Abstract
Background
Malaria is heterogeneously distributed across landscapes. Human population movement (HPM) could link sub-regions with varying levels of transmission, leading to the persistence of disease even in very low transmission settings. Malaria along the Thai–Myanmar border has been decreasing, but remains heterogeneous. This study aimed to measure HPM, associated predictors of travel, and HPM correlates of self-reported malaria among people living within malaria hotspots.
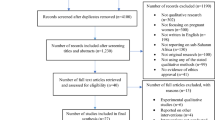
Methods
526 individuals from 279 households in two malaria hotspot areas were included in a prospective observational study. A baseline cross-sectional study was conducted at the beginning, recording both individual- and household-level characteristics. Individual movement and travel patterns were repeatedly observed over one dry season month (March) and one wet season month (May). Descriptive statistics, random effects logistic regressions, and logistic regressions were used to describe and determine associations between HPM patterns, individual-, household-factors, and self-reported malaria.
Results
Trips were more common in the dry season. Malaria risk was related to the number of days doing outdoor activities in the dry season, especially trips to Myanmar, to forest areas, and overnight trips. Trips to visit forest areas were more common among participants aged 20–39, males, individuals with low income, low education, and especially among individuals with forest-related occupations. Overnight trips were more common among males, and individual with forest-related occupations. Forty-five participants reported having confirmed malaria infection within the last year. The main place of malaria blood examination and treatment was malaria post and malaria clinic, with participants usually waiting for 2–3 days from onset fever to seeking diagnosis. Individuals using bed nets, living in houses with elevated floors, and houses that received indoor residual spraying in the last year were less likely to report malaria infection.
Conclusion
An understanding of HPM and concurrent malaria dynamics is important for consideration of targeted public health interventions. Furthermore, diagnosis and treatment centres must be capable of quickly diagnosing and treating infections regardless of HPM. Coverage of diagnosis and treatment centres should be broad, maintained in areas bordering malaria hotspots, and available to all febrile individuals.
Similar content being viewed by others
Background
Human population movement (HPM) and travel patterns are important with regard to infectious disease epidemiology. Infectious diseases such as malaria are heterogeneously distributed across landscapes, perhaps especially in low transmission settings. HPM can link sub-regions with varying levels of transmission, leading to the persistence of disease even in very low transmission settings [1, 2]. For example, very low transmission settings might achieve local elimination in the absence of being linked to high transmission settings via HPM [3, 4]. HPM has been suggested to be one factor in the failure to eliminate malaria during previous malaria eradication programs [3, 5, 6]. HPM data, when coupled with malaria epidemiological data, can help to identify potential “sources” and “sinks” of malaria parasites with direct implications for malaria control and elimination efforts [7, 8].
As in other low-transmission settings, malaria in the Greater Mekong Sub-region (GMS) is heterogeneous and patchy, with many sub-regions having little or no malaria transmission. The disease tends to cluster in border regions that have suitable environmental, ecological, socio-economic, and demographic characteristics that contribute to the persistence of malaria. For example, while malaria has been greatly reduced in Thailand over the last several decades, the disease continues to persist along international borders; one of the heaviest burdens has been along the Thai–Myanmar border. HPM within, to, and from this border area has been considered an important contributor to overall malaria epidemiology [9,10,11]. Moreover, travelling cross-border to Myanmar and/or into forest areas has been considered important with regard to the risk of malaria infection and the persistence of malaria along this international border [12,13,14,15].
Political unrest between ethnic and political groups in Myanmar has frequently led to significant cross-border population movements, and displaced minority populations have historically had increased risk of malaria infection. Human population expansions, connectivity, and environmental changes have all contributed to the risk of acquiring infection in a heterogeneous malaria landscape as well as the risk of reintroduction in places that have achieved elimination [11, 16,17,18].
