Abstract
Background
Malaria rapid diagnostic tests (RDTs) have expanded diagnostic service to remote endemic communities in Ethiopia, where 70% of malaria services per annum are reliant on them. However, diagnostic strategies are threatened by Plasmodium falciparum parasites with deletions of the histidine-rich protein 2 and/or 3 (pfhrp2/3) genes. Studies have reported pfhrp2/3 gene deletion prevalence in Ethiopia that exceeds the WHO recommended threshold to switch to non-HRP2 targeted RDTs for detection of P. falciparum. Therefore, RDTs that target alternative antigens, such as P. falciparum lactate dehydrogenase (PfLDH) are increasingly in programmatic use.
Methods
Malaria suspected patients visiting health facilities of Amhara, Tigray, Gambella, and Oromia regions of Ethiopia were screened by community health workers using Carestart Pf/Pv (HRP2/Pv-LDH) and SD-Bioline Pf (HRP2 for Pf/LDH for Pf) RDTs. Dried blood spot (DBS) samples were collected from selected patients for molecular and serological analysis. The clinical data and RDT results were recorded on standard forms, entered into EpiInfo, and analysed using STATA. The Pf-LDH detecting RDT results were compared with real-time PCR and bead-based immunoassay to determine their diagnostic performance.
Results
The 13,172 (56% male and 44% female, median age of 19 years ranging from 1 to 99 year) study participants were enrolled and tested with PfHRP2 and PfLDH detection RDTs; 20.6% (95% CI: 19.6 to 21.6) were P. falciparum RDT positive. A subset of samples (n = 820) were previously tested using P. falciparum lactate dehydrogenase (pfldh) quantitative real-time PCR, and 456 of these further characterized using bead-based immunoassay. The proportion of samples positive for P. falciparum by the PfHRP2 Carestart and SD-Bioline RDTs were 66% (539/820) and 59% (481/820), respectively; 68% (561/820) were positive for the PfLDH band on the SD-Bioline RDT. The sensitivity and specificity of the PfLDH RDT band were 69% and 38%, respectively, versus pfldh qPCR; and 72% and 36%, respectively, versus PfLDH detection by immunoassay. Among samples with results for RDT, qPCR, and immunoassay, higher proportions of P. falciparum were recorded by pfldh qPCR (90%, 411/456) and PfLDH immunoassay (88%, 363/413) compared to the PfLDH band on the SD-Bioline RDT (74.6%, 340/456).
Conclusion and recommendation
Both PfHRP2 RDTs detected fewer P. falciparum cases than PfLDH, and fewer cases than qPCR or immunoassay. The poor sensitivity and specificity of the PfLDH RDT compared to qPCR and to immunoassay in this study raises concern. Continuous operator training and RDTs quality assurance programme to ensure quality diagnostic services are recommended.
Similar content being viewed by others
Background
Human malaria is a mosquito-borne parasitic disease caused by protozoan parasites belonging to the genus Plasmodium [1]. Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae, Plasmodium ovale and Plasmodium knowlesi are the aetiologic agents of human malaria, of which P. falciparum is responsible for the most severe forms of the disease [2]. Over the last decade, there has been a tremendous reduction of malaria cases and deaths worldwide. Accordingly, mortality has reduced by 60% between 2000 and 2019 worldwide, whereas in Africa, where 94% of cases are accounted for, the annual mortality has fallen from 680,000 in 2000 to about 384,000 in 2019 [2].
In Ethiopia, malaria is one of the most important public health problems with more than 60% of Ethiopians at risk [3]. The country developed an elimination roadmap in 2016, which aims to reduce malaria incidence and mortality to zero by 2030 and prevent the re-establishment of malaria in all malaria-free areas [3]). Thus, the national programme is intensively implementing the elimination strategies, including parasitological diagnosis using rapid diagnostic tests (RDTs) or microscopy, and prompt treatment and prevention of relapse, using safe and effective anti-malarial drugs, vector control measures using indoor residual spray (IRS) and long-lasting insecticidal nets (LLINs), and health education.
