Abstract
Background
Funding for malaria control and elimination in Myanmar has increased markedly in recent years. While there are various malaria control tools currently available, two interventions receive the majority of malaria control funding in Myanmar: (1) insecticide-treated bed nets and (2) early diagnosis and treatment through malaria community health workers. This study aims to provide practical recommendations on how to maximize impact from investment in these interventions.
Methods
A simple decision tree is used to model intervention costs and effects in terms of years of life lost. The evaluation is from the perspective of the service provider and costs and effects are calculated in line with standard methodology. Sensitivity and scenario analysis are undertaken to identify key drivers of cost effectiveness. Standard cost effectiveness analysis is then extended via a spatially explicit resource allocation model.
Findings
Community health workers have the potential for high impact on malaria, particularly where there are few alternatives to access malaria treatment, but are relatively costly. Insecticide-treated bed nets are comparatively inexpensive and modestly effective in Myanmar, representing a low risk but modest return intervention. Unlike some healthcare interventions, bed nets and community health workers are not mutually exclusive nor are they necessarily at their most efficient when universally applied. Modelled resource allocation scenarios highlight that in this case there is no “one size fits all” cost effectiveness result. Health gains will be maximized by effective targeting of both interventions.
Similar content being viewed by others
Background
Malaria in Myanmar is important not only because of the health burden to the country’s own population, but because of the emergence of artemisinin resistant Plasmodium falciparum parasites in the region [1–3]. The burden of malaria in Myanmar is spatially heterogeneous and seasonal. An estimated 37 % of the population live in areas broadly considered at high risk of malaria (>1 case per 1000 population) and a further 23 % live in areas of low malaria risk (0–1 cases per 1000 population) [4]. Funds for malaria control and elimination in Myanmar have surged in recent years, including the Myanmar specific Three Millennium Development Goal (3MDG) fund and the Global Fund’s Regional Artemisinin Initiative; a US$ 100 million fund of which US$ 40 million has been allocated to Myanmar. The financial resources available to Myanmar at this time are both unprecedented in size and potentially time limited. It is critical, therefore, that these resources are allocated efficiently; maximizing impact and improving financially sustainability.
While there are various malaria control tools currently available, two interventions receive the majority of malaria control funding in Myanmar (1) insecticide-treated bed nets (ITN), including long-lasting insecticide-treated nets and (2) early diagnosis and treatment through malaria community health workers (CHW). ITN are most effective against mosquitoes which are nocturnal, endophagic blood feeders whereas most species commonly found in Myanmar tend toward crepuscular and exophagic biting [5–7]. The evidence base for the cost effectiveness of ITN against malaria spread by the former type of mosquito is strong [8] and previous modelling analysis found that while changes in mosquito biting behaviour could reduce effectiveness, nevertheless ITN could remain a cost effective intervention [9]. Malaria CHW costs have been estimated in Cambodia [10], Nigeria [11] and across sub-Saharan Africa [12].
The malaria policy discourse in Myanmar is frequently framed as a choice between prioritizing universal coverage of either ITN or CHW. While ITN and CHW can be thought of as competing for limited resources they are not mutually exclusive interventions and are in many senses complimentary. It is also the case however that funding is not available for universal access to both interventions, nor has it been demonstrated that such scale-up would be an efficient use of scarce resources in all settings. The factors which determine the costs and effects of both interventions will vary across the country, and context is important in understanding cost effectiveness. This study evaluates the costs and effects of these key malaria control interventions in Myanmar with an emphasis on sensitivity and scenario analysis rather than a generalized cost effectiveness result. Furthermore, targeted allocation of these resources is illustrated by an allocation model for a region of Myanmar.
Methods
Costing
Financial costs are included from the perspective of the National Malaria Control Programme or other malaria intervention funders. In this analysis ITN distribution is assumed to be conducted though a dedicated distribution campaign. ITN cost is comprised of procurement cost (c p ), direct distribution costs (c d ) and programme management (c m ). Cost data were obtained from Three Millennium Development Goal (3MDG), a funding organization in Myanmar, with crosschecking of components against private sector quotations. A distribution of two nets per household is assumed with 10 % wastage (w) and a mean household size of 5.2 people. The primary time horizon is one year and as such the per person ITN cost is annualized according to the lifespan of the net (l), assumed to be three years, using a discount rate of 5 % (r) [13].
