Abstract
Background
Over the past two decades, Zanzibar substantially reduced malaria burden. As malaria decreases, sustainable improvements in control interventions may increasingly depend on accurate knowledge of malaria risk factors to further target interventions. This study aimed to investigate the risk factors associated with malaria infection in Zanzibar.
Methods
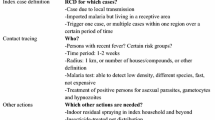
Surveillance data from Zanzibar’s Malaria Case Notification system from August 2012 and December 2019 were analyzed. This system collects data on malaria cases passively detected and reported by all health facilities (index cases), and household-based reactive case detection (RCD) activities linked to those primary cases. All members of households of the index cases were screened for malaria using a malaria rapid diagnostic test (RDT). Individuals with a positive RDT were treated with artemisinin-based combination therapy. Univariate and multivariate logistic regression analyses were done to investigate the association between RDT positivity among the household members and explanatory factors with adjustment for seasonality and clustering at Shehia level.
Results
A total of 30,647 cases were reported of whom household RCD was completed for 21,443 (63%) index case households and 85,318 household members tested for malaria. The findings show that younger age (p-value for trend [Ptrend] < 0.001), history of fever in the last 2 weeks (odds ratio [OR] = 35.7; 95% CI 32.3–39.5), travel outside Zanzibar in the last 30 days (OR = 2.5; 95% CI 2.3–2.8) and living in Unguja (OR = 1.2; 95% CI 1.0–1.5) were independently associated with increased odds of RDT positivity. In contrast, male gender (OR=0.8; 95% CI 0.7–0.9), sleeping under an LLIN the previous night (OR = 0.9; 95% CI 0.7–0.9), having higher household net access (Ptrend < 0.001), and living in a household that received IRS in the last 12 months (OR = 0.8; 95% CI 0.7–0.9) were independently associated with reduced odds of RDT positivity. A significant effect modification of combining IRS and LLIN was also noted (OR = 0.7; 95% CI 0.6–0.8).
Conclusions
The findings suggest that vector control remains an important malaria prevention intervention: they underscore the need to maintain universal access to LLINs, the persistent promotion of LLIN use, and application of IRS. Additionally, enhanced behavioural change and preventive strategies targeting children aged 5–14 years and travellers are needed.
Similar content being viewed by others
Background
Over the past two decades, Zanzibar substantially reduced malaria burden, with parasite prevalence decreasing from more than 30% in 2005 to 0.2% in 2017 [1]. These gains followed the introduction and rapid scale-up of malaria rapid diagnostic tests (RDTs), artemisinin-based combination therapy (ACT), long-lasting insecticidal nets (LLINs) and indoor residual spraying (IRS) of households with insecticide [2, 3]. The application of malaria control interventions in Zanzibar was aimed at achieving universal coverage and a recent impact evaluation comparing malaria incidence before and after inception of interventions suggested that this approach resulted in rapid declines of malaria [4]. Building on these achievements, Zanzibar is now pursuing malaria elimination by 2023 by maintaining high population-level coverage of malaria interventions, as well as by reinforcing malaria surveillance to actively investigate and classify 100% of confirmed malaria cases [5].
Numerous studies in Africa have examined the association of various demographic and behavioural factors with malaria outcomes. These studies have found that adolescent age, male gender, not sleeping under an LLIN the previous night, and the presence of fever in the 2 weeks preceding the study were positively associated with malaria infection [6, 7]. Similarly, several studies have shown LLIN ownership and use, and/or the application of IRS to be associated with a significant protective effect against malaria infection [6,7,8,9]. A recent literature review and meta-analysis of 22 studies investigating travel as a risk factor for malaria infection in sub-Saharan Africa showed that travel—within as well as to and from another country—was an important risk factor in many settings [10].
As malaria decreases, sustainable improvements in prevention and control interventions may increasingly depend on accurate knowledge of malaria risk factors. For Zanzibar to accelerate towards malaria elimination, it is crucial to obtain detailed knowledge of risk factors associated with malaria infection. Such knowledge will help to confirm whether currently implemented preventive and control measures are effective, as well as indicate programmatic areas where additional efforts should be targeted or reinforced.
