Abstract
Background
Indoor residual spraying (IRS) is considered a valuable transmission control measure against malaria but exact efficacy data are not available for many epidemiological settings. This study was conducted to determine indicators for malaria epidemiology and transmission among school children as baseline assessment before IRS implementation in Ghana.
Methods
A cross-sectional study was conducted in Adansi South District of the Ashanti Region and Wa West District of the Upper West Region of Ghana. Malarial parasitaemia and anaemia were determined in pupils between the ages of 2 and 14 years from Early Childhood Development Centres and primary schools. Plasmodium falciparum parasitaemia was detected by light microscopy.
Results
Out of 1,649 pupils who were enrolled at participating schools, 684 were positive for plasmodia resulting in a baseline parasitaemia prevalence of 41.5%. Parasite rate was similar in the two districts (42.0% in Adansi South and 40.7% in Wa West), but differed across the nine sentinel schools ranging from 21 to 63% (p < 0.001). The mean haemoglobin concentration was 11.3 g/dl [standard deviation (SD) ±2.1]. Pupils who had moderate to mild anaemia (7.0–10.9 g/dl) constituted 41.7% of the study sample.
Conclusion
The burden of parasitaemia, malaria and anaemia is a major public health problem among school children in rural Ghana with extensive heterogeneity between schools and warrants further investment in intervention measures.
Similar content being viewed by others
Background
The World Health Organization (WHO) estimates the burden of malaria to be 198 million cases with 584,000 deaths in the year 2013 being a major cause of poverty and low productivity and vice versa [1]. Despite the fact that decreasing numbers of malaria cases and mortality are recently reported in some endemic regions, most countries in sub-Saharan Africa still suffer from an immense burden of malaria mortality. Data indicates that 90% of global deaths due to malaria occur in Africa, especially among children under age five who are the hardest hit with at least 75% of the fatalities [1].
During the time when the study described here was performed, malaria accounted in Ghana for 32% of all outpatient department (OPD) visits and 49% hospital admissions in children under 5 years of age and morbidity was about three million cases with 4,000 deaths annually [2]. Besides hookworm infections, nutritional deficiencies and haemoglobinopathies, malaria is one of the major causes of anaemia in children [3, 4].
Ghana is implementing a malaria control programme with the aim of reducing malaria morbidity and mortality by 75% by the year 2015 in line with the millennium development goals (MDGs). Indoor residual spraying (IRS) has been introduced among other multiple prevention methods such as insecticide treated bed nets usage and chemoprophylaxis in pregnancy. The IRS programme specifically seeks to cover 90% of all structures in targeted districts [2] and has been conducted by the Anglogold Ashanti Malaria Control Programme (AGAMal) that was implemented as corporate social responsibility in the Obuasi Metropolitan District, Ashanti Region. In the first 2 years of its existence, it attained a 50% reduction in the number of malaria cases in Obuasi, and achieved more than 75% reduction in malaria cases within 6 years of implementation resulting in huge savings on malaria medication expenditure, from $55,000 in 2005 to $6,200 in 2010 (unpublished data). Work absenteeism dropped from 6,983 man-days in 2005 to 163 in 2010 indicating the impact of malaria on health in adults. The programme is currently being scaled up in 40 additional districts in Ghana with funding from the Global Fund.
A malaria parasite prevalence study was conducted at selected sentinel sites in the areas of operation to determine the prevalence of parasitaemia and anaemia among children in sentinel pre- and primary schools as baseline data before the start of the AGAMal IRS programme. In malaria-endemic areas, a significant proportion of children harbours parasites without presenting with signs of clinical malaria [5]. Asymptomatic parasitaemia can nevertheless affect the individuals who carry the parasites and these individuals act as transmission reservoirs [6].
Methods
Study setting
This study was conducted in two districts in different Regions in Ghana. The Adansi South District of the Ashanti Region in central Ghana occupies an area of 1,380 km2 in the forest zone. Most parts of Ghana are known to be holoendemic for malaria and transmission of parasites is stable in the rainforest area with an estimated entomological inoculation rate (EIR) of >400 per year [7, 8]. The predominant malaria parasite is Plasmodium falciparum [6] with an incidence of more than one malaria episode per person year at risk (PYAR) in children under 2 years of age [9]. The Wa West District, covering an area of 1,584 km2, is one of nine administrative districts in the Upper West Region in the Northern Belt of of Ghana with almost no detailed data on malaria epidemiology available.
