Abstract
Background
Malaria incidence has declined considerably over the last decade. This is partly due to a scale-up of control measures but is also attributed to increasing urbanization. This study aimed to analyse the association between malaria and urbanization and the effect of urbanicity on the acquisition of semi-immunity.
Methods
In 2012, children with fever presenting to St Michael’s Hospital Pramso/Ghana were recruited. The malaria-positive-fraction (MPF) of fever cases was calculated on community-level to approximate the malaria risk. The mean age of malaria cases was calculated for each community to estimate the acquisition of semi-immunity. The level of urbanicity for the communities was calculated and associations between MPF, urbanicity and immunity were modelled using linear regression.
Results
Twenty-six villages were included into the study with a mean MPF of 35 %. A linear decrease of 5 % (95 % CI: 4–6 %) in MPF with every ten-point increase in urbanicity was identified. The mean age of malaria patients increased by 2.9 months (95 % CI: 1.0–4.8) with every ten-point increase in urbanicity.
Discussion
The results confirm an association between an increase in urbanicity and declining malaria risk and demonstrate that the acquisition of semi-immunity is heterogeneous on a micro-epidemiological scale and is associated with urbanicity.
Similar content being viewed by others
Background
Plasmodium falciparum malaria is the most important parasitic disease worldwide with an estimated 1.1–1.4 billion people at risk of infection [1]. Despite a strong decrease in incidence and mortality in the last decade, the World Health Organization (WHO) estimates a total of 207 million clinical cases of malaria, resulting in approximately 627,000 deaths in 2012 [2]. The recent decline in incidence is largely due to a huge scale-up of malaria control efforts since 2003. However, the decline started before efforts were intensified and has occurred in regions that have not benefitted from these measures [3]. Among others, this effect has been attributed to economic development and urbanization in endemic areas [4]. The process of urbanization, including landscape modification, transformation of the environment and economic change, leads to entomological, parasitological and human behavioural changes reducing malaria transmission intensity [3, 5]. It is estimated that currently one-third of the world’s population lives in urban areas and further growth of urban populations is expected. This increase will mainly occur in the less developed regions of the world with a predicted rise from 0.41 billion in 2011 to 1.26 billion urban inhabitants in 2050 in the African region [6]. The speed of this process is particularly dramatic in West Africa, with an urban population growth rate of 6.3 % per annum [7].
Earlier studies on the differences between urban and rural malaria transmission often made comparisons on a regional [8] or even global scale [1, 3, 9]. Most of these studies compared malaria transmission on a binary scale between urban areas and a disjoint rural region, sometimes separated by hundreds of kilometres. However, this approach does not capture malaria transmission adequately as spatial heterogeneity is already observed over short distances [10], even between households [11].
It has been shown that changes in transmission intensity also influence the acquisition of immunity against malaria [12]. With declining transmission, the average age of patients with malaria increases and severe malaria also occurs in older children and adults. It is unclear to what extent urbanization influences the acquisition of immunity and how immunity varies over short distances. Understanding the heterogeneity of transmission on a micro-epidemiological scale and how it influences the acquisition of immunity is essential for an effective application of control measures and the development of new intervention strategies [11, 13, 14].
The aim of this study was to study the association between urbanicity and malaria and how this may influence the development of immunity on a micro-epidemiological level.
Methods
The study was conducted in the Bosomtwe district of the Ashanti Region in Ghana. Two sets of data were used for the analysis: (1) an individual-level survey containing data on residence, disease status and demography of children attending a local hospital; and, (2) a community-level survey containing data on community characteristics of villages located within the hospital catchment area.
Study site and study area
The Ashanti Region is located in the forest-belt of Ghana, characterized by wet tropical climate with a main rainy season from March to July and a minor rainy season from September to November. The vegetation in the study area is dominated by semi-deciduous forest, but farming activities thinned out much of the former closed forests. Malaria is endemic with high transmission intensity throughout the year [15].