Methods
Study setting and data sources
The archipelago of Zanzibar is located between longitudes 39.19793 and latitudes –6.16394, 25–50 km off the east coast of the Tanzania mainland in the Indian Ocean. There are two main islands—Pemba and Unguja—which cover a total land area of 2461 km2 and have an estimated population of 1,303,569 people [11]. There are two main rainfall seasons, a primary (March–May) and a secondary (November–December) season; rainfall is at its lowest in July. Both rainfall seasons are followed by peak malaria transmission seasons, with the highest malaria case count observed in the March–May rainfall season. A cross-sectional analysis of routine data collected by Zanzibar’s Malaria Case Notification (MCN) system between August 2012 and December 2019 was conducted. The MCN system was established in August 2012 with the goal to collect data from all passively detected malaria cases (which we define as index cases); it started in 52 public health facilities and has since progressively scaled-up to 189 public and 124 private health facilities. Case-based follow-up and reactive case detection (RCD) activities, including household-based screening and treatment (HSaT), are linked to index cases through the Coconut surveillance platform (https://coconutsurveillance.org/). Figure 1 (map) shows the location of the households of individuals included in the analysis between 2012 and 2019.
Data collection
The MCN system collects and reports details of individual malaria cases passively diagnosed by microscopy or RDT at health facilities in real-time using mobile phones and Android tablets to a central database. Once the Council Malaria Surveillance Officer (CMSO) is notified by the health facility worker, surveillance data are collected using an electronic, standardized questionnaire completed by CMSO during routine reactive case follow-up and detection at households of index cases. Household members are revisited if not found at their households during the first household visit. The goal of RCD is to test all household members of the index cases for malaria infection, regardless of presence or absence of symptoms, using RDTs. In most cases and years, the SD Bioline® HRP2/pLDH RDT from Standard Diagnostics, Giheung-ku, Republic of Korea, was used, others used are First Response® Malaria Antigen pLDH/HRP2 Combo card test from Premier Medical Corporation Private Limited, Gujarat, India and Paracheck® Pf—Rapid Test for P. falciparum Malaria Device (Ver. 3) from Orchid Biomedical Systems, Goa, India); members with a positive RDT result are treated with ACT following the national malaria diagnosis and treatment guidelines [12]. The specific variables collected are individual factors (i.e., age, gender, self-reported history of travel in the last 30 days, self-reported history of fever in the last 2 weeks, RDT positivity, and LLIN use the previous night); household factors (i.e., number of people residing in the household, number of household LLINs, and IRS application in the last 12 months); and geographical factors (i.e., household geolocation and weekly rainfall). During the study period, rainfall data were obtained from 11 meteorological stations managed by Zanzibar’s Tanzania Meteorological Agency, with rainfall data measured in millimetres (mm) and recorded daily.
Inclusion and exclusion criteria
Inclusion criteria included the index case’s household members identified during routine RCD efforts (i.e., through follow-up of index cases) and tested for malaria infection with an RDT. Individuals were excluded from the analysis if they had missing data for any of the socio-demographic and clinical variables (i.e., individual factors) collected during the RCD efforts. Figure 2 shows the breakdown of included and excluded individuals in the analysis.
Data analysis
Data analysis was performed using STATA (Version 16, College Station, TX, USA). Net access was defined as the proportion of population with access to LLIN within the household, where an intermediate variable “potential LLIN users” was generated by multiplying the reported number of LLINs in each household by a factor of 2 and divided by the number of household members [13], and a cut-off of ≥ 80% was applied to define universal coverage. Daily rainfall data were aggregated into weekly district-level rainfall data, which was transformed into a continuous variable in 10 mm increments [9]. To account for the lag time between rainfall and malaria cases, we applied the rainfall data for the previous 9 weeks to the current week [14].
