Abstract
Background
Intermittent preventive treatment (IPT) is a proven malaria control strategy in infants and pregnancy. School-aged children represent 26 % of the African population, and an increasing percentage of them are scholarized. Malaria is causing 50 % of deaths in this age group and malaria control efforts may shift the malaria burden to older age groups. Schools have been suggested as a platform for health interventions delivery (deworming, iron-folic acid, nutrients supplementation, (boost-)immunization) and as a possible delivery system for IPT in schoolchildren (IPTsc). However, the current evidence on the efficacy and safety of IPTsc is limited and the optimal therapeutic regimen remains controversial.
Methods
A systematic search for studies reporting efficacy and safety of IPT in schoolchildren was conducted using PubMed, Web of Science, Clinicaltrials and WHO/ICTRP database, and abstracts from congresses with the following key words: intermittent, preventive treatment AND malaria OR Plasmodium falciparum AND schoolchildren NOT infant NOT pregnancy.
Results
Five studies were identified. Most IPTsc regimes demonstrated substantial protection against malaria parasitaemia, with dihydroartemisinin-piperaquine (DP) given monthly having the highest protective effect (PE) (94 %; 95 % CI 93–96). Contrarily, SP did not provide any PE against parasitaemia. However, no IPT regimen provided a PE above 50 % in regard to anaemia, and highest protection was provided by SP+ amodiaquine (AQ) given four-monthly (50 %; 95 % CI 41–53). The best protection against clinical malaria was observed in children monthly treated with DP (97 %; 95 % CI 87–98). However, there was no protection when the drug was given three-monthly. No severe adverse events were associated with the drugs used for IPTsc.
Conclusion
IPTsc may reduce the malaria-related burden in schoolchildren. However, more studies assessing efficacy of IPT in particular against malaria-related anaemia and clinical malaria in schoolchildren must be conducted.
Similar content being viewed by others
Background
Malaria is a major public health problem in sub-Saharan Africa (SSA), with 90 % of the burden occurring in African children [1–3]. To date, development and implementation of interventions for malaria prevention and control have been mainly directed towards well-known risk groups, such as pregnant women and children younger than 5 years old [4]. However, the impact of health factors on educational outcomes for schoolchildren is widely recognized, including by governments [5]. Previous research on the effect of malaria on children’s education showed that malaria is the leading cause of school absenteeism [6, 7] and asymptomatic malaria was likely to affect school performance [8]. In addition, malaria remains the biggest killer among school-aged children, causing 50 % of deaths in this age group in sub-Saharan Africa [9]. School-aged children represent 26 % of the African population, and an increasing percentage of them are scholarized. Since 2000, school enrolment increased by 52 % in sub-Saharan Africa [10]. Moreover, studies suggest that increasing control efforts and subsequent decline of the malaria burden as well as further progress towards malaria elimination will lead to a shift of at-risk population from under-five to older children groups, to which schoolchildren belong [11, 12]. Little research assesses adapted intervention tools for this vulnerable target group. Effective control measures could indeed reduce the burden of malaria in school-aged children. Sleeping under insecticide-treated nets can reduce overall child mortality [13]. Unfortunately, schoolchildren seem to be less likely to sleep under a bed net than those under-5 years old [14]. Active screening and treatment is another strategy under investigation. This approach may raise the question of the appropriate test to track asymptomatic malaria, since the latter is generally associated with relatively low parasite density [15]. Intermittent preventive treatment (IPT) may be another promising therapeutic strategy to prevent malaria and its related adverse outcomes in school-aged children [16]. This strategy has largely been studied in groups bearing the highest burden of the disease. In infants (IPTi), children younger than 5 years (IPTc) and pregnant women (IPTp), IPT schemes have been demonstrated to be protective against malaria and its related adverse outcomes [17–21]. However, only a handful of studies have focused on the potential benefits of IPT on school-aged children’s health (IPTsc). This review summarizes published results of this subject and it presents efficacy and safety data for all available therapeutic regimes in order to produce more information on their impact on asymptomatic and symptomatic parasitaemia, and haemoglobin concentration.