Hospital survey
Patients were recruited at St Michael’s Hospital (SMH) in Pramso, a town of about 3300 inhabitants located 20 km southeast of the regional capital Kumasi, on one of the major roads leaving the city. SMH is the biggest health facility in the Bosomtwe district with a large general outpatient department (OPD) and four wards, one each for women, children and men and a maternity ward. The catchment area of SMH stretches from urban Kumasi and its suburbs in the northwest to rural areas of the Bosumtwe District in the southeast.
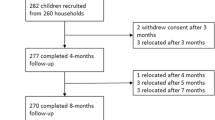
All children <15 years of age with fever (tympanic temperature ≥38 °C) presenting to the OPD during the study period (January to December 2012) were recruited if informed consent was given by their caregiver. A blood sample was taken by venipuncture and a questionnaire on basic demographic data was completed. Children were treated according to hospital guidelines. Children attending the hospital for a second time were only considered as a new case if this visit occurred >28 days after a previous visit.
Laboratory diagnostics
Thick and thin blood films for malaria parasite examination were prepared according to quality-controlled, standardized protocols. Two independent readers examined the slides and the mean of these readings was used to quantify parasitaemia as asexual parasites/µl. A third reading was performed in case of discrepancies in positivity, malaria species, or a less than threefold difference in quantification. An episode of malaria was defined as fever accompanied by an asexual parasite count of ≥5000/µl.
Community data
The catchment area of SMH was defined as a geographically continuous area around the hospital, which covered the residence of 95 % of SMH’s patients (Fig. 1). Data on community characteristics used to construct the urbanicity scale were retrieved from the ‘Ghana population and housing Census 2010’ [16]. Additional data on the availability of private services (e.g., banks, petrol stations) and information about road conditions and frequency of public transport were collected via systematic interviews conducted in each community.
Urbanicity scale
The urbanicity scale was constructed and validated according to the principles of scale development as described by DeVellis [17] and Netemeyer and Bearden [18]. Data used to establish the scale were selected by literature review and expert opinion. Eight components were defined within which variables were grouped: population, economic activity, education, healthcare, transportation, service-infrastructure, sanitation, and housing. Each component accounted for ten points. Consequently, the final scale ranged from 0 to 80 points. The components used to construct the scale are displayed in Table 1. To calculate each community’s urbanicity, score points were accumulated according to its particular characteristics. Unidimensionality of the scale was tested by exploratory factor analysis, Kaiser–Meyer–Olkin measure was used to assess sampling adequacy and internal consistency was validated using Cronbach’s alpha. For more details on scale construction and validation see Additional files 1 and 2.
Statistical analysis
The proportion of fever cases that fulfilled the malaria criteria was calculated for each community. To retrieve robust estimates, the malaria positive fraction (MPF), i.e., number of patients with malaria over all patients with fever from each community) was calculated only for communities with at least 20 study participants. As it can be expected that in areas of low transmission older children are still susceptible to malaria, therefore leading to a higher mean age of malaria patients compared to areas of high transmission, the mean age of malaria cases in each community was calculated to approximate the local age at infection and to estimate the acquisition of immunity. Summary statistics for the study participants are presented as proportions for dichotomous or categorical variables and as medians with interquartile range (IQR) or means with standard deviation (SD) for continuous variables.
First, bivariate linear regression analysis was performed: (1) between urbanicity (score) and MPF, to assess the association between urbanicity and malaria prevalence; (2) between urbanicity (score) and the mean age of malaria patients in each community to assess an association between urbanicity and acquisition of immunity to malaria; and, (3) between MPF and mean age of malaria patients in each community to assess an association between malaria prevalence and acquisition of immunity to malaria. Second, it was decided a priori to repeat the three models including insecticide-treated nets (ITNs) as a covariate, as the use of ITNs is known to be associated with malaria as well as urbanicity [19], and could be a potential confounder.
To exclude age of patients at presentation as a potential confounder, linear regression analysis was also conducted for MPF and urbanicity and the mean age of presentation for all children from a village, irrespective of malaria positivity. As no association was seen between mean age of all patients and MPF or urbanicity, age was not included in the multivariate regression model between MPF and urbanicity. In addition, linear regression models were applied to assess the association between the particular score-components (each ranging from 0 to 10 points) and MPF to analyse which components have the strongest association with MPF. A multivariate regression model was established to assess co-linearity between variables.
