Abstract
Background
To assess the effect on malaria prevalence, village specific monthly administrations of pyrimethamine, chlorproguanil, chloroquine or placebo were given to children in four previously treatment-naïve Liberian villages, 1976–78. Plasmodium falciparum in vivo resistance developed to pyrimethamine only. Selection of molecular markers of P. falciparum resistance after 2 years of treatment are reported.
Methods
Blood samples were collected from 191 study children in a survey in 1978. Polymorphisms in pfcrt, pfmdr1, pfdhfr, pfdhps, pfmrp1 and pfnhe1 genes were determined using PCR-based methods.
Results
Pfcrt 72–76 CVIET was found in one chloroquine village sample, all remaining samples had pfcrt CVMNK. Pfmdr1 N86 prevalence was 100%. A pfmdr1 T1069ACT→ACG synonymous polymorphism was found in 30% of chloroquine village samples and 3% of other samples (P = 0.008). Variations in pfnhe1 block I were found in all except the chloroquine treated village (P < 0.001). Resistance associated pfdhfr 108N prevalence was 2% in the pyrimethamine village compared to 45–65% elsewhere, including the placebo village (P = 0.001).
Conclusions
Chloroquine treatment possibly resulted in the development of pfcrt 72–76 CVIET. Selection of pfmdr1 T1069ACG and a pfnhe1 block 1 genotypes indicates that chloroquine treatment exerted a selective pressure on P. falciparum. Pyrimethamine resistance associated pfdhfr 108N was present prior to the introduction of any drug. Decreased pfdhfr 108N frequency concurrent with development of pyrimethamine resistance suggests a non-pfdhfr polymorphisms mediated resistance mechanism.
Similar content being viewed by others
Background
Plasmodium falciparum has historically shown considerable ability to develop resistance to antimalarial drugs. Increased malaria specific morbidity and mortality have been associated with development and spread of quinine (QN), chloroquine (CQ) and sulfadoxine–pyrimethamine (SP) resistance. Reports of resistance to the currently recommended artemisinin-based combination therapy are consequently of major concern and highlight the importance of understanding the evolution of drug resistance [1–6].
At least fifteen single nucleotide polymorphisms (SNP) in the P. falciparum chloroquine resistance transporter (pfcrt) gene have been associated with CQ resistance in field isolates [7–9]. Specific haplotypes at positions 72–76 have been linked to regional evolution of CQ resistance and the 76T allele appears essential for resistance [10–12]. Drug resistance associated SNPs have also been identified in the multidrug resistance gene 1 (pfmdr1) including N86Y, Y184F, S1034C, N1042D, F1226Y and D1246Y. Various combinations of these SNPs have been shown to modulate levels of drug resistance/tolerance to QN, CQ, amodiaquine, mefloquine and lumefantrine [13].
The P. falciparum Na+/H+ exchanger 1 gene (pfnhe1) has been associated with QN resistance [14, 15]. Specifically, >1 DNNND repeat and one DDNHNDNHNND repeat in the coding microsatellite ms4760 have been associated with reduced in vivo QN sensitivity [14, 16, 17]. The function of pfnhe1 has not been fully determined, but it has been proposed that it actively effluxes protons to maintain a pH of 7.4 within the parasite [18]. Pfnhe1 has also been suggested to play a role in CQ resistance [19, 20], but this was subsequently disputed [21, 22].
Pyrimethamine (PYR) resistance has been associated with polymorphisms A16V, N51I, C59R, S108N/T and I164L in P. falciparum dihydrofolate reductase (pfdhfr). Typically, an initial S108N change that is considered to be essential for PYR resistance occurs, causing a 7- to 50-fold increase of IC 50 in vitro. Accumulation of additional SNPs further increases IC 50 [23, 24]. Similarly, P. falciparum dihydropteroate synthase (pfdhps) SNPs S436F/A, A437G, K540E, A581G and A613S have been associated with sulphadoxine resistance. The A437G substitution appears to be the first step for resistance to sulphadoxine and addition of 540E, 436F/A, 581G and 613S further enhance resistance [25]. Quintuple pfdhfr 51I/59R/108N and pfdhps 437G/540E have been shown to result in highly sulphadoxine–pyrimethamine (SP) resistant parasites [26, 27]. The R1466K SNP of P. falciparum multi drug resistance protein 1 (pfmrp1) has also been associated with recrudescence after treatment with SP [28].