Methods
Search strategy and selection criteria
A single investigator (JMR) developed and conducted a systematic literature search for published IPTsc studies, on 28 April, 2014. Studies were identified using PubMed, Web of Science, Clinicaltrials [Clinicaltrials.gov and World Health Organization international clinical trials registry platform (WHO ICTRP) database] and abstracts from congresses. Combinations of the following search terms were used: intermittent, preventive treatment AND malaria OR Plasmodium falciparum AND schoolchildren NOT infant NOT pregnancy. Study eligibility was assessed in an unblinded manner. Studies had to be published articles written in English. Inclusion criteria were determined following the PICO format: (P) Participants: children of school age, resident in a malaria-endemic area; (I) Interventions: clinical trials evaluating the efficacy and safety of IPT; (C) Comparisons: the efficacy of available drug regimes compared to each other or with placebo; (O) Outcomes: the proportion of children with parasitaemia, anaemia and clinical malaria to provide the effect estimates (or sufficient data for calculation of an effect estimate), relative risk (RR), protective effect (PE), and their corresponding 95 % confidence interval (CI). If a selected study included more than one comparator or drug regimen, each comparison was regarded as a separate study. Studies which enrolled children younger than 5 years were included if data on children over 5 years were available for analysis. Studies evaluating chemoprophylaxis, screening and prompt treatment, as well as study protocol, were excluded.
Data extraction
All the titles and abstracts were collected through the electronic search and filtered for potentially eligible articles. For each study, the following information was extracted: first author, publication year, year of study start and end, study design, randomization procedures, inclusion criteria, insecticide-treated net or bed-net use, local malaria transmission details of study groups, number of enrolled children, outcomes assessed and adverse events. Data from eligible studies were extracted based on the intention to-treat principle into a purpose-built database (Excel, Microsoft, 2010). This review follows the PRISMA guidelines [22].
Results
Study characteristics
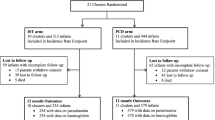
A total of five trials assessing the efficacy of IPT for preventing asymptomatic and clinical malaria and anaemia in school-aged children were identified and included for analysis (Fig. 1) [23–27]. The trials were undertaken in Bondo in Kenya, in Kambila in Mali, Kollé in Mali, and in Tororo in Uganda. Malaria transmission patterns ranged from seasonal in the Malian sites over perennial with seasonal peaks in Kenya to hyperendemic in Tororo, Uganda. Usage of bed nets was low (<5–35.4 %) in all trials. All trials were randomized and placebo controlled, except for Kimbila (Mali), which was randomized and controlled. Two were double blinded, two open and one single blinded. Block randomization by individual was done in all trials except for Bondo (Kenya), which was cluster-randomized by schools.
IPT schedules differed between trials and were given every 5 months, four-monthly, three-monthly, bimonthly, monthly, or only at baseline (Table 1). All five trials had received ethics approval. The efficacy and safety of sulfadoxine-pyrimethamine (SP) was assessed in four trials: alone [23, 26], combined with amodiaquine (SP + AQ) [24], or with artesunate (SP + AS) [25]. Other combinations used were AQ + AS [25]. Dihydroartemisinin-piperaquine (DP) monotherapy was used in two trials in different schedules: at baseline, monthly and trimonthly [26, 27]. Safety and efficacy were assessed by passive and active clinical surveillance in all trials. The primary endpoint was the incidence of clinical malaria in three trials [23, 25, 27]. One trial’s primary endpoint was the risk of asymptomatic parasitaemia at 42 days [26] and the trial conducted in Bondo (Kenya) had the prevalence of anaemia as primary endpoint. However, three trials assessed the prevalence of anaemia or the increase in haemoglobin concentration as secondary endpoint [25–27]. The study duration differed between trials. Three trials evaluated the efficacy and safety of IPTsc on the basis of a 12 months’ follow-up [23, 24, 27], whereas in the remaining trials the follow-up period was of 5 months [25] and 42 days [26]. Thick blood films were stained and read by use of standard procedures for malaria parasite detection in all trials. Parasite density was calculated on the assumption of a mean of 8000 leucocytes/µL in two trials, or a mean of 7500 leucocytes/µl in Kambila (Mali) trial, whereas two trials did not specify the number of leucocytes for the parasite density calculation. The haemoglobin concentration was measured with a Hemocue® photometer in all trials. Data on anaemia were reported in three of them [24, 25, 27]. Anaemia was defined as haemoglobin <11.0 g/dL [24, 25] and haemoglobin <11.5 g/dL for children aged 6–11 years and <12.0 g/dL for those aged 12–14 years [27]. The frequency and timing of outcome measurement varied greatly between studies. Malaria parasitaemia was assessed on days 7, 14, 28, and 42 [26] and monthly [25, 27]. The haemoglobin level was measure on day 42 [26], 6 weeks after the last treatment [24], every 3 and 5 months [27] and monthly [25]. Monitoring for clinical malaria was by active case detection [27], by active weekly follow-up visits and passive follow-up [23] and active monthly follow-up visits and passive follow-up [25].