All regression estimates were weighted by the number of observations from each community as the models used proportions (MPF) and means (age) as outcome measures. All measures of increase/decrease in the dependent variables were calculated based on a ten-point increase in the urbanicity score. An increase of ten points on the score would be achieved, e.g., by an increase in the proportion of households with tap water from the lowest to the highest quartile or an increase of the population from 800 to 8000 plus the availability of a post office and a bank (Table 1). All analyses were carried out using Stata v12.1 (StataCorp LP, College Station, USA).
Ethical approval
The Committee on Human Research, Publications and Ethics, School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana approved the study design and the informed consent procedure. Participants were recruited to the study after the aims of the study and the risks and benefits were explained and the informed consent form was signed by their caregiver.
Results
Study participants in the hospital survey
In total, 2230 children from the catchment area attended the OPD at SMH 2594 times during the study period. The vast majority of children visited the hospital once (1942; 74.9 %) or twice (257; 9.9 %) with a maximum of five visits per individual. To exclude counting a single infection twice, all children returning ≤28 days after a previous visit were excluded from the analysis. The analysis presented here includes 2203 (84.9 %) of the visits, made by 1907 children who lived in 26 communities (≥20 observations per community) within the catchment area. A total of 1023 (46.5 %) visits were made by females and the mean age was 3.3 years (SD: ±3.2). The mothers of 1769 cases (81.9 %) stated that their child had slept under an ITN in the previous night. Table 2 summarizes the characteristics of the cases and gives an overview on the variation by community.
Malaria cases
During the study period, a total of 708 malaria episodes in 660 children were observed, corresponding to 32.1 % of all hospital visits. Most children (n = 620; 87.6 %) had only one malaria episode, while one child presented with malaria four times during the study period. Patients with malaria had a mean age of 3.9 years (SD: ±3.1) compared to 3 years (SD: ±3.1) in children without malaria.
Community characteristics and urbanicity scale
Of the 26 communities included in this analysis, 20 were located in the Bosomtwe District and six were suburbs within the Kumasi Metropolitan Area. The population size of these communities ranged from 650 to 65,225 inhabitants, with a median size of 3195 (IQR: 1288–7474). The number of patients that attended SMH per study-community ranged from 21 to 369 and the median number of patients per study-community was 146 (IQR: 61–289).
The minimum score of a study-community on the urbanicity scale was 13.75 and the maximum was 77.5 points, with a median of 41 (IQR: 27–65.25) points. Validation of the scale showed good unidimensionality (eigenvalue of the first factor: 6.06 with 96.6 % of the overall variance explained), good sampling adequacy (Kaiser–Meyer–Olkin measure of 0.93 for the first factor) and a high internal consistency (Cronbach’s alpha of 0.96). The urbanicity characteristics of the study-communities and details on the scale validation are presented in the Additional files 1 and 2.
Association between urbanicity and malaria
Overall, the MPF varied strongly between the communities with the highest MPF of 54.5 % in Aduaden, a small rural community in Bosumtwe District scoring 23.25 points on the urbanicity scale, and the lowest MPF of 12.5 % in Kaase, a suburb of Kumasi with 68.5 points on the urbanicity scale. Increasing urbanicity was strongly associated with a linear decrease in the MPF (R2 = 0.70) in the univariate linear regression model. For every ten points increase on the urbanicity scale the MPF decreased by 5 % (95 % confidence interval [95 % CI]: 4–6 %, p < 0.001), corresponding to a modelled MPF-decrease from 52 to 20 % over the measured range of the urbanicity scale (Table 3; Fig. 2).
