Abstract
The emergence and spread of artemisinin partial resistance in East and Horn of Africa is alarming. However, artemisinin-based combination therapy (ACT) generally remains efficacious for the treatment of falciparum malaria. The emergence of partial artemisinin resistance does not currently meet the criteria to initiate change on treatment guidelines nor affect ACT routine procurement and distribution. It is high time for scientists and transitional researchers to be more critical and vigilant on further changes so that national programmes will be able to make informed decisions as well as remain alert and prepared for any change that may be required in the future.
Similar content being viewed by others
Background
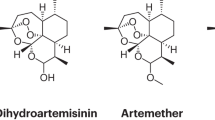
Artemisinin-based combination therapy (ACT) is the main and most effective treatment option for uncomplicated Plasmodium falciparum malaria in Africa. Artemisinin-based combinations are widely used across malaria-endemic countries in Africa, where resistance to chloroquine (CQ) and other anti-malarials [1]. is well established. In 2000, the first ACT partial resistance cases were reported in South East Asia (SEA), which has been the epicentre of anti-malarial resistance and treatment failure emergence [2, 3]. The major artemisinin-based combinations currently used in Africa are artemether-lumefantrine (AL), artesunate-amodiaquine (AA), dihydroartemisinin-piperaquine (DHAPPQ), artesunate-mefloquine (AM), and most recently artesunate-pyronaridine (AP). In Ethiopia, AL has been the first-line treatment for uncomplicated P. falciparum and second-line for Plasmodium vivax malaria since 2005 and has retained high efficacy (Table 1) [4].
While therapeutic efficacy studies (TES) show efficacy in Ethiopia, recent parasite genomic studies reveal molecular markers of artemisinin partial resistance (ArtR) in several African countries. These markers are found alongside fixed mutations associated with resistance to other anti-malarial drugs. New studies show an upsurge in the frequency of WHO-validated/candidate mutations in the Kelch 13 (k13) gene (R561H, A675V and C469Y) in several African countries (Rwanda, Tanzania and Uganda, respectively) [5,6,7] Recently, a new ACT partial-resistance marker k13 R662I and interactions with pfhrp2/3 deletion has been reported in Ethiopia [8] and Eritrea [9] Although most of these reports of genotypic resistance are not supported by phenotypic resistance determined using standard WHO TES methods, a few studies that technically deviate from the WHO protocol reported < 90% efficacy in Angola, DRC, and Burkina Faso [10].. While phenotypic evidence of treatment failure is limited, the increasing reports of validated ArtR mutations are alarming. The emergence of ArtR in Africa may herald the emergence of ACT treatment failure, as was observed in SEA [11, 12].
Artemisinin resistance is mediated by mutations in the K13 protein. ArtR is identified by several field validated drug pressure invitro assays as well as genetic engineering studies [13,14,15]. These mutations likely alter ubiquitination patterns and help parasites avoid accumulation of polyubiquitinated proteins. Mutations in the propeller domain of the k13 gene are now being routinely validated as markers of artemisinin resistance through the use of CRISPR gene editing and in vitro ring stage survival assay (RSA) [14]. However, the independent emergence of multiple partial resistance markers mostly unsupported by TES results makes policy recommendations challenging.
This commentary summarizes the recent data from East Africa and the Horn of Africa (EHoA), with an emphasis in Eritrea and Ethiopia where k13 R622I mutation and pfhrp2/3 deletions co-occur. The main objective of this commentary is to help inform the national malaria control programme (NMCP) and policymaker decision-making.
What do we know
Southeast Asia (SEA)
Clinical artemisinin resistance was first demonstrated in two parallel studies conducted in Western Cambodia in the late 2000s [2, 3]. Patients were identified with continued infection for up to 7 days after artesunate monotherapy and decreased parasite clearance rates. While propeller domain initially remained effective in SEA, ArtR emergence set the stage for ACT failure owing to rapid emergence of partner drug resistance [6]. In many areas, 35–45% of patients treated with ACT failed therapy due to the combined effect of artemisinin and partner drug resistance [12].