Univariate and multivariable logistic regression analyses were conducted to assess the association of RDT positivity and explanatory factors (i.e., age, gender, self-reported fever, net access, travel history, household characteristics, zone, and weekly rainfall) accounting for clustering of cases at Shehia (smallest administrative unit) level. The month of household reactive case investigation was included in the multivariable logistic regression to account for variability arising from malaria seasonality. A backward stepwise multiple logistic regression was used to identify independent risk factors for RDT positivity while controlling for potential confounders; the interaction between IRS and LLIN use was also assessed. Lastly, multicollinearity of the model was assessed using variance inflation factor (VIF) for the independent variables, with a VIF less than 5 indicating the model is not biased by multicollinearity of its independent variables.
Results
Characteristics of study population
Table 1 summarizes the number of index cases reported, case investigation, household follow-up and household members tested while Fig. 2 shows the number of individuals included/excluded in the analysis. Between August 2012 and December 2019, 30,647 index malaria cases were reported by health facilities through the MCN system; overall, an index case investigation and household RCD was completed for 21,443 (63%) index case households (Table 1). In these 21,443 index case households, 85,318 individuals were investigated, of whom varying numbers were excluded from the analyses due to missing malaria test, socio-demographic and clinical data (Fig. 2). Among the 82,021 individuals with malaria test results, the majority were: malaria negative (95.3%); female (51.7%); and living on Unguja Island (74.1%). The mean (standard deviation [sd]) age was 21.7 (17.0) years. Out of 21,443 households, 71.9% reported having received IRS in the previous year. Overall, the median weekly rainfall was 7.7 mm (inter quartile range, IQR: 0.0–31.4 mm).
Univariate analysis
Factors significantly associated with increased odds of RDT positivity were younger age (p-value for trend [Ptrend]< 0.001); self-reported history of fever during the last 2 weeks (odds ratio [OR] = 32.1; 95% CI 29.3–35.1); history of travel outside Zanzibar during the last 30 days (OR = 2.3; 95% CI 2.1–2.4); having more people in the household who travelled outside Zanzibar during the last 30 days (Ptrend < 0.001), and living on Unguja Island (OR = 1.2; 95% CI 1.0–1.4). Factors significantly associated with reduced odds of RDT positivity were being male (OR = 0.9; 95% CI 0.8–0.9); sleeping under an LLIN the previous night (OR = 0.7; 95% CI 0.6–0.7); higher household net access (Ptrend < 0.001); and living in a household that received IRS in the last 12 months (OR = 0.8; 95% CI 0.7–0.9)) (Table 2).
Multivariate analysis
The VIF was 1.9, suggesting low correlation between the independent variables (explanatory factors). Factors independently associated with increased odds of malaria positivity were younger age (Ptrend < 0.001); self-reported history of fever during the last 2 weeks (OR = 35.7; 95% CI 32.3–39.5); history of travel outside Zanzibar during the last 30 days (OR = 2.5; 95% CI 2.3–2.8); and living on Unguja Island (OR = 1.2; 95% CI 1.0–1.5). Factors independently associated with reduced odds of RDT positivity were being male (OR = 0.8; 95% CI 0.7–0.9); having higher household net access (Ptrend < 0.001); sleeping under an LLIN the previous night (OR = 0.9; 95% CI 0.7–0.9); and living in a household that received IRS in the last 12 months (OR = 0.8; 95% CI 0.7–0.9). There was significant effect modification when IRS in the last 12 months and sleeping under an LLIN the previous night were combined (OR = 0.7; 95% CI 0.6–0.8) (Table 3).
Discussion
This study investigated factors associated with malaria infection (as measured by RDT positivity) among the general population living in households where malaria cases had been detected passively when attending public or private health facilities in Zanzibar. The findings of this study suggest that age, history of fever during the last 2 weeks and history of travel outside Zanzibar during the last 30 days, and living on Unguja Island were independently associated with increased odds of RDT positivity. On the other hand, male gender, sleeping under an LLIN the previous night, higher household net access, living in a household that received IRS in the previous 12 months, as well as combining IRS in the last 12 months and sleeping under an LLIN the previous night were independently associated with reduced odds of RDT positivity.
