Abstract
Background
In 2020–2021, long-lasting insecticidal nets (LLINs) were distributed nationwide in Uganda during the COVID-19 pandemic. A cross-sectional survey was conducted in 12 districts to evaluate the impact of the campaign 1–5 months after LLIN distribution.
Methods
During April–May 2021, households were randomly selected from target areas (1–7 villages) surrounding 12 government-run health facilities established as Malaria Reference Centres; at least 50 households were enrolled per cluster. Outcomes included household ownership of LLINs distributed through the universal coverage campaign (UCC) (at least one UCC LLIN), adequate coverage of UCC LLINs (at least one UCC LLIN per 2 residents), and use of LLINs (resident slept under a LLIN the previous night). Multivariate logistic regression models were used to identify household- and individual-level factors associated with outcomes, controlling for clustering around health facilities.
Results
In total, 634 households, with 3342 residents and 1631 bed-nets, were included. Most households (93.4%) owned at least 1 UCC LLIN, but only 56.8% were adequately covered by UCC LLINs. In an adjusted analysis, the factor most strongly associated with adequate coverage by UCC LLINs was fewer household residents (1–4 vs 7–14; adjusted odds ratio [aOR] 12.96, 95% CI 4.76–35.26, p < 0.001; 5–6 vs 7–14 residents; aOR 2.99, 95% CI 1.21–7.42, p = 0.018). Of the 3166 residents of households that owned at least one UCC LLIN, only 1684 (53.2%) lived in adequately covered households; 89.9% of these used an LLIN the previous night, compared to 1034 (69.8%) of 1482 residents living in inadequately covered households. In an adjusted analysis, restricted to residents of inadequately covered households, LLIN use was higher in children under-five than those aged 5–15 years (aOR 3.04, 95% CI 2.08–4.46, p < 0.001), and higher in household heads than distantly-related residents (aOR 3.94, 95% CI 2.38–6.51, p < 0.001).
Conclusions
Uganda’s 2021–21 campaign was successful, despite the COVID-19 pandemic. In future campaigns, strategies should be adopted to ensure high LLIN coverage, particularly for larger households. A better understanding of the drivers of LLIN use within households is needed to guide future interventions, educational messages, and behaviour change communication strategies; school-aged children and distantly-related residents appear vulnerable and could be targeted.
Similar content being viewed by others
Background
Malaria remains a life-threatening public health concern, particularly in sub-Saharan Africa [1]. Long-lasting insecticidal nets (LLINs) have been shown to reduce malaria burden and mortality [2, 3], and are the primary vector control tool in Africa. Ownership of LLINs has increased markedly over the past 20 years, contributing to substantial progress in malaria control [4]. Between 2000 and 2019, an estimated 1.5 billion malaria cases were averted, 94% in Africa [1]; much of this success has been attributed to the scale-up of LLINs [5]. Recent evidence, however, suggests progress has stalled, particularly in high burden countries such as Uganda [5, 6]. To achieve universal coverage with LLINs (one LLIN for every two persons at risk), the World Health Organization (WHO) recommends delivering LLINs free-of-charge through mass distribution campaigns every 3 years [7]. Such mass campaigns have been shown to increase equitable ownership of LLINs [8], but achieving high LLIN coverage remains a challenge [9].
In 2021, Uganda ranked third in number of malaria cases globally [1]. Uganda’s Ministry of Health has committed to ensuring high LLIN coverage through mass distribution campaigns carried out every 3 years according to WHO guidelines. In Uganda, the first LLIN distribution campaign was conducted in 2013–14, delivering over 20 million LLINs to households free-of-charge nationwide [10]; a subsequent campaign was conducted in 2017–18. These campaigns successfully increased household ownership of at least one LLIN to over 90%, but in 2015, only 62% of households were adequately covered by one LLIN for every two residents [11]. In 2017–18, prior to the second mass campaign, adequate LLIN coverage had fallen to 18% [12], and in 2019, adequate coverage following the 2017–18 mass campaign was only 54% [13].
Uganda’s Ministry of Health and partners led the third mass LLIN distribution campaign in 2020–21, distributing about 28 million LLINs nationwide during the COVID-19 pandemic [14]. To evaluate the impact of this campaign on LLIN ownership, coverage, and use in Uganda, a cross-sectional survey was conducted soon after LLIN distribution in 12 districts.
Methods
Study design and setting
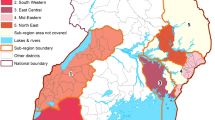
Target areas of 1–7 villages surrounding 12 government-run health facilities in 12 districts in Uganda were included (Fig. 1). These level III/IV health centres are located in moderate to high malaria transmission settings and have been established as Malaria Reference Centres (MRCs), sites for enhanced health facility-based malaria surveillance. These 12 MRCs were purposively selected to give good geographic spread of sites with some near borders with other countries, location in a rural area, and location along trade routes. The 12 sites were part of 64 MRCs included in a cluster-randomized trial to evaluate the impact of LLINs distributed in 2020–21 across 32 districts in Uganda (LLINEUP2, ClinicalTrials.gov: NCT04566510).