East and the Horn of Africa (EHoA)
Recently, ArtR has been reported across EHoA, including Rwanda [6], Uganda [7], Tanzania [5], Kenya [16]), Ethiopia [8, 17], Eritrea [9], Somalia [18], and Sudan [19, 20].
However, ACT remain efficacious in Africa (for now). Therapeutic efficacy studies show ACT efficacy > 95% in most settings, well above the WHO 90% threshold for policy change. However, there is strong evidence that WHO-validated and candidate k13 mutations associated with ArtR are emerging in Africa and beginning to spread. This includes R561H in Rwanda, Uganda and Tanzania; C469Y and A675V in Uganda [5, 6, 21]; and R622I in Ethiopia and Eritrea (Table 2). Recent study showed high prevalence of R622I in northern Ethiopia [8]. This mutation was first reported in two small studies in the northwest part of Ethiopia (North Gondar) with increasing prevalence over 5 years, 2.4% in 2013 and 9.5% in 2017–18 [22].
In Ethiopia, AL has been used for uncomplicated P. falciparum malaria since 2005. Accordingly, several TES have been conducted per WHO requirement, mainly led by the Ethiopian Public Health Institute (EPHI) and other groups. The results have been encouraging, with an average adequate clinical and parasitological response (ACPR) of approximately 96% The studies were conducted for programmatic purposes, and the data has been utilized by the NMCP to guide decision making and disseminated in peer-reviewed journals. However, major publications by Fola et al. [8], and Mihreteab et al. [9] reported established and expanding high prevalence of ArtR mutations (R622I) in Ethiopia and Eritrea, findings supported by a recent manuscript by Emiru et al. [17] from Ethiopia. These findings are alarming and surprising local programmes as they contradict high ACT efficacy observed during TES.
Implications
Reports of mutations associated with ArtR are relevant to the programme and require a careful response. Multiple WHO-candidate and -validated ArtR markers have been reported across EHoA (Table 3), with k13 622I prevalent in Ethiopia and Eritrea. Validated makers are known to improve parasite survival in vitro during RSA, as well as delayed parasite clearance in vitro or in clinical cases assessed by day 3 parasitaemia [23]. The k13 R622I mutation currently reported in Ethiopia and Eritrea is a WHO-validated marker. Because R622I prevalence varies from place to place within these countries and sampling was not nationally representative, nationwide genomic surveillance is warranted. Sampling across different eco-epidemiological transmission zones is important to understand the distribution of ArtR markers. The Ethiopian study by Fola et al. [8] used clinic-based sampling and built upon EPHI’s work on pfhrp2/3 deletion [24]. However, the Eritrean study byMihreteab et al. came from three consecutive TES surveys in 2016, 2017, 2019 [9]. The results indicate that ACT efficacy is threatened. However, the WHO definition of artemisinin partial resistance requires delay in the clearance of malaria parasites from the bloodstream or in an in vitro setting after ACT challenge. Patients infected by P. falciparum with partial resistance ACT may harbour parasites for more than 3 days after treatment. The remaining parasites have a better chance of survival and onward transmission unless partner drugs that remain in circulation are capable of killing them [2, 3]. Killing by partner drugs with longer half-life than artemisinin derivatives may explain the high efficacy of ACT despite partial resistance; these patients treated with an artemisinin-based combinations are fully cured if the partner drug is still efficacious [23].
In summary, the emergence of artemisinin partial resistance in EHoA requires immediate and more expansive clinical and genomic surveillance to closely monitor the extent of resistance and determine its clinical impact.