The aim of this study was to determine possible early P. falciparum in vivo selection of genetic markers associated with antimalarial drug resistance after repeated exposure to CQ, PYR or chlorproguanil (CPGN). A large field study conducted between 1976 and 1978 in four villages in northern Liberia where virtually no anti-malarials had been previously used was therefore revisited [29]. Children aged 2–9 years received monthly administrations of CQ, PYR, CPGN or placebo depending upon which village they lived in. One drug was consistently used in each village. During the study period P. falciparum developed in vivo resistance to PYR and partially reduced susceptibility to CPGN whilst CQ remained effective [29–31]. The in vivo drug susceptibilities were assessed as Day 7 clearance of parasitaemia by microscopy after single doses of 10 mg/kg CQ, 2 mg/kg PYR or 1.5 mg/kg CPGN respectively. For CQ the clearance rates were 100% among children in CQ village and the control village. For PYR the clearance rates were 7% among children in PYR village and 96% in the control village. For CPGN the clearance rates were 53% among children in CPGN village and 96% in the control village. Sequence variation in pfcrt, pfmdr1, pfnhe1, pfmrp1, pfdhfr and pfdhps in samples collected after 2 years of monthly presumptive treatment with either CQ, PYR, CPGN or placebo were determined.
Methods
Study area
The clinical study from which samples were used was conducted in a rural area of northern Liberia 25–35 km from Yekepa. Four villages, about 5 km from each other, were included in the study: Bondi, Baytonwee, Bonah and Kinon. Each village had around 500 inhabitants. The villages were separated by dense forest, which made access to and between the villages difficult. Access to healthcare and specifically anti-malarial treatment was very limited when the study started in 1976. The climate is tropical with a dry season from November to April and a rainy season from May to October. The temperature is generally between 21 and 32 °C. Malaria was holoendemic when the clinical study was conducted [29, 30]. In 1976 (prior to deployment of monthly presumptive treatment) the overall parasite prevalence in the study area assessed by blood slide microscopy in 2–9 years old children was 82% for P. falciparum, 39% for Plasmodium malariae and 9% for Plasmodium ovale [32].
Study group, consent, drug administration, sample collection and storage
Children 2–9 years old, present in the villages in November 1976 were invited to participate in the study. All (n = 282) agreed to participate after verbal informed consent. The four villages were visited every 14 days for 3 years. Children were given single dose anti-malarial drugs every 4 weeks for 2 years as follows. Bondi: 8–15 mg base/kg dose of CQ. Baytonwee: 1.0–2.0 mg base/kg of CPGN. Bonah: 1.3–2.5 mg base/kg of PYR. Kinon: 1 or 2 tablets of Vitamin B (placebo). Drug intake was supervised by the investigators [29].
Children in all villages were also treated with 8–15 mg/kg base of single dose CQ in case of fever and confirmed malaria infection throughout the two-year study period. At the time this was considered a therapeutic dose of CQ [29]. After 2 years of monthly presumptive treatment, capillary whole blood samples were collected 4–6 weeks after last intake of study drug (i.e. from 28th of February to 17th of March, 1978) from all children (n = 191) present and still included in the study. The children were now 4–11 years old. Samples were coded and stored at −20 °C. The prevalence of P. falciparum in each treated village, as assessed by microscopy, was 23% (CQ), 94% (PYR), 73% (CPGN) and 88% (placebo) [29], whereas P. malariae and P. ovale were rarely detected.
The study was approved by the Liberian Institute of Biomedical Research [29]. Molecular analyses were approved by the Stockholm regional ethics board (reference number: 2013/836-32).
Molecular analysis
DNA was extracted using QIAamp Blood Mini Kit (QIAgen Biosciences, Germantown, MD, USA). The samples were extracted separately from other samples in our research laboratory to minimise the risk of contamination. Extracted DNA was stored at −20 °C until use.
Pfcrt 72–76, pfmdr1 1034–1246, pfdhfr 16–185, pfdhps 436–632 and pfnhe1 ms4760 haplotypes were identified by PCR amplification followed by sequencing using previously described PCR protocols [12, 16, 33–35]. The Sequencher™ software version 4.6 (Gene Codes Corporation, Ann Arbor, MI, USA) was used for sequence analyses. The P. falciparum 3D7 clone sequence obtained from the NCBI database was used as references for pfcrt (Accession no. NC_004328), pfmdr1 (Accession no. XM_001351751.1), pfdhfr (Accession no. XM_001351443.1) pfdhps (Accession no. XM_001349382.1) and pfnhe1 (Accession no. XM_001349726). Pfnhe1 ms4760 sequences were also compared with previously described isolates and clones [16, 36].
