17 August 2020].
Vincent MJ, Allen B, Palacios OM, Haber LT, Maki KC. Meta-regression analysis of the effects of dietary cholesterol intake on LDL and HDL cholesterol. Am J Clin Nutr 2019;109:7–16. https://doi.org/https://doi.org/10.1093/ajcn/nqy273, 1.
Huang, Q., Jiang, H., Zhang, B., Wang, H., Jia, X., Huang, F., Wang, L., & Wang, Z. (2019). Threshold-effect Association of Dietary Cholesterol Intake with dyslipidemia in Chinese adults: results from the China health and nutrition survey in 2015. Nutrients, 11(12), 2885. https://doi.org/https://doi.org/10.3390/nu11122885.
Mazidi M, Katsiki N, Mikhailidis DP, Pencina MJ, Banach M. Egg consumption and risk of Total and cause-specific mortality: An individual-based cohort study and pooling prospective studies on behalf of the lipid and blood pressure meta-analysis collaboration (LBPMC) group. J Am Coll Nutr 2019;38:552–563. https://doi.org/https://doi.org/10.1080/07315724.2018.1534620, 6.
Xu L, Lam TH, Jiang CQ, Zhang WS, Zhu F, Jin YL, Woo J, Cheng KK, Thomas GN Egg consumption and the risk of cardiovascular disease and all-cause mortality: Guangzhou biobank cohort study and meta-analyses. Eur J Nutr 2019;58:785–796. https://doi.org/https://doi.org/10.1007/s00394-018-1692-3, 2.
Wang MX, Wong CH, Kim JE. Impact of whole egg intake on blood pressure, lipids and lipoproteins in middle-aged and older population: a systematic review and meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis 2019;29:653–664. https://doi.org/https://doi.org/10.1016/j.numecd.2019.04.004, 7.
Sajadi Hezaveh, Z., Sikaroudi, M. K., Vafa, M., Clayton, Z. S., & Soltani, S. (2019). Effect of egg consumption on inflammatory markers: a systematic review and meta-analysis of randomized controlled clinical trials. J Sci Food Agric, 99(15), 6663–6670. https://doi.org/https://doi.org/10.1002/jsfa.9903.
Zhong VW, Van Horn L, Cornelis MC, et al. Associations of dietary cholesterol or egg consumption with incident cardiovascular disease and mortality. JAMA. 2019;321:1081–1095. https://doi.org/https://doi.org/10.1001/jama.2019.1572, 11.
Muhammad, I. F., Borné, Y., Östling, G., Kennbäck, C., Gottsäter, M., Persson, M., Nilsson, P. M., & Engström, G. (2017). Arterial stiffness and incidence of diabetes: a population-based cohort study. Diabetes Care, 40(12), 1739–1745. https://doi.org/https://doi.org/10.2337/dc17-1071.
Wu S, Jin C, Li S, Zheng X., Zhang X., Cui L., Gao X. Aging, arterial stiffness, and blood pressure Association in Chinese Adults. Hypertension. 2019;73:893–899. https://doi.org/https://doi.org/10.1161/HYPERTENSIONAHA.118.12396, 4.
Sedaghat, S., Mattace-Raso, F. U., Hoorn, E. J., Uitterlinden, A. G., Hofman, A., Ikram, M. A., Franco, O. H., & Dehghan, A. (2015). Arterial stiffness and decline in kidney function. Clinical journal of the American Society of Nephrology : CJASN, 10(12), 2190–2197. https://doi.org/https://doi.org/10.2215/CJN.03000315.
Li X, Lyu P, Ren Y, An J, Dong Y. Arterial stiffness and cognitive impairment. J Neurol Sci. 2017;380:1–10. https://doi.org/10.1016/j.jns.2017.06.018 Epub 2017 Jun 27. PMID: 28870545.
Mancia, G., Fagard, R., Narkiewicz, K., Redón, J., Zanchetti, A., Böhm, M., Christiaens, T., Cifkova, R., De Backer, G., Dominiczak, A., Galderisi, M., Grobbee, D. E., Jaarsma, T., Kirchhof, P., Kjeldsen, S. E., Laurent, S., Manolis, A. J., Nilsson, P. M., Ruilope, L. M., Schmieder, R. E., … Task Force Members (2013). 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens, 31(7), 1281–1357. https://doi.org/https://doi.org/10.1097/01.hjh.0000431740.32696.cc.
