Abstract
Background
Malariometric information is needed to decide how to introduce malaria vaccines and evaluate their impact in sub-Saharan African countries.
Methods
This cross-sectional study (NCT01954264) was conducted between October and November, 2013, corresponding to the high malaria transmission season, in four sites with Health and Demographic Surveillance Systems (DSS) [two sites with moderate-to-high malaria endemicity in Burkina Faso (Nouna and Saponé) and two sites with low malaria endemicity in Senegal (Keur Socé and Niakhar)]. Children (N = 2421) were randomly selected from the DSS lists of the study sites and were stratified into two age groups (6 months–4 years and 5–9 years). A blood sample was collected from each child to evaluate parasite prevalence of Plasmodium falciparum and other Plasmodium species and gametocyte density by microscopy, and rapid diagnosis test in the event of fever within 24 h. Case report forms were used to evaluate malaria control measures and other factors.
Results
Plasmodium falciparum was identified in 707 (29.2%) children, with a higher prevalence in Burkina Faso than Senegal (57.5 vs 0.9% of children). In Burkina Faso, prevalence was 57.7% in Nouna and 41.9% in Saponé in the 6 months–4 years age group, and 75.4% in Nouna and 70.1% in Saponé in the 5–9 years age group. Infections with other Plasmodium species were rare and only detected in Burkina Faso. While mosquito nets were used by 88.6–97.0 and 64.7–80.2% of children in Burkina Faso and Senegal, other malaria control measures evaluated at individual level were uncommon. In Burkina Faso, exploratory analyses suggested that use of malaria treatment or any other medication within 14 days, and use of insecticide spray within 7 days decreased the prevalence of malaria infection; older age, rural residence, natural floor, grass/palm roof, and unavailability of electricity in the house were factors associated with increased malaria occurrence.
Conclusions
Plasmodium falciparum infection prevalence in children younger than 10 years was 57.5% in Burkina Faso and 0.9% in Senegal, and variability was observed, among others, by age, study site and malaria control measures.
Similar content being viewed by others
Background
In sub-Saharan Africa, malaria remains a major cause of morbidity and mortality, especially in young children [1]. In 2013, when the current study was conducted, approximately 198 million malaria cases occurred globally, causing 584,000 deaths. Most cases (90%) occurred in Africa, and most deaths (78%) were in children under 5 years of age [2].
In many African countries, malaria control programmes have been implemented since 2000, including the use of insecticide-treated nets (ITNs), long-lasting insecticidal nets (LLINs), indoor residual spraying of insecticides (IRS), rapid diagnostic tests (RDTs), and effective anti-malaria medicines [1]. Although these interventions have been associated with a reduction in malaria incidence rates, the increasing problem of multi-drug resistance and insecticide resistance highlights the need for new tools, especially in areas of moderate-to-high malaria transmission intensity (MTI) [1, 3–7].
Adding a malaria vaccine to the control programmes has been identified as a key component to complement current interventions [8, 9]. RTS,S/AS01 is the first malaria vaccine that underwent large-scale phase 3 evaluation in Africa [4, 10–12] and received a positive regulatory assessment by the European Medicines Agency in July 2015 [13]. Before considering its introduction for routine use, the World Health Organization (WHO) recommended further evaluation of its four-dose vaccination schedule in a series of pilot implementations in moderate-to-high transmission settings in sub-Saharan Africa [1].
Malariometric information is needed to guide decisions on how to prioritize interventions and introduce malaria vaccines. Among others, the level of malaria transmission, which is very heterogeneous within geographical areas, may have an effect on the efficacy of malaria control measures, including RTS,S/AS01 [12, 14]. The objectives of the present study were to evaluate the parasite prevalence (PP): an indirect, cost-effective way to evaluate the force of malaria transmission) of Plasmodium falciparum and other Plasmodium species, the extent of use of malaria control measures, and other factors in four sites, where phase IV studies on RTS,S/AS01 were expected to be conducted. These results are needed to anticipate the impact of RTS,S/AS01 if this vaccine is implemented in focalized pilot programmes or national vaccination programmes.