Sampling procedure and data collection
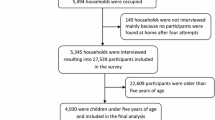
The data for the study were collected from Early Childhood Development Centres (ECDC) and primary school pupils aged from 2 to 14 years in the period between March and April 2012. Community entry was done by contacting the key stakeholders and informing the community at large through a public address system. Sampling frame was obtained through a list of circuits of schools from the District Education Service Directorate (DESD) in Adansi South District and Wa West District. A multi-stage cluster sampling with probability proportional to size (PPS) was conducted according to the protocol recommended by WHO [10]. Primary clusters were five schools circuits in Adansi South and three circuits in Wa West. A total of nine schools were then sampled from these circuits using simple random sampling with a physical randomization device. All pupils present at these schools at the time of sampling and meeting the inclusion criteria were then enrolled in the study. Whilst not representative for the entire district, these baseline data will allow comparison with the post-intervention data in the same schools.
Of the nine schools selected in the second stage of sampling, six schools were selected in Adansi South (Apagya D/A, Asarekrom D/A, Kokotenten D/A, Kwame Nkyi D/A, New Edubiase D/A, and Nsata Subiriso D/A). The remaining three schools were selected in Wa West (Kpanfa D/A, Lassie–Toulu R/C, and Nyoli R/C) whereas the D/As are public schools and the R/Cs are Roman Catholic schools.
Study participants were randomly selected from all eligible pupils using the schools attendance register as sampling frame. Parents or caretakers and teachers were informed about the background and procedures of the study by the research team. Selected pupils who not rejected to participate were recruited into the study after obtaining informed consent from their parents or caretakers. A standardized questionnaire was administered to the parents, two drops of blood were obtained via finger prick and the tympanic temperature recorded from each participant. Trained research staff interviewed the pupils and completed the questionnaire. An episode of clinical malaria was defined as any asexual Plasmodium parasitaemia and a body temperature ≥38°C.
Laboratory procedures
Thick and thin blood films were prepared from finger-prick blood samples and stained with 10% Giemsa for 30 min and examined by immersion oil microscopy with 1,000× magnification. A slide was declared negative after examining 200 high power fields without parasites. Each slide was read independently and blindly by two certified laboratory microscopists. Parasitaemia was quantified per 200 white blood cells (thick smear) or in case of very high parasitaemia per 1,000 erythrocytes (thin film). Slides with discrepant results were read again by a third reader and the median parasitaemia taken as the final result [11]. The haemoglobin concentration was determined with a HemoCue haemoglobin photometer (HemoCue AB, Angelholm, Sweden) as stated by the manufacturer using capillary blood samples from finger pricks.
Statistical analysis
Data were double-entered and cleaned by trained data entry staff at the KCCR using MS Access 2010 and then imported into STATA version 12 (Stata Corp., College Station, Texas: StataCorp LP, USA) for statistical analyses. Proportions are presented as descriptive statistics for all categorical variables. Prevalence of parasitaemia was calculated as overall prevalence and separately for each district. 95% confidence intervals (95% CI) were estimated to provide uncertainty surrounding the point estimates. Means and standard deviations for haemoglobin levels were calculated as overall mean and separately by district and by parasitaemia status. Anaemia was defined as follows: Hb level 10.9–7 g/dl (moderate anaemia) and <7 g/dl (severe anaemia). The level of statistical evidence for an association between parasitaemia and personal characteristics adjusted for school was assessed in a univariate conditional logistic regression. Variables that showed some evidence of an association with parasitemia (p < 0.10) were then included in a multivariate conditional regression model adjusted for school to account for potential confounding. Adjustment for district in univariate and multivariate analyses was not performed as there was no variation of this parameter after adjustment for school. Statistical significance was set at a default alpha of 0.05.
Ethics
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki. Ethical approval for the study was obtained from the Ethics committees of the School of Medical Sciences, Kwame Nkrumah University of Science and Technology (KNUST). Administrative clearance was obtained from district directorates of Ghana Education Service.
Results
A total of 1,649 pupils, 988 from Adansi South District and 661 from Wa West District, were enrolled in the study from nine schools. The ages of the pupils ranged from 2 to 14 years with a median age of 10 years. Some personal characteristics of study participants varied significantly between the two districts (Table 1). Participants in Adansi South were slightly older compared to participants from Wa West (median 9.7 vs 9.3 years). In Adansi South compound houses (small areas tightly surrounded by little connected buildings with a central court) were more common (19.0% vs 4.6%) and reported bednet use was higher (56.2% vs 31.6%). Finally, participants from Adansi South were less likely to be enrolled in the National Health Insurance Scheme (NHIS) (44.9% vs 56.7%) and also sought care at a hospital less frequently if taken ill (49.9% vs 58.0%).