Previous research on the space–time distributions of malaria along the Thai–Myanmar border indicated two persistent malaria hotspots of both Plasmodium falciparum and Plasmodium vivax incidence: one was in Tha Song Yang District, Tak Province, and another in the adjacent areas of Umphang District of Tak Province and Sangkhlaburi District of Kanchanaburi Province [19]. Malaria incidence has been decreasing, but remains heterogeneous; some sub-districts were near elimination levels, while most of sub-districts were in the pre-elimination level (< 1 case per 1000 people per year) [20]. As Thailand (and other nations of the GMS) has committed to eliminating malaria by the year 2030 [21], it will be important to have an understanding of the spatial demography (including human movement patterns) and epidemiology of endemic and surrounding areas that are prone to re-importation of parasites (e.g. with suitable environments and mosquito vector populations) [3, 22]. Thus, this study aimed to measure HPM patterns, associated predictors of travel, and HPM correlates of self-reported malaria (SRM) infections among people living within malaria hotspots on the Thai–Myanmar border.
Methods
Study design
This study began with a baseline cross-sectional study, recording both individual- and household-level characteristics. Repeated cross-sectional surveys that recorded individual movement and travel patterns were collected weekly over one dry season month (March) and one wet season month (May), with seasons defined based on Thai Meteorological Department classifications (described in more detail below).
Study site
Previous work in the region showed two persistent malaria clusters at the sub-district level: Tha Song Yang Sub-district of Tak Province (Cluster I) and Nong Lu Sub-district of Kanchanaburi Province (Cluster II). Both sub-districts were purposively selected to representative malaria hotspots in this research. Here we use the term “hotspot” to indicate an area (i.e. district) with higher than normal malaria burden. The area is mountainous and partly covered by rainforests. Generally the climate of Thailand divided into three seasons: rainy or southwest monsoon season (mid-May to mid-October), winter or northeast monsoon season (mid-October to mid-February), and summer or pre-monsoon season (mid-February to mid-May) [23]. However, in the region along the border with Myanmar the monsoon rains are more intense than in other parts of Thailand. In 2017, cumulative rainfall in this region was 1000 to 1800 mm, average temperature was 26 to 27 °C.
The total population of the study sub-districts at the end of 2017 was 39,237 people. Two villages from each sub-district were chosen, with criteria being that they must have transmission reported ≥ 6 months per year. The selected villages in Cluster I were SO and KMN and in Cluster II were SNP and WKD. The villages are located on forest fringes, in hilly-to-lower hillslope areas. All study villages are located in the Thai side (≤ 10 km.) of the international border, adjacent to Kayin State of Myanmar (Fig. 1). Clinical malaria cases in the study sites exhibit similar seasonal patterns and decreased over time. Total malaria case numbers in Cluster II were higher than Cluster I (Fig. 2).
Sample size
The sampling strategy was set up to capture normal movement patterns among people who live in malaria endemic villages on the Thai–Myanmar border. Persistent sub-district level clusters of malaria incidence were previously identified [19] and these clusters were targeted for this study. Four villages were chosen based on their location (within the identified persistent malaria clusters) and based on year-round transmission of malaria, according to local Vector Borne Disease Control Unit data (Fig. 2). The total population of the four selected villages in 2017 was 5073. Survey participants were selected by household. Previous work in the region has shown an average household size of approximately 5 individuals per house [24], leading to an estimated 1015 households across the four villages. Assuming that 50% of households will have a participant who has a trip during the study period, it would be necessary to sample 280 households in order to achieve 95% confidence level with a precision of 0.05.
Data collection and analysis
The individual- and household-level data were collected using a questionnaire at the beginning of the study period, targeting the head of household and one other family member who engages in activities which potentially involve travelling into forest areas or outside of the village. The questionnaire comprised of (1) household characteristics; number of household members, roof materials, wall materials, floor structure, and receiving indoor residual spraying (IRS) in the last year, (2) general respondent characteristics; age, gender, educational level, Thai literacy (complete listening-speaking-reading-writing skills), forest-related occupations (rice paddy field, corn and sugar cane fields, rubber plantation, fruit orchard, agricultural laborers, forestry officer, livestock), and monthly income, and (3) history of malaria infection, personal protection, and treatment behaviours. Malaria infection in this region is diagnosed in malaria posts (by rapid diagnostic test), malaria clinics, or hospitals (both by microscopy).