Methods
Study design and area
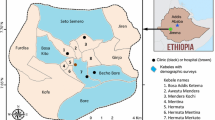
This epidemiological, cross-sectional study was carried out at four sites with Health and Demographic Surveillance Systems (HDSS) in Burkina Faso and Senegal (NCT01954264). The first site was located in the area of Nouna at about 300 km from Ouagadougou (northwestern Burkina Faso), where malaria is hyper- to holo-endemic, the malaria transmission peak occurs at the end of the rainy season (June to October), and reduced transmission is observed during the dry season (December to May) [15]. The second site in Burkina Faso was located in Saponé (30 km southwest of Ouagadougou), where malaria transmission is also seasonal, and the peak is observed at the end of the rainy season in September [16]. The third site was located in the Keur Socé area (200 km southeast of Dakar, Senegal), which is characterized by the alternation of a long dry season and a short rainy season from July to November, and has a peak in malaria transmission between October and November [17, 18]. The last site was located in the Niakhar area (115 km southeast of Dakar, Senegal), where malaria is meso-endemic and transmission is seasonal from September to December [19].
Study population
Participants were children aged ≥6 months to <10 years, whose parents or legally acceptable representative had provided informed consent prior to any study-specific procedure. Children in care, or actively participating in any trial involving administration of an investigational malaria vaccine or drug were excluded. Children were randomly selected from the HDSS list at each site, and were stratified into two age groups for the analyses, as defined by the Joint Technical Expert Group (JTEG) criteria: children aged 6 months–4 years and children aged 5–9 years. Analyses were performed on all evaluable children for whom at least one laboratory result was available.
Data collection
This study was conducted during or just after the rainy season, at the peak of malaria transmission. Data were collected at one visit between 19 October and 25 November, 2013, and no follow-up was done (Fig. 1). Internet-based electronic case report forms were used to record demographic details, relevant medical history, malaria control measures used in the household, malaria risk factors, anti-malaria medication and other medication received within 14 days, and history of fever in the last 24 h. Axillary body temperature at the time of the survey was measured by trained personnel according to the study protocol.
The malaria control measures evaluated at the individual level were the use of mosquito bed nets the night before the visit, mosquito coils, insecticide sprays, and commercial and traditional repellents over 7 days, and IRS on interior walls in previous 12 months. The other factors evaluated in this study were age, gender, study centre, number of persons living in the same house, localization (rural vs urban area; town vs countryside), main house construction material (walls, floor, roof, windows/eaves, nets), main source of drinking water, and availability of electricity.
Each study site was requested to provide centre-specific information about control measures from the malaria control programme in the study area and, if available, meteorological data for the study site, such as rainfall and temperature. The information was collected in the form of a questionnaire recorded in a separate database.
Biological methods
Approximately 200 µL of whole blood was collected from all participants. A RDT was performed in the event of recent history of fever (axillary temperature ≥37.5 °C measured at the time of visit or reported in the previous 24 h). The RDT was used to detect HRP-II (Histidine-rich protein II) specific to P. falciparum and pLDH (Plasmodium lactate dehydrogenase) specific to Plasmodium vivax (SD BIOLINE Malaria Ag P.f/P.v test). If the RDT was positive or the child was identified as being parasite-positive following microscopy, treatment was given according to national guidelines.
The presence of parasites on capillary blood samples was assessed by 100-field microscopic examination, assuming 8000 leukocytes/µl of blood. The count was made by species (P. falciparum, P. malariae, P. vivax, or Plasmodium ovale), and counts for P. falciparum were made for both gametocytes and asexual parasites. Two slides, each containing a thick and thin blood smear, were prepared; positive parasitaemia was identified on the thick blood film, and species on the thin blood film, except in case of low parasitaemia. The parasite presence and density were determined independently by two readers for the same slide; if readings were judged to be discordant, a third independent read was organised. A child was defined as infected by a specific parasite if at least two readings were positive for the corresponding parasite. If the final decision was positive, the parasite density (parasites/μL) was calculated as the geometric mean of the two positive readings (two geometrically closest readings in the case of three positive reads). The following classes were used to categorize the parasite densities: low (<2500 parasites/μL); medium (2500–9999 parasites/μL); high (10,000–19,999 parasites/μL), and very high (≥20,000 parasites/μL).
A child was defined as having gametocytes when gametocytes were detected during at least one reading. In children with a positive status, the gametocyte density (units/μL) was defined as the geometric mean of the readings of the positive slides.