Efficacy of IPTsc on malaria parasitaemia
IPT with SP combined with AS and AQ + AS reduced significantly the risk of malaria parasitaemia. The prevalence of parasitaemia by treatment group was 6.6, 6.2 and 34.4 % for SP + AS, AQ + AS and vitamin C, respectively (P < 0.001) [25]. The risk of parasitaemia in DP and AQ + SP groups (11.7 and 44.3 %, respectively) was significantly lower than in those receiving SP (79.7 %) (risk difference AQ + SP vs placebo: 68.0 %; 95 % CI 60.6–75.4, p < 0.001; DP vs placebo: 35.4 %; 95 % CI 26.3–44.5, p < 0.001), and SP vs placebo: −4.9 %; 95 % CI −12.6 to 2.9, p = 0.2). DP was superior to AQ + SP (risk difference 32.6 (95 % CI 24.3–40.9); p < 0.001) [26]. SP plus AQ administered four-monthly reduced the prevalence of parasitaemia (SP + AQ: 4.6 %; 95 % CI 0.8–14.1) vs placebo: 39.7 %; 95 % CI 26.2–58.1 %, p < 0.0001) in Bondo, Kenya. The prevalence of parasitaemia was 2 % in DP monthly arm, 18 % in DP three-monthly and 38 % in control arm, in Uganda, 2014. The IPTsc with SP monotherapy in Tororo, Uganda did not demonstrate any PE against parasitaemia (0.05 %; 95 % CI −4 to 14). The PE of SP + AQ administered four-monthly was 88 % (95 % CI 86–90) in Bondo, Kenya, but this drug regimen demonstrated a lower PE (49 %; 95 % CI 38–56) in Tororo, Uganda. SP + AS and AQ + AS administered in Mali demonstrated similar PE (81 % (95 % CI 56–92) and 81 % (95 % CI 57–91), respectively. The PE of DP in Tororo in 2010 was 86 % (95 % CI 80–91) after 42 days’ follow-up. In 2014 the PE of DP given monthly in Tororo was the highest (94 %; 95 % CI 93–96), but this same drug regimen administered three-monthly in Tororo in 2014 had a significantly lower PE of 54 % (95 % CI 49–58) (Fig. 2; Table 2).
Effect of IPTsc on malaria parasitaemia during the intervention period. RR rate ratio, SP sulfadoxine-pyrimethamine, SP + AQ sulfadoxine-pyrimethamine plus amodiaquine, SP + AS sulfadoxine-pyrimethamine plus artesunate, AQ + AS amodiaquine plus artesunate, DP dihydroartemisinin-piperaquine, CI confidence interval
Efficacy of IPTsc on anaemia
Children treated with IPT were significantly less likely to be anaemic (SP + AS, 17.7 %; AQ + AS, 16.0 %; vitamin C, 29.6 %; P = 0.039) in Kollé, Mali. In Tororo, Uganda (2014), the prevalence of anaemia was significantly lower in the DP given monthly arm (12 %) but not the DP given three-monthly arm (17 %), compared with the placebo arm (20 %). SP + AQ (given four-monthly) reduced significantly the risk of anaemia (6.3 %), in Bondo, Kenya (SP + AQ: 6.3 % vs placebo: 12.6 %; p = 0.041). The PE effect of IPTsc on anaemia was generally lower in all trials that assessed this endpoint, and ranged from 14 to 50 %. SP + AQ (given three-monthly), SP + AS, AQ + AS and DP (administered monthly) demonstrated similar PE of IPTsc against anaemia in schoolchildren. The PE effect of DP given three monthly was the lowest (14 %; 95 % CI 2–23) (Table 3). The change in mean haemoglobin level did not differ between children who received SP + AS and AQ + AS, compared to those receiving placebo in Kollé, Mali. In Tororo as well, SP in 2010 and DP given three-monthly in 2014 did not increase the mean haemoglobin level compared to placebo. However, in the same trials held in Tororo, IPTsc with DP and SP + AQ (in 2010) increased the mean haemoglobin level (mean difference: 0.37 g/dL (95 % CI 0.18, 0.56) and 0.34 g/dL (95 % CI 0.15, 0.53), respectively) compared to baseline. Similarly, DP given monthly (in 2014) significantly increased the mean haemoglobin level compared to placebo group (1.20 vs 0.79 g/dL; P = 0.003). A high mean haemoglobin level was also observed in children treated with SP + AQ compared to those in placebo group (mean difference: 5.62 g/L (95 % CI 2.19–9.05) in Bondo, Kenya (Fig. 3).