Association between urbanicity and MPF. The Figure illustrates a linear decrease of MPF with increasing levels of urbanicity. The linear regression models a 5 % decrease per ten-point increase on the urbanicity scale (95 % CI: 4–6 %, R2 = 0.70, p < 0.001). Data points are scaled proportional to the number of individuals contributing to the measurement of MPF
The use of ITNs was high in the study group with a proportion of 82 % (1769 of 2203 visits) of the mothers stating that their child had slept under an ITN the night before the hospital visit. This proportion varied from 68 % in Esereso to 100 % in Oyoko and there was no evidence for an association with the level of urbanicity (1 % decrease in ITN use per 10 % increase in urbanicity score, 95 % CI: −3–0.1 %, p = 0.07). Higher use of ITNs in the study group was associated with an increase in MPF [6 % increase in MPF per 10 % increase in ITN use (95 % CI: 1–11 %, p = 0.02)].
In the multivariate model for association between MPF and urbanicity, adjusted for ITN use, the explained variance hardly changed (R2 = 0.70) and the association between urbanicity and MPF was only slightly lower with a 4.6 % (95 % CI: 3–6 %, p < 0.001) decrease in MPF for each ten-point increase in urbanicity (Table 3).
Malaria, urbanicity and acquisition of immunity
The mean age at presentation for patients with malaria varied strongly between communities, from 26 months in Aduadaden (23.25 points on the urbanicity scale) in Bosumtwe District to 68 months in Chirapatre (69.5 points on the urbanicity scale), a suburb of Kumasi. There was strong evidence for an association between urbanicity and mean age of malaria patients (R2 0.27; p = 0.004) with an increase of 2.9 months (95 % CI: 1.0–4.8) per ten-point increase on the urbanicity scale (Table 3; Fig. 3a).
Association between urbanicity and age, and MPF and age. The Figure illustrates an association between urbanicity and the mean age of malaria patients in months (a R2 0.27; p = 0.004), while there is no association between urbanicity and mean age of all patients (b R2 = 0.03; p = 0.21). In addition, there is an association between MPF and mean age of malaria patients (c R2 = 0.27; p = 0.004) and no association between MPF and mean age of all patients (d R2 = 0.08; p = 0.09). Data points are scaled proportional to the number of individuals contributing to the measurement of mean age
There was also strong evidence for a linear association between the mean age of malaria patients and community MPF (R2 0.27; p = 0.004) with a modelled decrease of 4.9 months (95 % CI: 1.7–8.1) in the mean age per 10 % increase in MPF (Table 3; Fig. 3c). ITN use was also associated with mean age of malaria patients with a modelled decrease in mean age of 5.3 months per 10 % increase in ITN use (95 % CI: 0.8–9.7, p = 0.02). Adjusting the estimates for ITN use in multivariate models reduced both the association between mean age of malaria patients and urbanicity (2.3-month increase per ten points, 95 % CI: 0.2–4.4, p = 0.03) and mean age and MPF (3.9-month decrease per 10 %, 95 % CI: 0.2–7.4, p = 0.04).
The mean age at presentation for all patients also varied strongly between communities, from 28 months in Aduadaden (23.25 points on the urbanicity scale) in Bosumtwe District to 58 months in Gyinyase (72.5 points on the urbanicity scale), a suburb of Kumasi. However, there was no association with urbanicity (β = 0.007; R2 = 0.03; p = 0.21, Fig. 3b), or MPF (β = −1.1; R2 = 0.08; p = 0.09, Fig. 3d).
Single score-components and MPF
The bivariate models showed that all components correlate negatively with MPF (Table 4), while the strongest associations were observed for population size (coefficient −0.04, R2 0.59), economic activity (coefficient −0.04, R2 0.57), education (coefficient −0.04, R2 0.52), and housing (coefficient −0.04, R2 0.65). In the multivariate model no variable remained associated with MPF, but R2 squared increased to 0.77. The model showed the strong co-linearity between components, which was also seen in the exploratory factor analysis performed to validate the score (see Additional file 1).
Discussion
Using data from a hospital-based study, an ecological analysis of the association between urbanicity and clinical malaria episodes was performed. Using MPF as outcome and a continuous measure of urbanicity as exposure, a linear decrease of 5 % in MPF with every ten-point increase in urbanicity was identified. In addition, it was found that the mean age of malaria patients increased by 2.9 months with every ten-point increase on the urbanicity scale, indicating a potential influence of urbanicity on the acquisition of semi-immunity against malaria. This is supported by the finding of a lower mean age of malaria patients in communities with a higher MPF.