Movement and travel patterns were observed using a standardized daily movement form for a complete month in March (dry season) and again in May (wet season) 2018. Data included in the form included whether or not the head of household or other household participant made a trip within the previous week, whether the trip was within Thailand or to Myanmar, visited areas (i.e. other villages or forest), and the type of trip (daytrip or overnight). The form was repeatedly filled in at the end of each week (on Sunday) for four consecutive weeks during both of the study months.
Descriptive statistics (frequency, percentage, mean, and standard deviation) were used to describe travel and movement patterns. Random effects logistic regressions were used to assess potential predictors (previously listed covariates) of travel, with different regressions by travel type (day or overnight trip), times (wet or dry season), and location (within Thailand or to Myanmar, to another village or to a forest area). Random intercepts were used to account for repeat observations within individual participants and within households. Trips were aggregated at the week level and an offset was used to account for the number of trips within a week. Subsequent logistic regressions were used to determine factors that were associated with malaria infections. Model adjusted odds ratios and 95% confidence interval (AOR [95% CI]) were calculated to assess the magnitude and statistical significance of potential predictors of travel and self-reported malaria infections.
Results
Summary stats of human population movement (HPM) patterns
In total, 526 individuals from 279 households in the two cluster areas were included in the full prospective observational study, of which 249 individuals from 140 households were in the Cluster I and 277 individuals from 139 households were in the Cluster II. The individual movement data indicate daily travel destinations and travel types among individual participants by study village (Fig. 3). In both clusters, trips were more common in the dry season.
In Cluster I during the dry season, 10.04% of all participants did not leave their village while in the wet season 16.87% of all participants never left their village (Table 1). Seventy-six percent of all participants made at least one trip within the Thai side, 69.88% made trips to other villages, 72.29% made trips to forest areas, 88.35% made daytrips, and 19.28% made overnight trips in the dry season. Trips to Myanmar were similar in both dry and wet seasons (≅ 44.00%). In the wet season, more days were spent (on average, indicated by (\(\overline{d}\)) in Table 1) on each trip type, with the exception being trips to other villages.
In Cluster II, 65.34% of all participants made trips within the Thai side, 6.50% made trips to the Myanmar side, 55.23% made trips to other villages, 64.62% made daytrips, and 39.35% made overnight trips during the dry season. Trips to forest areas were similar in both seasons (≅ 49.00%). During the wet season the number of days spent on each trip type were greater than during the dry season, with the exception of trips to Myanmar (Table 1). However, most participant spent 2–4 days on each trip and trips were more frequent in the dry season (see Additional file 1).
Logistic regressions for odds of having a trip, by trip destination and duration
Logistic regressions by travel destinations
Predictors for the odds of travelling to Myanmar
During the dry season, there were more trips among people who have forest-related occupations (2.07 [1.22–3.52]), in the earlier weeks of the month (0.82 [0.73–0.93]), and in Cluster I. During the wet season, there were more trips among males (2.71 [1.52–4.83]) and among participants from Cluster I (Fig. 4).
Predictors for the odds of travelling within Thailand
Males (1.37 [1.02–1.82]) and study participants with forest-related occupations (1.66 [1.19–2.31]) were more likely to have trips within Thailand in particular in the dry season (Fig. 4).