Sample size and power determination
This survey was embedded in a cluster-randomized trial to evaluate the impact of LLINs distributed in 2020–21 across 32 districts in Uganda (ClinicalTrials.gov: NCT04566510). The sample size for the cross-sectional community surveys was predetermined for the main trial, using calculations applied for the outcome of parasite prevalence. A total of 50 households with at least one child aged 2–10 years were recruited from each cluster. A sample size of 634 households is estimated to provide a power of 100% for the primary outcome of adequate coverage with UCC LLINs, assuming baseline (pre-distribution) LLIN coverage of 17.9% and post-distribution coverage of 54.0% [12, 13], a level of significance of 0.05, and design effect of 2 [15].
Sampling procedure, recruitment and enrollment
Target areas surrounding each MRC were identified, including the village where the MRC is located and adjacent villages that met the following criteria: (1) did not contain another government-run health facility, (2) located in the same sub-county as the MRC, and (3) similar incidence of malaria as the MRC’s village. All households within the MRC target areas were mapped and enumerated to generate a sampling frame for the survey. A random sample of enumerated households was selected from each target area to generate a list of households to approach for recruitment. Households on the recruitment list were approached and enrolled if the following criteria were met: (1) at least one adult aged 18 years or older present, (2) adult is a usual resident who slept in the sampled household on the night before the survey, and (3) agreement of the adult resident to provide informed consent. For each MRC target area, consecutive eligible households were surveyed until 50 households with at least one child aged 2–10 years were enrolled.
Household registration and LLIN distribution
LLINs were distributed in the LLINEUP2 study sites by the Ugandan Ministry of Health through the national universal coverage campaign (UCC) in December 2020 (369,317 LLINs) and March 2021 (603,064 LLINs). LLIN distribution was conducted according to detailed national guidelines based on prior experiences from UCCs conducted in 2013–2014 and 2017–18 [16]. The guidelines were adapted to adhere to COVID-19 standard operating procedures. This campaign was conducted by multidisciplinary team who went door-to-door to register households and distribute LLINs. Data were managed through an Electronic Data Management Information System (EDMIS), which calculated the number of LLINs to allocate to each household, based on the registration data. The LLINs were issued to the head of household, or another adult resident. The target was to distribute one LLIN for every two household residents; with households of more than 10 residents receiving a maximum of 5 LLINs.
Data collection and management
Household surveys were administered to heads of household or their designate using electronic questionnaires on hand-held tablet computers, which were programmed to include range checks and internal consistency checks. Information was gathered on characteristics of households and residents, proxy indicators of wealth including ownership of assets, and ownership and use of LLINs in the households. To objectively identify the LLINs, the RAs observed the nets within each household surveyed, and recorded the details of each net/LLIN. Data collected were transferred daily to a secure server on a private network at the core data facility in Kampala.
Statistical analysis
Data were analysed using Stata version 14.1 (College Station, TX). Principal component analysis was used to generate a wealth index based on ownership of common household items. Households were ranked by wealth scores and grouped into terciles to provide a categorical measure of socioeconomic status. Modern houses were defined as having plaster or cement walls, metal or wooden roofs, and closed eaves; all other houses were defined as traditional [17]. The primary outcome was adequate UCC LLIN coverage (proportion of households that own at least one UCC LLIN for every two residents), and other outcome measures included: (1) UCC LLIN ownership (defined as the proportion of households that own at least one UCC LLIN), (2) LLIN access (proportion of residents who could sleep under UCC LLIN, if each UCC LLIN in the household were used by up to two residents), and (3) LLIN use (the proportion of household residents who slept under any LLIN the previous night).
Associations between variables of interest and outcome measures including adequate UCC LLIN coverage and LLIN use were estimated using multivariate logistic regression models with robust standard errors adjusted for clustering at the level of the health facility. Measures of association were expressed as odds ratios (ORs). A two-sided p-value of < 0.05 was considered statistically significant. Associations between variables of interest with ownership of UCC LLINs were also explored (Additional file 1).
Results
Characteristics of the households, and residents surveyed
Of 993 households approached for recruitment (Fig. 2), 359 were excluded before enrollment, primarily because no adult was available (89.1%). Most household heads were male (Table 1), with a median age of 40 years (range 18–95 years). The median number of household residents was 5 (range 1–14); 153 households (24.1%) had 7 or more residents. Most households had at least one child under 5 years, and were constructed with traditional materials. Close to a third of households were located ≥ 2 km from the nearest health facility.