Effect of IPTsc on anaemia during the intervention period. RR rate ratio, SP sulfadoxine-pyrimethamine, SP + AQ sulfadoxine-pyrimethamine plus amodiaquine, SP + AS sulfadoxine-pyrimethamine plus artesunate, AQ + AS amodiaquine plus artesunate, DP dihydroartemisinin-piperaquine, CI confidence interval
Efficacy of ITPsc on clinical malaria
The PE of IPTsc with SP given bimonthly against clinical malaria was 40.1 % (95 % CI 17.9–56.4) in Kambila, Mali. The PE of SP + AS in Mali was 67 % (95 % CI: 42–98). In the trial conducted in Kollé, Mali, AQ + AS had a PE of 47 % (95 % CI 32–67). In 2014 DP given monthly in Tororo had the highest PE (97 %; 95 % CI 87–98), however, this same drug regimen administered three- to five-monthly in Tororo in 2014 had a no PE (Fig. 4; Table 4).
Safety outcome
Seven deaths occurred in the trial conducted in Bondo, Kenya, two in the IPT group and five in the placebo group. Cause of death could not be reliably ascertained in all cases. Twenty-three drug-related severe adverse events were observed during this study. Of these 23 adverse events, 19 occurred in the IPTsc goup (SP + AQ three-monthly) and four in the placebo group. The most commonly severe adverse events were: problems of balance, dizziness, feeling faint, nausea, or vomiting. One severe skin reaction was reported in the placebo group. In the study conducted in Tororo, Uganda, 2014, one death occurred in the IPT intervention group (DP three-monthly) due to acute lymphoblastic leukaemia. Fourteen severe adverse events were observed, but were judged unlikely to be associated with treatment. In almost all trials, mild or moderate adverse events were frequent in IPT group compared to placebo group. However, in the study conducted in Tororo (2014), mild or moderate adverse events including: fever, headache, nausea and vomiting were commonly associated with malaria, and were more frequent in placebo group than in the intervention arms. SP + AQ was significantly associated with vomiting in Tororo, 2010, and AQ + AS had the highest rate of headache in Kollé (Table 5).
Discussion
The aim of this review was to provide an overview of the effectiveness of IPT to prevent parasitaemia, clinical malaria and malaria-related anaemia in older children and to find out the most promising drug regimen for IPT in this specific population. The most appropriate drug regimen for IPTsc should provide protection against malaria-related anaemia and asymptomatic malaria parasitaemia, as these are the main features of malaria in this specific population. In this review, the studies used a wide variety of IPT regimes incorporating different drugs, dosages, timings, and numbers of IPT rounds.
The PE of IPT against malaria parasitaemia ranged from 49 to 94 % in the trials that assessed this endpoint. The highest PE was observed using DP monthly. SP + AQ given four-monthly, also demonstrated a high PE. SP monotherapy provided the lowest PE against malaria parasitaemia. This low efficacy of SP is not surprising and highlights the wide spread of resistance to this drug across Africa. The prevalence of 540E, one of the key SP resistance mediators, was found to be less than 50 % in Mali, whereas high prevalence of this marker (above 50 %) was observed in Uganda and Kenya [28]. This is in agreement with other findings from trials conducted in children younger than 5 years [29]. DP given monthly in Tororo, 2014, showed the highest PE against clinical malaria, but this drug given three-monthly did not show any PE against clinical malaria. These results are consistent with the theory stipulating that IPT protects by providing a period of post-treatment prophylaxis and that the length of this period of protection is determined by the pharmacodynamics of the drugs used [30].