Despite the multiple emergences of partial resistance molecular markers, ACT remain efficacious in Ethiopia and fulfill WHO requirements for the treatment of uncomplicated P. falciparum malaria. Therefore, the emergence of partial artemisinin resistance does not currently meet criteria for changes in routine treatment of patients with ACT or affect routine procurement and distribution of ACT. Researchers and scientists need to work together to generate deeper and wider studies that are representative and monitor closely for evidence of decreased clinical efficacy of ACT. While increasing reports of ArtR mutations are alarming, careful and conscientious decisions will allow the programme to remain alert and to prepare for future policy changes if needed.
Take home message to national malaria control programmes: do not panic but remain vigilant!
-
Recent reports of ArtR should alert the programme to the need for robust, representative phenotypic and genomic surveillance. Genomic surveillance may need to be integrated into ongoing routine TES activities.
-
Alternative artemisinin-based combinations and second-line drugs need to be sought and procurement plans developed.
-
Lessons from Southeast Asia need to be reviewed and used to control the spread of ArtR parasites and for mitigation.
-
Currently available data is in its early stage. Recent reports should generate concern but not panic. The programme does not need revise its current treatment regimen, nor should health providers hesitate to continue routine use of ACT. However, the programme has an opportunity to be proactive against the threat of ArtR, including close monitoring and exploring options for alternative therapies should they be required in future.
-
The programme and researchers must work together to enable evidence-based decision-making.
-
Mapping partner drug resistance needs to be expedited, as their efficacy is a key reason why ACT remains effective in regions affected by ArtR P. falciparum.
Data availability
No datasets were generated or analysed during the current study.
References
WHO. Guideline for the treatment of Malaria. Geneva: World Health Organization; 2015.
Noedl H, Socheat D, Satimai W. Artemisinin-resistant malaria in Asia. N Engl J Med. 2009;361:540–1.
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, et al. Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009;361:455–67.
Federal Democratic Republic of Ethiopia Ministry of Health. Malaria diagnosis and treatment guidelines for health workers in Ethiopia. Addis Ababa; 2004.
Moser KA, Madebe RA, Aydemir O, Chiduo MG, Mandara CI, Rumisha SF, et al. Describing the current status of Plasmodium falciparum population structure and drug resistance within mainland Tanzania using molecular inversion probes. Mol Ecol. 2021;30:100–13.
Uwimana A, Legrand E, Stokes BH, Ndikumana JLM, Warsame M, Umulisa N, et al. Emergence and clonal expansion of in vitro artemisinin-resistant Plasmodium falciparum kelch13 R561H mutant parasites in Rwanda. Nat Med. 2020;26:1602–8.
Conrad MD, Asua V, Garg S, Giesbrecht D, Niaré K, Smith S, et al. Evolution of partial resistance to artemisinins in malaria parasites in Uganda. N Engl J Med. 2023;389:722–32.
Fola AA, Feleke SM, Mohammed H, Brhane BG, Hennelly CM, Assefa A, et al. Plasmodium falciparum resistant to artemisinin and diagnostics have emerged in Ethiopia. Nat Microbiol. 2023;8:1911–9.
Mihreteab S, Platon L, Berhane A, Stokes BH, Warsame M, Campagne P, et al. Increasing prevalence of artemisinin-resistant HRP2-negative malaria in Eritrea. N Engl J Med. 2023;389:1191–202.
Rosenthal MR, Ng CL. A proteasome mutation sensitizes P. falciparum Cam3.II K13C580Y parasites to DHA and OZ439. ACS Infect Dis. 2021;7:1923–31.
Phyo AP, Jittamala P, Nosten FH, Pukrittayakamee S, Imwong M, White NJ, et al. Antimalarial activity of artefenomel (OZ439), a novel synthetic antimalarial endoperoxide, in patients with Plasmodium falciparum and Plasmodium vivax malaria: an open-label phase 2 trial. Lancet Infect Dis. 2016;16:61–9.
van der Pluijm RW, Imwong M, Chau NH, Hoa NT, Thuy-Nhien NT, Thanh NV, et al. Determinants of dihydroartemisinin-piperaquine treatment failure in Plasmodium falciparum malaria in Cambodia, Thailand, and Vietnam: a prospective clinical, pharmacological, and genetic study. Lancet Infect Dis. 2019;19:952–61.