Malaria case management is a crucial elimination strategy to reduce morbidity, mortality, prevent subsequent transmission and manage non-malarial febrile illnesses [4]. Diagnostic service provision in remote areas has been possible through the wide use of RDTs, an antigen detection test that gives rapid results with minimal operator training [5]. Malaria RDTs can detect the following three reliable target antigens: histidine-rich protein-2 (HRP2), parasite-specific lactate dehydrogenase (LDH) (species specific and pan specific), and Plasmodium aldolase, of which HRP2 antigen is the preferred and most commonly used for the detection of P. falciparum, due to its high abundance in the blood, high heat stability and species-specificity [6]. In sub-Saharan Africa, 99% of malaria is caused by P. falciparum [1]. Whereas in Ethiopia, 60–70% of annual malaria is caused by P. falciparum, 30–40% of cases are caused by P. vivax, and < 1% by both P. ovale and P. malariae based on routine facility report [3]. The small-scale community-based sero survey in Ethiopia has shown up to 11% P. ovale and 7% P. malariae antibody exposure history [7]. A study in China indicated that 1.5% confirmed P. ovale curtisi cases imported from Ethiopia [8].
Light microscopy is the gold standard for diagnosis of clinical malaria [9]. However, malaria RDTs are widely used in Ethiopia particularly in health posts by community health workers also called health extension workers (HEWs) and in health facilities that have no electricity, which accounts for about 70% of malaria diagnostic services per annum [3]. The national programme is using HRP2 and LDH detecting combination RDTs targeting P. falciparum and P. vivax, respectively [3], with detection capacity limited to both species only but not the P. ovale and P. malariae parasites. Besides this limitation, the malaria diagnostic programme is threatened by the emergence and spread of P. falciparum parasites that have single or dual deletion mutations of the pfhrp2/3 genes and hence not detected by the widely used HRP2-detecting RDTs [10].
A recent large survey conducted in three regions of north and west Ethiopia and estimated that HRP2-based RDTs would miss 9.7% of symptomatic falciparum malaria cases owing to deletion of the P. falciparum histidine-rich protein 2 (hrp2) genes [11]. Because this estimate exceeds the WHO-recommended 5% prevalence threshold for transitioning to non-HRP2 detecting RDTs, the national malaria programme is evaluating RDTs that detect alternative antigens for programmatic use. The only available alternatives P. falciparum-specific RDTs that meet procurement criteria detect P. falciparum-specific parasite lactate dehydrogenase (PfLDH) [12]. In the initial paper, the prevalence of false-negative RDTs in the three regions tested and the genetic epidemiology of parasites with pfhrp2 and/or pfhrp3 gene deletions has been described. In this paper, the analysis includes the performance of two WHO pre-qualified RDTs, to include comparison to bead-based immunoassay results for HRP2, aldolase, and parasite LDH antigens and to include additional samples collected from the Oromia region that were not included in the original study.
Methods
Study site and design
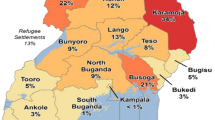
This cross-sectional survey was conducted in selected health facilities of Amhara, Tigray, and Gambella regions of Ethiopia (Fig. 1) between 2017and 2018 as described in previous study [11]. The present study also includes subjects from the Oromia region who were enrolled following the same procedures exactly as described in the previous work [11]. In brief, malaria suspected patients visiting the health facilities were enrolled in the study, and each patient was subjected to laboratory tests using Care Start Pf/Pv (HRP2/LDH) RDT (product code RM 103 VM-02571) and SD Bioline Malaria Ag Pf (HRP2 for Pf/LDH for Pf) (product code 05FK90). The RDTs were performed using finger-prick fresh whole blood following the manufacturer's instructions. Dried blood spot (DBS) samples were collected from selected positive patients for advanced testing run based on the published standard protocols for immunoassay [13] at the Centers for Disease Prevention and Control (CDC) laboratory, Atlanta, USA, and PCR assays [14] in North Carolina University, Chapel Hill, USA. The qPCR test is used to confirm the Plasmodium species, quantify the parasite and test P. falciparum (hrp2, pfldh and aldolase) target genes. Whereas, the bead based immunoassay [7] was used to test for HRP2, LDH and Aldolase antigens in the samples.