In addition to sequencing PCR–RFLP (restriction fragment length polymorphism) was used to identify the following SNPs; pfcrt K76T, A220S, Q271E, N326D/S, I356L/T, R371I, pfdhfr N51I, C59R, S108T/N, pfdhps S436F/A, A437G and K540E and pfmdr1 N86Y and Y184F using previously described methods [12, 37, 38]. The pfmrp1 allele K1466R was determined by pyrosequencing [28].
PCR and restriction products were resolved on 2% agarose gels (Amresco, Solon, OH, USA). All gels were stained with a nucleic acid gel stain (GelRed™, Biotium Inc. Hayward, CA, USA) and visualized under UV transillumination (GelDoc®, Biorad, Hercules, CA, USA). PCR products were purified and sequenced commercially (Macrogen Inc. Seoul, Korea).
Statistics
Data were entered, validated and analysed on Microsoft Excel 2003 and StataCorp 12. Allele proportions were calculated by dividing the number of samples with a certain allele by the number of samples with an identifiable allele at that position. Thus mixed infections contributed to the proportion of both alleles. Associations were determined using Fishers Exact test using StataCorp 12.
Results
A total of 191 samples were included in the study, of which 50, 48, 48 and 45 were from the CQ, PYR, CPGN and placebo village, respectively. At least one SNP was identified in all samples (not only microscopy positive) and each SNP was identified in 81–98% of samples. Negative controls were used throughout without any signs of contamination.
Pfcrt
Pfcrt K76 was found in 185/186 (99%) samples. A single sample carrying pfcrt 76T was detected in the village using CQ. The CVMNK haplotype was found in 177/178 (99%) successfully sequenced samples and the CVIET haplotype was found in the sample that had pfcrt 76T by RFLP. The pfcrt CVIET result was confirmed by PCR–RFLP and sequencing after re-extracting the sample alone. The pfcrt haplotype at codons 220, 271, 326, 356 and 371 was determined in the CQ and placebo villages only. The wild type AQNIR haplotype was found in all successfully amplified samples (88/95 [93%]) including the sample with the pfcrt CVIET haplotype.
Pfmdr1
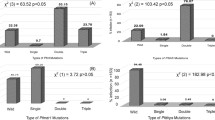
Pfmdr1 N86 was found in all 161 (100%) successfully amplified samples. Pfmdr1 Y184 was found in 75/160 (47%), 184F in 47/160 (29%) and Y184+184F in 38/160 (24%). The ratio of 184F was non-significantly higher in the CPGN (19/37 [51%]), PYR (27/46 [59%]) and CQ (19/33 [58%]) villages compared to the placebo village (20/44 [45%]). Similarly, no significant difference was observed in Y184 ratio in the CPGN (22/37 [59%]), PYR (32/46 [70%]), CQ (20/33 [61%]) villages compared with the placebo village (29/44 [66%]). Excluding mixed infections did not alter the findings significantly.
The pfmdr1 S1034C, N1042D, F1226Y and D1246Y haplotypes were SNFD in all 163 (100%) successfully sequenced samples. The frequency of a synonymous SNP at codon 1069 (ACT→ACG) was found to be significantly higher in the CQ village (11/17 [30%]) compared to the PYR (3/45, P = 0.008), CPGN (1/38, P = 0.001) and placebo (1/43, P = 0.001) villages. Three novel synonymous SNPs 1061 (GAT→GAC), 1137 (TCA→TCC) and 1185 (ATT→ATC) were found in 1, 4 and 2 of the 163 samples, respectively. Two novel non synonymous SNPs 1166 (GGA→GCA) and 1190 (GAT→AAT) were found in 2 and 1 samples, respectively.
Pfnhe-1
Pfnhe1 ms4760 was successfully amplified in 156/191 (82%) samples. Eight of the 114 previously described pfnhe1 haplotypes [16, 36] and 47 novel ms4760 haplotypes were found. The haplotypes found are shown in Additional file 1: Table S1. Of the 47 new haplotypes, 32 consisted of variation in Block I. Proportions of samples with haplotypes in block I are presented in Table 1. Variation in pfnhe1 block I were significantly more common in the villages using CPGN (9/35 [26%], P < 0.001), PYR (18/44 [41%], P < 0.001) and placebo (16/39 [41%], P < 0.001) compared to the CQ treated village (0/38). Though Block I did not vary in the CQ village 10 different ms4760 haplotypes were identified due to variations in other parts of ms4760.