Tun KM, Imwong M, Lwin KM, Win AA, Hlaing TM, Hlaing T, et al. Spread of artemisinin-resistant Plasmodium falciparum in Myanmar: a cross-sectional survey of the K13 molecular marker. Lancet Infect Dis. 2015;15:415–21.
Straimer J, Gnädig NF, Witkowski B, Amaratunga C, Duru V, Ramadani AP, et al. Drug resistanceK13-propeller mutations confer artemisinin resistance in Plasmodium falciparum clinical isolates. Science. 2015;347:428–31.
Imwong M, Nguyen TN, Tripura R, Peto TJ, Lee SJ, Lwin KM, et al. The epidemiology of subclinical malaria infections in South-East Asia: findings from cross-sectional surveys in Thailand-Myanmar border areas, Cambodia, and Vietnam. Malar J. 2015;14:381.
Owoloye A, Olufemi M, Idowu ET, Oyebola KM. Prevalence of potential mediators of artemisinin resistance in African isolates of Plasmodium falciparum. Malar J. 2021;20:451.
Emiru T, Getachew D, Murphy M, Sedda L, Ejigu LA, Bulto MG, et al. Evidence for a role of Anopheles stephensi in the spread of drug- and diagnosis-resistant malaria in Africa. Nat Med. 2023;29:3203–11.
Jalei AA, Na-Bangchang K, Muhamad P, Chaijaroenkul W. Monitoring antimalarial drug-resistance markers in Somalia. Parasites Hosts Dis. 2023;61:78–83.
Mohamed AO, Hussien M, Mohamed A, Suliman A, Elkando NS, Abdelbagi H, et al. Assessment of Plasmodium falciparum drug resistance molecular markers from the Blue Nile State Southeast Sudan. Malar J. 2020;19:78.
de la Fuente IM, Benito MJS, Ousley J, de Gisbert FB, García L, González V, et al. Screening for K13-propeller mutations associated with artemisinin resistance in Plasmodium falciparum in Yambio County (Western Equatoria State), South Sudan. Am J Trop Med Hyg. 2023;109:1072–6.
Balikagala B, Fukuda N, Ikeda M, Katuro OT, Tachibana SI, Yamauchi M, et al. Evidence of artemisinin-resistant malaria in Africa. N Engl J Med. 2021;385:1163–71.
Bayih AG, Getnet G, Alemu A, Getie S, Mohon AN, Pillai DR. A unique Plasmodium falciparum K13 gene mutation in Northwest Ethiopia. Am J Trop Med Hyg. 2016;94:132–5.
WHO. Responding to antimalarial drug resistance. Geneva, World Health Organization, http://www.who.int/malaria/areas/drug_resistance/overview/en/. Accessed 22 Mar 2019.
Feleke SM, Reichert EN, Mohammed H, Brhane BG, Mekete K, Mamo H, et al. Plasmodium falciparum is evolving to escape malaria rapid diagnostic tests in Ethiopia. Nat Microbiol. 2021;6:1289–99.
Acknowledgements
This work was partly supported by the US National Institutes of Health (R01AI177791). Jonathan B Parr is acknowledged for the review of the document.
Funding
There was no direct funding for this work. All authors receive their salaries from their respective institutes.
Author information
Authors and Affiliations
Contributions
AA, AF, GT participate on a discussion and conceptualize the perspective concept. AA wrote the first draft. All authors critically reviewed and approved the final draft.
Corresponding author
Ethics declarations
Competing interests
All authors declare there is no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Assefa, A., Fola, A.A. & Tasew, G. Emergence of Plasmodium falciparum strains with artemisinin partial resistance in East Africa and the Horn of Africa: is there a need to panic?. Malar J 23, 34 (2024). https://doi.org/10.1186/s12936-024-04848-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-024-04848-8