Statistical methods
The target sample size was 2400 children (600 at each participating site), according to the following stratification by age groups: 6 months-<1 year-olds (N = 60), 1 and 2 year-olds (N = 120 per group), 3 and 4 year-olds (N = 50 per group), and 5, 6, 7, 8, and 9 year-olds (N = 40 per group). To allow for 10% non-response, 660 children over all age categories were randomly selected from the demographic surveillance system databases of each site. This sample size ensured sufficiently narrow confidence intervals (CIs) around centre-wise PP estimates (with a maximum relative standard error of 0.25) in children from the 6 months–4 years (JTEG definition) and 29 years (WHO definition) age groups for sites with low (<10%), moderate (10–50%), or high (>50%) endemicity.
Continuous variables were described with mean, standard deviation (SD), median, and range. Categorical variables were described in frequency tables with absolute numbers and percentages. For some categorical variables, 95% CIs were also calculated.
Potential differences between groups were detected in exploratory analyses based on non-overlapping 95% CIs. The impact of various malaria control measures and other factors on the P. falciparum infection status was evaluated as exploratory analysis by centre in univariate logistic regression analyses and summarized using unadjusted odds ratios (ORs) with 95% CIs. A potential impact was detected if the 95% CI of the unadjusted ORs did not include the value ‘1’. The statistical analyses were performed using the Statistical Analysis Systems, version 9.2.
Results
Characteristics of the study participants
In this study, 2421 children were enrolled, with a similar distribution among the four sites. A few minor protocol deviations were reported (inconsistencies in terms of RDT testing based on the temperature), but no child was excluded from the total cohort randomly selected to participate in the study. A total of 1210 children were enrolled in Burkina Faso (610 in Nouna and 600 in Saponé) and 1211 children in Senegal (603 in Keur Socé centre and 608 in Niakhar). Among all participants, 52.3% were boys, with an even gender distribution among the four centres. The proportion of children living in rural areas was higher in the two Senegalese centres (≥99.8%) and in Saponé (≥98.7%) than in Nouna (53.6% in the 6 months–4 years and 51.7% in the 5–9 years age groups) (Table 1).
Fever in the last 24 h was reported in 24.6, 17.5, 12.0, and 9.0% of children aged 6 months–4 years, and in 16.3, 6.0, 9.8, and 5.5% of children aged 5–9 years in Nouna, Saponé, Keur Socé, and Niakhar, respectively (Table 1). The fever started, on average, 3 days before the study visit. At the study visit, 7.6, 8.3, 2.3, and 13.9% of children aged 6 months–4 years and 6.9, 2.0, 2.0, and 13.6% of children aged 5–9 years had fever in Nouna, Saponé, Keur Socé, and Niakhar, respectively. Among children with fever, the mean (SD) temperature was 38.0 °C (0.6), 38.1 °C (0.7), 38.4 °C (0.8), and 37.9 °C (0.5) in Nouna, Saponé, Keur Socé, and Niakhar, respectively.
In the Senegalese centres, ≤1.2% of children received any malaria treatment in the past 14 days, while in Burkina Faso, this percentage was 22.1 and 16.7% in Nouna, and 11.0 and 5.0 in Saponé in the 6 months–4 years and 5–9 years age groups, respectively (Table 1). The average duration of malaria treatment was 3 days, and for 14.1% of these children, the malaria treatment was still ongoing at the visit. In Burkina Faso, 149 out of the 178 children who received an anti-malarial were treated with artesunate-amodiaquine (83.7%), while in Senegal, four/nine children were treated with dihydroartemisinin-piperaquine (Niakhar centre), four/nine with artemether-lumefantrine, and one/nine with an unknown medication. The proportion of children who had received other medications in the past 14 days ranged from 3.9 to 43.5% (Table 1).
Parasite prevalence
Malaria infections caused by P. falciparum were detected in 29.2% of children; 57.9% of them were in the 6 months–4 years age group and 42.1% in the 5–9 years age group (Table 2; Fig. 1). The vast majority of infections (98.4%) were observed in Burkina Faso. In Nouna and Saponé, 57.7 and 41.9% of children in the 6 months–4 years age group, and 75.4 and 70.1% of children in the 5–9 years age group were infected, respectively. In Keur Socé, 0.5% of children were infected in both age groups, while infections were observed in 1.2% of children in the 6 months–4 years age group and 1.5% of children in the 5–9 years age group in Niakhar. In Burkina Faso, the P. falciparum PP seemed to increase with age during the first 9 years of life, while it seemed more uniform in Senegal (Fig. 2). Among the 404 children with results available for both RDT and microscopy, the degree of agreement between the two diagnostic tests was 85.3%.