The ratio of ms4760 haplotypes in successfully amplified samples were significantly lower in the villages using CQ (10/38 [26%], P = 0.006) but non-significantly lower in the villages using CPGN (13/35 [37%], P = 0.07) and PYR 19/44 (43%, P = 0.19) compared to placebo 23/39 (59%).
The number of quinine resistance associated DDNHNDNHNND repeats in block V were one in 30/156 (19%), two in 124/156 (80%) and 3 in 2/156 (1%) samples. The distributions of repeats were similar in all villages. There were no associations of variations in block I or V and any SNPs in pfmdr1, pfdhfr or pfdhps.
Pfdhfr
Allele proportions are presented in Table 2. The proportion of the PYR resistance associated 108N was significantly lower in the village using PYR (1/46 [2%]) compared to the villages using CPGN (17/39 [44%], P < 0.001), CQ (18/39 [46%], P < 0.001) and placebo (29/45 [64%], P < 0.001). The other codons found were all A16, N51, C59 and I164 that are associated with sensitivity to PYR.
Pfdhps
Allele proportions are presented in Table 3. The sulphadoxine resistance associated pfdhps 613S was found in 10% (14/135) of samples in this sulphadoxine–pyrimethamine naïve area. No other resistance associated polymorphisms were found. The proportion of pfdhps 613S was significantly lower in the PYR village (0/38) compared to the village using CQ (7/26 [27%], P = 0.001) and non-significantly lower in the villages using CPGN (3/31 [10%], P = 0.09) and placebo (4/39 [10%], P = 0.12). When data from the CPGN, CQ and placebo villages were pooled the findings were significantly different compared with the PYR village (P = 0.01).
Pfmrp1
Pfmrp1 R1466 (wild type) was found in 137/137 (100%) successfully amplified samples.
Discussion
This study provides a unique insight into the early appearance of genetic markers associated with anti-malarial drug resistance and their selection 2 years after monthly presumptive treatment with CQ, PYR and CPG or placebo in a previously virtually anti-malarial treatment-naïve area of Liberia.
One sample had the pfcrt 76T SNP in the 72-76 CVIET haplotype not previously recorded in Africa as early as 1978. Pfcrt CVIET was confirmed by repeated PCR analyses on re-extracted DNA several months after the first analyses. Contamination is, therefore, unlikely to explain this remarkable finding. Throughout the world pfcrt 76T has been linked to CQ resistance within various pfcrt 72–76 haplotypes. By 1978, pfcrt CVIET had existed in Southeast Asia for many years but not in Africa. Molecular analysis has shown that the CVIET later found throughout Africa was derived from this Southeast Asian lineage [8]. Southeast Asian pfcrt typically have additional downstream SNPs at codons 220, 271, 326, 356 and 371. Our sample had those typical among African origin CQ sensitive genotypes (and 3D7) [39]. Furthermore, the study area was very isolated making importation unlikely. The most likely explanation is thus that pfcrt 72–76 CVIET arose in the CQ study village de-novo following a period of intermittent presumptive treatment with CQ.
Irrespective of how this isolated CVIET haplotype came to be in the study area it did not seem to have become widespread as only pfcrt CVMNK parasites were found in 50 samples collected 3 years later in the same area [40]. This observation is consistent with longitudinal surveillance of high in vivo efficacy and in vitro susceptibility to CQ in Bondi (CQ village) between 1976 and 1978 [29, 41]. In the ordered evolution of pfcrt SNPs that eventually give rise to CQ resistance described by Summers et al. [42], having CVIET alone with no other pfcrt SNPs only resulted in a small increase in Pfcrt’s ability to transport CQ and hence to confer resistance [42]. Furthermore, these mutations interfere with haemoglobin digestion resulting in a loss of fitness [43]. Thus CVIET might have developed in Liberia but did not become widespread as it provided only weak selective advantage in this holoendemic area.
The increased frequency of the synonymous SNP pfmdr1 T1069ACG and decreased diversity in pfnhe1 block I in the CQ treated village indicates that CQ exerted a selective pressure on the drug-naïve parasite population. In line with this both genes have previously been linked to CQ resistance [19, 20] and previously described block I ms4760 haplotypes in samples collected after the spread of CQ resistance had the same block I type as that selected for in the CQ village [36]. However, as pfmdr1 T1069ACG is a synonymous SNP it was not selected itself but is probably a marker for selection of a parasite strain or a pfmdr1 genotype that had a survival advantage when CQ was used.