All enrolled subjects provided informed consent, and any subject with a positive test for malaria received treatment as directed by national guidelines. The study was carried out after the ethical approval is obtained from the Ethiopia Public Health Institute Institutional Review Board (IRB; protocol number EPHI-IRB-033–2017 for Amhara, Tigray and Gambella study, and EPHI-6.13/596 28 Jan 2020 for Oromia studies) and the WHO Ethics Review Committee Protocol number: ERC.0003174. Data cleaning and analysis was performed using Stata SE version 14 software. The association of the clinical and demographic variables with the P. falciparum positivity was measured using the T-test. The sensitivity and specificity of PfHRP2 and PfLDH detecting RDTs (screening tests) were performed against its qPCR and immunoassay (reference tests) results.
Results
A total of 13,172 malaria-suspected patients, 56% of whom were male and 44% female with an age range between 0 and 99 years and median age of 19 years who have visited health facilities in Amhara (30% study participants), Tigray (50%), Oromia (4%), and Gambella regions (16%) were enrolled in the study. Of all malaria suspected patients, 20.6% (2714/13172) were P. falciparum positives either by one or both RDTs. The patient’s information on clinical sign and symptoms showed a 91.4% fever cases (reported), 63.5% joint pain, 58% poor appetite, 57.4% feeling cold, 45% nausea and 18.4% headache. In addition, 75.7% were rural residents and, 6% (n = 777) of them had history of anti-malarial treatment a month before enrolled in the study, of which 31% received ACT, 11% chloroquine, 7% quinine, and 51% other drugs. All the variables including sex, clinical signs and symptoms, house location and anti-malarial treatment history had strong association with P. falciparum positivity (P < 0.001) (Table 1).
Molecular analysis was carried out in selected samples (n = 820) from P. falciparum cohort samples. The proportion of P. falciparum in PfHRP2 detecting CareStart RDT and SD-Bioline RDT were 66% (539/820) and 58.7% (481/820), respectively (Table 2). Whereas, the PfLDH targeted RDTs and pfldh PCR result showed 68% (561/820) and 86% (701/811) P. falciparum, respectively (Table 2). The PfHRP2 and PfLDH RDT test results showed a 97% high agreement (k: 0.94).
The sensitivity and specificity of the PfLDH targeted RDT result compared with the pfldh PCR assay was 69% and 38%, respectively, as previously reported [11] (Table 3). Here the false-negatives further analysed showed most (29%) of them had low parasitaemia (< 100 p/ul); low-density infections may have antigenaemia below the detection threshold of the RDTs. If the 36% (83/225) low-parasitaemia (< 200 p/µl) false-negatives are excluded from the analysis, given that they are below the expected RDT limit of detection, the PfLDH RDT’s sensitivity and specificity improve to 78% and 68%, respectively. However, 23% false negatives had > 2000 p/µl – well above the RDTs limit of detection – suggestive of operator, procedural, product related or administrative errors during RDT use (Table 3).
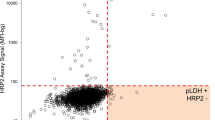
In addition, 456 of these 820 samples were further tested using bead-based immunoassay. The results in PfHRP2 detection by CareStart RDT, SD-Bioline RDT, PCR and bead-based immunoassay showed 61% (278/456), 55% (251/456), 57% (260/456) and 65% (297/456) P. falciparum positivity, respectively (Table 4). Whereas, the PfLDH-detecting SD Bioline RDT, pfldh PCR and PfLDH bead-based immunoassay showed 74.6% (340/456), 90% (411/456) and 88% (363/413) positives, respectively (Table 4). The PfLDH-targeted RDTs results compared with PLDH bead based immunoassay showed 72% and 36% sensitivity and specificity, respectively.