Miyatani M, Masani K, Oh PI, Miyachi M, Popovic MR, Craven BC. Pulse wave velocity for assessment of arterial stiffness among people with spinal cord injury: a pilot study. J Spinal Cord Med 2009;32:72–78. https://doi.org/https://doi.org/10.1080/10790268.2009.11760755, 1.
Yamashina A, Tomiyama H, Arai T, et al. Brachial-ankle pulse wave velocity as a marker of atherosclerotic vascular damage and cardiovascular risk. Hypertens Res 2003;26:615–622. https://doi.org/https://doi.org/10.1291/hypres.26.615, 8.
Wu S, An S, Li W, et al. Association of trajectory of cardiovascular health score and incident cardiovascular disease. JAMA Netw Open. 2019;2:e194758. https://doi.org/10.1001/jamanetworkopen.2019.4758.
Jin C, Chen S, Vaidya A, et al. Longitudinal change in fasting blood glucose and myocardial infarction risk in a population without diabetes. Diabetes Care. 2017;40:1565–72. https://doi.org/10.2337/dc17-0610.
Zheng X, Jin C, Liu Y, et al. Arterial stiffness as a predictor of clinical hypertension. J Clin Hypertens (Greenwich). 2015;17:582–91. https://doi.org/10.1111/jch.12556.
Li Y, Song J, Pan H, Yao M, Hu X, Ma G. Validity of food frequency questionnaire to investigate the dietary energy and nutrients intake. Ying Yang Xue Bao. 2006;28:143–7.
Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168(7):713–20. https://doi.org/10.1001/archinte.168.7.713.
Your Guide to Lowering Your Blood Pressure with DASH: DASH eating plan: lower your blood pressure. Bethesda: Dept. of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute; 2006.
Chen S, Li W, Jin C, Vaidya A, Gao J, Yang H, Wu S, Gao X. Resting heart rate trajectory pattern predicts arterial stiffness in a community-based Chinese cohort. Arterioscler Thromb Vasc Biol. 2017;37(2):359–64. https://doi.org/10.1161/ATVBAHA.116.308674.
The IPAQ Group. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ) – Short and Long Forms Contents. 2015. http://www.ipaq.ki.se/.
Deng HB, Macfarlane DJ, Thomas GN, et al. Reliability and validity of the IPAQ-Chinese: the Guangzhou Biobank Cohort Study. Med Sci Sports Exerc. 2008;40:303–7. https://doi.org/10.1249/mss.0b013e31815b0db5.
Ohkuma T, Ninomiya T, Tomiyama H, et al. Brachial-ankle pulse wave velocity and the risk prediction of cardiovascular disease: an individual participant data meta-analysis. Hypertension. 2017;69:1045–52. https://doi.org/10.1161/HYPERTENSIONAHA.117.09097.
Dehghan M, Mente A, Rangarajan S, Mohan V, Lear S, Swaminathan S, et al. Associations of intake with blood lipids, cardiovascular disease, and mortality in 177,000 people in 50 countries. Am J Clin Nutr. 2020;pii:nqz348. https://doi.org/10.1093/ajcn/nqz348. [Epub ahead of print].
Larsson SC, Åkesson A, Wolk A. Egg consumption and risk of heart failure, myocardial infarction, and stroke: results from 2 prospective cohorts. Am J Clin Nutr. 2015;102:1007–13. https://doi.org/10.3945/ajcn.115.119263.
Schwingshackl L, Schwedhelm C, Hoffmann G, et al. Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr. 2017;105:1462–73. https://doi.org/10.3945/ajcn.117.153148.
Shirwany, N. A., & Zou, M. H. (2010). Arterial stiffness: a brief review. Acta Pharmacol Sin, 31(10), 1267–1276. https://doi.org/https://doi.org/10.1038/aps.2010.123.
Siasos, G., Tousoulis, D., Antoniades, C., Stefanadi, E., & Stefanadis, C. (2007). L-arginine, the substrate for NO synthesis: an alternative treatment for premature atherosclerosis?. Int J Cardiol, 116(3), 300–308. https://doi.org/https://doi.org/10.1016/j.ijcard.2006.04.062.
Tousoulis, D., Böger, R. H., Antoniades, C., Siasos, G., Stefanadi, E., & Stefanadis, C. (2007). Mechanisms of disease: L-arginine in coronary atherosclerosis--a clinical perspective. Nature clinical practice. Cardiovascular medicine, 4(5), 274–283. https://doi.org/https://doi.org/10.1038/ncpcardio0878.