Decreased in vitro and in vivo QN susceptibility has been associated with the pfnhe1 ms4760-1 haplotype that has two DNNND and one DDNHNDNHNND and with having more than one DNNND repeat and one DDNHNDNHNND repeat in some studies but not in others [14, 16, 36, 44]. Though QN was not used in the Yekepa area at the time of this study the frequency of pfnhe1 ms4760-1 (26%) was similar to the frequency found at day 0 in a recent study in Mali where ms4760-1 was associated with decreased QN susceptibility [16]. Considering the geographic separation of Liberia and Mali results should be compared with considerable caution. However, similar frequencies found in Liberia in 1978, prior to a drug selective pressure and in Mali and Senegal several decades later suggest that ms4760-1 has not been under a strong selective pressure.
The PYR resistance associated pfdhfr 108N was surprisingly not selected for in the PYR village despite development of in vivo resistance to PYR within a year of initiating monthly intermittent presumptive therapy [29]. In contrast it was found at significant frequencies in the placebo and CQ villages where no antifolate drugs had been used, suggesting that it was a wild type in Liberia in 1978. Similarly, resistance associated pfdhfr 51I, 59R, 108N were found in 9/66 samples collected in The Gambia in 1984 prior to widespread use of SP [45]. These intriguing results suggest that there may have been an alternate mechanism of PYR resistance in our study village as has previously been suggested [13, 46]. Furthermore, the 108N did not provide a selective advantage in the presence of this alternate mechanism but rather the opposite. Amplifications of the pfdhfr or GTP-cyclohydrolase (gch1) genes have been linked to PYR resistance in the past [47, 48]. Gene amplifications could have occurred in Liberia and might thus constitute an early method of PYR resistance in line with the correlation between pfmdr1 amplifications and drug resistance to mefloquine and artemisinin derivatives [49]. An alternative mechanism of PYR resistance might be a greater influx of folate into the parasite as has been suggested to be mediated by pfmrp1 1466K [28]. However, in Liberia only pfmrp1 R1466 was found. Concerning pfdhps, PYR is not likely to directly exert a selective effect, yet the frequency of pfdhps 613S (that is related to sulphadoxine resistance) was lower in the PYR treated village. Perhaps this represents an indirect effect of selection of other genes.
Chlorproguanil (CPGN) is believed to be a DHFR inhibitor that is partly metabolized to the probably more P. falciparum active chlorcycloguanil in vivo. In line with this parasites with pfdhfr 16V and 108T and 108N have been associated with decreased susceptibility to the structurally similar cycloguanil in vitro and ex vivo, [26, 50–52]. Finding no difference in pfdhfr 108N frequency in the CPGN village compared with the placebo village indicates that 108 N was not the cause of the partly reduced CPGN susceptibility seen in the study area [29].
Conclusion
Unique data on the effect of monthly intermittent presumptive CQ, PYR and CPGN therapy on selection of known resistance genes in previously treatment-naïve P. falciparum populations is presented. The pfcrt 72–76 haplotype CVIET was detected in the CQ village and possibly developed de-novo. However, none of the downstream pfcrt SNPs commonly found throughout CQR genotypes in Africa today were detected. Decreased variation of pfnhe1 was seen and a synonymous pfmdr1 1069T SNP was selected detected in the CQ village suggesting that CQ exerted a selective pressure on the drug naïve parasite population. The PYR resistance associated SNP pfdhfr 108N was highly prevalent in this antifolate naïve parasite population and intriguingly deselected concomitant with emergence of PYR resistance suggesting alternative mechanisms of PYR resistance. The results provide new insights into the evolution of anti-malarial drug resistance in Africa.
References
Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM. Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med. 2008;359:2619–20.
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, et al. Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009;361:455–67.
Amaratunga C, Sreng S, Suon S, Phelps ES, Stepniewska K, Lim P, et al. Artemisinin-resistant Plasmodium falciparum in Pursat province, western Cambodia: a parasite clearance rate study. Lancet Infect Dis. 2012;12:851–8.
Phyo AP, Nkhoma S, Stepniewska K, Ashley EA, Nair S, McGready R, et al. Emergence of artemisinin-resistant malaria on the western border of Thailand: a longitudinal study. Lancet. 2012;379:1960–6.
Kyaw MP, Nyunt MH, Chit K, Aye MM, Aye KH, Aye MM, et al. Reduced susceptibility of Plasmodium falciparum to artesunate in southern Myanmar. PLoS ONE. 2013;8:e57689.
Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C, Lim P, Suon S, et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2014;371:411–23.
Fidock DA, Nomura T, Talley AK, Cooper RA, Dzekunov SM, Ferdig MT, et al. Mutations in the P. falciparum digestive vacuole transmembrane protein PfCRT and evidence for their role in chloroquine resistance. Mol Cell. 2000;6:861–71.
Wootton JC, Feng X, Ferdig MT, Cooper RA, Mu J, Baruch DI, et al. Genetic diversity and chloroquine selective sweeps in Plasmodium falciparum. Nature. 2002;418:320–3.
Millet J, Alibert S, Torrentino-Madamet M, Rogier C, Santelli-Rouvier C, Bigot P, et al. Polymorphism in Plasmodium falciparum drug transporter proteins and reversal of in vitro chloroquine resistance by a 9,10-dihydroethanoanthracene derivative. Antimicrob Agents Chemother. 2004;48:4869–72.
Mita T, Tanabe K, Kita K. Spread and evolution of Plasmodium falciparum drug resistance. Parasitol Int. 2009;58:201–9.
Plowe CV. Monitoring antimalarial drug resistance: making the most of the tools at hand. J Exp Biol. 2003;206:3745–52.
Djimde A, Doumbo OK, Cortese JF, Kayentao K, Doumbo S, Diourte Y, et al. A molecular marker for chloroquine-resistant falciparum malaria. N Engl J Med. 2001;344:257–63.
Muller IB, Hyde JE. Antimalarial drugs: modes of action and mechanisms of parasite resistance. Future Microbiol. 2010;5:1857–73.
Ferdig MT, Cooper RA, Mu J, Deng B, Joy DA, Su XZ, et al. Dissecting the loci of low-level quinine resistance in malaria parasites. Mol Microbiol. 2004;52:985–97.
Bennett TN, Patel J, Ferdig MT, Roepe PD. Plasmodium falciparum Na+/H+ exchanger activity and quinine resistance. Mol Biochem Parasitol. 2007;153:48–58.
Kone A, Mu J, Maiga H, Beavogui AH, Yattara O, Sagara I, et al. Quinine treatment selects the pfnhe-1 ms4760-1 polymorphism in Malian patients with Falciparum malaria. J Infect Dis. 2013;207:520–7.
Sinou V, le Quang H, Pelleau S, Huong VN, Huong NT, le Tai M, et al. Polymorphism of Plasmodium falciparum Na(+)/H(+) exchanger is indicative of a low in vitro quinine susceptibility in isolates from Vietnam. Malar J. 2011;10:164.
Bosia A, Ghigo D, Turrini F, Nissani E, Pescarmona GP, Ginsburg H. Kinetic characterization of Na+/H+ antiport of Plasmodium falciparum membrane. J Cell Physiol. 1993;154:527–34.
Sanchez CP, Horrocks P, Lanzer M. Is the putative chloroquine resistance mediator CG2 the Na+/H+ exchanger of Plasmodium falciparum? Cell. 1998;92:601–2.
Wunsch S, Sanchez CP, Gekle M, Grosse-Wortmann L, Wiesner J, Lanzer M. Differential stimulation of the Na+/H+ exchanger determines chloroquine uptake in Plasmodium falciparum. J Cell Biol. 1998;140:335–45.
Bray PG, Ward SA, Ginsburg H. Na+/H+ antiporter, chloroquine uptake and drug resistance: inconsistencies in a newly proposed model. Parasitol Today. 1999;15:360–3.
Spillman NJ, Allen RJ, Kirk K. Acid extrusion from the intraerythrocytic malaria parasite is not via a Na(+)/H(+) exchanger. Mol Biochem Parasitol. 2008;162:96–9.
Mita T. Origins and spread of pfdhfr mutant alleles in Plasmodium falciparum. Acta Trop. 2010;114:166–70.
Hastings IM, Donnelly MJ. The impact of antimalarial drug resistance mutations on parasite fitness, and its implications for the evolution of resistance. Drug Resist Updat. 2005;8:43–50.
Abdul-Ghani R, Farag HF, Allam AF. Sulfadoxine–pyrimethamine resistance in Plasmodium falciparum: a zoomed image at the molecular level within a geographic context. Acta Trop. 2013;125:163–90.
Basco LK, Ringwald P. Molecular epidemiology of malaria in Yaounde, Cameroon. VI. Sequence variations in the Plasmodium falciparum dihydrofolate reductase-thymidylate synthase gene and in vitro resistance to pyrimethamine and cycloguanil. Am J Trop Med Hyg. 2000;62:271–6.