Predictors for the odds of travelling to a forest area
During the dry season, there were more trips among people who have forest-related occupations (2.47 [1.74–3.51]), and among participants from Cluster I. In comparison to those with no education, those with ≥ high school education had half the odds of visiting the forest (0.55 [0.31–0.98]). During the wet season, there were more trips among people in the 20–39 year age group (2.09 [1.14–3.86]), male (1.52 [1.11–2.09]), forest-related occupations (1.61 [1.11–2.33]), and among participants from Cluster I. Trips to the forest were more common among people who had no education, and who had lower monthly income. In comparison to those with no education, individuals with primary school education had a 45% decrease in odds of making a forest visit (0.65 [0.44–0.96]), and those with monthly income > 5000 THB had 69% decrease in the odds of making a trip to the forest (0.31 [0.17–0.55]) (Fig. 5).
Predictors for the odds of travelling to another village
During the dry season, there were more trips among people who had monthly income > 5000 THB (1.74 [1.18–2.56]) and among participant in Cluster I. During the wet season, there were more trips among males (1.34 [1.01–1.80]) and individuals with primary school education (1.79 [1.27–2.53]) (Fig. 5).
Logistic regression by type of trip (overnight or daytrip)
Overnight trips
During the dry season, there were more overnight trips among people age < 20 years compared to those age 20–39 (0.42 [0.19–0.91]), those with ≥ high school (2.30 [1.25–4.23]), forest-related occupations (2.72 [1.64–4.51]), and among participant in Cluster II. During the wet season, there were more trips among males (1.63 [1.06–2.51]) forest-related occupations (2.50 [1.29–4.87]), and among participants in Cluster II (Fig. 6).
Daytrips
During the dry season, there were more trips among people with forest-related occupations (1.80 [1.32–2.44]), and among participants in Cluster I. During the wet season, there were more trips among people with primary school education (2.35 [1.30–4.26]), males (1.67 [1.23–2.26]), and among participants in Cluster I (Fig. 6).
Associations between duration of trip and SRM, by trip destination and type
The adjusted odds ratio and 95% confidence interval (AOR [95% CI]) indicated the increasing of the day in each trip in the dry season were more likely to increase the risk of malaria infection, especially trips to Myanmar (1.11 [1.03–1.17]), forested areas (1.08 [1.03–1.13]), and overnight trips (1.10 [1.02–1.19]). However, trips within Thailand and daytrips in the dry season also showed an association with SRM (1.05 [1.01–1.09] and 1.06 [1.02–1.11], respectively) (Table 2).
Associations between individual- and household-characteristics and SRM
There were 45 participants who reported having confirmed malaria infection(s) within the last year (see Additional file 2 for individual characteristics by study village). The majority of SRM were among participants aged 20 to 39 (42.22%), females (51.11%), those with no education (55.56%), who were not literate in Thai (73.33%), with forest-related occupations (64.44%), and with monthly income < 5000 THB (91.11%). Individuals living in houses with elevated floors (e.g. on stilts, see in Fig. 7) (0.27 [0.08–0.88]) and houses which received IRS in the last year (0.32 [0.11–0.92]) were less likely to report malaria infections (Table 3).
Association between personal protection measures and SRM
Personal protection measures among individuals with SRM were mainly using long-sleeved shirts and pants (12.17%) and smoke or fire (11.02%) as protection against mosquito bites. Approximately 16.98% did not used bed nets and 21.05% did not sleep under bed net in the last night were found in SRM. Individuals who reported using bed nets had a 64% decrease in the odds of also having a malaria infection in the past year (0.36 [0.18–0.72]) (Table 4).
The main place of malaria blood examination and treatment was malaria post and malaria clinic (88.89%). Over 50% of these individuals with SRM also reported having waited for 2–3 days from onset fever to blood examination and treatment (51.11%) (Table 5). Almost 36% reported waiting > 3 days to seek diagnosis and treatment for malaria.
Discussion
The results from this analysis show that HPM among individuals living in malaria hotspots along the Thai–Myanmar border are frequent and also revealed seasonal, socio-economic, and demographic correlates of those movement patterns. This analysis also showed associations between participant characteristics, movement types, and SRM. This information is important for ongoing control and elimination efforts for the overall region.
