Abstract
Background
During the last decade, Colombia presented a significant decrease in malaria clinical cases and associated mortality. However, there is a lack of reliable information about the prevalence and characteristics of complicated malaria cases as well as its association with different Plasmodium species. A description of the epidemiological and clinical aspects of complicated malaria in Colombia is presented here.
Methods
A descriptive study was conducted using data collected between 2007 and 2013 by the Public Health Surveillance System (SIVIGILA). Demographic and clinical features were described. Frequency of complicated malaria cases, annual parasite index (API) and annual percent change (APC) for trend modelling by gender and age were also calculated.
Results
A total of 547,542 malaria cases were recorded by SIVIGILA during the study period, of which 2553 (0.47 %) corresponded to complicated cases with similar distribution by Plasmodium vivax and Plasmodium falciparum species. Mixed infections were found in 153 cases (6.0 %). Trend modelling of the API for complicated malaria for all parasite species showed a non-significant increase throughout the years (APC 14.4 %; 95 % CI −4.3 to 36.6 %). Complicated malaria individuals were mostly males (62.2 %) and young adults (median age of 23 years). Notably, 72.4 % of the patients attended for malaria diagnosis >72 h after symptoms onset and 17 % reported malaria episodes in the last 30 days. All patients received anti-malarial treatment, but only 40 % received the first-line as recommended by the Colombian guidelines. Overall, hepatic and renal complications were the most common severe manifestations (63.6 %). Whereas hepatic and pulmonary complications were more common in P. vivax infections, renal and cerebral complications were significantly more frequent in patients with P. falciparum. In contrast with mono-infected patients, severe anaemia and shock were more frequent in patients with mixed infection.
Conclusion
In contrast with the malaria-decreasing trend over the last years, the complicated malaria trend showed a non-significant annual increase. Therefore, in addition to existing national policies on early diagnosis and prompt anti-malarial treatment, more efforts have to be committed addressing the delayed diagnosis and inadequate treatment found in this study. Improving malaria notification forms, medical assistance skills, and capacity should be prioritized.
Similar content being viewed by others
Background
Malaria continues to be an important public health problem in the developing world with 214 million clinical cases and 438,000 deaths estimated worldwide in 2015. Plasmodium falciparum is the predominant species worldwide responsible for ~94 % of malaria cases [1]. Conversely, in the Americas region, where malaria transmission is typically defined as hypoendemic and unstable (annual parasite index, API < 0.1 per 1000 per year) about 71 % of malaria cases are due to Plasmodium vivax [1]. In 2014, Colombia was the third most endemic country in Latin America (LA) and reported 17 % of the total 390,000 malaria cases [1]. Nonetheless, the country has displayed a malaria decreasing trend in prevalence and mortality the last decade; from 121,629 cases and 87 deaths in 2005 to 40,763 cases and 17 deaths in 2014 [1]. However, there is no reliable information about trends regarding complicated malaria cases.
Malaria exhibits a broad spectrum of clinical manifestations, including asymptomatic infection, uncomplicated and complicated malaria. This spectrum depends on multiple parasite, host and environmental factors [2–4]. Whereas in areas of high malaria transmission, individuals continuously exposed to Plasmodium develop partial protection for severe symptoms at an early age [4]; under conditions of low and unstable malaria transmission, individuals of all age groups may present with acute or severe disease as a consequence of low levels of naturally acquired immunity, although also subclinical infections are detected [4, 5].
In Colombia, a high frequency of uncomplicated P. vivax and P. falciparum malaria was reported recently [6], which appears to correlate with the relatively low malaria transmission and early diagnosis [7]. However, only a few studies have specifically focused on the description of complicated malaria cases in Colombia [8–14]. Before 2010, the criteria used for defining severe malaria in Colombia were the same established by the WHO for severe falciparum malaria [15], which were defined based on high transmission areas. In 2010, the Colombian Ministry of Health (MoH) adapted these criteria to the Colombian population, establishing more conservative parameters of complications to improve the detection and ensure a more effective treatment of these cases (Table 1).