The protective effect of IPTsc against malaria-related anaemia was relatively low in most trials that assessed this endpoint. DP given three- to five-monthly had the lowest PE against anaemia while DP given three- to five-monthly, or SP + AS and AQ + AS did not demonstrate any superiority in terms of mean change in haemoglobin levels compared to placebo. However, the combination of two drugs with long half-life (SP + AQ) in two studies [24, 26] increased the mean haemoglobin level compared to placebo. This relative low PE of ITPsc regimes on anaemia could be, at least partly, explained by the fact that haemoglobin or haematocrit continue to fall after treatment and may return to the normal level within 1 month from the start of malaria treatment. Moreover, malaria recrudescence has been found to delay haematological recovery [31]. Also, more importantly, the negative effect of malaria parasitaemia on heamoglobin level has been shown to decrease with age [32], suggesting that IPT would have a relatively low impact on malaria-related anaemia in schoolchildren. However a low PE of IPT against anaemia has also been observed in infants [33]. This adds more evidence on the expected efficacy of long half-life drug to protect against malaria parasitaemia recrudescence and thus against malarial anaemia. Given that malaria-related anaemia is multifactorial, involving haemolysis, iron deficiency due to impaired intestinal iron absorption, and red cell production failure (RCPF) [34, 35], the supplementation of ingested iron may rapidly replenish red blood cells (RBCs) and shorten haematological recovery after malaria infection has been cleared.
No deaths could be attributed to administration of drugs for IPTsc and observed severe adverse events occurred in both interventions and control groups. However, some adverse events judged mild or moderate were more frequent in intervention groups in one study.
Based on these findings, SP monotherapy should be considered the worst therapeutic regimen for IPTsc in area of high resistance to SP. However, SP has several benefits, including its low cost and proven safety. Moreover, studies have shown that SP could still be effective even in the presence of a high level of resistance in adults [36]. The underlying explanation could be that immunity increases with age and may modify the effect of anti-malarial drugs [37]. On the other hand, DP and SP + AQ appear to be the most promising drug regimen for IPTsc. However, given that the effect of IPT is mainly prophylactic, short-acting drugs such as artemesinins would be expected to provide little direct benefit in asymptomatic children and monthly administration of such drugs, though effective, may be challenging and costly. Moreover, the drug pressure in the context of IPT may lead to an increase of the selection of mutants resistant to artemisinin. Therefore, combination of SP with another long half-life such as piperaquine (PQ), AQ or mefloquine may be better option for investigation in clinical trials in schoolchildren. An additional advantage of combining two long half-life drugs is the reduction of risk of resistance to the two drugs as they have similar elimination half-lives [38]. IPT using long half-life drugs also appears to be more realistic in terms of frequency of drug administration, which can be bi- or three-monthly, and in children compliance.
This review suggests a need for harmonization in regard to the timing and frequency of drug administration as well as the time frame for drug evaluation in the context of IPT. IPT describes the administration of a drug at specified time intervals, allowing a very low concentration of drug (below the inhibitory level) between two treatments, with the aim of preventing mortality or morbidity. This should differ from chemoprophylaxis where the drug concentration is maintained above the level that inhibits parasitic growth [16]. A great variation in IPT drug timing and frequency of administration as well as the time frame for evaluation of IPT between studies has been observed, suggesting some overlaps between IPT and chemoprophylaxis. When a long-acting drug such as SP or piperaquine is used for IPT, a protective blood concentration may be sustained for several weeks, thus providing a period of chemoprophylaxis. Dicko et al. evaluated the efficacy of the SP administered every 2 months [23]. Given the long half-life of SP, this clinical trial should be considered evaluating chemoprophylaxis based on SP, rather than an IPT. In fact, a study conducted in the context of high resistance of SP reported that SP offered optimum protection until the fifth week after administration and that protection disappeared after the eighth week [30]. Similarly, the time frame for the evaluation of IPT should differ from that of chemoprophylaxis. An evaluation occurring when the drug concentration is optimal or above the minimum inhibitory concentration (MIC) would account for the effectiveness of chemoprophylaxis rather than an IPT.