Through the use of a continuous scale of urbanicity that provides more detailed information than a binary classification, it was possible to assess linear associations with the covariates. The vast majority of previous studies [3, 5, 8, 9, 20, 21] used a crude rural–urban dichotomy that is more arbitrary and cannot distinguish localities and cities on a continuum of urbanicity. In contrast to these studies, this continuous scale is based on standardized methods of scale construction [17] that have been applied and validated to measure urbanicity in different settings [22–24].
The results confirm heterogeneity of malaria prevalence in areas of high endemicity as previously reported [10] and underpin the postulated association between urbanization and the decreasing incidence of malaria. The most detailed study on the effect of urbanization on malaria was conducted in the Republic of Congo between 1982 and 1984 and found high spatial variation of malaria prevalence in Brazzaville [8, 25, 26]. Water bodies in urban areas were scarce or polluted and thus unfavourable as breeding sites for mosquitoes. The authors also found that the flight range of mosquitoes was reduced from several kilometres in rural areas to a few 100 m in urban areas [8], probably due to higher human population density. Data from the city of Dakar showed highly focused malaria transmission and a decreasing malaria risk in urbanized areas [27, 28]. More recently, a study from Ouagadougou showed a decreasing risk of malaria from the periphery of the city towards the urban centre and identified urban agriculture and residence near mosquito breeding sites as risk factors for urban malaria [20]. The relationship between urbanicity and malaria transmission has been modelled on a global scale in several studies. These models found a pattern of decreasing malaria transmission coinciding with increased urbanization [3, 5, 9]. Furthermore, in a meta-analysis of entomological inoculation rate (EIR) surveys, lower EIRs in urban or peri-urban areas compared to rural areas were found [21]. The decline in transmission in urban areas is best explained by a rise in socio-economic status, housing quality and access to infrastructure, sanitation and education, as well as a higher use of prevention methods (e.g., ITNs) and access to healthcare [29, 30]. In the study presented here, the strongest associations between MPF and single components of the score were observed for population size, economic activity, education, and housing. However, the observed unidimensionality of the score components supports the approach to combine the components into one measure of urbanicity rather than assessing component’s associations with MPF.
The use of ITNs in the current study was not significantly associated with urbanicity, but surprisingly associated with a higher MPF. However, the analysis was performed on an ecological level and individual risk was not assessed. Therefore, ITN use may have been higher in communities with a high MPF as a response to higher transmission there. The reported use of ITNs was also higher than in previous studies where 22 % of children below the age of five slept under a bed net in 2006 [31]. This difference is possibly due to a recent upscaling in ITN distribution [32] or a result of a possible interviewer bias.
The findings of varying mean ages of malaria patients over short distances and a correlation of mean age with urbanicity and MPF indicate that the acquisition of immunity is spatially heterogeneous and possibly slower in urban areas. The association between prevalence of malaria and the acquisition of immunity is well known and has been studied on a macro-epidemiological scale and in modelling approaches [12, 33, 34]. A recent meta-analysis found that clinical malaria is experienced at all ages, but the age of severe symptoms is inversely associated with transmission intensity [35]. However, data on heterogeneity in immunity on a micro-epidemiological level are scarce and there are few studies on the effect of urbanicity. An early, cross-sectional study from southern Ghana found a markedly lower prevalence of antibodies against P. falciparum in an urban setting compared to a rural area [36]. However, antibody responses to malaria are not necessarily correlated to immunity and may just be markers of a higher exposure in rural areas. Several studies have looked at the mean age of malaria patients in regions or countries of low and high transmission intensity [37, 38] and as a change over time with decreasing malaria incidence [39]. All these studies consistently found a lower mean age of malaria in higher transmission settings. However, to the authors’ knowledge the only study that looked at varying age of infection over short distances is a recent ecological analysis from Kenya that also found a correlation between MPF and mean age of infection [40].