In 2010, during a malaria outbreak in Colombia, 623 (0.5 %) complicated malaria cases were diagnosed among the 117,108 total cases reported to the Public Health Surveillance System (SIVIGILA) [16]. In this outbreak, the proportion of complicated malaria cases was similar for P. vivax and P. falciparum, with most patients (70.1 %) in the 15–64 years age group. In this and other studies [6, 17] hepatic and renal dysfunction were the most frequently reported complications. However, some studies have reported either hyperparasitaemia [10], severe anaemia [9, 17], or severe thrombocytopaenia [8, 13] as main malaria complications in Colombia.
All complicated malaria studies conducted in Colombia have been restricted to two of the most endemic areas in the country (Northwestern and Pacific regions), with many of them presenting gaps regarding epidemiological and clinical characteristics of complicated malaria cases [6, 8–13, 17–20]. Indeed, associations between Plasmodium species and clinical profile have been hardly explored [6, 8, 11, 12]. The aim of this study was to describe the clinical and epidemiological characteristics of complicated malaria in Colombia using national epidemiological records obtained by SIVIGILA from the whole country during the 2007–2013 period.
Methods
Study design and surveillance system
A descriptive study was conducted using data from the Colombian Public Health Surveillance System (SIVIGILA) for the 2007–2013 period. Briefly, all malaria cases including complicated and deaths cases are reported to the SIVIGILA by the primary data generating units (PDGU) and the information units (IU). The PDGU are the health institutions or points-of-care (POC) from both the private and the public system, where microscopists and physicians report to SIVIGILA. The IU are mobile or permanent malaria-diagnosis posts, where a trained and certified “primary agent” usually from the community is responsible for malaria diagnosis, notification and treatment of uncomplicated malaria cases. Malaria infection is confirmed by microscopic examination of Giemsa-stained thick blood smear (TBS) or by a positive rapid diagnostic test [21]. Uncomplicated malaria cases are reported on a weekly basis while complicated cases and deaths cases are reported on a daily basis [22].
Case definitions
Case definitions were used as established by the Colombian MoH guidelines [21, 22]. A malaria case was defined by clinical malaria manifestations, i.e., history of fever and a positive TBS or RDT, regardless of the parasite species. Confirmed complicated malaria was defined as a malaria case with one or more of the clinical or laboratory parameters as described in Table 1. Complications are reported as it is discriminated in the SIVIGILA malaria notification forms: hepatic, renal, pulmonary and cerebral complication.
Database mining and quality assurance
Databases were refined in agreement with SIVIGILA recommendations. Briefly, these recommendations included verification of data integrity, which means calculating the proportion of “empty data” and “no information data” for each study variable in the notification form. Only variables with integrity higher than 85 % were included in the study analyses. Integrity for demographic and epidemiological variables was higher than 99 %, whereas in some clinical and laboratory variables such as hyperemesis, shock, haemoglobin <5 g/dL and platelet counts <100,000 platelets/μL integrity was 88 %.
Statistical analysis
Information was processed using Microsoft Excel spreadsheets and analysed using GraphPad Prism version 6.0 (GraphPad Software, San Diego, California, USA). The descriptive analysis included demographic and clinical variables. Univariate analysis was performed for all variables. Frequencies, measures of central tendency and dispersion were calculated. Chi square test was used to compare proportion differences. Odds ratios (OR) and 95 % confidence interval (95 % CI) were also calculated. A p value <0.05 was considered statistically significant.
The API for complicated malaria was calculated by relating the total number of complicated malaria cases with the population at risk multiplied by 100,000. Specific rates by 5-year age groups and gender were calculated and expressed as the number of cases per 100,000 individuals per year. The Joinpoint Regression® software 4.0.4 (Surveillance Research Program, National Cancer Institute, Bethesda, USA) was used to calculated complicated malaria trends [23] adjusted by gender and API by 5-year age groups from 2005 national census [24]. Briefly, this method allows to identify the time point (year in this case) where a significant change happens and to estimate the magnitude of this change through the annual percent change (APC). A model using a maximum of three joinpoints was established to fits the simplest joinpoint model that the data allow. Heteroscedasticity was assumed and Monte Carlo Permutation method and Bonferroni correction were used as tests of significance. Trends were interpreted as (i) rising when 95 % IC of APC was >0 and statistically significant; (ii) decreasing when 95 % CI of APC was <0 and statistically significant; (iii) stable when 95 % CI of APC was between −0.5 and 0.5 and not statistically significant; (iv) non-significant when 95 % CI of APC was <−0.5 or >0.5 and not statistically significant. A p value <0.05 was considered statistically significant.