Discussion
Malaria case management through accurate diagnosis and prompt treatment is vital especially in elimination setting. In this study, relatively low malaria cases (21%) in spite of high fever prevalence (91%) in 13,172 self-presenting malaria suspected patients are reported which implies the need for accurate parasitological confirmation of cases for the rational use of treatment and management of non-malaria illnesses [15]. Given P. falciparum is the major cause of malaria mortality and morbidity in Africa, effective case management is needed to reach the goal of elimination. The use of malaria rapid diagnostic tests for the national diagnostic programme since the 1990th has been a backbone with significant increase of use over the last two decades which accounts for over 70% of diagnosis in Ethiopia [3]. However, the emergence of pfhrp2/3 gene mutated parasites in Ethiopia [7] is threatening because the widely used PfHRP2-detecting RDT is compromised. A recent study in Ethiopia reported high prevalence (~ 10%) of pfhrp2/3 gene deletions causing false negative HRP2-RDT results, which is above the 5% WHO prevalence threshold to change the diagnostic strategy [16], as a result the country is shifting to non-HRP2 (i.e. PfLDH) detection RDTs for programme use.
This study evaluates the performance of PfLDH detection RDT for programme use and presents the proportion and sensitivity of P. falciparum in HRP2 and PfLDH targeted RDTs, qPCR and multiplex assay results. The results show that generally higher proportion of P. falciparum is reported by the PfLDH RDT, pfldh qPCR and PfLDH multiplex assays (74%, 90% and 88%, respectively), with more cases are identified by PCR and bead-based immunoassay, compared to HRP2 RDTs and HRP2 bead-based immunoassay (55% and 65%, respectively) which implies that the PfLDH target antigen is performing better than HRP2 antigen detection for P. falciparum prevalence estimation.
Both RDTs used during the survey are WHO prequalified and, therefore, should meet requirements for safety and quality ([17] and https://extranet.who.int/pqweb/vitro-diagnostics/vitro-diagnostics-lists). However, the performance of malaria RDT is dependent on several factors in addition to parasite densities [18] such as reduced community level transmission intensities [19]; operator skill [20, 21], correct transport and storage conditions [22] and a strong product lot quality monitoring program [21]. In spite of high performance of PfLDH detection RDTs reported by others [12, 23,24,25], the lower sensitivity and specificity of LDH detection RDT reported in this study, 69% and 72% sensitivity against PCR and multiplex assay, respectively and 38% and 36% specificity against PCR multiplex, respectively, could be partly driven by samples with low parasitaemia below the detection threshold of the PfLDH RDT. Indeed, 29% of LDH detection RDT false-negatives are below 100 p/µl. In addition, operator’s skill gaps and low intensities of the transmission as most of this study sites are in elimination phase with annual parasite incidence (API) of less than one per 1000 population [7]. Therefore, laboratory and field level quality monitoring, operator’s refresher training, storage and transportation temperature monitoring are important to improve malaria RDTs service quality.
Limitation of the study
Subjects were enrolled using an adaptation of the WHO protocol for pfhrp2/3 deletion surveillance that prioritized enrollment of participants with discordant RDT results (16). This study design could introduce selection bias that limits the generalizability of our findings to the broader population. Nonetheless, analysis of multiple diagnostic assays applied to each sample provides a valuable opportunity to evaluate the performance of PfLDH RDTs. In addition, the field-level RDT tests were carried out by community health workers in remote health posts which could have impacted the results related to operators limited skills, inaccessibility for adequate supervision and, uncontrolled storage and transportation conditions. For example, faint test bands are not uncommon with the PfLDH-detecting RDT evaluated here and might be detected by expert readers, but missed by community health workers.