A difference in the age of infection between urban and rural areas and a possible delay in the acquisition of immunity has several implications for clinicians and intervention programmes. First, severe disease in urban areas may be more evenly distributed across childhood [41] and clinicians should also consider malaria as a cause of severe febrile illness in older children. Second, intervention programmes focusing on infants may not be accurately targeted in the future even if the brunt of malaria deaths is still borne by the youngest children today [35]. Third, delayed and potentially waning immunity may lead to populations susceptible to severe disease and potentially to epidemics of severe malaria.
While these findings could have major implications, the data should be interpreted with care. First, MPF is a measure of disease prevalence in patients attending the hospital and not a direct measure in the community. Calculating malaria prevalence/incidence based on data from healthcare facilities is biased by access to care and unknown hospital coverage. By using the MPF among children with fever, as previously done in several studies [40, 42], the measure of prevalence is not biased by access to care. MPF, as a measure within the population attending the hospital, would only be influenced by healthcare-seeking behaviour if it is different between malaria cases and fever cases with other causes (e.g., if mothers took children with malaria to private clinics and attended the hospital with other infections). As malaria is clinically indistinguishable from other febrile infections, such an effect is unlikely to have biased the results. However, it is impossible to know whether the families attending the hospital are representative of the communities that they come from and the findings may therefore not be transferable. Second, MPF was calculated based on all cases of malaria presenting to an OPD and did not stratify for degrees of disease severity. The pattern of association between MPF and urbanicity might vary by disease severity [35] and further studies are needed to study this in detail. Third, malaria infection may have been acquired while travelling outside residential areas and therefore falsely attributed to the community of residence in this analysis. However, this limitation is less likely for children and the main vector in the area, Anopheles gambiae is known to be mainly endophilic [43]. Fourth, as immunity is influenced by changes in urbanicity, which is an ongoing process, the population immunity may not be at equilibrium with the environment. However, as the data presented here are from children with a mean age of 3.3 years, changes in urbanicity over such a short period are unlikely to be large enough to have a strong effect on the effects seen here. Finally, this is a cross-sectional study and the data were analysed on an ecological level, making causal inferences difficult.
The results demonstrate the feasibility of hospital-based studies to analyse crude associations in the micro-epidemiology of malaria and acquired immunity. However, further studies including clinical data on disease severity, especially cerebral malaria, and analyses on an individual level are needed. Future studies should also include additional risk factors such as surrounding breeding sites. Such studies will lead to a better understanding of the heterogeneity of both transmission and immunity and provide data for geographically targeted interventions.
References
Gething PW, Patil AP, Smith DL, Guerra CA, Elyazar IRF, Johnston GL, et al. A new world malaria map: Plasmodium falciparum endemicity in 2010. Malar J. 2011;10:378.
WHO. World Malaria Report 2013. Geneva: World Health Organization; 2013.
Tatem AJ, Gething PW, Smith DL, Hay SI. Urbanization and the global malaria recession. Malar J. 2013;12:133.
WHO. World Health Statistics 2012. Geneva: World Health Organization; 2012.
Tatem AJ, Guerra CA, Kabaria CW, Noor AM, Hay SI. Human population, urban settlement patterns and their impact on Plasmodium falciparum malaria endemicity. Malar J. 2008;7:218.
UN. World urbanization prospects—the 2011 Revision. New York: 2011.
Donnelly MJ, McCall P, Lengeler C, Bates I, D’Alessandro U, Barnish G, et al. Malaria and urbanization in sub-Saharan Africa. Malar J. 2005;4:12.
Trape J-F, Zoulani A. Malaria and urbanization in central Africa: the example of Brazzaville Part III: relationships between urbanization and the intensity of malaria transmission. Trans R Soc Trop Med Hyg. 1987;81:19–25.
Hay SI, Guerra CA, Tatem AJ, Atkinson PM, Snow RW. Urbanization, malaria transmission and disease burden in Africa. Nat Rev Microbiol. 2005;3:81–90.
Kreuels B, Kobbe R, Adjei S, Kreuzberg C, Von Reden C, Bater K, et al. Spatial variation of malaria incidence in young children from a geographically homogeneous area with high endemicity. J Infect Dis. 2008;197:85–93.