Results
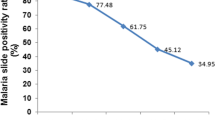
Between 2007 and 2013, a total of 547,542 malaria cases were diagnosed and reported to SIVIGILA, with a notably decreasing trend over those years (Fig. 1a). While most of the cases corresponded to mono-infection caused by P. vivax (71.4 %) or P. falciparum (27.4 %), mixed malaria infection by both species were less frequent (1.2 %). During the same period, 2553 (0.47 %) complicated malaria cases were reported. A total of 1274 (49.9 %) of them were caused by P. falciparum, 1126 (44.1 %) by P. vivax and 153 cases (6.0 %) corresponded to mixed malaria infections (P. falciparum plus P. vivax; Fig. 1b). However, the average proportion of complicated over total cases per parasite species was higher for mixed infection than for P. falciparum (2.6 vs 0.9 %, respectively) and P. vivax (0.3 %; Fig. 1c). Of the total complicated cases, 1139 (44.6 %) were diagnosed between 2010 and 2011 (Fig. 1b). The highest numbers of cases were reported in the first semesters of 2010, 2011 and 2013 respectively, which corresponds with the average monthly highest incidence of malaria in Colombia, although transmission is reported throughout the year.
Malaria cases in Colombia. The number of total malaria cases (a) and complicated malaria cases (b) reported monthly between 2007 and 2013 are shown. Black dashed line (b), corresponds to the number of malaria-related deaths per year. c Percentage of complicated malaria cases over total cases according to the parasite species
Most complicated malaria cases were recorded in the departments of Antioquia, Córdoba, Chocó, Nariño and Valle del Cauca (Fig. 2), all of them with endemic malaria transmission in several municipalities. Notably, four malaria-endemic municipalities in the Pacific Coast: Quibdó (Chocó), Buenaventura (Valle del Cauca), Istmina (Chocó), and Tumaco (Nariño) reported 21 % of the total complicated cases in the whole country. Moreover, cities without malaria transmission also reported complicated cases because patients from endemic municipalities are regularly referred to tertiary hospitals from other departments. Of those, Cali (Valle del Cauca) reported 7.1 % of the complicated cases, mainly referred from Buenaventura and Quibdó.
Population characteristics
Individuals with complicated malaria were mostly males (62.2 %; Table 2), with a median age of 23 years (range 0–94 years). The highest number of cases was reported in young adults between 20 and 29 years of age (n = 759, 29.7 %) and children younger than 5 years of age (n = 330, 12.9 %; Fig. 3). In children ≤15 years of age, mixed malaria was more frequent than single infections (p = 0.012; Table 2). Overall, patients presented late at health facilities for malaria diagnosis. Notably, 72.4 % of the patients attended for malaria diagnosis >72 h after symptoms onset (Table 2), a situation that was more frequent in the Pacific region (Additional file 1) and in patients with mixed malaria infection (p = 0.04).
Seventeen percent of the patients reported malaria episodes in the last 30 days, mainly those with mixed malaria infection. Only 4 % of cases referred blood transfusion history in the last month. About half of cases (47.5 %) had a history of travelling to a malaria-endemic region during the 15 days prior to diagnosis, 37 % of them to a distant region from their residency, mainly to the Pacific and Urabá regions; a situation that was more common in P. vivax-infected patients (p < 0.001). Although all patients received anti-malarial treatment according to the Colombian guidelines [21], only 40 % of patients received first-line treatment for complicated malaria whereas the remaining 60 % received either second or third line of treatment (Table 2). Unfortunately, complaints such as poor compliance of either dose or duration of treatment cannot be ruled out, as those are not registered in the malaria notification forms.