This analysis showed that trips were more common in the dry season, which is consistent with seasonality and synchronicity of HPM that has previously been reported [22, 25]. Travel during the rainy season is hampered by heavy rains and poor road conditions. Travel among the mostly agricultural populations in this region is also heavily dependent on the agricultural seasons, which are largely driven by the rainy season [22, 26, 27]. There is also a consistent second peak of malaria each year in some parts of the Thai–Myanmar border (evident in Fig. 2), occurring during the dry season (December to January) when travel was more frequent [28]. Infections could be acquired during travel and introduced to the village upon return. Furthermore, parasites from within villages can be exported via travel.
Travel to Myanmar has been considered a risk factor for malaria infection, given that this region in particular has had little health infrastructure (a result of decades of conflict) and therefore higher burdens of malaria [28]. In this analysis, trips to Myanmar were more common among villagers in Cluster I (Tha Song Yang District of Tak Province). The study villages in Cluster I are located immediately adjacent to Myanmar (Fig. 1), and many of the individuals living in this part of Thailand have strong cross-border community and family ties, perhaps especially for those who have relatively few occupational options on the Thai side of the border [14, 29].
Malaria in Southeast Asia (SEA) has also frequently been associated with forests [4, 12, 15], though few studies have shown an empirical relationship. Forest visits among participants in this study were more common among 20 to 39 year olds, males, individuals with low income, low education, and especially among individuals with forest-related occupations. Perhaps especially for individuals with low socio-economic status, forest products offer a means to supplement household food or economic needs [30, 31]. Forest visits may therefore be related to both socio-economic status and to risk of malaria infection in this part of SEA [4, 11, 14].
There were several statistically significant predictors of malaria infection at both the individual and household-level. Individuals who made trips into forested areas during the dry season were more likely to report malaria infections. Individuals who made frequent trips in the dry season in general (i.e. within Thailand or to Myanmar, either overnight or daytrips), were more likely to also report a malaria infection. Individuals who owned and reported using bed nets and those living in elevated houses (Fig. 7) were also less likely to report having a malaria infection. This finding with regard to elevated houses is in line with previous research that suggests mosquito vectors are more common inside ground-level houses than in houses on stilts metre [32,33,34,35,36].
This analysis also suggests that a sizeable proportion (36%) of individuals with malaria infections wait 3 or more days before seeking treatment after the onset of fever. Such delays in treatment can contribute to ongoing transmission, with gametocyte production occurring over the duration of an infection and with increased cumulative exposure to mosquito bites over longer periods of time.
Malaria in the GMS is frequently considered to be more common in adult males. In this analysis there was no significant difference by gender (detailed data by village and gender are provided in Additional file 1). There are several potential reasons for this finding. The infections in this study were self-reported and there were more female participants than males. It is possible that some males who were not present in the villages during the study period would have also reported having malaria infections. The relative number of participants reporting infections was also small (total of 45), and in a larger survey there might have been a detectable difference by gender. It is also possible that the lack of gender difference in SRM is indicative of the real situation in these study villages. When malaria clusters in adult males, it generally indicates exposure to infectious vectors outside of the home village; for example in forests, plantations, agricultural fields, or potentially in other villages that have been visited and act as a reservoir for parasites. Conversely, if a home village is acting as a parasite reservoir, and transmission occurs in village, then infections tend to be more common in both males and females, with demographic (i.e. age and gender) patterns being influenced by village population structure, transmission intensity, and immunity. While most aggregate studies and reports from this region show clustering of malaria in adult males, there are several studies showing little or no difference between males and females [15, 29]. The villages in this study were purposely selected because of their malaria burden and therefore may have different age and gender patterns when compared to areas with less malaria.
There are several limitations to this study. This study attempted to measure the general HPM patterns in malaria hotspots or clusters using community-based surveys and interviews among villagers in these clusters. Therefore, malaria cases used in this analysis were self-reported. It is possible that there is some bias in SRM. However, there are clinics in each of the study villages that regularly diagnose and treat malaria, and a malaria diagnosis is unlikely to have been poorly remembered or forgotten [37]. Other participants may have had asymptomatic infections that were never diagnosed. It is therefore possible that malaria is underestimated in this analysis. Finally, travel was recorded through cross-sectional surveys for a portion of the year (one dry season month and one wet season month). Movement patterns in other months may differ from what was recorded in this study.