CHW costs are derived from separate detailed cost analysis currently under review. To briefly summarize, CHW costs are estimated using an ingredients based micro costing of six cost centres: patient services; training; monitoring and supervision, programme management; incentives and overheads. For this cost effectiveness analysis the cost of treatment (c ACT ) is separated from the remaining CHW cost per person covered (c CHW ). In addition to intervention costs, diagnosis and treatment direct costs for malaria cases treated by the basic health system are included (c ACT ).
Model
CHW are an extension of the health system and therefore marginal utility will depend on locally specific access to treatment. The model must define a common metric to quantify the effects of ITN and CHW. The model calculates the number of years of life lost (YLL), a widely used metric for health impact, through treatment of cases or cases directly averted by bed nets. In this case YLL are likely to be similar to disability adjusted life years as the contribution of morbidity will be negligible compared with mortality. The model was developed in both R (version 3.1.2) and TreeAge (TreeAge Pro 2014, USA).
The probability tree (Fig. 1) traces an individual through a chronological series of event possibilities beginning with an annual probability of contracting malaria (m) which is adjusted by the protective effect of ITN (p), if applicable. Individuals with malaria have a probability they will receive treatment from a provider other than a CHW (a). If a CHW is available in the village there is a probability (q) that a malaria case will seek treatment from the CHW, from both those who would have received treatment elsewhere and from those who would not have received any treatment. Each case of malaria has a probability of death in absence of treatment (μ) and a mean number of YLLs lost per death (d). Treatment is assumed to be with an ACT. The direct reduction in mortality is assumed to be the same for ACT (r 1). The terminal payoffs are scaled by population (v) and calculate the net cost and net effects for each intervention arm for one village (or one township when applied in the resource allocation model, see below). Parameter values can be found in Table 1. For the purpose of this model only one provider is attended per person, individuals may seek treatment at a CHW instead of their previous provider. This is intended to reflect the greater marginal utility is areas with poor access to treatment, even when uptake at the CHW is equal.
The model was developed as the simplest structure that incorporates the key relevant data and provides the desired output metrics of cost and years of life lost. The advantages of a simple model are ease of communication to end users, speed of development and flexibility of application.
Analysis
Bed nets and community health workers are not universally applied interventions and a general estimate of intervention costs and effects misses important variation, particularly with respect to the sometimes extreme remoteness of different populations in Myanmar. Instead, intervention cost effectiveness is calculated in four illustrative accessibility or remoteness scenarios, whereby more remote settings are characterized by increased cost of programme delivery, increased CHW uptake and decreased baseline access to treatment (Table 2). Data are not available to support specific parameterizations for these assumption but the direction of trends are intuitive and supported by policy makers at the national malarial control programme and programme managers at an affiliated non-governmental organization, Medical Action Myanmar. In addition to the scenario analysis, univariate sensitivity analysis is undertaken to identify key determinants of intervention cost effectiveness. Probabilistic Sensitivity Analysis (PSA) can be found in the supporting documentation (Additional File 1). Quantified and non-quantified costs and consequences are summarized in Table 3 to aid interpretation and to highlight potentially important factors which are not included in the quantitative analysis, as recommended for economic evaluations of public health interventions by Weatherly and colleagues [17].
Cost effectiveness ratios are calculated for each intervention against a common null comparator or “no additional intervention” baseline, which includes the number of YLLs expected in absence of intervention and the cost of treatment for patients who receive it. The marginal benefit of each in the presence of the other is not equal to the marginal benefit of each in isolation. A CHW in a village with good bed net coverage has lower impact than in the same village without bed net coverage because there are fewer cases to treat, and vice versa. For this reason the combined intervention arm is included explicitly as a model output rather than as a sum of separate interventions. Estimates are per year and reflect a village of 500 people with 25 malaria cases per year in absence of interventions.
Resource allocation
An extension to standard cost effectiveness analysis, the second stage of this study applies a spatially explicit resource allocation model for a given budget. The model is applied to the Tier 1 or ‘MARC’ region of Myanmar, an area in the east of Myanmar identified as a priority area for malaria control. There are 52 townships in Tier 1 to which a fixed budget of US$ 10 million is allocated. Township specific data on population is from the 2014 census [18] and malaria incidence is based on routine health system surveillance records, currently managed by WHO Myanmar on behalf of the Ministry of Health (2013, unpublished). The malaria surveillance system in Myanmar is undergoing systemic improvements and data capture is not complete. All other parameter values are as reported in Table 1.