Trend modelling of the API
The API for complicated malaria was 0.8 for 100,000 (1.01 for male and 0.60 for female). Although some differences in the API were observed between P. falciparum and P. vivax infected patients (0.40 and 0.35 respectively) the APC for complicated malaria for both parasite species showed a non-significant annual increase in the whole population between 2007 and 2013 (14.4 %; 95 % CI −4.3 to 36.6). Similar trends were observed for P. falciparum (15.0 %; 95 % CI −1.7 to 34.7) and P. vivax (14.6 %; 95 % CI −7.8 to 42.5; Fig. 4). Age-stratified analysis (Additional file 2) showed a significant rising trend between 2007 and 2010 in the 0 to 4 years group (121.0 %; 95 % CI 8.4–350.5) and a stable trend between 2010 and 2013 (−13.0 %; 95 % CI −39.0 to 24.1). A rising trend between 2007 and 2013 was also observed for women, particularly in those infected by P. falciparum (Table 3).
Clinical findings
Some specific symptoms and signs were reported in complicated patients in addition to those frequently observed in acute malaria episodes (e.g., fever, headache, chills, and myalgias). Compared to patients with P. vivax mono-infections, those with P. falciparum had a higher risk of confusion (OR 1.76, 95 % CI 1.20–2.62), clinical jaundice (OR 1.60, 95 % CI 1.06–2.44), somnolence (OR 1.50, 95 % CI 1.17–1.93), and hepatomegaly (OR 1.34, 95 % CI 1.07–1.69). Interestingly, these manifestations were even more frequent in patients with mixed malaria infections (Table 4).
According to SIVIGILA classification, hepatic (33 %) and renal (31 %) complications were the most frequently presented regardless of parasite species. Renal (34.7 %) and cerebral complications (15.3 %) were significantly more common in patients with P. falciparum, while hepatic (37 %) and pulmonary complications (15.1 %) were more frequent in P. vivax cases (Table 5). Furthermore, a higher proportion of severe anaemia (10.9 %) and shock (3.3 %) was seen in patients with mixed malaria (Table 4).
Malaria-related deaths
During 2007 and 2013, 116 (0.02 %) malaria-related deaths were reported (Fig. 1b). Those remained relatively low and decreased during the study period, with a mean of 17 ± 5 deaths per year and a mean of 2.2 ± 0.6 deaths per 10,000 total malaria cases. The malaria-related fatality rate (over all malaria cases) ranged between 0.02 and 0.03 %. Although a similar number of deaths was reported in mono-infections, the fatality rate per species was higher in those infected by P. falciparum than P. vivax (0.03 vs 0.01 %). Moreover, the fatality rate for mixed infection was particularly high (0.2 %).
Discussion
Although Colombia has experienced a malaria-decreasing trend during the last decade [1], the observed trend for complicated malaria cases reflected a non-significant increase during 2007–2013 (APC 14.4 %; 95 % CI −4.3 to 36.6), with the highest number of cases reported after 2010 [16]. Notably, between 2007 and 2010 a significant rising trend for complicated malaria was found in children younger than 5 years of age and women mostly infected by P. falciparum. This could be explained by both the overall rise on the number of total malaria cases [16] and changes in complicated malaria criteria occurred in 2010. However, the proportion of total malaria cases in women compared to men remained similar during the study period. While changes in complicated malaria trend could be explained by a higher diagnosis rate due to more conservative definitions after 2010, improvement in the surveillance system and health care infrastructure should also be considered. Those data together suggest the need for new public health strategies focused on these vulnerable populations.
Complicated malaria represented 0.47 % of 547,542 malaria cases during 2007–2013, in agreement with a previous report of malaria outbreak using SIVIGILA information [16]. However, in a passive surveillance conducted between 2011 and 2013 was reported that 45 of 99 complicated malaria cases were not diagnosed and treated as such, but were classified during the laboratory data analyses [6], suggesting a possible underreporting of complicated malaria cases found here.
Although P. falciparum has been classically associated with a more severe clinical spectrum, there are multiple studies worldwide reporting an increasing number of severe manifestations in P. vivax infections [6, 9, 13, 17, 25–28], a relevant matter now on the malaria eradication agenda [29]. In this study, P. vivax was responsible for 44 % of complicated malaria cases, underscoring the importance of P. vivax malaria in a country where it causes about 70 % of malaria cases. Although the mechanisms involved in the clinical complications by P. vivax are not well understood [30, 31]; recent ex vivo studies have shown that P. vivax-infected red blood cells (Pv-iRBC) can adhere to endothelial cells [32–34], supporting the hypothesis that P. vivax undergoes sequestration in vivo.