Overall, 3342 household residents were surveyed (Table 1). About half of the residents were female, and over 15 years of age. Most residents were either the head of household (19.0%) or their first degree relative (66.4%); fewer residents were more distantly, or not, related to the household head (14.6%).
Impact of the 2020–21 UCC on LLIN ownership and coverage
LLINs were distributed through the UCC to surveyed households in December 2020 (n = 475) and March 2021 (n = 159). Most households (86.4%) reported receiving some education about malaria and LLINs when the UCC nets were distributed. LLIN ownership was high in the households enrolled in the survey (Fig. 2, Table 2); 609 of 634 households (96.1%) owned at least one LLIN, 25 (3.9%) did not own a LLIN of any type, and 42 (6.6%) did not own a LLIN distributed through the UCC campaign. Of those households that did not own LLINs, most (59.5%) were away when nets were distributed, 19.1% reported that nets had run out, 16.6% were never told or did not collect the nets, and 4.8% households did not register or their local leaders refused to accept nets.
Despite high LLIN ownership, far fewer households were adequately covered by LLINs. Of the 634 households, 360 (56.8%) owned at least one UCC LLIN for every 2 residents, and 374 (59.0%) were adequately covered by LLINs of any type. Adequate coverage with UCC LLINs varied markedly by study site, from 32.7% to 94.4% in the different districts (Fig. 3).
Impact of the 2020–21 UCC on LLIN use
Of the 3342 residents surveyed (Table 2), 79.1% had access to UCC LLINs (defined as the proportion of residents who could sleep under an LLIN, if every LLIN in the household was used by up to two residents); slightly more residents had access to an LLIN of any type. Most residents reported sleeping under a UCC LLIN the previous night (71.0%), and even more slept under any LLIN. Of the 1631 nets observed, nearly all were LLINs (99.1%), and most were distributed during the 2020–21 UCC (89.4%). Most UCC LLINs were hung, and had been used the previous night.
Factors associated with adequate coverage by UCC LLINs
In an adjusted analysis, the factor most strongly associated with adequate coverage with UCC LLINs was fewer household residents (Table 3); only 29.7% of households with 7–14 residents were adequately covered with UCC LLINs vs 82.2% of those with 1–4 residents (adjusted odds ratios [aOR] 12.96, 95% CI 4.76–35.26, p < 0.001); vs 58.7% of those households with 5–6 residents (aOR 2.99, 95% CI 1.21–7.42, p < 0.018). Other factors associated with adequate coverage with UCC LLINs included household ownership of UCC nets only (64.3% vs 39.0% in households that owned non-UCC LLINs; aOR 3.55, 95% CIs 2.02–6.25, p < 0.001), older household heads (65.3% in households led by heads aged 50–85 years vs 57.2% in those led by heads aged 18–39 years; aOR 2.34, 95% CIs 1.54–3.56, p < 0.001), female heads of household (78.1% vs 52.8% in households led by males; aOR 1.87, 95% CIs 1.17–3.00, p = 0.009) and greater household wealth (63.8% in least poor vs 60.7% in poorest households, aOR 1.92, 95% CI 1.37–2.69, p < 0.001).
Factors associated with use of any LLIN by residents living in households with, and without, adequate UCC LLIN coverage
Of the 3166 residents living in households that owned at least one UCC LLIN, 1684 (53.2%) lived in households that were adequately covered by UCC LLINs, while 1482 (46.8%) lived in households that were inadequately covered (Table 4). The proportion of residents who reported sleeping under any LLIN the previous night was significantly higher in households that were adequately covered with UCC LLINs than in inadequately covered households (89.9% vs 69.8%, p < 0.001).
In an adjusted analysis restricted to residents of households that were adequately covered by UCC LLINs (n = 1684), LLIN use was higher in children < 5 years (95.5% vs 85.1% in children aged 5–15 years; aOR 2.52, 95% CI 1.53–4.16, p < 0.001), in households with at least one child under 5 years (92.5% vs 84.1% in households without young children, aOR 2.52, 95% CI 1.62–3.93, p < 0.001), and in heads of household (95.3% vs 87.5% in residents who were more distantly (or not) related to the household head, aOR 3.29, 95% CI 1.30–7.72, p = 0.006). Other factors associated with LLIN use the previous night in households that were adequately covered by UCC LLINs included ownership of non-UCC LLINs, timing of the UCC LLIN distribution, and female gender.
In a similar adjusted analysis restricted to residents of households that were not adequately covered by UCC LLINs (n = 1482), LLIN use was higher in heads of household (83.6% vs 59.4% in residents who were more distantly related; aOR 3.94, 95% CI 2.38–6.51, p < 0.001), and in children < 5 years (80.8% vs 59.5% in children aged 5–15 years; aOR 3.04, 95% CI 2.08–4.46, p < 0.001). Other factors associated with use of any LLIN in households that were inadequately covered by UCC LLINs included household size and presence of non-UCC LLINs.