The allocation model uses the decision tree in Fig. 1 to calculate cost effectiveness ratios for all intervention options for each geographic patch, in this case a township. Once all scenario cost effectiveness ratios are calculated the model allocates the available budget starting with the most cost effective intervention. As the budget is allocated, the most cost effective intervention in a particular township may be replaced by a less cost effective, but more effective intervention. Dominated intervention scenarios, those where any increase in effect can be achieved by a more cost effective alternative, are excluded. The allocation process ceases when the remaining budget is less than the marginal cost of the next most cost effective intervention. It is worth noting that the optimal allocation of resources is not identified through sequential iteration and improvement of budget allocation options since the cost effectiveness ratios provide sufficient information to identify the allocation result directly. This is more accurate and computationally efficient than identification of a distribution of resources through iterative optimization or “brute-force” calculation of all or a large number of possible distribution scenarios. The resource allocation analysis is repeated to examine the impact of variations in bed net protective effectiveness, CHW uptake and cost sharing for integrated CHW programmes.
Results
The cost effectiveness of malaria control in Myanmar is context dependent. CHW have greater potential effects, particularly in more remote settings, but are also more costly. In the scenario analysis, easily accessible village setting CHW avert 0.51 YLLs per year at a cost of US$ 556 (US$ 1089 per YLL averted). This rises in the very difficult to reach villages to 4.05 YLLs averted at a cost of US$ 2295 (US$ 567 per YLL averted), a higher cost but a more cost effective use of CHWs. Bed nets were consistently less costly and a modestly effective intervention. In the easily accessible village setting bed nets avert 1.24 YLLs at a cost of US$ 238 (US$ 193 per YLL averted), rising to 2.25YLL averted for US$ 750 (US$ 333 per YLL averted). In the very difficult to access village setting, a combination of both bed nets and CHW gives the greatest impact of 5.08 YLLs averted for a cost of US$ 3031 (US$ 597 per YLL averted). The above results are summarized in Table 4 and Fig. 2 and assume that CHW only provide malaria services (this assumption is relaxed in the resource allocation analysis).
Sensitivity analysis
Univariate sensitivity analysis was conducted for the cost effectiveness of CHW (Fig. 3) and bed nets (Fig. 4) using the wide uncertainty ranges in Table 1. The key determinants of cost effectiveness for CHW are baseline access to treatment with an ACT and the likelihood that a person with malaria seeks treatment from the CHW. In reality these two factors may be related; low baseline access to treatment might be expected to increase treatment seeking at a CHW. Univariate sensitivity analysis treats these values as independent. The key determinants of bed net cost effectiveness are the untreated malaria mortality risk and the protective effect of the net. Changes in malaria incidence and mortality affect the magnitude of effects substantially but proportionally for all intervention options, and therefore do not affect intervention comparison.
Resource allocation
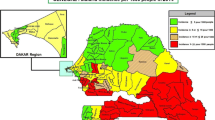
Figure 5a presents an illustrative optimal allocation of an annual budget of US$ 10 million to CHW and ITN roll out in the 52 townships of the MARC region, Myanmar. Almost half of the townships are allocated both CHW and ITN, 12 townships receive ITN only and 15 townships are allocated to provide standard health services without CHW or ITN. Figure 5b–d present the scenario variations where key assumptions are varied in order to observe the effect on resource allocation. Panel b assumes a low ITN protective effect of 5 %, rather than the default 30 %. Panel c presents resource distribution assuming 95 % uptake of CHW by individuals with malaria, rather than 30 %. Panels b and c find that at the margin, CHW rather than ITN should be prioritized. The specific townships receiving these marginal interventions is likely to be an artefact of population size and the residual budget amount at the end of the allocation process. Panel d presents a cost-sharing scenario, where the benefits of an integrated CHW programme are represented by an assumption that funds allocated for malaria control need only fund 50 % of the total programme cost. Notably, the allocation of both CHW and ITN to the majority of Southern, and Western township and to the Kachin townships in the North, is robust to these scenario variations.