Bousema T, Drakeley C, Gesase S, Hashim R, Magesa S, Mosha F, et al. Identification of hot spots of malaria transmission for targeted malaria control. J Infect Dis. 2010;201:1764–74.
Reyburn H, Mbatia R, Drakeley C, Bruce J, Carneiro I, Olomi R, et al. Association of transmission intensity and age with clinical manifestations and case fatality of severe Plasmodium falciparum malaria. JAMA. 2005;293:1461–70.
Greenwood B. The microepidemiology of malaria and its importance to malaria control. Trans R Soc Trop Med Hyg. 1989;83:25–9.
Snow RW, Omumbo JA, Lowe B, Molyneux CS, Obiero JO, Palmer A, et al. Relation between severe malaria morbidity in children and level of Plasmodium falciparum transmission in Africa. Lancet. 1997;349:1650–4.
Ministry of local government and rural development G. Ghana districts–Bosomtwe district [Internet]. 2006 [cited 2013 Sep 3]. Available from: http://www.ghanadistricts.com/districts/?r=2&_=20&sa=4555.
Ghana Statistical Service. GSS Population & Housing Census. 2010.
DeVellis RF. Scale development: theory and aplications. 2nd ed. vol 26. Thousand Oaks: Sage Publications Inc.; 2003.
Netemeyer RG, Bearden WO, Sharma S. Scaling procedures—issues and applications. Tousand Oaks: Sage Publications Inc; 2003.
Van Eijk AM, Hill J, Larsen DA, Webster J, Steketee RW, Eisele TP, et al. Coverage of intermittent preventive treatment and insecticide-treated nets for the control of malaria during pregnancy in sub-Saharan Africa: a synthesis and meta-analysis of national survey data, 2009-11. Lancet Infect Dis. 2013;13:1029–42.
Wang S-J, Lengeler C, Smith TA, Vounatsou P, Diadie DA, Pritroipa X, et al. Rapid urban malaria appraisal (RUMA) I: epidemiology of urban malaria in Ouagadougou. Malar J. 2005;4:43.
Robert V, Macintyre K, Keating J, Trape J-F, Duchemin J-B, Warren M, et al. Malaria transmission in urban sub-Saharan Africa. Am J Trop Med Hyg. 2003;68:169–76.
Dahly DL, Adair LS. Quantifying the urban environment: a scale measure of urbanicity outperforms the urban-rural dichotomy. Soc Sci Med. 2007;64:1407–19.
Jones-Smith JC, Popkin BM. Understanding community context and adult health changes in China: development of an urbanicity scale. Soc Sci Med. 2010;71:1436–46.
Novak NL, Allender S, Scarborough P, West D. The development and validation of an urbanicity scale in a multi-country study. BMC Public Health. 2012;12:530.
Trape J-F, Zoulani A. Malaria and urbanization in central Africa: the example of Brazzaville. Part II: results of entomological surveys and epidemiological analysis. Trans R Soc Trop Med Hyg. 1987;81:10–8.
Trape J-F. Malaria and urbanization in central Africa the example of Brazzaville Part IV: parasitological and serological surveys in urban and surrounding areas. Trans R Soc Trop Med Hyg. 1987;81:26–33.
Machault V, Vignolles C, Pagès F, Gadiaga L, Gaye A, Sokhna C, et al. Spatial heterogeneity and temporal evolution of malaria transmission risk in Dakar, Senegal, according to remotely sensed environmental data. Malar J. 2010;9:252.
Machault V, Vignolles C, Pagès F, Gadiaga L, Tourre YM, Gaye A, et al. Risk mapping of Anopheles gambiae s.l. densities using remotely-sensed environmental and meteorological data in an urban area: Dakar, Senegal. PLoS One. 2012;7:e50674.
De Silva PM, Marshall JM. Factors contributing to urban malaria transmission in sub-saharan Africa: a systematic review. J Trop Med. 2012;2012:819563.