Beside the choice of the appropriate drug regimen, one would anticipate the feasibility of this strategy. Schools have been suggested as a platform for health intervention delivery (deworming, iron-folic acid, nutrients supplementation, (boost-immunization). These interventions have been shown to improve not only children’s health and nutrition, but also their learning ability [39, 40]. Therefore, the increasing number of children of school-age and a higher number of these children attending a primary school [41] combined with the known impact of malaria on school-aged children’s health reasonably suggests that IPTsc could be part of the package of school health intervention, if this benefit is sufficiently proven.
The present study has a number of limitations. Since the search focused on the Pubmed database and articles published in English, there is a risk some other studies are missing. However, this is unlikely given the very limited number of trials conducted on IPTsc. Individual patient data were unavailable, therefore, the effect of baseline parasitaemia, age, ITN usage, or nutritional status on the efficacy of IPT could not be assessed. The high variability (heterogeneity in clinical, methodological and statistical aspects) across studies precludes a meta-analysis. Moreover, the small number of available studies could not allow a pooled analysis in sub-group regimes. Therefore, protective effect of regimes vs placebo or controls against clinical or asymptomatic malaria and anaemia were assessed without combined estimates.
Conclusion
This systematic review found only five studies assessing the efficacy of IPTsc. Today, SP may not be a promising regimen for IPTsc in areas where resistance to this drug is high. Arteminisinin combination therapies (ACTs) (DP, SP + AS, AQ + AS) provided acceptable protective efficacy against clinical malaria, parasitaemia and anaemia. DP administered monthly demonstrated the highest PE. However, acceptability, feasibility and thus, effectiveness of a monthly administration of IPTsc is not known. Further, ACT is used for curative purposes. Combining at least two long half-life drugs, such as piperaquine plus SP may be, at present, the most promising option. More studies assessing efficacy of IPTsc in particular against malaria-related anaemia and clinical malaria must be conducted.
Abbreviations
- CI:
-
confidence interval
- DP:
-
dihydroartemisinin-piperaquine
- DRC:
-
Democratic Republic of the Congo
- IPT:
-
intermittent preventive treatment
- IPTsc:
-
intermittent preventive treatment in schoolchildren
- IRR:
-
incidence rate ratio
- PE:
-
protective effect
- PYAR:
-
person years at risk
- RCPF:
-
red cell production failure
- RR:
-
rate ratio
- SP:
-
sulfadoxine-pyrimethamine
- SP + AQ:
-
sulfadoxine-pyrimethamine plus amodiaquine
- SP + AS:
-
sulfadoxine-pyrimethamine plus artesunate
- AQ + AS:
-
Amodiaquine plus artesunate
- SSA:
-
sub-Saharan Africa
- DP:
-
dihydroartemisinin-piperaquine
- WHO:
-
World Health Organization
- ICTRP:
-
International Clinical Trials Registry Platform
- MIC:
-
minimum inhibitory concentration
- RBC:
-
red blood cells
References
WHO: World malaria report 2014. Geneva: World Health Organization, 2014.
Breman JG, Alilio MS, Mills A. Conquering the intolerable burden of malaria: what’s new, what’s needed: a summary. Am J Trop Med Hyg. 2004;71:1–15.
Brooker S, Clarke S, Snow RW, Bundy DA. Malaria in African schoolchildren: options for control. Trans R Soc Trop Med Hyg. 2008;102:304–5.
Clarke SE, Brooker S, Njagi JK, Njau E, Estambale B, Muchiri E, et al. Malaria morbidity among school children living in two areas of contrasting transmission in western Kenya. Am J Trop Med Hyg. 2004;71:732–8.
Bundy D, Shaeffer S, Jukes M, Beegle K, Gillespie A, Drake L, et al. School-based health and nutrition programs. In: Jamison D, Breman J, Meacham A, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P, editors. Disease control priorities for developing countries. New York: Oxford University Press; 2006. p. 1091–108.
King N, Dewey C, Borish D. Determinants of primary school non-enrollment and absenteeism: results from a retrospective, convergent mixed methods, cohort study in rural Western Kenya. PLoS One. 2015;10:e0138362.
Bundy DA, Lwin S, Osika JS, McLaughlin J, Pannenborg CO. What should schools do about malaria? Parasitol Today. 2000;16:181–2.