Age was an important factor within the model, with children aged 5–14 years being at greatest risk of malaria infection. Malaria prevalence in children under 5 years of age has decreased in Tanzania in recent years [15], and other studies in mainland Tanzania suggest the risk of malaria infection is now higher in school-aged children compared to children under 5 years of age [6, 16]. The finding of this study might partially be explained by the association between age and those who slept under an LLIN the previous night, with a lower proportion of children aged 5–14 years (55.2%) and young adults aged 15–24 years (47.5%) having been observed to sleep under LLINs, compared to children < 5 years [6, 9, 17]. Given their higher odds of having a positive RDT result, targeting interventions to improve LLIN access and use in children aged 5–14 years and young adults aged 15–24 years will thus be important in Zanzibar, since these age groups appear to be at greater risk of infection and are likely to contribute to on-going malaria transmission. Our analysis also showed that males had reduced odds of having a positive RDT result. Typically, an increased, gender-associated risk for a vector-borne disease such as malaria suggests gender-related differences in behaviour (e.g., night time work or leisure activities) [18]. It is likely that the reactive case detection through HSaT was systematically missing males with increased risk of malaria because only residents present at time of DMSO visit are tested., Nonetheless, further studies are needed to investigate specific factors that could explain the higher odds of malaria RDT positivity among females observed in our study.
As reported previously [8, 16, 19, 20], history of fever during the last 2 weeks was significantly associated with having a positive RDT result. While self-reported fever as a proxy for symptomatic malaria infection is prone to recall and/or reporting bias and thus lacks both the sensitivity and specificity, particularly in elimination settings [20, 21], the finding suggests there is a subset of the population who do not present to health facilities when they experience malaria symptoms such as fever. Therefore, persistent messaging on recognizing malaria symptoms and prompting care-seeking behaviour at health facilities is needed even in a low transmission setting such as Zanzibar. The finding also reinforces the continued need for timely RCD, including the testing of all household members in index case households and possibly neighbouring households with or without malaria symptoms.
The results of this study confirm prior studies showing that individuals who travelled outside Zanzibar during the last 30 days had increased odds of a positive RDT result at the time of the household investigations [10]. Malaria infection associated with travel (“malaria importation”) is frequently considered a concern in low transmission or elimination settings [22,23,24,25]. There is evidence that the majority of people travelling outside Zanzibar head to malaria endemic areas on the Tanzania mainland [23]. Therefore, implementing control measures to prevent infection among Zanzibaris visiting the mainland, as well as timely detection of travel-associated malaria cases and controlling onward transmission will be key to sustaining the low malaria burden and progressing towards malaria elimination in Zanzibar. Several approaches to limit the size and impact of travel-associated malaria could be considered, including targeting information and education messaging to potential travellers regarding the risks of malaria when travelling, malaria symptomatology, and the possible approaches for individual protection. Advice for travellers to malaria endemic locations could include recommendations to sleep under an LLIN every night, use mosquito repellents, and possibly take anti-malarial chemoprophylaxis depending on the travel destination and malaria risk. An approach to early detection for travel-associated malaria might involve screening every person arriving at key border entry points using ultra-sensitive diagnostic tests such loop-mediated isothermal amplification polymerase chain reaction, and when clinically appropriate treating or referring positive individuals. Such approach could also reinforce malaria surveillance and education on malaria prevention among travellers at these entry points.
The reduced odds of RDT positivity independently associated with LLIN access and use shown here adds to the vast body of evidence supporting the effectiveness of LLIN in their protection against malaria and other vector-borne diseases [26]. This study also found that increased availability of LLINs in households was associated with a reduced odd of RDT positivity, with universal coverage (net access ≥ 80%) having the greatest protective effect [27]. Nonetheless, having access to LLINs at household level is not sufficient, and approaches to encourage at-risk populations to consistently sleep under an LLIN, even in a low transmission setting like Zanzibar, are essential.
The protective effect of IRS reported in this study was within the range reported by other studies [19, 28, 29]. The study findings suggest that IRS reduces the risk of malaria infection in the household; however, IRS operations are expensive and require considerable human resources. IRS operations in Zanzibar started in 2006, with different classes of insecticides used over the past 14 years [30]. To mitigate programmatic costs and limit the expansion of insecticide resistance, Zanzibar has shifted from a blanket IRS approach used between 2006 and 2012 to a more targeted and focal approach from 2015 onwards, whereby only areas experiencing a high number of cases and malaria incidence are prioritized.