Discussion
LLINs are the mainstay of malaria control in Uganda. To ensure Ugandans have access to LLINs, the Ministry of Health delivers free nets through mass distribution campaigns every 3–4 years. However, achieving and sustaining high LLIN coverage remains a challenge. To better understand the impact of Uganda’s campaign to distribute LLINs in 2020–21, and factors associated with LLIN coverage and use, a cross-sectional survey was conducted 1–5 months post-distribution in 12 districts across Uganda. Considering several key LLIN indicators, the 2020–21 campaign was a success. Over 93% of households owned at least one LLIN distributed through the 2020–21 UCC, and over 70% of residents reported sleeping under a UCC LLIN the previous night. However, less than 60% of households owned at least one UCC LLIN for every two residents, which varied substantially by site, suggesting that the number of nets distributed to many households was insufficient to ensure adequate coverage. Prior studies in Uganda have highlighted that net attrition is also a major problem [2, 12], with the lifespan of many LLINs less than the anticipated 3 years. Strategies to ensure that households receive enough nets to guarantee high coverage and access to LLINs must be employed in future mass distribution campaigns.
The WHO recommends distributing LLINs every 3 years through mass campaigns supplemented by delivery of LLINs through routine channels, such as antenatal clinics [7]. Uganda’s Ministry of Health and partners have maintained commitment to mass distribution campaigns, and the success of the 2020–21 campaign, despite the ongoing COVID-19 pandemic, is remarkable. Contributors to this success include the door-to-door distribution model, which allowed the team to access individual households. Lockdowns and movement restrictions imposed to mitigate the spread of SARS-CoV-2 in Uganda may have also confined adults at home, making it easier to locate them and to distribute LLINs to individual households. Use of an electronic database to register households and residents, and to allocate the number of LLINs at the household level, was another major advance; in prior UCCs registration data were entered by hand and aggregated to determine the number of LLINs to allocate at the level of the subcounty [18]. This aggregated approach was susceptible to errors of omission, leaving some households without LLINs. Future campaigns should leverage and build on the electronic database established for this campaign to more accurately estimate the number of LLINs needed in advance to guide procurement, and to calculate the number of LLINs required in each household. Although few households did not own a UCC LLIN, engaging with community members to ensure they are aware of the distribution plans, and are available when LLINs are delivered, is essential as LLIN ownership is the foundation to improve LLIN access, coverage, and use.
In this study, the strongest predictor of adequate coverage with UCC LLINs was the number of household residents; the odds of adequate coverage with UCC LLINs were 13 times higher in households with only 1–4 residents than in those with 7–14 residents. Wealthier households, and those led by older individuals and female heads of household, were also more likely to be adequately covered by UCC LLINs. In the 2020–21 campaign, the number of LLINs distributed to each household was restricted to a maximum of five nets, regardless of household size. The practice of capping the number of LLINs distributed was likely the major contributing factor to inadequate LLIN coverage [7]. In future LLIN campaigns, strategies to increase the number of nets available for distribution (starting with adequate procurement), and to ensure that large households receive the correct number of LLINs to cover all residents (avoiding any blanket approaches to restricting the number of LLINs distributed) should be adopted. Routine distribution channels should also be strengthened to fill any gaps resulting from insufficient delivery of nets in the mass campaigns, which will be compounded by net attrition over time. In Uganda, LLINs are routinely distributed to vulnerable groups through the Expanded Program on Immunization, antenatal clinics, schools, and community health workers. Approaches to expand these routine channels, and to target poorer households and households led by younger males, should be explored.
Achieving adequate LLIN coverage is an important step toward maximizing access and use of LLINs. In this study, 86% of residents of households that were adequately covered with UCC LLINs slept under a LLIN the previous night, compared to only 62% in households that were inadequately covered. This link between adequate LLIN coverage and use of LLINs has been demonstrated elsewhere [19,20,21,22]. In western Kenya, households with more residents were less likely to own adequate numbers of LLINs, which strongly reduced the likelihood of using LLINs [19]. Similarly, elsewhere in Africa, including the Democratic Republic of Congo, Zambia, and Madagascar, as well as in Papua New Guinea and India, LLIN use was significantly higher in households that were adequately covered, with low LLIN coverage the main barrier to LLIN use [20,21,22,23,24]. In Tanzania, 2 years following a mass campaign, larger households, including those with more than four residents, were less likely to have access to, and to use, LLINs [25]. In Ethiopia and southern Africa, a study of over 6,000 households found that household size was associated with lack of equality in LLIN ownership and use of LLINs [26, 27]. These findings suggest that improving LLIN coverage would likely increase use of LLINs.