In Burkina Faso, the minimum parasite density recorded was 16 parasites/µL in children aged 6 months–4 years and 11.31 parasites/µL in children aged 5–9 years. In Niakhar, similar results were obtained, with a minimum parasite density of 28.67 parasites/µL in children aged 6 months–4 years and 7.75 parasites/µL in children aged 5–9 years. In Keur Socé, however, the minimum parasite density recorded in the three children positive for P. falciparum was higher: 244.75 parasites/µL in the two children aged 6 months–4 years and 61,744.63 parasites/µL in the children aged 5–9 years.
In Nouna, potential differences in the proportion of children who received any malaria treatment in the past 14 days were detected between infected and non-infected children: 15.3 vs 31.4% for 6 months–4 years old children, and 10.5 vs 36.0% for 5–9 years old children. In 6 months–4 years old children in Saponé, potential differences were detected in terms of proportion of children who received any malaria treatment in the past 14 days (4.2% of infected children vs 15.9% of non-infected) and in terms of children with fever within the last 24 h (25.7% of infected children vs 11.6% of non-infected). In 5–9 years old children in Saponé, 0.7 and 15.0% of infected and non-infected children received any malaria treatment in the past 14 days, and 2.1 and 15.0% of infected and non-infected children received other medication in the past 14 days, respectively.
There was a greater likelihood of fever in the last 24 h for children with very high malaria parasite density (48.4%) compared to low (15.8%) or negative (10.8%) parasite density. Moreover, the overall proportion of children hospitalized for malaria in the last 3 months tended to be higher in children with very high malaria parasite density (6.5%) compared to those with low (3.4%) or negative parasite results (1.8%).
Gametocytes were more frequently detected in children from the centres with a higher PP (12.3 and 11.8% in Nouna, and 18.5 and 15.9% in Saponé in the 6 months–4 years and 5–9 years age groups, respectively). In the Senegalese centres, the number of gametocytes was extremely low, with a proportion of 0.3 and 0.0% in Keur Socé, and 1.0 and 0.5% in Niakhar in the same age groups. However, gametocytes were also frequently detected in children with low parasite density: 39.5% of 6 months–4 years old children and 64.9% of 5 to 9 years old children with gametocytes had a parasite density <2500 parasites/µL. P. falciparum was identified in 80.6 and 86.0% of children with gametocytes in the 6 months–4 years and 5–9 years age groups, respectively.
No other Plasmodium species were identified in the Senegalese centres. In Burkina Faso, infection with P. malariae was observed in eight/407 (2.0%) and 12/203 (5.9%) children in Nouna, and 15/399 (3.8%) and 20/201 (10.0%) children in Saponé in the 6 months–4 years and 5–9 years age groups, respectively. Infection with P. ovale was observed in nine children. No infection with P. vivax was recorded.
Impact of malaria control measures and other factors
The actual implementation of recommended malaria control measures was evaluated at the site level. ITNs were distributed for free in Niakhar, but were not free of charge in Nouna. No policy regarding the distribution of ITNs was implemented in Saponé, and no information was reported for Keur Socé. LLINs were distributed for free to pregnant women in Nouna, to the entire population with a replacement period of ≥24 months in Saponé and Keur Socé, and to children younger than 5 years and pregnant women in Niakhar. Artemisinin-based combination therapy (ACT) was given for free to patients with malaria symptoms and positive RDT test at the four sites, except in Saponé where ACT was not free of charge.
Among the malaria control measures evaluated at the individual level, mosquito nets were the most frequently used in both countries (Table 3). In Burkina Faso, 88.6–97.0% of children slept under a mosquito net the night before the visit: the vast majority were new (≥95.5% less than 1 year) and impregnated (≥98.5%), and less than 5% were pierced/torn, as reported to the investigators. In Senegal, 64.7–80.2% of children slept under a mosquito net the night before the visit. In Keur Socé, ≥99.2% of bed nets were new and impregnated, but ≥41.2% of them were also pierced/torn. In Niakhar, ≤18.3% of bed nets were new and impregnated, and ≥43.0% of them were pierced/torn. In Burkina Faso, no differences in parasite density were observed between children who slept or did not sleep under a bed net the night before the visit.
In Burkina Faso, the secondmost common malaria control measure was the use of mosquito coils, with a larger extent in Nouna (8.4% of children) compared to Saponé (0.8% of children). In Senegal, the secondmost common malaria control measure was the use of traditional repellents, which were not used in Burkina Faso, and the highest number of children using traditional repellents was registered in Niakhar (37.3% of children).