Al Serouri AW, Grantham-McGregor SM, Greenwood B, Costello A. Impact of asymptomatic malaria parasitaemia on cognitive function and school achievement of schoolchildren in the Yemen Republic. Parasitology. 2000;121:337–45.
Lalloo DG, Olukoya P, Olliaro P. Malaria in adolescence: burden of disease, consequences, and opportunities for intervention. Lancet Infect Dis. 2006;6:780–93.
Fast-Track-Initiative. Quality education for all children: meeting the challenge. Washington DC: World Bank 2007.
Ceesay SJ, Casals-Pascual C, Erskine J, Anya SE, Duah NO, Fulford AJ, et al. Changes in malaria indices between 1999 and 2007 in The Gambia: a retrospective analysis. Lancet. 2008;372:1545–54.
O’Meara WP, Bejon P, Mwangi TW, Okiro EA, Peshu N, Snow RW, et al. Effect of a fall in malaria transmission on morbidity and mortality in Kilifi, Kenya. Lancet. 2008;372:1555–62.
K’Oyugi BO. Effects of bed nets and anti-malaria drugs use on childhood mortality in Kenya’s malaria endemic and epidemic areas. BMC Public Health. 2015;15:34.
Lengeler C: Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev 2004; CD000363.
Trape JFPPM-PB. Criteria for diagnosing clinical malaria among a semi-immune population exposed to intense and perennial transmission. Trans R Soc Trop Med Hyg. 1985;79:435–42.
Greenwood B. Intermittent preventive treatment–a new approach to the prevention of malaria in children in areas with seasonal malaria transmission. Trop Med Int Health. 2006;11:983–91.
Konate AT, Yaro JB, Ouedraogo AZ, Diarra A, Gansane A, Soulama I, et al. Intermittent preventive treatment of malaria provides substantial protection against malaria in children already protected by an insecticide-treated bednet in Burkina Faso: a randomised, double-blind, placebo-controlled trial. PLoS Med. 2011;8:e1000408.
Bojang K, Akor F, Bittaye O, Conway D, Bottomley C, Milligan P, et al. A randomised trial to compare the safety, tolerability and efficacy of three drug combinations for intermittent preventive treatment in children. PLoS One. 2010;5:e11225.
McGready R. Intermittent preventive treatment of malaria in infancy. Lancet. 2009;374:1478–80.
Shulman CE, Dorman EK, Cutts F, Kawuondo K, Bulmer JN, Peshu N, et al. Intermittent sulphadoxine-pyrimethamine to prevent severe anaemia secondary to malaria in pregnancy: a randomised placebo-controlled trial. Lancet. 1999;353:632–6.
Schultz LJ, Steketee RW, Macheso A, Kazembe P, Chitsulo L, Wirima JJ. The efficacy of antimalarial regimens containing sulfadoxine-pyrimethamine and/or chloroquine in preventing peripheral and placental Plasmodium falciparum infection among pregnant women in Malawi. Am J Trop Med Hyg. 1994;51:515–22.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–12.
Dicko A, Sagara I, Sissoko MS, Guindo O, Diallo AI, Kone M, et al. Impact of intermittent preventive treatment with sulphadoxine-pyrimethamine targeting the transmission season on the incidence of clinical malaria in children in Mali. Malar J. 2008;7:123.
Clarke SE, Jukes MC, Njagi JK, Khasakhala L, Cundill B, Otido J, et al. Effect of intermittent preventive treatment of malaria on health and education in schoolchildren: a cluster-randomised, double-blind, placebo-controlled trial. Lancet. 2008;372:127–38.
Barger B, Maiga H, Traore OB, Tekete M, Tembine I, Dara A, et al. Intermittent preventive treatment using artemisinin-based combination therapy reduces malaria morbidity among school-aged children in Mali. Trop Med Int Health. 2009;14:784–91.
Nankabirwa J, Cundill B, Clarke S, Kabatereine N, Rosenthal PJ, Dorsey G, et al. Efficacy, safety, and tolerability of three regimens for prevention of malaria: a randomized, placebo-controlled trial in Ugandan schoolchildren. PLoS One. 2010;5:e13438.