Patients with mono-infections by P. falciparum had a higher risk of hepatic and neurological manifestations in comparison with P. vivax malaria patients. Non-severe thrombocytopaenia was found in almost half of complicated malaria cases, similar to a previous report in Colombia [6]. That is an important manifestation since altered platelet indices have been found as potential markers of severe malaria [18, 35]. Unfortunately, further information of severe thrombocytopaenia in patients studied here was not available.
Although severe anaemia was rather uncommon in mono-infections (~8 %), as also shown by other Colombian studies [6, 8, 10–13], renal and cerebral complications were significantly more common in patients with P. falciparum infections. In contrast, in patients with P. vivax, cerebral complications were less frequent (11 %), while hepatic and pulmonary complications were more common than in P. falciparum patients. The presence of other possible central nervous system pathogens has not been ruled out in this and other studies reporting malaria cerebral complications as reviewed in [28]. Indeed, it has been suggested that comma in P. vivax is 23 times less common than in P. falciparum infections [28]. The high number of cases with cerebral complications reported in this study contrasts significantly with previous reports from Colombia, with 1/92 complicated cases by P. falciparum [11], no cerebral malaria cases in 16 P. vivax complicated patients [13], and only one case of P. vivax cerebral malaria complicated with venous sinus thrombosis reported recently [36]. The contrasting high number of cerebral malaria cases reported to SIVIGILA, suggests an inappropriate classification probably due to errors during the filling or typing form process.
In contrast with mono-infected patients, complicated malaria was more frequent in patients with mixed infections, which presented commonly with hepatic and neurological manifestations, as well as severe anaemia and shock complications. Moreover, a high fatality rate was observed in those patients. Although some studies have suggested that P. vivax appears to attenuate the severity of the P. falciparum infection [37–39], others suggest that mixed infections could be associated with more severe disease, leading to a higher risk for severe anaemia, multiple organ dysfunction and mortality [12, 38, 40].
In agreement with other studies, a higher number of complicated malaria cases was found in young males [6, 16, 25, 28]; which could be explained by occupational factors such as mining, timber or farming that increase the risk of malaria infection. Notably, a diagnosis delay (>72 h after symptoms onset) was found in most patients, possibly due to either limited access to healthcare services (less developed on the Pacific Coast) or health staff failure to identify complicated malaria manifestations. Moreover, this delayed diagnosis increases the risk of anaemia [41]. Although a re-infection or relapse cannot be ruled out in patients reporting previous malaria episodes in the last month, which was significantly more common in cases with mixed infection, it suggests therapeutic failure or low adherence to anti-malarial treatment. Both delayed and the limited availability of the first line of anti-malarial drugs at health institutions could be responsible for higher parasite burden and secondary severe malaria.
These findings demonstrate the Colombian Health System faults in prompt recognition of complicated malaria patients as well as the difficulties around appropriate treatment provision; which may explain why the API for complicated malaria remained almost stable while API for total malaria cases decreased over the years. Although the databases were refined according to the national system, some data including demographic, epidemiological and clinical information were missed in less than 2 % of cases. Other constraints such as errors during the malaria notification form filling or typing process cannot be ruled out. Also, there may be misclassification of cases resulting from lack of adherence to case definitions, errors in species diagnosis -since molecular confirmation was not performed- and missing information about co-morbidities or co-infections. Although the Colombian guidelines use the same criteria to define complicated vivax and falciparum malaria [21], similar to the established by the WHO in 2014 [42]; the criterion of hyperparasitaemia must be re-evaluated in the Colombian guidelines since P. vivax invades reticulocytes and their parasite densities are usually lower than P. falciparum. Moreover, because the co-morbidities may modify the malaria episode course, this must be also included in the notification forms. Currently, the MoH is doing efforts in the reinforcement of health personnel knowledge and training about malaria disease and the correct notification process, especially in endemic areas with limited health infrastructure to strength the malaria information system in Colombia.