Fobil JN, Kraemer A, Meyer CG, May J. Neighborhood urban environmental quality conditions are likely to drive malaria and diarrhea mortality in Accra, Ghana. J Environ Public Health. 2011;2011:484010.
Noor AM, Mutheu JJ, Tatem AJ, Hay SI, Snow RW. Insecticide-treated net coverage in Africa: mapping progress in 2000-07. Lancet. 2009;373:58–67.
Ghana Health Service. Expanded programme on immunization report. 2008.
Ghani AC, Sutherland CJ, Riley EM, Drakeley CJ, Griffin JT, Roly D, et al. Loss of population levels of immunity to malaria as a result of exposure-reducing interventions: consequences for interpretation of disease trends. PLoS One. 2009;4:e4383.
Bandeiras C, Trovoada MJ, Gonçalves LA, Marinho CR, Turner L, Hviid L, et al. Modeling malaria infection and immunity against variant surface antigens in Príncipe Island, West Africa. PLoS One. 2014;9:e88110.
Carneiro I, Roca-Feltrer A, Griffin JT, Smith L, Tanner M, Schellenberg A, et al. Age-patterns of malaria vary with severity, transmission intensity and seasonality in sub-Saharan Africa: a systematic review and pooled analysis. PLoS One. 2010;5:e8988.
Gardiner C, Biggar RJ, Collins WE, Nkrumah FK. Malaria in urban and rural areas of southern Ghana: a survey of parasitaemia, antibodies, and antimalarial practices. Bull World Health Organ. 1984;62:607–13.
Okiro EA, Al-Taiar A, Reyburn H, Idro R, Berkley JA, Snow RW. Age patterns of severe paediatric malaria and their relationship to Plasmodium falciparum transmission intensity. Malar J. 2009;8:4.
Roca-Feltrer A, Carneiro I, Smith L, Schellenberg JRA, Greenwood B, Schellenberg D. The age patterns of severe malaria syndromes in sub-Saharan Africa across a range of transmission intensities and seasonality settings. Malar J. 2010;9:282.
Meara WPO, Mwangi TW, Williams TN, Mckenzie FE, Robert W, Marsh K. Relationship between exposure, clinical malaria, and age in an area of changing transmission intensity. Am J Trop Med Hyg. 2008;79:185–91.
Bejon P, Williams TN, Nyundo C, Hay SI, Benz D, Gething PW, et al. A micro-epidemiological analysis of febrile malaria in Coastal Kenya showing hotspots within hotspots. Elife. 2014;3:e02130.
Snow RW, Marsh K. The consequences of reducing transmission of Plasmodium falciparum in Africa. Adv Parasitol. 2002;52:235–64.
Jensen TP, Bukirwa H, Njama-Meya D, Francis D, Kamya MR, Rosenthal PJ, et al. Use of the slide positivity rate to estimate changes in malaria incidence in a cohort of Ugandan children. Malar J. 2009;8:213.
Seyoum A, Sikaala C, Bayoh N, Huho B, Brie O, Killeen G. Consistently high estimates for the proportion of human exposure to malaria vector populations occurring indoors in rural Africa. Int J Epidemiol. 2013;42:235–47.
Authors’ contributions
CF collected the data, performed data analysis and wrote the manuscript. RK performed data analysis. NS, PS, GF, and JF collected the data and conducted the study procedures. LE performed geographic analysis and assisted in the development of the figures. EOD, YAS, FM, RRS, and JM gave input to the design of the study, the data analysis and the writing of the manuscript. BK designed the study, analysed the data and wrote the manuscript. All authors gave substantial input to the writing of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank all participants and their guardians for participating in the study. This work was supported by the German Centre for Infection Research (Deutsches Zentrum für Infektionsforschung, DZIF) through a Clinical Leave Stipend to BK (Grant Number: TI 07.001). This work is part of Ph.D. thesis of CF.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Frank, C., Krumkamp, R., Sarpong, N. et al. Spatial heterogeneity of malaria in Ghana: a cross-sectional study on the association between urbanicity and the acquisition of immunity. Malar J 15, 84 (2016). https://doi.org/10.1186/s12936-016-1138-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-016-1138-4