Exploratory analyses in Burkina Faso suggested that the use of any malaria treatment or other medication in the past 14 days at both the Nouna and Saponé sites, and the use of insecticide sprays at the Nouna site had a potential impact on the occurrence of P. falciparum parasitaemia (Table 4). Concerning the other factors, rural vs urban localization, natural vs cement floor, open vs closed drinking water source, and availability of electricity in the house in Nouna, and age and iron vs grass/palm roof in Saponé were also shown to have a potential impact on the occurrence of P. falciparum parasitaemia (Table 4). In the Senegalese centres, the 95% of all unadjusted ORs included the value ‘1’ for the assessed malaria control measures and risk factors due to the low number of infected children.
Discussion
Although efforts to control malaria infections have expanded considerably over the last years, this disease remains a major cause of morbidity and mortality in many sub-Saharan Western African countries [1, 20]. In this study, a much higher PP of P. falciparum was observed during the peak of malaria transmission in the two centres in Burkina Faso, where malaria endemicity is moderate to high, than in the two Senegalese centres, where malaria endemicity is low. A lower proportion of children with gametocytes, who constitute a parasite reservoir responsible for malaria transmission, was also observed in Senegal [21].
In Senegal, the prevalence of P. falciparum ranged between 0.5 and 1.5% across both age groups, and was the lowest at the Keur Socé site. The low prevalence observed in Keur Socé was in line with previous studies conducted in 2010 in the same area in children younger than 10 years (0.3% [95% CI 0.06–0.8]) [18], and in children younger than 5 years (1.5% [95% CI 0.7–2.6]) [22]. In Burkina Faso, 41.9–75.4% of children across both age groups and both sites were infected with P. falciparum. These results were in line with a previous study suggesting that the Saponé district is a stable malaria transmission area, where the malaria burden remained significant despite the introduction of effective medications and control measures [23]. However, these findings did not confirm the decline in malaria transmission previously observed in children and adults in the region of Nouna, where PP over the rainy season decreased from 78.9 in 2000 to 58.4% in 2009, 55.9% in 2010 and 49.3% in 2011 [15]. This discrepancy may be explained by between-study differences in terms of recruitment period, as participants were enrolled in October in the previous study and mainly in November in this study, and age, as this study was limited to children and the other study recruited participants from all age groups.
In this study, the prevalence of P. falciparum was lower in infants than in older children, which is in line with previous observations [20]. Potential explanations for the low prevalence in infants include the protection by maternal antibodies, and the fact that infants are less attractive to mosquitoes [20, 24, 25] and spend less time outdoors after sunset.
Infections with other Plasmodium species were scarce, with no infection with P. vivax and only a few cases with P. malariae and P. ovale, which is in line with other studies in Burkina Faso [15, 26], and with the World Malaria Report of WHO [2].
In Burkina Faso, malaria control policies include free distribution of ITNs, intermittent preventive treatment for pregnant women, treatment of malaria cases with ACT, and seasonal malaria chemoprevention [27]. In Senegal, malaria control measures recommended by WHO, including clinical management of malaria cases using RDTs and ACT, universal coverage of LLINs, IRS and intermittent preventive treatment, have been implemented since 2005, resulting in a decreased malaria burden [16]. These results suggest that most recommended malaria control measures were actually used at the study site level, except the distribution of ITNs which were not free of charge in Nouna and not included in the policies in Saponé, and the distribution of LLINs which was limited to children younger than 5 years and pregnant women in Niakhar. The only recommended malaria control measures evaluated at individual level were the use of mosquito bed nets and IRS. Mosquito nets were frequently used in Burkina Faso (88.6–97.0%) and Senegal (64.7–80.2%), and the majority were new and impregnated. In Burkina Faso, PP was higher than expected given the strong bed net coverage and the national recommendations for usage of malaria treatment. The similar proportion of infected and uninfected children who slept under a bed net the night before the visit and the absence of observed differences in terms of parasite density, were other unexpected findings. However, since the vast majority of children slept under a bed net, the power to detect a significant difference was low. Moreover, the proportion of children sleeping under a bed net and the number of new and impregnated bed nets might have been overestimated because bed nets were not inspected and their presence was not confirmed by study staff. Similar results were obtained in a previous study showing no effect of the ITN campaign in 2010 on the proportion of young children with P. falciparum parasitaemia after the rainy season in the Nouna area [28]. In Senegal, the low use of IRS was unexpected since it is recommended by the national guidelines. Besides the recommended control measures, the use of additional malaria control measures was also evaluated. In both countries, only a small number of children used mosquito coils or insecticide sprays. Traditional repellents (plant-based methods or petroleum oils [29]) were the secondmost common malaria control measure in Senegal, but these were not used in Burkina Faso.