Conclusion and recommendation
The field-level performance of PfLDH detection RDTs results showed that the overall proportion of P. falciparum cases detected by PfLDH detecting RDT, pfldh qPCR and a PfLDH immunoassay is generally higher than HRP2 detection by RDT or immunoassay. However, the sensitivity and specificity of PfLDH detection RDTs compared to both pfldh PCR and to PfLDH bead-based immunoassay was lower than expected. As the country is preparing to switch to non-HRP2 detection in response to pfhrp2 deletion problem, a strong RDT quality assurance system and adequate in-service training for operators is needed before introducing alternative RDT products for national programme use.
Availability of data and materials
The database analysed in this study are available from the corresponding author.
References
Attila JT. The potential persistence of ancient malaria through the Quaternary period in Europe. Quaternary Int. 2021;586:1–13.
WHO. 20 years of global progress and challenges. Geneva: World Health Organization; 2020.
Ethiopian Federal Ministry of Health (FMoH). National malaria elimination roadmap. Addis Ababa: Ethiopian Federal Ministry of Health; 2016.
Eskild P, Martin PG. Accurate malaria diagnosis: not only essential for malaria case management, but prerequisite for managing febrile disease in the tropics. Clin Infect Dis. 2021;73:e1168–9.
Kojom Foko LP, Pande V, Singh V. Field performances of rapid diagnostic tests detecting human Plasmodium species: a systematic review and meta-analysis in India, 1990–2020. Diagnostics (Basel). 2021;11:590.
Martiáñez-Vendrell X, Jiménez A, Vásquez A, Campillo A, Incardona S, Gonzalez R, et al. Quantification of malaria antigens PfHRP2 and pLDH by quantitative suspension array technology in whole blood, dried blood spot and plasma. Malar J. 2020;19:12.
Feleke SM, Brhane BG, Mamo H, Assefa A, Woyessa A, Ogawa GM, et al. Sero-identification of the aetiologies of human malaria exposure (Plasmodium spp.) in the Limu Kossa District of Jimma Zone. South western Ethiopia Malar J. 2019;18:292.
Zhang T, Wang S, Wang D, Auburn S, Lu S, Xu X, et al. Epidemiological profile of Plasmodium ovale spp. imported from Africa to Anhui Province, China, 2012–2019. Malar J. 2021;20:15.
WHO. Global technical strategy for malaria 2016–2030. Geneva: World Health Organization, 2015; 1–35.
Kojom LP, Singh V. Prevalence of Plasmodium falciparum field isolates with deletions in histidine-rich protein 2 and 3 genes in context with sub-Saharan Africa and India: a systematic review and meta-analysis. Malar J. 2020;19:46.
Feleke SM, Reichert EN, Mohammed H, Brhane B, Mekete K, Mamo H, et al. Plasmodium falciparum is evolving to escape malaria rapid diagnostic tests in Ethiopia. Nat Microbiol. 2021;6:1289–99.
Alemayehu GS, Lopez K, Dieng CC, Lo E, Janies D, Golassa L. Evaluation of PfHRP2 and PfLDH malaria rapid diagnostic test performance in Assosa Zone. Ethiopia Am J Trop Med Hyg. 2020;103:1902–9.
Herman C, Huber CS, Jones S, Syeinhardt L, Plucinski MM, Lemoine JF, et al. Multiplex malaria antigen detection by bead-based assay and molecular confirmation by PCR shows no evidence of Pfhrp2 and Pfhrp3 deletion in Haiti. Malar J. 2019;18:380.
Parr JB, Anderson O, Juliano JJ, Meshnick SR. Streamlined, PCR-based testing for pfhrp2- and pfhrp3-negative Plasmodium falciparum. Malar J. 2018;17:137.
WHO. Guidelines for malaria. Geneva: World Health Organization, 2021.