Township allocation of malaria interventions in the MARC region, Myanmar. Legends: Maps indicate allocation of US$ 10 million to bed nets and malaria community health workers in the MARC region, Myanmar. a Allocation using default parameter values detailed in Table 1. b Allocation assuming a lower bed net protective effect of 5 %. c Allocation assuming a higher uptake of community health workers; 95 % of malaria infections. d Allocation assuming 50 % cost-sharing for community health workers. For panels (b–d) all parameters other than the specified variation are the default values outlined in Table 1
Discussion
Malaria intervention decisions in Myanmar are based on judgement supported by the limited available evidence. The average and incremental cost effectiveness ratios give decision makers a sense of “bang for buck” to inform these judgements while the resource allocation modelling highlights the importance of targeting both interventions to where they can have the greatest impact. This study finds that CHW have the potential for high impact on malaria, particularly in difficult to access areas, where availability of other services may be low and if CHW use is good. However, CHW are more costly and, if only delivering malaria services, are associated with higher cost-effectiveness ratios. ITN are a robustly cost effective intervention but the total health impact is expected to be lower in Myanmar due to the biting habits of the of the main mosquito vector species. The annualization of the ITN cost over the lifespan of the net, conservatively assumed to be three years, means the comparative cost is lower. Although the cost of health gains is low with ITN, in the context of planning for malaria elimination more impactful interventions will need to be considered.
The cost effectiveness of both CHW and ITN is sensitive to the baseline availability of treatment, indicating that services will be most cost effective when targeted to areas with poor access to malaria diagnosis and treatment. The utilization of CHW is also very important and investment is quality training, CHW supervision and community engagement may be important to implementing a cost effective CHW programme [19]. A further option available to planners seeking to improve the cost effectiveness of CHW programmes is to expand the package of services offered by CHW. This is already happening and many CHW are now also providing a basic health care package or providing additional services such as tuberculosis detection and treatment. Measures to improve the cost effectiveness of community health workers include expanding the scope of available services; strategies to improve the likelihood that community members seek treatment from the community health worker when they have fever; and targeting community health workers to where they will be most cost effective.
For several reasons the main analysis does not apply a cost effectiveness threshold. It is difficult to define an appropriate threshold for the cost per YLL or DALY averted; the budget context in Myanmar is complex with modest NMCP funds being supplemented by international aid. Moreover in the context of a drive towards elimination all interventions will cease to appear cost effective as the malaria burden decreases (in absence of a model for long term benefits). The use of measures such as cost-per DALY averted are, therefore, less relevant and highly uncertain [20, 21]. The most immediately relevant question is how to maximize impact from malaria funds available in Myanmar and for this no threshold is necessary.
An extension of standard cost effectiveness analysis to spatially (in this case township-wise) specific resource allocation modelling highlights the need for a paradigm shift in policy discussion from prioritizing universal coverage of the “most cost effective” intervention to targeting of both interventions and presents illustrative township specific recommendations. In this analysis, malaria burden and to a lesser extent population numbers determine the optimal distribution of resources. Future work will seek to include additional data specific to each township.
Part of the aim of this study is to formalize through a cost effectiveness framework the kind of intuitive judgements that many policy makers and influencers in Myanmar are discussing. There has been much debate regarding the various merits of bed nets and malaria CHW. This paper does not come down on either side of this debate but seeks to summarize the characteristics of each and highlight the importance of targeting both to areas where impact can be maximized.
Limitations
This study has several limitations. The model does not include human population movement or malaria transmission dynamics. A malaria transmission model, incorporated into the cost effectiveness model, would be a useful extension. This would allow indirect effects to be incorporated into the analysis and allow provide projections of the impact on malaria transmission going forward. The analysis does not include benefits to the patient beyond malaria impact, such as reduced costs to access care nor are issues of service quality examined here. For CHW there is a strong interest in extending their ability to diagnose and treat other causes of illness and therefore higher health gains than accounted for here. The model considers malaria control in the general population and does not specifically include high-risk groups such as migrant or mobile populations. Resource allocation modelling is applied at the township level whereas in Myanmar townships make decisions to allocate malaria interventions on a village-by-village basis. Finally, township variation here is characterized by population and malaria burden. Costs, baseline access to treatment and treatment-seeking behaviour are not assumed to vary between townships.
References
Tun KM, Imwong M, Lwin KM, Win AA, Hlaing TM, Hlaing T et al. Spread of artemisinin-resistant Plasmodium falciparum in Myanmar: a cross-sectional survey of the K13 molecular marker. Lancet Infect Dis. 2015;15:415–21.
Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C, Lim P, Suon S et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2014;371:411–23.
Takala-Harrison S, Jacob CG, Arze C, Cummings MP, Silva JC, Dondorp AM, et al. Independent emergence of artemisinin resistance mutations among Plasmodium falciparum in Southeast Asia. J Infect Dis. 2014.
WHO. World Malaria Report. Geneva: World Health Organization; 2013.