Conclusion
The results from this study suggest that HPM in these malaria hotspots is common, dynamic, and varies by season. Future work should look into the potential importance of the HPM patterns with regard to malaria dynamics in this region. An understanding of HPM (including seasonal patterns in HPM) and concurrent malaria dynamics is important for consideration of targeted public health interventions. Several potential targeted interventions warrant consideration in order to reduce new infections and prevent re-importation of malaria. Vector based approaches, such as residual spraying, using bed nets or insecticide-treated clothing, could help to disrupt transmission in active foci [38, 39]. In addition, a better understanding of mosquito vector behaviour, for example peak biting times for each vector species, could help inform public health approaches. Coverage of diagnosis and treatment centres should be broad, maintained in areas bordering malaria hotspots (even when cases are few), and available to all febrile individuals. In areas with high proportions of asymptomatic infections, other interventions (such as chemoprophylaxis or targeted mass drug administration) may be warranted [40] in order to achieve malaria elimination.
Abbreviations
- AOR:
-
adjusted odds ratio
- CI:
-
confidence interval
- GMS:
-
Greater Mekong Sub-region
- HPM:
-
human population movement
- IRS:
-
indoor residual spraying
- OR:
-
odds ratio
- SEA:
-
Southeast Asia
- SRM:
-
self-reported malaria
- THB:
-
Thai Baht
References
Silal SP, Little F, Barnes KI, White LJ. Hitting a moving target: a model for malaria elimination in the presence of population movement. PLoS ONE. 2015;10:e0144990.
Ariey F, Duchemin J-B, Robert V. Metapopulation concepts applied to falciparum malaria and their impacts on the emergence and spread of chloroquine resistance. Infect Genet Evol. 2003;2:185–92.
Stoddard ST, Morrison AC, Vazquez-Prokopec GM, Paz Soldan V, Kochel TJ, Kitron U, et al. The role of human movement in the transmission of vector-borne pathogens. PLoS Neglect Trop Dis. 2009;3:e481.
Prothero RM. Malaria, forests and people in Southeast Asia. Singapore J Trop Geogr. 1999;20:76–85.
Pim M, Lisbeth H. Malaria on the move: human population movement and malaria transmission. Emerg Infect Dis J. 2000;6:103.
Jitthai N. Migration and malaria. Southeast Asian J Trop Med Public Health. 2013;44(Suppl 1):166–200 (discussion 306-167).
Prosper O, Ruktanonchai N, Martcheva M. Assessing the role of spatial heterogeneity and human movement in malaria dynamics and control. J Theoret Biol. 2012;303:1–14.
Wangdi K, Gatton ML, Kelly GC, Clements AC. Cross-border malaria: a major obstacle for malaria elimination. Adv Parasitol. 2015;89:79–107.
Richards AK, Banek K, Mullany LC, Lee CI, Smith L, Oo EK, et al. Cross-border malaria control for internally displaced persons: observational results from a pilot programme in eastern Burma/Myanmar. Trop Med Int Health. 2009;14:512–21.
Kounnavong S, Gopinath D, Hongvanthong B, Khamkong C, Sichanthongthip O. Malaria elimination in Lao PDR: the challenges associated with population mobility. Infect Dis Poverty. 2017;6:81.
Bhumiratana A, Intarapuk A, Sorosjinda-Nunthawarasilp P, Maneekan P, Koyadun S. Border malaria associated with multidrug resistance on Thailand–Myanmar and Thailand–Cambodia borders: transmission dynamic, vulnerability, and surveillance. Biomed Res Int. 2013;2013:363417.