WHO. Master protocol for surveillance of pfhrp2/3 deletions and bio banking to support future research. Geneva: World Health Organization 2020.
Cunningham J, Jones S, Gatton ML, Barnwell JW, Cheng Q, Chiodini P, et al. A review of the WHO malaria rapid diagnostic test product testing programme (2008–2018): performance, procurement and policy. Malar J. 2019;18:387.
Coldiron ME, Assao B, Langendorf C, Makombe NS, Ciglenecki I, De TR, et al. Clinical diagnostic evaluation of HRP2 and pLDHȁ4based rapid diagnostic tests for malaria in an area receiving seasonal malaria chemoprevention in Niger. Malar J. 2019;18:443.
WHO. Malaria rapid diagnostic test performance results of WHO product testing of malaria RDTs: round 3 (2010–2011). Geneva: World Health Organization.
Ali IM, Nji AM, Bonkum JC, Moyeh MN, Carole GF, Efon S, et al. Diagnostic accuracy of CareStart™ malaria HRP2 and SD Bioline Pf/PAN for malaria in febrile outpatients in varying malaria transmission settings in Cameroon. Diagnostics (Basel). 2021;11:1556.
Tetteh M, Dwomoh D, Asamoah A, Kupeh EK, Malm K, Nonvignon J. Impact of malaria diagnostic refresher training programme on competencies and skills in malaria diagnosis among medical laboratory professionals: evidence from Ghana 2015–2019. Malar J. 2021;20:255.
Albertini A, Lee E, Coulibaly SO, Sleshi M, Faye B, Mationg ML, et al. Malaria rapid diagnostic test transport and storage conditions in Burkina Faso, Senegal. Ethiopia and the Philippines Malar J. 2012;11:406.
Abba K, Deeks JJ, Olliaro PL, Naing CM, Jackson SM, Takwoingi Y, et al. Rapid diagnostic tests for diagnosing uncomplicated P falciparum malaria in endemic countries. Cochrane Database Syst Rev. 2011;2011:CD008122.
Gatton ML, Chaudhry A, Glenn J, Wilson S, Ah Y, Kong A, et al. Impact of Plasmodium falciparum gene deletions on malaria rapid diagnostic test performance. Malar J. 2020;19:392.
Hendriksen IC, Mtove G, Pedro AJ, Gomes E, Silamut K, Lee SJ, et al. Evaluation of a PfHRP2 and a pLDH-based rapid diagnostic test for the diagnosis of severe malaria in 2 populations of African children. Clin Infect Dis. 2011;52:1100–7.
Acknowledgements
The author duly acknowledges the Ethiopian Public Health Institute (EPHI), Ministry of Health of Ethiopia (MoH), University of North Carolina at Chapel Hill (UNC) and Addis Ababa University (AAU) for supporting the study. We thank Jane Cunningham from World Health Organizations (WHO), Geneva and Eric Rogier from Center for Disease Prevention and Control (CDC) for their technical and laboratory work support. We would also like to thank the study participants who volunteered to be part of the study.
Funding
This study was funded by the Global fund for AIDS, Tb and malaria through the Ministry of Health (MoH) (Grant number—EPHI 5405).
Author information
Authors and Affiliations
Contributions
SMF, HM, BP, GT, GT, JBP and HS designed the study. SM drafted the manuscript. BG, HM, DN, SMF, DG and MH conducted the field study, drafted and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethical approval from the scientific and ethical review board of Ethiopian Public Health Institute (protocol approval number—EPHI-IRB-033-2017 and EPHI-6.13/596 28 Jan 2020). All study participants had provided signed consent to be part of the study.
Consent for publication
All authors have given their consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Feleke, S.M., Gidey, B., Mohammed, H. et al. Field performance of Plasmodium falciparum lactate dehydrogenase rapid diagnostic tests during a large histidine-rich protein 2 deletion survey in Ethiopia. Malar J 21, 236 (2022). https://doi.org/10.1186/s12936-022-04257-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04257-9