In Burkina Faso, exploratory analyses suggested that malaria control measures having an impact on the P. falciparum infection status included the use of malaria treatment or other medications in the past 14 days and the use of insecticide sprays. Other factors influencing malaria occurrence included age, the main house construction material (natural floor and grass/palm roof), lack of electricity in the house, and rural residence.
The main strengths of this cross-sectional study are the indicators of the high quality of data collection, as no child was excluded from the total cohort, and the low number of protocol deviations, which were all considered as minor. The limitations included the low number of sites per country and the small sample size per site. Moreover, the results from a single cross-sectional survey should be interpreted cautiously because they do not take annual fluctuations of malaria transmission into account and they may not accurately represent the average MTI in endemic areas. The PP in Saponé could have been slightly underestimated since the peak in malaria transmission occurs in September in this area [16]. Another limitation was the potential underestimation of the PP when microscopy is used alone, especially in Senegal where malaria transmission is reduced and individuals may carry sub-microscopic malaria parasites [18].
The estimation of PP could be improved if microscopy results were confirmed by molecular detection techniques. Polymerase chain reactions (PCR) have a higher sensitivity than microscopy, but this technique is not frequently used in routine clinical practice due to its high cost. An estimate of PCR prevalence could be obtained by using a tool that has been developed to assess the relationship between microscopy and PCR measures [30]. Finally, the potential differences observed in this study and the evaluation of the impact of the various factors on the P. falciparum infection status were based on exploratory analyses, which should be interpreted with caution because there was no adjustment for multiplicity and no analysis on multi-collinearity was done before the regression.
Conclusions
This study showed that the prevalence of P. falciparum was much higher in the two sites in Burkina Faso with moderate-to-high malaria endemicity compared with the two sites in Senegal with low malaria endemicity. Mosquito nets were frequently used in both countries, but additional malaria control measures evaluated at individual level were uncommon. Exploratory analyses suggested that control measures having an impact on the P. falciparum infection status included the use of malaria treatment, other medications and insecticide sprays. In the centres with moderate-to-high malaria endemicity, age, main house construction material and lack of electricity in the house were also associated with an increased malaria occurrence. The high PP observed in the two sites in Burkina Faso suggests that new malaria control measures are needed in these areas.
Abbreviations
- ACT:
-
artemisinin-based combination therapy
- CI:
-
confidence interval
- HDSS:
-
Health and Demographic Surveillance Systems
- IRS:
-
indoor residual spraying
- ITN:
-
insecticide-treated net
- JTEG:
-
Joint Technical Expert Group
- LLIN:
-
long-lasting insecticidal net
- MTI:
-
intensity of malaria transmission
- OR:
-
odds ratio
- PCR:
-
polymerase chain reaction
- PP:
-
parasite prevalence
- RDT:
-
rapid diagnostis test
- SAS:
-
statistical analysis systems
- SD:
-
standard deviation
- WHO:
-
World Health Organization
References
WHO. Malaria vaccine: WHO position paper. Wkly Epidemiol Rec. 2016;91:33–51.
WHO. World malaria report. Geneva: World Health Organization; 2014. http://www.who.int/malaria/publications/world_malaria_report_2014/report/en/. Accessed 23 May 2016.
Meeting of the Strategic Advisory Group of Experts on Immunization. Conclusions and recommendations. Wkly Epidemiol Rec. 2015;2015(90):681–99.
The RTS,S Clinical Trials Partnership. Efficacy and safety of the RTS, S/AS01 malaria vaccine during 18 months after vaccination: a phase 3 randomized, controlled trial in children and young infants at 11 African sites. PLoS Med. 2014;11:e1001685.
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, et al. Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009;361:455–67.
Noor AM, Kinyoki DK, Mundia CW, Kabaria CW, Mutua JW, Alegana VA, et al. The changing risk of Plasmodium falciparum malaria infection in Africa: 2000–10: a spatial and temporal analysis of transmission intensity. Lancet. 2014;383:1739–47.