Combining IRS and LLINs has increasingly become a common approach to control malaria in sub-Saharan Africa. This study provides further evidence of the added benefit offered to individuals when combining IRS and LLINs [31, 32]. While people who lived in households where IRS was applied in the last 12 months were less likely to be RDT positive compared to those who were not living in households where IRS has been applied, regardless of whether they slept under a LLIN or not, they were even less likely to test RDT positive if sleeping under an LLIN. This suggests that even in low transmission settings, the possibility of combining these two vector control interventions is effective.
This study has a number of potential limitations. Firstly, the analysis included members living in the same households as passively detected malaria cases (index cases); therefore, it is expected that this population may be at greater risk of malaria compared to the general population in Zanzibar. Secondly, only two thirds of the 30,647 passively detected cases were followed-up for HSaT; therefore, this may be a source of bias since most of the index cases lost-to-follow-up were detected during the peak malaria transmission season. Thirdly, RDTs’ have a limited sensitivity and are likely to miss a large proportion of infections, since in Zanzibar’s elimination setting most of these are sub-clinical, low-parasite density infections [21]. The RDTs’ low sensitivity during RCD is a potential source of bias because they are designed to identify symptomatic malaria cases that are typically high-density infections. This low RDT sensitivity has broader programmatic implications, with Zanzibar possibly having to consider the use of more sensitive diagnostics (e.g., Polymerase chain reaction [PCR]), in addition to other strategies such as focal mass drug administration or seasonal malaria chemoprevention, to eliminate malaria [3]. Finally, a fifth of the individuals with malaria test results were missing one or more explanatory variable; however, sensitivity analysis showed that this missingness was not a source of bias.
Conclusions
This study has identified risk factors associated with malaria infection (as measured by RDT positivity) that could be addressed through increased surveillance and targeted interventions. This study found that between 2012 and 2019 children aged 5–14 years, females, residents of Unguja and residents who travel outside of Zanzibar had greater odds of having a positive RDT result.
These findings suggest that even in a low transmission setting like Zanzibar, vector control remains an important malaria prevention intervention and underscores the need to maintain universal access to LLIN, persistent promotion of LLIN use, and IRS. In addition to continued effective coverage and use of vector control interventions, enhanced behavioural change and preventive strategies specifically targeting children aged 5–14 years and travellers could enhance Zanzibar’s progress towards malaria elimination.
Availability of data and materials
The datasets used and /or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACT :
-
Artemisinin-based combination therapy
- CI :
-
Confidence interval
- CMSO :
-
Council malaria surveillance officer
- HSaT :
-
Household-based screening and treatment
- IRS :
-
Indoor residual spraying
- IQR :
-
Inter quartile range
- LLIN :
-
Long-lasting insecticidal net
- MCN :
-
Malaria case notification (system)
- RDT :
-
Rapid diagnostic test
- OR :
-
Odds ratio
- PCR :
-
Polymerase chain reaction
- RCD :
-
Reactive case detection
- VIF :
-
Variance inflation factor
- ZAHRI :
-
Zanzibar Health Research Institute
References
Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF. Tanzania Malaria Indicator Survey 2017. Dar es Salaam, Tanzania, and Rockville, Maryland, USA: MoHCDGEC, MoH, NBS, OCGS, and ICF. 2017. https://dhsprogram.com/pubs/pdf/MIS31/MIS31.pdf.
Roll Back Malaria Partnership. Global Strategic Plan, 2018–2020. 2020. https://endmalaria.org/sites/default/files/RBM-Strategic-Plan-digital-JW-220218.pdf.
Björkman A, Shakely D, Ali AS, Morris U, Mkali H, Abbas AK, et al. From high to low malaria transmission in Zanzibar—challenges and opportunities to achieve elimination. BMC Med. 2019;17:14.
Ashton RA, Bennett A, Al-Mafazy A-W, Abass AK, Msellem MI, McElroy P, et al. Use of routine health information system data to evaluate impact of malaria control interventions in Zanzibar, Tanzania from 2000 to 2015. EClinicalMedicine. 2019;12:11–9.