Parasitaemia prevalence and Plasmodium species
The overall parasitaemia prevalence in the study sample was 41.7% and was similar in the two districts: 42.0% [95% confidence interval (CI) 38.9–45.1] in Adansi South and 40.7% (95% CI 36.9–44.4) in Wa West (Table 2). However, the proportion of participants with parasitaemia showed strong heterogeneity between different schools in Adansi South (p < 0.001), varying from 21% in New Edubiase to 63% in Nsata Subiriso (Table 2). Species of Plasmodium detected were: single infections with P. falciparum in 95.9%, Plasmodium malariae in 2.3%, and Plasmodium ovale 0.2% of all cases of parasitaemia. Mixed infections with P. falciparum and P. malariae were present in 1.6% of all cases. Gametocytes were present in 7.6% of participants with parasitaemia (3.1% of all participants).
Haemoglobin concentration
The mean haemoglobin concentration in the study population was 11.3 g/dl (SD ±2.1) (Table 2) and differed slightly between the two districts [Adansi South: 10.9 g/dl (SD ±2.5); Wa West: 11.8 g/dl (SD ±1.3); p < 0.001]. Overall, 55.9% (n = 914) had a normal Hb level (Hb ≥ 11.0 g/dl), 41.7% (n = 682) had a mild to moderate anaemia (Hb 10.9–7 g/dl) and 2.4% (n = 40) a severe anaemia (Hb < 7.0 g/dl). The prevalence of anaemia differed considerably between the two districts [mild to moderate anaemia: Adansi South 52.5% vs Wa West 25.4% (Table 2)].
Body temperature
Body temperature of the pupils ranged from 36.0 to 39.4°C with a mean of 37.3°C (SD ±0.38). Out of the 1,649 apparently healthy participants attending school, 23 (1.4%) had a temperature ≥38.0°C. Out of these, 11 (0.6%) were positive for parasitaemia and thus fulfilled the case definition of symptomatic malaria and of which nine came from the Adansi South. The cases were equally distributed between the schools.
Parasitaemia and anaemia
The mean haemoglobin concentration was significantly lower (p < 0.001) in participants with parasitaemia (10.9 g/dl, SD ±2.1) compared to those without (11.6 g/dl, SD ±2.1). Corresponding to this, only 47.6% of parasitaemic participants had a normal Hb compared to 61.8% of the group without parasitaemia (p < 0.001).
Association between personal characteristics and parasitaemia
Several of the surveyed personal characteristics were associated with a risk of parasitaemia. Table 3 shows the unadjusted (univariate) and adjusted (multivariate conditional logistic regression) analyses of the influence of personal characteristics on the odds of parasitaemia. There was declining risk for parasitaemia with age (multivariate: OR 0.91, 95% CI 0.87–0.95, p < 0.001) and NHIS enrolment (multivariate: OR 0.75, 95% CI 0.60–0.94, p = 0.01). There was no evidence for an association between housing type and parasitaemia. Both the univariate and multivariate analysis indicated that having slept under a bed net in the night before the survey was associated with a higher risk of parasitaemia, but this trend was not significant in the multivariate analaysis (univariate: OR 1.28, 95% CI 1.02–1.59, p = 0.03; multivariate: OR 1.25, 95% CI 0.99–1.57, p = 0.06).
Discussion
Prevalence of malaria parasitaemia among school children without obvious illness was 42% and 41% in participating schools within Adansi South and Wa West, respectively. While the overall parasite rate in the two districts was similar, there was a strong variation of parasitaemia prevalences across schools. As a tendency, the frequency of parasite carriers without fever was higher in the remote villages (e.g. Nsata Subiriso, 63%) than in the district capital (New Edubiase, 21%). This finding is in accordance with other studies demonstrating that the most exposed households are those in the more remote parts of a village or district [12]. Microscopic detection of parasites as used in the study presented here may be limited by a low sensitivity in comparison to PCR and information on multiplicity of P. falciparum infection is lacking. Nevertheless, microscopy was considered sufficient for the comparison of parasite prevalences before and after IRS intervention given that the same methodology is used.