Protopopoff N, Matowo J, Malima R, Kavishe R, Kaaya R, Wright A, et al. High level of resistance in the mosquito Anopheles gambiae to pyrethroid insecticides and reduced susceptibility to bendiocarb in north-western Tanzania. Malar J. 2013;12:149.
Breman JG. Eradicating malaria. Sci Prog. 2009;92(Pt 1):1–38.
Greenwood BM, Fidock DA, Kyle DE, Kappe SH, Alonso PL, Collins FH, et al. Malaria: progress, perils, and prospects for eradication. J Clin Invest. 2008;118:1266–76.
The RTS,S Clinical Trials Partnership. First results of phase 3 trial of RTS, S/AS01 malaria vaccine in African children. N Engl J Med. 2011;365:1863–75.
The RTS,S Clinical Trials Partnership. A phase 3 trial of RTS, S/AS01 malaria vaccine in African infants. N Engl J Med. 2012;367:2284–95.
The RTS,S Clinical Trials Partnership. Efficacy and safety of RTS, S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet. 2015;386:31–45.
European Medicines Agency (EMA). First malaria vaccine receives positive scientific opinion from EMA. EMA/CHMP/488348/2015. http://www.ema.europa.eu/docs/en_GB/document_library/Press_release/2015/07/WC500190447.pdf. Accessed 29 Feb 2016, 2015.
Diboulo E, Sie A, Diadier DA, Voules DA, Ye Y, Vounatsou P. Bayesian variable selection in modelling geographical heterogeneity in malaria transmission from sparse data: an application to Nouna Health and Demographic Surveillance System (HDSS) data, Burkina Faso. Parasit Vectors. 2015;8:118.
Geiger C, Agustar HK, Compaore G, Coulibaly B, Sie A, Becher H, et al. Declining malaria parasite prevalence and trends of asymptomatic parasitaemia in a seasonal transmission setting in North-Western Burkina Faso between 2000 and 2009–2012. Malar J. 2013;12:27.
Ilboudo-Sanogo E, Tiono BA, Sagnon N, Cuzin Ouattara N, Nebie I, Sirima SB. Temporal dynamics of malaria transmission in two rural areas of Burkina Faso with two ecological differences. J Med Entomol. 2010;47:618–24.
Ndiath M, Faye B, Cisse B, Ndiaye JL, Gomis JF, Dia AT, et al. Identifying malaria hotspots in Keur Soce health and demographic surveillance site in context of low transmission. Malar J. 2014;13:453.
Sylla K, Tine RC, Ndiaye M, Sow D, Sarr A, Mbuyi ML, et al. Sero-epidemiological evaluation of Plasmodium falciparum malaria in Senegal. Malar J. 2015;14:275.
Vafa M, Troye-Blomberg M, Anchang J, Garcia A, Migot-Nabias F. Multiplicity of Plasmodium falciparum infection in asymptomatic children in Senegal: relation to transmission, age and erythrocyte variants. Malar J. 2008;7:17.
Ceesay SJ, Casals-Pascual C, Erskine J, Anya SE, Duah NO, Fulford AJ, et al. Changes in malaria indices between 1999 and 2007 in The Gambia: a retrospective analysis. Lancet. 2008;372:1545–54.
Ouedraogo AL, Bousema T, Schneider P, de Vlas SJ, Ilboudo-Sanogo E, Cuzin-Ouattara N, et al. Substantial contribution of submicroscopical Plasmodium falciparum gametocyte carriage to the infectious reservoir in an area of seasonal transmission. PLoS ONE. 2009;4:e8410.
Tine RCK, Faye B, Ndour CT, Sylla K, Sow D, Ndiaye M, et al. Parasitic infections among children under 5 years in Senegal: prevalence and effect on anaemia and nutritional status. ISRN Parasitol. 2013;2013:272701.
Ouedraogo A, Tiono AB, Diarra A, Sanon S, Yaro JB, Ouedraogo E, et al. Malaria morbidity in high and seasonal malaria transmission area of Burkina Faso. PLoS ONE. 2013;8:e50036.
Lindsay S, Ansell J, Selman C, Cox V, Hamilton K, Walraven G. Effect of pregnancy on exposure to malaria mosquitoes. Lancet. 2000;355:1972.