Lynch C, Pearce R, Pota H, Cox J, Abeku TA, Rwakimari J, et al. Emergence of a dhfr mutation conferring high-level drug resistance in Plasmodium falciparum populations from southwest Uganda. J Infect Dis. 2008;197:1598–604.
Dahlstrom S, Veiga MI, Mårtensson A, Björkman A, Gil JP. Polymorphism in PfMRP1 (Plasmodium falciparum multidrug resistance protein 1) amino acid 1466 associated with resistance to sulfadoxine–pyrimethamine treatment. Antimicrob Agents Chemother. 2009;53:2553–6.
Björkman A, Brohult J, Pehrson PO, Willcox M, Rombo L, Hedman P, et al. Monthly antimalarial chemotherapy to children in a holoendemic area of Liberia. Ann Trop Med Parasitol. 1986;80:155–67.
Björkman A, Brohult J, Sirleaf V, Willcox M, Bengtsson E. Plasmodium falciparum resistance to pyrimethamine and chlorproguanil—host or parasite dependent? Ann Trop Med Parasitol. 1980;74:245–8.
Björkman A, Brohult J, Willcox M, Pehrson PO, Rombo L, Hedman P, et al. Malaria control by chlorproguanil. I. Clinical effects and susceptibility of Plasmodium falciparum in vivo after seven years of monthly chlorproguanil administration to children in a Liberian village. Ann Trop Med Parasitol. 1985;79:597–601.
Björkman A, Hedman P, Brohult J, Willcox M, Diamant I, Pehrsson PO, et al. Different malaria control activities in an area of Liberia—effects on malariometric parameters. Ann Trop Med Parasitol. 1985;79:239–46.
Vinayak S, Alam MT, Mixson-Hayden T, McCollum AM, Sem R, Shah NK, et al. Origin and evolution of sulfadoxine resistant Plasmodium falciparum. PLoS Pathog. 2010;6:e1000830.
Alam MT, de Souza DK, Vinayak S, Griffing SM, Poe AC, Duah NO, et al. Selective sweeps and genetic lineages of Plasmodium falciparum drug -resistant alleles in Ghana. J Infect Dis. 2011;203:220–7.
Malmberg M, Ferreira PE, Tarning J, Ursing J, Ngasala B, Bjorkman A, et al. Plasmodium falciparum drug resistance phenotype as assessed by patient antimalarial drug levels and its association with pfmdr1 polymorphisms. J Infect Dis. 2013;207:842–7.
Ménard D, Andriantsoanirina V, Khim N, Ratsimbasoa A, Witkowski B, Benedet C, et al. Global analysis of Plasmodium falciparum Na+/H+ exchanger (pfnhe-1) allele polymorphism and its usefulness as a marker of in vitro resistance to quinine. Int J Parasitol Drugs Drug Resist. 2013;3:8–19.
Veiga MI, Ferreira PE, Bjorkman A, Gil JP. Multiplex PCR-RFLP methods for pfcrt, pfmdr1 and pfdhfr mutations in Plasmodium falciparum. Mol Cell Probes. 2006;20:100–4.
Holmgren G, Hamrin J, Svard J, Mårtensson A, Gil JP, Björkman A. Selection of pfmdr1 mutations after amodiaquine monotherapy and amodiaquine plus artemisinin combination therapy in East Africa. Infect Genet Evol. 2007;7:562–9.
Summers RL, Nash MN, Martin RE. Know your enemy: understanding the role of PfCRT in drug resistance could lead to new antimalarial tactics. Cell Mol Life Sci. 2012;69:1967–95.
Jovel IT, Ferreira PE, Veiga MI, Malmberg M, Mårtensson A, Kaneko A, et al. Single nucleotide polymorphisms in Plasmodium falciparum V type H(+) pyrophosphatase gene (pfvp2) and their associations with pfcrt and pfmdr1 polymorphisms. Infect Genet Evol. 2014;24:111–5.
Björkman A, Rombo L, Willcox M, Hanson AP, Bengtsson E. In vivo response of Plasmodium falciparum to different doses of chloroquine in semi-immune children in Liberia, West Africa. Ann Trop Med Parasitol. 1986;80:1–6.
Summers RL, Dave A, Dolstra TJ, Bellanca S, Marchetti RV, Nash MN, et al. Diverse mutational pathways converge on saturable chloroquine transport via the malaria parasite’s chloroquine resistance transporter. Proc Natl Acad Sci USA. 2014;111:1759–67.