Zanzibar Malaria Elimination Programme. Zanzibar Malaria Elimination Strategic Plan IV 2018/19-2022/23. 2020.
Winskill P, Rowland M, Mtove G, Malima RC, Kirby MJ. Malaria risk factors in north-east Tanzania. Malar J. 2011;10:98.
Rulisa S, Kateera F, Bizimana JP, Agaba S, Dukuzumuremyi J, Baas L, et al. Malaria prevalence, spatial clustering and risk factors in a low endemic area of Eastern Rwanda: a cross sectional study. PLoS One. 2013;8:e69443.
Temu EA, Coleman M, Abilio AP, Kleinschmidt I. High prevalence of malaria in Zambezia, Mozambique: the protective effect of IRS versus increased risks due to pig-keeping and house construction. PLoS One. 2012;7:e31409.
Graves PM, Richards FO, Ngondi J, Emerson PM, Shargie EB, Endeshaw T, et al. Individual, household and environmental risk factors for malaria infection in Amhara, Oromia and SNNP regions of Ethiopia. Trans R Soc Trop Med Hyg. 2009;103:1211–20.
Ahmed S, Reithinger R, Kaptoge SK, Ngondi JM. Travel is a key risk factor for malaria transmission in pre-elimination settings in sub-Saharan Africa: a review of the literature and meta-analysis. Am J Trop Med Hyg. 2020;103:1380–7.
2012 Population and housing census. National Bureau of Statistics, Tanzania; Office of Cheif Government Statistician, Zanzibar; 2020. http://www.tzdpg.or.tz/fileadmin/documents/dpg_internal/dpg_working_groups_clusters/cluster_2/water/WSDP/Background_information/2012_Census_General_Report.pdf.
Zanzibar guidelines for malaria diagnosis and treatment. Zanzibar malaria elimination programme. Revolutionary Government of Zanzibar, Ministry of Health and Social Welfare. https://searchworks.stanford.edu/view/11527091.
Koenker H, Ricotta E, Olapeju B, Choiriyyah I. Insecticide-Treated Nets (ITN) access and use report. Baltimore, MD. PMI, VectorWorks Project, Johns Hopkins Center for Communication Programs; 2018.
Nkrumah B, Fobil J, Krefis AC, Loag W, Ranft U, Acquah S, et al. Modeling the relationship between precipitation and malaria incidence in children from a holoendemic area in Ghana. T Am J Trop Med Hyg. 2011;84:285–91.
Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF. 2017. Tanzania Malaria Indicator Survey 2017. Dar es Salaam, Tanzania, and Rockville, Maryland, USA: MoHCDGEC, MoH, NBS, OCGS, and ICF. 2010. https://dhsprogram.com/pubs/pdf/MIS31/MIS31.pdf.
Khatib RA, Chaki PP, Wang D-Q, Mlacha YP, Mihayo MG, Gavana T, et al. Epidemiological characterization of malaria in rural southern Tanzania following China-Tanzania pilot joint malaria control baseline survey. Malar J. 2018;17:292.
Tchinda VHM, Socpa A, Keundo AA, Zeukeng F, Seumen CT, Leke RGF, et al. Factors associated to bed net use in Cameroon: a retrospective study in Mfou health district in the Centre Region. http://www.panafrican-med-journal.com/content/article/12/112/full/.
Quaresima V, Agbenyega T, Oppong B, Awunyo JADA, Adu Adomah P, Enty E, et al. Are malaria risk factors based on gender? a mixed-methods survey in an urban setting in Ghana. Trop Med Infect Dis. 2021;6:161.
West PA, Protopopoff N, Rowland M, Cumming E, Rand A, Drakeley C, et al. Malaria risk factors in North West Tanzania: the effect of spraying, nets and wealth. PLoS One. 2013;8:e65787.
Carlucci JG, Blevins Peratikos M, Cherry CB, Lopez ML, Green AF, Gonzalez-Calvo L, et al. Prevalence and determinants of malaria among children in Zambézia Province, Mozambique. Malar J. 2017;16:108.