It is important to highlight that since the information reported here was obtained from the SIVIGILA, the data contained in the notification forms are the required for malaria surveillance and not for the clinical characterization. Thus, in this study malaria complications were presented as organ-related complications grouped in four categories (cerebral, pulmonary, hepatic, and renal complications) as appear in the SIVIGILA malaria case notification forms, instead of clinical and/or laboratory criteria of complications, as it is suggested by national and international guidelines. This categorization excludes several of the defined clinical and laboratory parameters but includes others in the notification forms under the clinical findings section. Therefore, parameters such as shock, haematological alterations, metabolic acidosis, haemoglobinuria, and hyperparasitaemia, which did not completely fit any of the four categories of complications, were excluded from the surveillance; suggesting considerable underreporting of total complicated malaria cases. Nevertheless, SIVIGILA malaria case notification forms were modified in 2016, reclassifying complications in six groups: cerebral, renal, hepatic, pulmonary, haematological, and other complication. Prospective studies that evaluate parasite (virulence, genetic profile, anti-malarial drug resistance) and host susceptibility factors (co-morbidities, co-infections, age of exposure, immunological and nutritional status) in conjunction with clinical and laboratory profile of complicated malaria patients should be conducted to improve existing knowledge of the clinical presentation spectrum and risks.
Conclusion
During the last decade, Colombia presented a significant decrease in malaria clinical cases and associated mortality. However, it appears that the prevalence of complicated malaria remained stable. Despite existing national policies on early diagnosis and prompt anti-malarial treatment to prevent complicated malaria cases, more efforts have to be committed to decrease the total number of malaria cases, including the complicated ones. These efforts should include taking action to improve the malaria notification forms, medical assistance skills and capacity as well as to increase the knowledge of malaria-related risk factors, morbidity and mortality.
Abbreviations
- APC:
-
annual percent change
- API:
-
annual parasitic index
- iRBC:
-
infected red blood cell
- IU:
-
information units
- MoH:
-
Ministry of Health
- PDGU:
-
primary data generating units
- OR:
-
odds ratio
- POC:
-
point-of-care
- SIVIGILA:
-
Public Health Surveillance System
- TBS:
-
thick blood smears
References
WHO. World Malaria Report 2015. Geneva: World Health Organization; 2015. p. 280.
Miller LH, Baruch DI, Marsh K, Doumbo OK. The pathogenic basis of malaria. Nature. 2002;415:673–9.
Langhorne J, Ndungu FM, Sponaas AM, Marsh K. Immunity to malaria: more questions than answers. Nat Immunol. 2008;9:725–32.
Doolan DL, Dobano C, Baird JK. Acquired immunity to malaria. Clin Microbiol Rev. 2009;22:13–36.
Bousema T, Okell L, Felger I, Drakeley C. Asymptomatic malaria infections: detectability, transmissibility and public health relevance. Nat Rev Microbiol. 2014;12:833–40.
Arevalo-Herrera M, Lopez-Perez M, Medina L, Moreno A, Gutierrez JB, Herrera S. Clinical profile of Plasmodium falciparum and Plasmodium vivax infections in low and unstable malaria transmission settings of Colombia. Malar J. 2015;14:154.
Rodriguez JC, Uribe GA, Araujo RM, Narvaez PC, Valencia SH. Epidemiology and control of malaria in Colombia. Mem Inst Oswaldo Cruz. 2011;106(Suppl 1):114–22.
Gonzalez LM, Guzman M, Carmona J, Lopera T, Blair S. Clinical and epidemiologic characteristics of 291 hospitalized patients for malaria in Medellin (Colombia). Acta Med Colomb. 2000;25:163–70 (in Spanish).
Arboleda M, Perez MF, Fernandez D, Usuga LY, Meza M. Clinical and laboratory profile of Plasmodium vivax malaria patients hospitalized in Apartado, Colombia. Biomedica. 2012;32(Suppl 1):58–67 (in Spanish).
Tobon A, Giraldo C, Pineros-Jimenez JG, Arboleda M, Blair S, Carmona-Fonseca J. The epidemiology of complicated falciparum malaria: case and controls study in Tumaco and Turbo, Colombia, 2003. Rev Bras Epidemiol. 2006;9:283–96 (in Spanish).