Lewis IA, Wacker M, Olszewski KL, Cobbold SA, Baska KS, Tan A, et al. Metabolic QTL analysis links chloroquine resistance in Plasmodium falciparum to impaired hemoglobin catabolism. PLoS Genet. 2014;10:e1004085.
Pascual A, Fall B, Wurtz N, Fall M, Camara C, Nakoulima A, et al. In vitro susceptibility to quinine and microsatellite variations of the Plasmodium falciparum Na+/H+ exchanger transporter (Pfnhe-1) gene in 393 isolates from Dakar, Senegal. Malar J. 2013;12:189.
Nwakanma DC, Duffy CW, Amambua-Ngwa A, Oriero EC, Bojang KA, Pinder M, et al. Changes in malaria parasite drug resistance in an endemic population over a 25-year period with resulting genomic evidence of selection. J Infect Dis. 2014;209:1126–35.
Kidgell C, Volkman SK, Daily J, Borevitz JO, Plouffe D, Zhou Y, et al. A systematic map of genetic variation in Plasmodium falciparum. PLoS Pathog. 2006;2:e57.
Thaithong S, Ranford-Cartwright LC, Siripoon N, Harnyuttanakorn P, Kanchanakhan NS, Seugorn A, et al. Plasmodium falciparum: gene mutations and amplification of dihydrofolate reductase genes in parasites grown in vitro in presence of pyrimethamine. Exp Parasitol. 2001;98:59–70.
Heinberg A, Siu E, Stern C, Lawrence EA, Ferdig MT, Deitsch KW, et al. Direct evidence for the adaptive role of copy number variation on antifolate susceptibility in Plasmodium falciparum. Mol Microbiol. 2013;88:702–12.
Cui L, Wang Z, Miao J, Miao M, Chandra R, Jiang H, et al. Mechanisms of in vitro resistance to dihydroartemisinin in Plasmodium falciparum. Mol Microbiol. 2012;86:111–28.
Basco LK, Eldin de Pecoulas P, Wilson CM, Le Bras J. Mazabraud A. Point mutations in the dihydrofolate reductase-thymidylate synthase gene and pyrimethamine and cycloguanil resistance in Plasmodium falciparum. Mol Biochem Parasitol. 1995;69:135–8.
Foote SJ, Galatis D, Cowman AF. Amino acids in the dihydrofolate reductase-thymidylate synthase gene of Plasmodium falciparum involved in cycloguanil resistance differ from those involved in pyrimethamine resistance. Proc Natl Acad Sci USA. 1990;87:3014–7.
Peterson DS, Milhous WK, Wellems TE. Molecular basis of differential resistance to cycloguanil and pyrimethamine in Plasmodium falciparum malaria. Proc Natl Acad Sci USA. 1990;87:3018–22.
Authors’ contributions
AB conducted the original clinical studies. IJ did the molecular work and drafted the manuscript together with JU. All authors contributed to the planning of the study and the writing of the manuscript and read and approved the final manuscript. All authors read and approved the final manuscript.
Acknowledgements
We wish to thank Dr. A. Hanson for support from the Liberian Institute of Biomedical research and Mr. E. Kollie for laboratory assistance.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request. Pfnhe-1 haplotypes found are available on supplementary materials and the exact sequence of each new ms4760 haplotype has been submitted to GenBank (accession no. KM515813 to KM515862).
Ethics approval and consent to participate
The study was approved by the Liberian Institute of Biomedical Research [29]. Molecular analyses were approved by the Stockholm regional ethics board (reference number: 2013/836-32).
Funding
This work was supported by Swedish Research Council and Sigurd och Elsa Goljes Minne Fund (project No. LA2010-0537). JU has a postdoctoral position funded by Stockholms läns landsting.
Author information
Authors and Affiliations
Corresponding author
Additional file
12936_2017_1747_MOESM1_ESM.pdf
Additional file 1: Table S1. Alignment of pfnhe1 ms4760variants found in Liberia in 1978 (Jovel et al. [40]).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Jovel, I.T., Björkman, A., Roper, C. et al. Unexpected selections of Plasmodium falciparum polymorphisms in previously treatment-naïve areas after monthly presumptive administration of three different anti-malarial drugs in Liberia 1976–78. Malar J 16, 113 (2017). https://doi.org/10.1186/s12936-017-1747-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-017-1747-6