Stuck L, Fakih BS, Al-mafazy AH, Hofmann NE, Holzschuh A, Grossenbacher B, et al. Malaria infection prevalence and sensitivity of reactive case detection in Zanzibar. Int J Infect Dis. 2020;97:337–46.
Bradley J, Monti F, Rehman AM, Schwabe C, Vargas D, Garcia G, et al. Infection importation: a key challenge to malaria elimination on Bioko Island, Equatorial Guinea. Malar J. 2015;14:46.
Le Menach A, Tatem AJ, Cohen JM, Hay SI, Randell H, Patil AP, et al. Travel risk, malaria importation and malaria transmission in Zanzibar. Sci Rep. 2011;1:93.
WHO Global Malaria Programme. A framework for malaria elimination. Geneva, World Health Organization. 2017 (cited 2020 Jun 30). http://apps.who.int/iris/bitstream/10665/254761/1/9789241511988-eng.pdf.
Sturrock HJW, Hsiang MS, Cohen JM, Smith DL, Greenhouse B, Bousema T, et al. Targeting asymptomatic malaria infections: active surveillance in control and elimination. PLoS Med. 2013;10:e1001467.
Lengeler C. Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev. 2004;2:CD000363.
Ngondi JM, Graves PM, Gebre T, Mosher AW, Shargie EB, Emerson PM, et al. Which nets are being used: factors associated with mosquito net use in Amhara, Oromia and Southern Nations, Nationalities and Peoples’ Regions of Ethiopia. Malar J. 2011;10:92.
Pluess B, Tanser FC, Lengeler C, Sharp BL. Indoor residual spraying for preventing malaria. Cochrane Database Syst Rev. 2010;2010:CD006657.
Kleinschmidt I, Sharp B, Benavente LE, Schwabe C, Torrez M, Kuklinski J, et al. Reduction in infection with Plasmodium falciparum one year after the introduction of malaria control interventions on Bioko Island, Equatorial Guinea. Am J Trop Med Hyg. 2006;74:972–8.
Haji KA, Thawer NG, Khatib BO, Mcha JH, Rashid A, Ali AS, et al. Efficacy, persistence and vector susceptibility to pirimiphos-methyl (Actellic® 300CS) insecticide for indoor residual spraying in Zanzibar. Parasites Vectors. 2015;8:628.
Kleinschmidt I, Schwabe C, Shiva M, Segura JL, Sima V, Mabunda SJA, et al. Combining indoor residual spraying and insecticide-treated net interventions. Am J Trop Med Hyg. 2009;81:519–24.
Okumu FO, Moore SJ. Combining indoor residual spraying and insecticide-treated nets for malaria control in Africa: a review of possible outcomes and an outline of suggestions for the future. Malar J. 2011;10:208.
Acknowledgements
This analysis was supported by RTI International through Okoa Maisha Dhibiti Malaria (OMDM) activity (Cooperative Agreement Number: 72062118CA-00002) in collaboration with the President’s Malaria Initiative, the United States Agency for International Development and the U.S. Centers for Disease Control and Prevention.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect the views of the President’s Malaria Initiative, the United States Agency for International Development, the U.S. Centers for Disease Control and Prevention, or other employing organizations or sources of funding.
Funding
This study was made possible through support provided to the RTI International through Okoa Maisha Dhibiti Malaria (OMDM) activity (Cooperative agreement number 72062118CA-00002) by the President’s Malaria Initiative (PMI) via the United States Agency for International Development (USAID) and the U.S. Centers for Disease Control and Prevention (CDC).
Author information
Authors and Affiliations
Contributions
The study was designed by HRM, EJR and JMN. HRM, EJR and JMN undertook the analysis. HRM, EJR and JMN drafted the first versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance to undertake secondary analysis of surveillance data was granted by the Zanzibar Health Research Institute (ZAHRI) with reference number ZAHREC/03/AUG/2021/20. All personal identifiers were removed during data cleaning before analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mkali, H.R., Reaves, E.J., Lalji, S.M. et al. Risk factors associated with malaria infection identified through reactive case detection in Zanzibar, 2012–2019. Malar J 20, 485 (2021). https://doi.org/10.1186/s12936-021-04025-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-021-04025-1