Anderson T. J. Arterial stiffness or endothelial dysfunction as a surrogate marker of vascular risk. The Canadian journal of cardiology, 22 Suppl B(Suppl B), 72B–80B. https://doi.org/10.1016/s0828-282x(06)70990-4.
Duprez D. A. (2010). Arterial stiffness and endothelial function: key players in vascular health. Hypertension, 55(3), 612–613. https://doi.org/10.1161/HYPERrTENSIONAHA.109.144725.
Mayer O Jr, Seidlerová J, Wohlfahrt P, Filipovský J., Cífková R., Černá V., Kučerová A., Pešta M., Fuchsová R., Topolčan O., Jardon K.M.C., Drummen N.E.A., Vermeer C. Synergistic effect of low K and D vitamin status on arterial stiffness in a general population. J Nutr Biochem 2017;46:83–89. https://doi.org/https://doi.org/10.1016/j.jnutbio.2017.04.010.
Kim JE, Leite JO, DeOgburn R, Smyth JA, Clark RM, Fernandez ML. A lutein-enriched diet prevents cholesterol accumulation and decreases oxidized LDL and inflammatory cytokines in the aorta of Guinea pigs. J Nutr 2011;141:1458–1463. https://doi.org/https://doi.org/10.3945/jn.111.141630, 8.
Detopoulou P, Panagiotakos DB, Antonopoulou S, Pitsavos C, Stefanadis C. Dietary choline and betaine intakes in relation to concentrations of inflammatory markers in healthy adults: the ATTICA study. Am J Clin Nutr 2008;87:424–430. https://doi.org/https://doi.org/10.1093/ajcn/87.2.424, 2.
Miller CA, Corbin KD, da Costa KA, Zhang S, Zhao X, Galanko JA, Blevins T, Bennett BJ, O’Connor A, Zeisel SH Effect of egg ingestion on trimethylamine-N-oxide production in humans: a randomized, controlled, dose-response study. Am J Clin Nutr 2014;100:778–786. https://doi.org/10.3945/ajcn.114.087692, 3.
Tang WH, Wang Z, Levison BS, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med 2013;368:1575–1584. https://doi.org/https://doi.org/10.1056/nejmoa1109400, 17.
R. O. Alvim, J. Mourão, G. L. Magalhães et al. Non-HDL cholesterol is a good predictor of the risk of increased arterial stiffness in postmenopausal women in an urban Brazilian population. Clinics. 2017;72:106–110. http://dx.doi.org/https://doi.org/10.6061/clinics/2017(02)07
Zhao W, Gong W, Wu N, Li Y, Ye K, Lu B, Zhang Z, Qu S, Li Y, Yang Y, Hu R Association of lipid profiles and the ratios with arterial stiffness in middle-aged and elderly Chinese. Lipids Health Dis 2014;13:37. https://doi.org/https://doi.org/10.1186/1476-511X-13-37, 1.
Livingstone KM, Givens DI, Cockcroft JR, Pickering JE, Lovegrove JA. Is fatty acid intake a predictor of arterial stiffness and blood pressure in men? Evidence from the Caerphilly prospective study. Nutr Metab Cardiovasc Dis 2013;23:1079–1085. https://doi.org/https://doi.org/10.1016/j.numecd.2012.12.002, 11.
Acknowledgments
Not applicable.
Funding
The Penn State University and the start-up grant from the college of health and human development and the department of nutritional sciences, Penn State University.
Author information
Authors and Affiliations
Contributions
NJ and ZH interpreted the analyzed data regarding the egg consumption and baPWV and were major contributors in writing the manuscript. XZ conducted the statistical analysis. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The data utilized are from the Kailuan Study, a population-based prospective cohort launched in 2006 in Tangshan, China (The Chinese Clinical Trial Registry #: ChiCTR-TNRC-1101489).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Adjusted means (± standard error) of baPWV change rate (cm/s/year) by egg consumption group in Chinese adults, after further adjusted for DBP, MAP and PP.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ji, N., Huang, Z., Zhang, X. et al. Association between egg consumption and arterial stiffness: a longitudinal study. Nutr J 20, 67 (2021). https://doi.org/10.1186/s12937-021-00720-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12937-021-00720-6