School-aged children were less likely to use LLINs in this study than younger children or older residents, regardless of whether they lived in a household that was adequately covered with UCC LLINs, or not. LLIN use among children aged 5–15 years from inadequately covered households was particularly low (< 60%). Multiple studies have found that school-aged children are less well-covered by LLINs [10, 12, 28]. These older children are often overlooked by malaria control strategies, which have traditionally focused on children under-five and pregnant women who typically bear the burden of malaria morbidity and mortality in higher transmission areas [29, 30]. Older children, who have developed anti-disease immunity through repeated exposure, are often asymptomatic when infected with malaria parasites. As a result, malaria infections in this age group may be missed. Malaria in school-aged children is not benign, however; older children may suffer consequences of malaria including clinical malaria episodes, anaemia, and cognitive impairment [28, 31]. School-aged children typically have the highest prevalence of asymptomatic malaria infection in higher transmission areas, serving as important reservoirs of infection for onward transmission of malaria [32,33,34]. Moreover, as the epidemiology of malaria in Africa evolves in response to intensified control efforts, increasing urbanisation, and climate change, transmission intensity and exposure to malaria parasites will decline, and consequently, acquisition of immunity may be slower. As a result, older children could have less robust immunity to malaria, and be at higher risk of clinical consequences of malaria infection. Studies conducted in Uganda, and Mali report shifts in the burden of malaria to older children [35,36,37], supporting this theory. Strategies such as school-based interventions aiming to improve LLIN coverage and use in older children are gaining traction. In Tanzania, a study to evaluate a school-based LLIN distribution programme found that LLIN use increased from 57 to 77% among primary school children [38]. Targeting school-aged children, who can serve as agents of change, can also improve LLIN use within households [39].
In this study, relationship of household residents to the head of household was associated with LLIN use in all households, regardless of LLIN coverage, suggesting that hierarchy and status within households may influence LLIN access and use. The odds of using a LLIN were 3–4 times greater for heads of household compared to second-degree relatives or unrelated residents. In households that were inadequately covered by UCC LLINs, less than 60% of distantly related household residents used an LLIN. This finding is somewhat unexpected given that settlements in most African countries tend to function as close units, irrespective of whether household members are nuclear or extended family [40]. However, a prior survey in Uganda also identified relationship to the head of household as a factor strongly associated with LLIN use, with second-degree relatives and unrelated household members less likely to use LLINs that household heads, regardless of adequate LLIN coverage [12]. Similarly, in Kenya, non-nuclear family members were less likely to use nets than residents closely related to the head of household (nuclear vs nonnuclear members, aOR = 4.75 (2.89–7.81) and aOR = 4.16 (1.40–12.38) in highland areas and lowlands respectively) [19]. In this study 15% of household residents were second-degree relatives or not related to the head of household. However, we were not able to explore these relationships, or to gain an understanding of whether these residents are permanent, or more transient, members of the household. An in-depth understanding of this population, including their role in the household and household dynamics is needed, to ensure that this vulnerable group is better targeted in future LLINs campaigns and interventions.
This study had several limitations. First, an in-depth understanding of why household residents use LLIN, or not, is limited by the quantitative nature of the questionnaire used in this survey. Further exploration of these important issues using qualitative research methods is needed to better understand determinants of LLIN use within households. Second, target areas included only a few villages surrounding the MRCs, which may have limited generalizability of these findings. However, all statistical models adjusted for site-specific clustering, to minimize any bias arising from the non-representativeness of few villages, and included conservative standard errors [41]. Third, LLIN use was self-reported, which could have under- or over-estimated actual LLIN use, but is the standard approach to measuring LLIN use [42].
Conclusion
The 2020–21 mass campaign to distribute LLINs in Uganda was a success, as evidenced by high ownership of UCC LLINs soon after distribution. However, far fewer households were adequately covered by UCC LLINs (one UCC LLIN for every two residents), specifically larger households with 7 or more residents. Children aged 5–15 years, and residents who were distantly related to the head of household, were less likely to use LLINs, particularly in households that were inadequately covered by UCC LLINs. In future LLIN campaigns, strategies to increase the number of nets available for distribution, and to ensure that large households receive the correct number of LLINs to cover all residents, should be adopted. Understanding the complexities of contextual and behavioural drivers of LLIN use is needed to guide future interventions, educational messages, and behavioural change communication strategies. Malaria control programmes should re-focus on school-aged children, who contribute disproportionately to malaria transmission [43], and may be at greater risk of clinical consequences of malaria as the epidemiology of malaria in Africa changes.
Availability of data and materials
The datasets reported herein will be made publicly available on completion of the LLINEUP2 project but are available from the corresponding author on reasonable request.