Tobon-Castano A, Giraldo-Castro C, Blair S. Prognostic value of clinical and parasitological signs for severe malaria in patients from Colombia. Biomedica. 2012;32(Suppl 1):79–94 (in Spanish).
Medina-Morales DA, Montoya-Franco E, Sanchez-Aristizabal VD, Machado-Alba JE, Rodriguez-Morales AJ. Severe and benign Plasmodium vivax malaria in Embera (Amerindian) children and adolescents from an endemic municipality in Western Colombia. J Infect Public Health. 2016;9:172–80.
O’Brien AT, Ramirez JF, Martinez SP. A descriptive study of 16 severe Plasmodium vivax cases from three municipalities of Colombia between 2009 and 2013. Malar J. 2014;13:404.
Piñeros-Jiménez JG, Arboleda M, Jaramillo JC, Blair S. Report of five cases of severe neonatal Plasmodium vivax malaria in Uraba, Colombia. Biomedica. 2008;28:471–9 (in Spanish).
WHO. Severe falciparum malaria. World Health Organization, communicable diseases cluster. Trans R Soc Trop Med Hyg. 2000;94(Suppl 1):1–90.
Chaparro P, Padilla J, Vallejo AF, Herrera S. Characterization of a malaria outbreak in Colombia in 2010. Malar J. 2013;12:330.
Pineros-Jimenez JG, Arboleda M, Jaramillo JC, Blair S. Report of five cases of severe neonatal Plasmodium vivax malaria in Uraba, Colombia. Biomedica. 2008;28:471–9.
Martínez-Salazar EL, Tobón-Castaño A. Platelet profile is associated with clinical complications in patients with vivax and falciparum malaria in Colombia. Rev Soc Bras Med Trop. 2014;47:341–9.
Pineros JG, Tobon-Castano A, Alvarez G, Portilla C, Blair S. Maternal clinical findings in malaria in pregnancy in a region of northwestern Colombia. Am J Trop Med Hyg. 2013;89:520–6.
López ML, Arango EM, Arias LR, Carmona-Fonseca J, Blair S. Intraleucocytic hemozoine as an indicator malaria complicated by Plasmodium falciparum. Acta Méd Colomb. 2004;29:80–7 (in Spanish).
MinSalud. Ministerio de la Protección Social. Colombia. Guía de atención clínica de malaria Ministerio de la Protección Social, Bogotá. 2010. p. 132.
INS. Protocolo para la vigilancia en salud pública de malaria. http://www.ins.gov.co/temas-de-interes/Documentacin%20Malaria/01%20Protocolo%20Malaria.pdf. Accessed 28 Aug 2015.
Carter KH, Singh P, Mujica OJ, Escalada RP, Ade MP, Castellanos LG, et al. Malaria in the Americas: trends from 1959 to 2011. Am J Trop Med Hyg. 2015;92:302–16.
DANE. Series de población 1985–2020. Colombia. http://www.dane.gov.co/index.php/poblacion-y-demografia/series-de-poblacion. Accessed 5 Feb 2015.
Rodriguez-Morales AJ, Benitez JA, Arria M. Malaria mortality in Venezuela: focus on deaths due to Plasmodium vivax in children. J Trop Pediatr. 2008;54:94–101.
Quispe AM, Pozo E, Guerrero E, Durand S, Baldeviano GC, Edgel KA, et al. Plasmodium vivax hospitalizations in a monoendemic malaria region: severe vivax malaria? Am J Trop Med Hyg. 2014;91:11–7.
Lacerda MV, Mourao MP, Alexandre MA, Siqueira AM, Magalhaes BM, Martinez-Espinosa FE, et al. Understanding the clinical spectrum of complicated Plasmodium vivax malaria: a systematic review on the contributions of the Brazilian literature. Malar J. 2012;11:12.
Rahimi BA, Thakkinstian A, White NJ, Sirivichayakul C, Dondorp AM, Chokejindachai W. Severe vivax malaria: a systematic review and meta-analysis of clinical studies since 1900. Malar J. 2014;13:481.
Arévalo-Herrera M, Soto L, Perlaza BL, Céspedes N, Vera O, Lenis AM, et al. Antibody-mediated and cellular immune responses induced in naive volunteers by vaccination with long synthetic peptides derived from the Plasmodium vivax circumsporozoite protein. Am J Trop Med Hyg. 2011;84:35–42.