Verhulst NO, Qiu YT, Beijleveld H, Maliepaard C, Knights D, Schulz S, et al. Composition of human skin microbiota affects attractiveness to malaria mosquitoes. PLoS ONE. 2011;6:e28991.
Gnémé A, Guelbéogo WM, Riehle MM, Tiono AB, Diarra A, Kabré GB, et al. Plasmodium species occurrence, temporal distribution and interaction in a child-aged population in rural Burkina Faso. Malar J. 2013;12:67.
Tiono AB, Kangoye DT, Rehman AM, Kargougou DG, Kabore Y, Diarra A, et al. Malaria incidence in children in South-West Burkina Faso: comparison of active and passive case detection methods. PLoS ONE. 2014;9:e86936.
Louis VR, Schoeps A, Tiendrebeogo J, Beiersmann C, Ye M, Damiba MR, et al. An insecticide-treated bed-net campaign and childhood malaria in Burkina Faso. Bull World Health Organ. 2015;93:750–8.
Ntonifor NN, Ngufor CA, Kimbi HK, Oben BO. Traditional use of indigenous mosquito-repellents to protect humans against mosquitoes and other insect bites in a rural community of Cameroon. East African Med J. 2006;83:553–8.
Okell LC, Bousema T, Griffin JT, Ouedraogo AL, Ghani AC, Drakeley CJ. Factors determining the occurrence of submicroscopic malaria infections and their relevance for control. Nat Commun. 2012;3:1237.
Authors’ contributions
BC, ADial, JYP, ERB, AS, SS, CS, and MY designed the study. EHB, MB, GC, BC, MdB, ADial, ADiar, BF, MN, AN, EO, AO, JYP, ERB, AS, SS, CS, KS, RT, AT, and MY collected the data. EHB, MB, GC, BC, MdB, ADial, BF, MN, EO, AO, JYP, AS, SS, CS, RT, and AT performed or supervised the analysis. MB, MdB, ADial, JYP, ERB, AS, SS, CS, AT, and EAU interpreted the data. All authors reviewed and commented on a draft version of the manuscript and gave their final approval for it to be submitted for publication. All authors read and approved the final manuscript.
Acknowledgements
The authors thank the study participants. They also acknowledge the investigators and their clinical teams for their contribution to the study and their support and care of participants. The authors thank the global and regional clinical teams of GlaxoSmithKline Vaccines for their contribution to the study, the R&D group for analyses of laboratory work, the scientific writers for clinical protocol and clinical report writing and the statistician team for input on statistical analysis. The authors also thank Myriam Wilbaux (XPE Pharma & Science, Belgium c/o GlaxoSmithKline Vaccines) for publication management and Claire Verbelen and Alexandra Arion (XPE Pharma & Science, Belgium) for drafting the manuscript.
Competing interests
MdB and JYP are employees, and ERB a former employee, of the GSK group of companies. EAU is a former WHO TDR fellow at the GSK group of companies.
Availability of data and materials
The authors declare that all data supporting the findings of this study are available within the article.
Ethics approval and consent to participate
This study was designed and conducted according to the principles from the Declaration of Helsinki, Good Clinical Practice guidelines and all other applicable regulatory requirements. The study protocol, the informed consent and other information that required pre-approval were reviewed and approved by national and local Ethics Committees: the Comité d’Éthique pour la Recherche en Santé du Burkina for the Saponé and Nouna sites and in addition the Comité Institutionnel de Bioéthique du Centre National de Recherche et de Formation sur le Paludisme (Ouagadougou) for the Saponé site and the Comité Institutionnel d’Éthique du Centre de Recherche en Santé de Nouna for the Nouna site in Burkina Faso, and the Comité National d’Éthique et de Recherche en Santé for the Senegalese sites. Prior to any study-specific procedure, a written informed consent was obtained from the parents or legally acceptable representative of every child enrolled in the study.
Funding
GlaxoSmithKline Biologicals SA was the funding source and was involved in all stages of the study conduct and analysis. GlaxoSmithKline Biologicals SA also funded all costs associated with the development and submission of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Aldiouma Diallo, Ali Sié, Sodiomon Sirima and Khadime Sylla contributed equally to the work
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Diallo, A., Sié, A., Sirima, S. et al. An epidemiological study to assess Plasmodium falciparum parasite prevalence and malaria control measures in Burkina Faso and Senegal. Malar J 16, 63 (2017). https://doi.org/10.1186/s12936-017-1715-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-017-1715-1