Abbreviations
- AL:
-
Artemether-lumefantrine
- ACTs:
-
Artemisinin-based combination therapies
- DHS:
-
Demographic health survey
- EDMIS:
-
Electronic data management information system
- IDRC:
-
Infectious disease research collaboration
- IRS:
-
Indoor residual spraying
- LLIN:
-
Long lasting insecticidal net
- MIS:
-
Malaria indicator survey
- MOH:
-
Ministry of health
- MOLAB:
-
Molecular research laboratory
- MRC:
-
Malaria reference centre
- OR:
-
Odds ratio
- PCR:
-
Polymerase chain reaction
- PBO:
-
Piperonyl butoxide
- RDT:
-
Rapid diagnostic test
- UCC:
-
Universal coverage campaign
- WHO:
-
World Health Organization
References
WHO. World malaria report. 20 years of global progress and challenges. Geneva: World Health Organization; 2020. p. 2020.
Staedke SG, Gonahasa S, Dorsey G, Kamya MR, Maiteki-Sebuguzi C, Lynd A, et al. Effect of long-lasting insecticidal nets with and without piperonyl butoxide on malaria indicators in Uganda (LLINEUP): a pragmatic, cluster-randomised trial embedded in a national LLIN distribution campaign. Lancet. 2020;395:1292–303.
Katureebe A, Zinszer K, Arinaitwe E, Rek J, Kakande E, Charland K, et al. Measures of malaria burden after long-lasting insecticidal net distribution and indoor residual spraying at three sites in Uganda: a prospective observational study. PLoS Med. 2016;13: e1002167.
Wanzira H, Eganyu T, Mulebeke R, Bukenya F, Echodu D, Adoke Y. Long lasting insecticidal bed nets ownership, access and use in a high malaria transmission setting before and after a mass distribution campaign in Uganda. PLoS ONE. 2018;13: e0191191.
Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015;526:207–11.
World Health Organization. World malaria report 2019. World Health Organization; 2019. https://apps.who.int/iris/handle/10665/330011. License: CC BY-NC-SA 3.0 IGO.
World Health Organization. Achieving and maintaining universal coverage with long-lasting insecticidal nets for malaria control. World Health Organization. 2017. https://apps.who.int/iris/handle/10665/259478. License: CC BY-NC-SA 3.0 IGO.
Taylor C, Florey F, Ye Y. Increasing equity of insecticide-treated net ownership in sub-Saharan Africa from 2003 to 2014. DHS analytic studies No. 52. Rockville, Maryland, USA: ICF International. 2015.
World Health Organization. World malaria report 2017. World Health Organization. https://apps.who.int/iris/rest/bitstreams/1091608/retrieve. License: CC BY-NC-SA 3.0 IGO.
Wanzira H, Katamba H, Rubahika D. Use of long-lasting insecticide-treated bed nets in a population with universal coverage following a mass distribution campaign in Uganda. Malar J. 2016;15:311.
Uganda Bureau of Statistics (UBOS) and ICF International. 2015. Uganda Malaria Indicator Survey 2014–15. Kampala, Uganda, and Rockville, Maryland, USA: UBOS and ICF International. 2015 [cited 2019 Jul 14] [p 141]. Available from: https://www.ubos.org/onlinefiles/uploads/ubos/2014-15%20Uganda%20Malaria%20Indicator%20Survey.pdf
Gonahasa S, Maiteki-Sebuguzi C, Rugnao S, Dorsey G, Opigo J, Yeka A, et al. LLIN Evaluation in Uganda Project (LLINEUP): factors associated with ownership and use of long-lasting insecticidal nets in Uganda: a cross-sectional survey of 48 districts. Malar J. 2018;17:421.
Uganda National Malaria Control Division (NMCD), Uganda Bureau of Statistics (UBOS), and ICF. Uganda Malaria Indicator Survey 2018–19. Kampala: NMCD UBOS and Uganda ICF Kampala and Rockville; 2020.
AMF funds 11.6 million nets for distribution in Uganda in 2020. [cited 2021 Nov 9]. Available from: https://www.againstmalaria.com/newsitem.aspx?newsitem=AMF-funds-11.6-million-nets-for-distribution-in-Uganda-in-2020
Wang H, Chow SC. Sample size calculation for comparing proportions. In: D’Agostino RB, Sullivan L, Massaro J, editors. Wiley Encyclopedia of Clinical Trials. Hoboken: John Wiley & Sons; 2007.
Ministry of Health Uganda, 2020; Mass distribution of long lasting insecticide treated nets to achieve Universal Coverage in 2020 in Uganda: detailed implementation guidelines Kampala, Uganda.
Tusting LS, Bottomley C, Gibson H, Kleinschmidt I, Tatem AJ, Lindsay SW, et al. Housing improvements and malaria risk in sub-Saharan Africa: a multi-country analysis of survey data. PLoS Med. 2017;14: e1002234.