Price RN, Tjitra E, Guerra CA, Yeung S, White NJ, Anstey NM. Vivax malaria: neglected and not benign. Am J Trop Med Hyg. 2007;77:79–87.
Anstey NM, Russell B, Yeo TW, Price RN. The pathophysiology of vivax malaria. Trends Parasitol. 2009;25:220–7.
Carvalho BO, Lopes SC, Nogueira PA, Orlandi PP, Bargieri DY, Blanco YC, et al. On the cytoadhesion of Plasmodium vivax-infected erythrocytes. J Infect Dis. 2010;202:638–47.
Lopes SC, Albrecht L, Carvalho BO, Siqueira AM, Thomson-Luque R, Nogueira PA, et al. Paucity of Plasmodium vivax mature schizonts in peripheral blood is associated with their increased cytoadhesive potential. J Infect Dis. 2014;209:1403–7.
De las Salas B, Segura C, Pabon A, Lopes SC, Costa FT, Blair S. Adherence to human lung microvascular endothelial cells (HMVEC-L) of Plasmodium vivax isolates from Colombia. Malar J. 2013;12:347.
Leal-Santos FA, Silva SB, Crepaldi NP, Nery AF, Martin TO, Alves-Junior ER, et al. Altered platelet indices as potential markers of severe and complicated malaria caused by Plasmodium vivax: a cross-sectional descriptive study. Malar J. 2013;12:462.
Pinzon MA, Pineda JC, Rosso F, Shinchi M, Bonilla-Abadia F. Plasmodium vivax cerebral malaria complicated with venous sinus thrombosis in Colombia. Asian Pac J Trop Med. 2013;6:413–5.
Luxemburger C, Ricci F, Nosten F, Raimond D, Bathet S, White NJ. The epidemiology of severe malaria in an area of low transmission in Thailand. Trans R Soc Trop Med Hyg. 1997;91:256–62.
Mayxay M, Pukrittayakamee S, Newton PN, White NJ. Mixed-species malaria infections in humans. Trends Parasitol. 2004;20:233–40.
Price RN, Simpson JA, Nosten F, Luxemburger C, Hkirjaroen L, ter Kuile F, et al. Factors contributing to anemia after uncomplicated falciparum malaria. Am J Trop Med Hyg. 2001;65:614–22.
Kochar DK, Das A, Kochar A, Middha S, Acharya J, Tanwar GS, et al. A prospective study on adult patients of severe malaria caused by Plasmodium falciparum, Plasmodium vivax and mixed infection from Bikaner, northwest India. J Vector Borne Dis. 2014;51:200–10.
Lopez-Perez M, Alvarez A, Gutierrez JB, Moreno A, Herrera S, Arevalo-Herrera M. Malaria-related anemia in patients from unstable transmission areas in Colombia. Am J Trop Med Hyg. 2015;92:294–301.
WHO. Severe malaria. Trop Med Int Health. 2014;19(Suppl 1):7–131.
Authors’ contributions
PEC and JP conceived and designed the study. PEC and JP analysed data. MLP, LR and SHV wrote the manuscript. SHV and MAH critically revised the manuscript and contributed to the discussion section. All authors read and approved the final manuscript.
Acknowledgements
We thank the Subdirección de Vigilancia y Control en Salud Pública-INS for their support and SIVIGILA for making the data available.
Competing interests
The authors declare that they have no competing interests.
Funding
This work was sponsored by the Ministry of Health of Colombia and the NIAID/ICEMR (U19AI089702). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Additional files
12936_2016_1323_MOESM1_ESM.tif
Additional file 1. Time between onset of symptoms and malaria diagnosis. Percentage of complicated malaria cases from total cases reported is shown for each indicated Colombian region according to time between onset of symptoms and malaria diagnosis.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chaparro-Narváez, P.E., Lopez-Perez, M., Rengifo, L.M. et al. Clinical and epidemiological aspects of complicated malaria in Colombia, 2007–2013. Malar J 15, 269 (2016). https://doi.org/10.1186/s12936-016-1323-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-016-1323-5