Smithuis FM, Kyaw MK, Phe UO, van der Broek I, Katterman N, Rogers C, et al. The effect of insecticide-treated bed nets on the incidence and prevalence of malaria in children in an area of unstable seasonal transmission in western Myanmar. Malar J. 2013;12:363.
Kongmee M, Achee NL, Lerdthusnee K, Bangs MJ, Chowpongpang S, Prabaripai A, et al. Seasonal abundance and distribution of Anopheles larvae in a riparian malaria endemic area of western Thailand. Southeast Asian J Trop Med Public Health. 2012;43:601–13.
Shi W, Zhou X, Zhang Y, Zhou X, Hu L, Wang X, et al. An investigation on malaria vectors in western part of China–Myanmar border. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2011;29:134–7.
White MT, Conteh L, Cibulskis R, Ghani AC. Costs and cost-effectiveness of malaria control interventions–a systematic review. Malar J. 2011;10:337.
Briet OJ, Chitnis N. Effects of changing mosquito host searching behaviour on the cost effectiveness of a mass distribution of long-lasting, insecticidal nets: a modelling study. Malar J. 2013;12:215.
Yeung S, Damme WV, Socheat D, White NJ, Mills A. Cost of increasing access to artemisinin combination therapy: the Cambodian experience. Malar J. 2008;7:84.
Onwujekwe O, Uzochukwu B, Ojukwu J, Dike N, Shu E. Feasibility of a community health worker strategy for providing near and appropriate treatment of malaria in southeast Nigeria: an analysis of activities, costs and outcomes. Acta Trop. 2007;101:95–105.
McCord GC, Liu A, Singh P: Deployment of community health workers across rural sub-Saharan Africa: financial considerations and operational assumptions. Bull World Health Organ. 2013; 91:244–53B.
Drummond MF, Sculpher MJ, Torrance GW. Methods for the economic evaluation of health care programs. Oxford: Oxford University Press; 2005.
Lubell Y, Staedke SG, Greenwood BM, Kamya MR, Molyneux M, Newton PN, et al. Likely health outcomes for untreated acute febrile illness in the tropics in decision and economic models; a Delphi survey. PLoS One. 2011;6:e17439.
Lindblade KA, Mwandama D, Mzilahowa T, Steinhardt L, Gimnig J, Shah M, et al. A cohort study of the effectiveness of insecticide-treated bed nets to prevent malaria in an area of moderate pyrethroid resistance, Malawi. Malar J. 2015;14:31.
Lengeler C. Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev. 2004;2:CD000363.
Weatherly H, Drummond M, Claxton K, Cookson R, Ferguson B, Godfrey C, et al. Methods for assessing the cost-effectiveness of public health interventions: key challenges and recommendations. Health Policy Amst Neth. 2009;93:85–92.
Myanmar Census [http://countryoffice.unfpa.org/myanmar/census/].
Kok MC, Dieleman M, Taegtmeyer M, Broerse JEW, Kane SS, Ormel H, et al. Which intervention design factors influence performance of community health workers in low- and middle-income countries? A systematic review. Health Policy Plan. 2014. doi:10.1093/heapol/czu126.
Lubell Y. Investment in malaria elimination: a leap of faith in need of direction. Lancet Glob Health. 2014;2:e63–4.
Drake T. Priority setting in global health: towards a minimum DALY value. Health Econ. 2014;23:248–52.
Authors’ contributions
TD and YL conceived of the study. TD and SSK completed the costing sections. TD developed the model and undertook the analyses. FS, ND, LJ, MPK and YL provided critical feedback during several iterations of the analysis and manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to acknowledge the support of the National Malaria Control Programme, the Department of Medical Research and the World Health Organization, Myanmar Country Office.
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Funding statement This work was supported by the Three Millennium Development Goal (3MDG) Fund, the Bill and Melinda Gates Foundation (BMGF) and the Wellcome Trust Major Overseas Programme in SE Asia (grant number 106698/Z/14/Z).
Author information
Authors and Affiliations
Corresponding author
Additional file
12936_2015_886_MOESM1_ESM.pdf
Additional file 1. Cost effectiveness and resource allocation of malaria control in Myanmar: further sensitivity and scenario analyses.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Drake, T.L., Kyaw, S.S., Kyaw, M.P. et al. Cost effectiveness and resource allocation of Plasmodium falciparum malaria control in Myanmar: a modelling analysis of bed nets and community health workers. Malar J 14, 376 (2015). https://doi.org/10.1186/s12936-015-0886-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-015-0886-x