Nankabirwa JI, Wandera B, Amuge P, Kiwanuka N, Dorsey G, Rosenthal PJ, et al. Impact of intermittent preventive treatment with dihydroartemisinin-piperaquine on malaria in Ugandan schoolchildren: a randomized, placebo-controlled trial. Clin Infect Dis. 2014;58:1404–12.
Naidoo I, Roper C. Drug resistance maps to guide intermittent preventive treatment of malaria in African infants. Parasitology. 2011;138:1469–79.
Kweku M, Liu D, Adjuik M, Binka F, Seidu M, Greenwood B, et al. Seasonal intermittent preventive treatment for the prevention of anaemia and malaria in Ghanaian children: a randomized, placebo controlled trial. PLoS One. 2008;3:e4000.
Cairns M, Gosling R, Gesase S, Mosha J, Greenwood B, Chandramohan D. Mode of action and choice of antimalarial drugs for intermittent preventive treatment in infants. Trans R Soc Trop Med Hyg. 2009;103:1199–201.
Price RN, Simpson JA, Nosten F, Luxemburger C, Hkirjaroen L, ter Kuile F, et al. Factors contributing to anemia after uncomplicated falciparum malaria. Am J Trop Med Hyg. 2001;65:614–22.
Knoblauch AM, Winkler MS, Archer C, Divall MJ, Owuor M, Yapo RM, et al. The epidemiology of malaria and anaemia in the Bonikro mining area, central Cote d’Ivoire. Malar J. 2014;13:194.
Aponte JJ, Schellenberg D, Egan A, Breckenridge A, Carneiro I, Critchley J, et al. Efficacy and safety of intermittent preventive treatment with sulfadoxine-pyrimethamine for malaria in African infants: a pooled analysis of six randomised, placebo-controlled trials. Lancet. 2009;374:1533–42.
van Boele HM, Calis JC, Phiri KS, Vet R, Munthali F, Kraaijenhagen R, et al. Pathophysiological mechanisms of severe anaemia in Malawian children. PLoS One. 2010;5:e12589.
Crawley J. Reducing the burden of anemia in infants and young children in malaria-endemic countries of Africa: from evidence to action. Am J Trop Med Hyg. 2004;71:25–34.
Likwela JL, d’Alessandro U, Lokwa BL, Meuris S, Dramaix MW. Sulfadoxine-pyrimethamine resistance and intermittent preventive treatment during pregnancy: a retrospective analysis of birth weight data in the Democratic Republic of Congo (DRC). Trop Med Int Health. 2012;17:322–9.
Francis D, Nsobya SL, Talisuna A, Yeka A, Kamya MR, Machekano R, et al. Geographic differences in antimalarial drug efficacy in Uganda are explained by differences in endemicity and not by known molecular markers of drug resistance. J Infect Dis. 2006;193:978–86.
White NJ. Intermittent presumptive treatment for malaria. PLoS Med. 2005;2:e3.
Beasley NM, Tomkins AM, Hall A, Kihamia CM, Lorri W, Nduma B, et al. The impact of population level deworming on the haemoglobin levels of schoolchildren in Tanga, Tanzania. Trop Med Int Health. 1999;4:744–50.
Guyatt HL, Brooker S, Kihamia CM, Hall A, Bundy DA. Evaluation of efficacy of school-based anthelmintic treatments against anaemia in children in the United Republic of Tanzania. Bull World Health Organ. 2001;79:695–703.
Report of the Secretary-General on the work of the Organization, A/68/1, United Nations, New York, 2013. http://mdgs.un.org/unsd/mdg/Resources/Static/Products/SGReports/68_1/A_68_1_E.pdf. Visited on 25-05-2015.
Authors’ contributions
JRM developed and conducted a systematic literature search, performed statistical analysis and drafted the manuscript. RAIL, PM, PTL, and JPVG reviewed the manuscript and provided critical inputs. All authors read and approved the final manuscript.
Acknowledgements
The authors thank the Flemish Interuniversity Council (VLIR-UOS) and the Research Foundation—Flanders (FWO) of Belgium for their technical support.
Competing interests
The authors have declared they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Matangila, J.R., Mitashi, P., Inocêncio da Luz, R.A. et al. Efficacy and safety of intermittent preventive treatment for malaria in schoolchildren: a systematic review. Malar J 14, 450 (2015). https://doi.org/10.1186/s12936-015-0988-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-015-0988-5