Parker DM, Carrara VI, Pukrittayakamee S, McGready R, Nosten FH. Malaria ecology along the Thailand–Myanmar border. Malar J. 2015;14:388.
Nguitragool W, Mueller I, Kumpitak C, Saeseu T, Bantuchai S, Yorsaeng R, et al. Very high carriage of gametocytes in asymptomatic low-density Plasmodium falciparum and P. vivax infections in western Thailand. Parasit Vectors. 2017;10:512.
Panvisavas S. Poverty and malaria: a study in a Thai–Myanmar border area. Southeast Asian J Trop Med Public Health. 2001;32:608–14.
Tipmontree R, Fungladda W, Kaewkungwal J, Tempongko MA, Schelp FP. Migrants and malaria risk factors: a study of the Thai–Myanmar border. Southeast Asian J Trop Med Public Health. 2009;40:1148–57.
World Health Organization. Population mobility and malaria. Geneva: World Health Organization; 2017.
Cui L, Yan G, Sattabongkot J, Cao Y, Chen B, Chen X, et al. Malaria in the Greater Mekong Subregion: heterogeneity and complexity. Acta Trop. 2012;121:227–39.
Pindolia DK, Garcia AJ, Wesolowski A, Smith DL, Buckee CO, Noor AM, et al. Human movement data for malaria control and elimination strategic planning. Malar J. 2012;11:205.
Saita S, Silawan T, Parker DM, Sriwichai P, Phuanukoonnon S, Sudathip P, et al. Spatial heterogeneity and temporal trends among Thais in malaria clusters on the Thai–Myanmar border (2012–2017): a retrospective observational study. Unpublished. 2018.
WHO. A framework for malaria elimination. Geneva: World Health Organization; 2017.
WHO. Strategy for malaria elimination in the Greater Mekong Subregion: 2015–2030. Geneva: World Health Organization; 2015.
Searle KM, Lubinda J, Hamapumbu H, Shields TM, Curriero FC, Smith DL, et al. Characterizing and quantifying human movement patterns using GPS data loggers in an area approaching malaria elimination in rural southern Zambia. R Soc Open Sci. 2017;4(5):170046.
Thai Meteorological Department. The climate of Thailand. https://www.tmd.go.th/en/archive/thailand_climate.pdf. Accessed 22 Oct 2018.
Parker DM, Wood JW, Tomita S, DeWitte S, Jennings J, Cui L. Household ecology and out-migration among ethnic Karen along the Thai–Myanmar border. Demogr Res. 2014;30:1129–56.
Parker DM. Human migration and spatial synchrony: spatial patterns in temporal trends. In: Howell FM, Porter JR, Matthews SA, editors. Recapturing space: new middle-range theory in spatial demography. Cham: Springer; 2016. p. 325–51.
Guyant P, Canavati SE, Chea N, Ly P, Whittaker MA, Roca-Feltrer A, et al. Malaria and the mobile and migrant population in Cambodia: a population movement framework to inform strategies for malaria control and elimination. Malar J. 2015;14:252.
Peeters Grietens K, Gryseels C, Dierickx S, Bannister-Tyrrell M, Trienekens S, Uk S, et al. Characterizing types of human mobility to inform differential and targeted malaria elimination strategies in northeast Cambodia. Sci Rep. 2015;5:16837.
Zaw MT, Thant M, Hlaing TM, Aung NZ, Thu M, Phumchuea K, et al. Asymptomatic and sub-microscopic malaria infection in Kayah State, eastern Myanmar. Malar J. 2017;16:138.
Parker DM, Matthews SA, Yan G, Zhou G, Lee M-C, Sirichaisinthop J, et al. Microgeography and molecular epidemiology of malaria at the Thailand–Myanmar border in the malaria pre-elimination phase. Malar J. 2015;14:198.
Rasolofoson RA, Hanauer MM, Pappinen A, Fisher B, Ricketts TH. Impacts of forests on children’s diet in rural areas across 27 developing countries. Sci Adv. 2018;4:e2853.