Notably, 11 of the study participants attending school fulfilled the WHO criteria of malaria. The occurrence of malaria in children at school is in line with findings from other countries in sub-Saharan Africa [13, 14] with major impact on performance [15]. The observation that there was no association between malarial parasitaemia and tympanic temperature or fever is in contrast to the findings reported in another study from Cameroon were a significant association between axillary temperature and malarial parasitaemia among apparently asymptomatic school children was found [16]. The observation in the current study could possibly be due to the low number of participants with fever (n = 23) and the resulting low statistical power for this question. Children with Plasmodium infection might have been co-infected with other pathogens causing the fever and resulting in a misclassification as malaria [17].
Similar to the prevalence of parasitaemia, haemoglobin levels and the prevalence of anaemia varied widely between schools. However, there was also significant variation between the two districts because, all cases of anaemia with a haemoglobin <7 g/dl were detected in Adansi South. Interestingly, 9 of the 11 children with fever came from one village possibly indicating a small outbreak of another infection. Furthermore, while our data showed that parasitaemia and anaemia were associated, the different prevalence of anaemia in two districts with similar prevalence of parasitaemia indicated that other co-factors might be involved. Previous studies have shown that causes of paediatric anaemia beyond malaria in Ghana include various nutritional deficiencies, other infections, as well as genetic defects including haemoglobinopathies [18].
Several personal characteristics of the participants were associated with a risk for parasitaemia. As expected, the odds of parasitaemia declined with age. In stable transmission areas such as in Ghana, parasitaemia and malaria symptoms are strongly dependent on the development of semi-immunity after prior exposures [19].
Surprisingly, the data showed that reported use of a bed net in the night before the survey was not associated with any protective effect but, as a tendency, was associated with a slightly higher risk of infection. This finding may be by chance or a result that is confounded by transmission heterogeneity on a microepidemiological scale [20]. Living in an area of high transmission may lead to a higher rate of net usage due to the nuisance of mosquito bites while individuals living in lower transmission areas may not use nets that often. This could result in the paradoxical finding that net usage is a risk factor for parasitaemia. Moreover, there are no data on the quality of the nets, correct use, or whether they were treated with insecticides.
As anticipated, parasitaemia prevalence among pupils enrolled in the national health insurance scheme was lower than those who were not enrolled. Possibly those with membership in NHIS might have better chance of seeking medical care compared to those without membership. It has been shown that households participating in the NHIS scheme had a higher socio-economic status [21] and children from these families had a lower risk for malaria.
Conclusions
The heterogeneity of parasitaemia and haemoglobin levels was high among schools. Accordingly, a large number of schools must be monitored to provide representative figures for a district. The present data will serve as pre-intervention data for comparison with post-intervention data for the estimation of IRS efficacy. It is recommended to perform regular evaluations over time since the degree of temporal and seasonal fluctuations of malaria and haematological parameters in the study areas have neither been investigated previously nor in the present study. The findings indicate that the burden of malaria and anaemia is a relevant public health problem among school children in Ghana and warrants investment in intervention measures to stem the tide.
References
WHO (2014) World Malaria Report 2014. World Health Organization, Geneva. (Available: http://www.who.int/entity/malaria/publications/world_malaria_report_2014/report/en/index.html)
WHO (2011) World Malaria Report 2011. World Health Organization, Geneva. (Available: http://www.who.int/malaria/publications/country/profile_gh_en.pdf)
Ronald LA, Kenny SL, Klinkenberg E, Akoto AO, Boakye I, Barnish G et al (2006) Malaria and anaemia among children in two communities of Kumasi, Ghana: a cross-sectional survey. Malar J 5:105
Murphy SC, Breman JG (2001) Gaps in the childhood malaria burden in Africa: cerebral malaria, neurological sequelae, anaemia, respiratory distress, hypoglycemia, and complications of pregnancy. Am J Trop Med Hyg 64:57–67