Evaluation (Phase II) of the Universal Coverage Campaign for long-lasting insecticidal nets in Uganda: assessing effectiveness, efficiency and impact of the mass llin distribution. 2016. [cited 2021 Dec 21]. Available from: https://pdf.usaid.gov/pdf_docs/PA00MFPQ.pdf
Coalson JE, Santos EM, Little AC, Anderson EJ, Stroupe N, Agawo M, et al. Insufficient ratio of long-lasting insecticidal nets to household members limited universal usage in Western Kenya: a 2015 cross-sectional study. Am J Trop Med Hyg. 2020;102:1328–42.
Ntuku HM, Ruckstuhl L, Julo-Réminiac JE, Umesumbu SE, Bokota A, Tshefu AK, et al. Long-lasting insecticidal net (LLIN) ownership, use and cost of implementation after a mass distribution campaign in Kasaï Occidental Province. Democr Repub Congo Malar J. 2017;16:22.
Millat-Martínez P, Gabong R, Balanza N, Luana S, Sanz S, Raulo S, et al. Coverage, determinants of use and repurposing of long-lasting insecticidal nets 2 years after a mass distribution in Lihir Islands, Papua New Guinea: a cross-sectional study. Malar J. 2021;20:336.
Raghavendra K, Chourasia MK, Swain DK, Bhatt RM, Uragayala S, Dutta GDP, et al. Monitoring of long-lasting insecticidal nets (LLINs) coverage versus utilization: a community-based survey in malaria endemic villages of Central India. Malar J. 2017;16:467.
Simubali L, Colantuoni E, Hamapumbu H, Moss WJ, Norris DE, Kobayashi T, et al. Factors associated with sustained use of long-lasting insecticide-treated nets following a reduction in malaria transmission in Southern Zambia. Am J Trop Med Hyg. 2015;93:954–60.
Finlay AM, Butts J, Ranaivoharimina H, Cotte AH, Ramarosandratana B, Rabarijaona H, et al. Free mass distribution of long lasting insecticidal nets lead to high levels of LLIN access and use in Madagascar, 2010: a cross-sectional observational study. PLoS ONE. 2017;12: e0183936.
Mboma ZM, Overgaard HJ, Moore S, Bradley J, Moore J, Massue DJ, et al. Mosquito net coverage in years between mass distributions: a case study of Tanzania, 2013. Malar J. 2018;17:100.
Hailu A, Lindtjørn B, Deressa W, Gari T, Loha E, Robberstad B. Equity in long-lasting insecticidal nets and indoor residual spraying for malaria prevention in a rural South Central Ethiopia. Malar J. 2016;15:366.
Kanyangarara M, Hamapumbu H, Mamini E, Lupiya J, Stevenson JC, Mharakurwa S, et al. Malaria knowledge and bed net use in three transmission settings in southern Africa. Malar J. 2018;17:41.
Walldorf JA, Cohee LM, Coalson JE, Bauleni A, Nkanaunena K, Kapito-Tembo A, et al. School-age children are a reservoir of malaria infection in Malawi. PLoS ONE. 2015;10: e0134061.
Smith JL, Mumbengegwi D, Haindongo E, Cueto C, Roberts KW, Gosling R, et al. Malaria risk factors in northern Namibia: the importance of occupation, age and mobility in characterizing high-risk populations. PLoS ONE. 2021;16: e0252690.
Peter N, Aduogo P, Mutero CM. Long lasting insecticidal mosquito nets (LLINs) ownership, use and coverage following mass distribution campaign in lake victoria basin Western Kenya. BMC Public Health. 2021;21:1046.
Nankabirwa J, Brooker SJ, Clarke SE, Fernando D, Gitonga CW, Schellenberg D, et al. Malaria in school-age children in Africa: an increasingly important challenge. Trop Med Int Health. 2014;19:1294–309.
Staedke SG, Maiteki-Sebuguzi C, Rehman AM, Kigozi SP, Gonahasa S, Okiring J, et al. Assessment of community-level effects of intermittent preventive treatment for malaria in schoolchildren in Jinja, Uganda (START-IPT trial): a cluster-randomised trial. Lancet Global Health. 2018;6:e668–79.
Rehman AM, Maiteki-Sebuguzi C, Gonahasa S, Okiring J, Kigozi SP, Chandler CIR, et al. Intermittent preventive treatment of malaria delivered to primary schoolchildren provided effective individual protection in Jinja, Uganda: secondary outcomes of a cluster-randomized trial (START-IPT). Malar J. 2019;18:318.
Makenga G, Menon S, Baraka V, Minja DTR, Nakato S, Delgado-Ratto C, et al. Prevalence of malaria parasitaemia in school-aged children and pregnant women in endemic settings of sub-Saharan Africa: a systematic review and meta-analysis. Parasite Epidemiol Control. 2020;11: e00188.
Kigozi SP, Kigozi RN, Epstein A, Mpimbaza A, Sserwanga A, Yeka A, et al. Rapid shifts in the age-specific burden of malaria following successful control interventions in four regions of Uganda. Malar J. 2020;19:128.