Siebert SF, Belsky JM. Some socioeconomic and environmental aspects of forest use by lowland farmers in Leyte, Philippines and their implications for agricultural development and forest management. Philippine Q Cult Soc. 1985;13:282–96.
Charlwood JD, Pinto J, Ferrara PR, Sousa CA, Ferreira C, Gil V, et al. Raised houses reduce mosquito bites. Malar J. 2003;2:45.
May JM. The ecology of human disease. Ann N Y Acad Sci. 1960;84:789–94.
Liu JX, Bousema T, Zelman B, Gesase S, Hashim R, Maxwell C, et al. Is housing quality associated with malaria incidence among young children and mosquito vector numbers? evidence from Korogwe, Tanzania. PLoS ONE. 2014;9:e87358.
Tusting LS, Ippolito MM, Willey BA, Kleinschmidt I, Dorsey G, Gosling RD, et al. The evidence for improving housing to reduce malaria: a systematic review and meta-analysis. Malar J. 2015;14:209.
Ondiba IM, Oyieke FA, Ong’amo GO, Olumula MM, Nyamongo IK, Estambale BBA. Malaria vector abundance is associated with house structures in Baringo County, Kenya. PLoS ONE. 2018;13:e0198970.
Maheu-Giroux M, Casapía M, Gyorkos TW. On the validity of self-reports and indirect reports to ascertain malaria prevalence in settings of hypoendemicity. Soc Sci Med. 2011;72:635–40.
Crawshaw AF, Maung TM, Shafique M, Sint N, Nicholas S, Li MS, et al. Acceptability of insecticide-treated clothing for malaria prevention among migrant rubber tappers in Myanmar: a cluster-randomized non-inferiority crossover trial. Malar J. 2017;16:92.
Banks SD, Murray N, Wilder-Smith A, Logan JG. Insecticide-treated clothes for the control of vector-borne diseases: a review on effectiveness and safety. Med Vet Entomol. 2014;28:14–25.
Landier J, Parker DM, Thu AM, Lwin KM, Delmas G, Nosten FH, et al. Effect of generalised access to early diagnosis and treatment and targeted mass drug administration on Plasmodium falciparum malaria in Eastern Myanmar: an observational study of a regional elimination programme. Lancet. 2018;391:1916–26.
Authors’ contributions
SS, WP, TS, SP, PS, LJW and DMP contributed to the conception and design of the study. SS, PS, and SP conducted the data collection. SS, DMP, and WP performed the data analysis and drafted manuscript. TS, DMP, LJW, PS, and WP critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Acknowledgements
We gratefully acknowledge the Ministry of Public Health, Thailand for providing and allowing use of the national malaria database. We also thank the staff from the Vector-Borne Disease Units 2.3.1 (Tha Song Yang) and 5.1.9 (Sangkhlaburi), the Department of Disease Control and the International Centers of Excellence for Malaria Research (ICEMR) project for consulting and providing useful suggestions during data collection. Finally, we also would like to thank the staff of the Mahidol-Oxford Tropical Medicine Research Unit Department of Tropical Medicine, and the Department of Population Health and Disease Prevention, University of California, Irvine for support.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethical approval for this study was received from the Ethics Committee of the Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand. Number of Certificate of Ethic Approval is MUTM 2018-007-01.
Funding
This study was funded by the Faculty of Public Health, Thammasat University, Thailand (Grant Number T.LP.3/2013). Also, this study was part of the Wellcome-Trust Major Overseas Programme in SE Asia (Grant Number 106698/Z/14/Z).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1.
Histogram of number of days spent in trips.
Additional file 2.
Counts of people with SRM by gender and village.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Saita, S., Pan-ngum, W., Phuanukoonnon, S. et al. Human population movement and behavioural patterns in malaria hotspots on the Thai–Myanmar border: implications for malaria elimination. Malar J 18, 64 (2019). https://doi.org/10.1186/s12936-019-2704-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-019-2704-3