Greenwood BM (1987) Asymptomatic malaria infections: do they matter? Parasitol Today 3:206–214
Kobbe R, Neuhoff R, Marks F, Adjei S, Langefeld I, von Reden C et al (2006) Seasonal variation and high multiplicity of first Plasmodium falciparum infections in children from a holoendemic area in Ghana, West Africa. Trop Med Int Health 11:613–619
Abonuusum A, Owusus-Daako K, Tannich E, May J, Garms R, Kruppa T (2011) Malaria transmission in two rural communities in the forest zone of Ghana. Parasitol Res 108:1465–1471
Appawu M, Owusu-Agyei S, Dadzie S, Asoala V, Anto F, Koram K et al (2004) Malaria transmission dynamics at a site in northern Ghana proposed for testing malaria vaccines. Trop Med Int Health 9:164–170
Kobbe R, Adjei S, Kreuzberg C, Kreuels B, Thompson B, Thompson PA et al (2007) Malaria incidence and efficacy of intermittent preventive in infants (IPTi). Malar J 6:163
Bierrenbach A (2008) Steps in applying probability proportional to size (PPS) and calculating basic probability weights. In: Training workshops on TB prevalence surveys. World Health Organization. http://www.who.int/tb/advisory_bodies/impact_measurement_taskforce/meetings/prevalence_survey/psws_probability_prop_size_bierrenbach.pdf. Accessed 12 June 2015
Greenwood BM, Armstrong JR (1991) Comparison of two simple methods for determining malaria parasite density. Trans R Soc Trop Med Hyg 85:186–188
Kreuels B, Kobbe R, Adjei S, Kreuzberg C, von Reden C, Bäter K et al (2008) Spatial variation of malaria incidence in young children from a geographically homogeneous area with high endemicity. J Infect Dis 197:85–93
May J, Mockenhaupt FP, Ademowo OG, Falusi AG, Olumese PE, Bienzle U et al (1999) High rate of mixed and subpatent malarial infections in southwest Nigeria. Am J Trop Med Hyg 61:339–343
Brooker S, Guyatt H, Omumbo J, Shretta R, Drake L, Ouma J (2000) Situation analysis of malaria in school-aged children in Kenya—what can be done? Parasitol Today 16:183–186
Colbourne MJ (1955) The effect of malaria suppression in a group of Accra school children. Trans R Soc Trop Med Hyg 49:556–569
Kimbi HK, Nformi D, Ndamukong KJ (2005) Prevalence of asymptomatic malaria among school children in an urban and rural area in the Mount Cameroon region. Cent Afr J Med 51:5–10
Bejon P, Mwangi T, Lowe B, Peshu N, Hill AV, Marsh K (2007) Clearing asymptomatic parasitaemia increases the specificity of the definition of mild febrile malaria. Vaccine 25:8198–8202
Kreuels B, Kreuzberg C, Kobbe R, Ayim-Akonor M, Apiah-Thompson P, Thompson B et al (2010) Differing effects of HbS and HbC traits on uncomplicated falciparum malaria, anemia, and child growth. Blood 115:4551–4558
Clarke SE, Brooker S, Njagi JK, Njau E, Estambale B, Muchiri E et al (2004) Malaria morbidity among school children living in two areas of contrasting transmission in Western Kenya. Am J Trop Med Hyg 71:732–738
Kreuels B, Kobbe R, Adjei S, Kreuzberg C, von Reden C, Bäter K et al (2008) Spatial variation of malaria incidence in young children from a geographically homogeneous area with high endemicity. J Infect Dis 197:85–93
Sarpong N, Loag W, Fobil J, Meyer CG, Adu-Sarkodie Y, May J et al (2010) National health insurance coverage and socio-economic status in a rural district of Ghana. Trop Med Int Health 15:191–197
Authors’ contributions
NS made contributions to conception, acquisition of data, and drafting of manuscript. EOD made contributions to conception and design. BK made contributions to conception, analysis and manuscript writing. JF made contributions to conception. SS made contributions to organization and acquisition of data. FA acquisition of data and analysis. AH made contributions to data analysis; TK made contributions to organization and acquisition of data. JM made contributions to conception, study design and paper writing. All authors read and approved the final manuscript.
Acknowledgements
We are grateful to the AngloGold Ashanti Malaria Control Limited Programme, District Education Directors, and parents of the pupils for facilitating the study. We extend our thanks to the teachers of the schools involved in the study and the District Education Directorate health coordinators for their enormous contribution to make the study a success. We are grateful to all fieldworkers, the data entry staff, and Dr. Benedikt Hogan for their contributions. This study received financial assistance from the AngloGold Ashanti Malaria Control Limited.
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sarpong, N., Owusu-Dabo, E., Kreuels, B. et al. Prevalence of malaria parasitaemia in school children from two districts of Ghana earmarked for indoor residual spraying: a cross-sectional study. Malar J 14, 260 (2015). https://doi.org/10.1186/s12936-015-0772-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-015-0772-6