Coulibaly D, Guindo B, Niangaly A, Maiga F, Konate S, Kodio A, et al. A decline and age shift in malaria incidence in rural Mali following implementation of seasonal malaria chemoprevention and indoor residual spraying. Am J Trop Med Hyg. 2021;104:1342–7.
Touré M, Sanogo D, Dembele S, Diawara SI, Oppfeldt K, Schiøler KL, et al. Seasonality and shift in age-specific malaria prevalence and incidence in Binko and Carrière villages close to the lake in Selingué. Mali Malar J. 2016;15:219.
Stuck L, Chacky F, Festo C, Lutambi A, Abdul R, Greer G, et al. Evaluation of long-lasting insecticidal net distribution through schools in Southern Tanzania. Health Policy Plan. 2022;37:243–54.
Wanzira H, Yeka A, Kigozi R, Rubahika D, Nasr S, Sserwanga A, et al. Long-lasting insecticide-treated bed net ownership and use among children under 5 years of age following a targeted distribution in central Uganda. Malar J. 2014;13:185.
Mafumbate R. The undiluted african community: values, the family, orphanage and wellness in traditional Africa. IKM. 2019;9(8):7–13.
Bell A, Fairbrother M, Jones K. Fixed and random effects models: making an informed choice. Qual Quant. 2019;53:1051–74.
MEASURE Evaluation. Household survey indicators for malaria control Measure DHS 2018. [cited 2021 Dec 20]. Available from: https://www.malariasurveys.org/documents/Household%20Survey%20Indicators%20for%20Malaria%20Control_FINAL.pdf
Andolina C, Rek JC, Briggs J, Okoth J, Musiime A, Ramjith J, et al. Sources of persistent malaria transmission in a setting with effective malaria control in eastern Uganda: a longitudinal, observational cohort study. Lancet Infect Dis. 2021;21:1568–78.
Acknowledgements
We would like to thank Emmanuel Bakashaba, Lillian Taaka, Isiko Joseph, Daniel Ochuli, Patrick Leuban Okello, Paul Oketch, Guma Benjamin, Jolly Job Odongo, Peter Mutungi, Simon Peter Kigozi, Geoff Lavoy, Nicholas Wendo, Yasin Kisambira, Chris Ebong, Asadu Sserwanga and the administration of the Infectious Diseases Research Collaboration for all their contributions. We would also like to acknowledge and thank the members of the Uganda National Malaria Control Division and the Liverpool School of Tropical Medicine for logistical and other support rendered as we carried out these surveys. We are grateful to the district health, administrative, and political leadership teams for all their support and guidance during community entry in the 12 districts of the study area.
Funding
Research reported in this publication was supported by the Against Malaria Foundation and the Fogarty International Centre (D43TW010526). This work was also supported in part by the Bill & Melinda Gates Foundation (BMGF) INV-017893 and INV-023690. Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission. The content of the manuscript is solely the responsibility of the authors
Author information
Authors and Affiliations
Contributions
SGS, MRK, GD, and CMS conceived the study, with input from SG, JO, JB and JN. SGS, GD, and SG developed the procedures and drafted the protocol with MRK, JN and JFN. MN, IB, and JFN led the data collection in the field, with oversight from SG, and support from CMS, JO, MRK and SGS. JO and GD managed the data and led the data analysis. JO and SG interpreted the data and drafted the manuscript, with input from SGS and GD. All authors reviewed the manuscript and gave permission for publication. JO, the corresponding author, had full access to all the data in the study and had final responsibility for the decision to submit for publication. All authors read and approved the final manuscript
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ugandan National Council for Science and Technology (UNCST Ref HS1097ES), Makerere University School of Medicine Research & Ethics Committee (SOMREC Ref 2020–193), London School of Hygiene & Tropical Medicine Ethics Committee (LSHTM Ref 22615–1) and the University of California San Francisco Human Research Protection Program Institutional Review Board (UCSF Ref 289107). Written informed consent to participate in the study was obtained by the head of household (or their designate) for all participating households. Verbal assent was obtained from all participants over the age of 8 years. Ethical approval for study procedures was provided by ethics committee of the School of Medicine College of Health Sciences, Makerere University (#REC P.EF 2019–122), and Uganda National Council of Science and Technology (HS1033ES).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Factors associated with households owning at least one UCC LLIN
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Okiring, J., Gonahasa, S., Nassali, M. et al. LLIN Evaluation in Uganda Project (LLINEUP2)—Factors associated with coverage and use of long‑lasting insecticidal nets following the 2020–21 national mass distribution campaign: a cross-sectional survey of 12 districts. Malar J 21, 293 (2022). https://doi.org/10.1186/s12936-022-04302-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04302-7