Abstract
Background
Although leukemic blast cells of Pro-B cell acute lymphoblastic leukemia (ALL) are arrested at the same stage of B cell differentiation, the immature B cell subtype is still biologically heterogeneous and is associated with diverse outcomes. This study aimed to explore the clinical-biological characteristics of pediatric pro-B ALL and factors associated with outcomes.
Methods
This study enrolled 121 pediatric patients aged 6 months to 14 years with newly diagnosed CD19+CD10− pro-B cell acute lymphoblastic leukemia (pro-B ALL) treated at Beijing Children’s Hospital from March 2003 to October 2018. Genetic abnormalities, immunophenotypic markers, minimal residual disease (MRD) at early treatment stage and long-term outcomes of children treated on two consecutive protocols were analyzed.
Results
KMT2A rearrangements were the most frequent abnormalities (incidence rate 33.06%), and were associated with lower frequency of CD13, CD33, CD22 and CD34 expression and higher frequency of CD7 and NG2 expression. Higher frequency of CD15 and CD133 expression was found in KMT2A-AFF1+ patients, exclusively. Presence of CD15 and absence of CD34 at diagnosis correlated with the high burden of MRD at the early stage of treatment. Outcomes were more favorable in patients older than 1 year, with absence of CD20 expression and KMT2A rearrangements, and with MRD lower than 1% at the end of induction and 0.1% before consolidation. Increased intensity of chemotherapy based on MRD analysis did not improve outcomes significantly (5-year EFS 73.9 ± 6.5% for BCH-2003 and 76.1 ± 5.3% for CCLG-2008, P = 0.975). Independent adverse prognostic factors were MRD ≥ 0.1% before consolidation and presence of KMT2A gene rearrangements (odds ratios [ORs] 9.424 [95% confidence interval (CI) 3.210, 27.662; P < 0.001]; 4.142 [1.535, 11.715, P = 0.005]; respectively).
Conclusions
Pediatric pro-B ALL is a heterogeneous disease. Genetic analysis and MRD evaluation can predict patients with dismal prognosis; however, intensive chemotherapy alone does not improve outcomes of these patients and targeted therapy or hematopoietic stem cell transplantation may be required.
Similar content being viewed by others
Background
B cell precursor acute lymphoblastic leukemia (BCP-ALL) is the most frequent type of pediatric leukemia, representing about 80% of childhood ALL. Based on the stages of differentiation of normal B cell progenitors, BCP-ALL is classified into pro-B ALL (CD19+ CD10− cyμ− Igκ− Igλ−), common-B ALL (CD19+ CD10+ cyμ− Igκ− Igλ−) and pre-B ALL (CD19+ CD10+/− cyμ+ Igκ− Igλ−) [1]. Pro-B ALL, accounting for 6% of pediatric and 16% of adult ALL [2, 3]. This is the most immature subtype of B-ALL and it originates from immature B cell precursors with maturational arrest at the pro-B cell stage. Pro-B ALL has been reported to be associated with unfavorable clinical features and poor prognosis in both childhood and adult patients [2, 4].
Although the leukemic blast cells of pro-B ALL are arrested at the same stage of B cell differentiation, the immature B cell lineage subtype of ALL is biologically heterogeneous and is associated with diverse outcomes [3]. KMT2A rearrangements are the most frequent genetic alteration in pro-B ALL, occurring in one-third of patients, with male prevalence and age less than 1 year; it is associated with dismal prognosis and aggressive clinical features, including hyperleukocytosis and central nervous system (CNS) involvement at diagnosis [2, 5]. High expression of Neuron-Glial antigen 2 (NG2), stem-cell antigen CD133, CD135, myeloid-associated antigen CD15 and CD65s, no expression of CD13, CD 33, and low expression of CD34 are found in KMT2A-AFF1 positive patients [6,7,8]. Other genetic abnormalities, such as BCR-ABL1, have also been reported in about 9% of adult pro-B-ALL patients [3].
In current clinical practice, minimal residual disease (MRD) is assessed to determine the treatment response and subsequent prognosis in children with B-ALL. In many cohorts, MRD testing is introduced in the classification strategy and patients with high MRD levels receive more intensive chemotherapy [9]. In a multicenter clinical study of childhood ALL in China, better 5-year event-free survival (EFS) was achieved in an MRD adjustment group [10]. However, little is known about the significance of MRD in the pro-B ALL subset.
In the present study, we investigated the clinical features, genetic alterations, immunological characteristics, MRD at the early treatment stage and long-term outcomes in a large cohort of pediatric pro-B ALL patients in China treated with two consecutive protocols. Our objective was to further elucidate the biological heterogeneity of this immunophenotypic subgroup and the prognostic factors associated with patient outcomes.
Methods
Patients and treatment protocols
This study included 121 pediatric patients, 6 months to 14 years of age (median, 5 years) with newly diagnosed CD19+CD10− pro-B cell acute lymphoblastic leukemia (pro-B ALL) treated at the Hematology and Oncology Center of Beijing Children’s Hospital, Capital Medical University, between March 2003 and October 2018. The BCH-2003 (Beijing Children’s Hospital-2003) and CCLG-2008 (Chinese Childhood Leukemia Group-2008) protocols were followed in 46 and 75 patients, respectively. The BCH-2003 protocol stratified patients into standard-risk (SR), intermediate-risk (IR) and high-risk (HR) according to their clinical and biological characteristics, prednisone response and morphological remission at the end of induction. Based on this stratification, the CCLG-2008 protocol administered MRD evaluation to modify treatment intensity, in which SR patients with day 33 MRD ≥ 0.01% and < 1% were upstaged to IR, and patients with day 33 MRD > 1% or week 12 MRD > 0.1% were upstaged to HR. Details regarding the stratification and treatment regimens for BCH-2003 and CCLG-2008 protocols are outlined in Additional file 1: Figure S1 and Additional file 2: Table S1, as previously described [11,12,13]. Both protocols were approved by the Beijing Children’s Hospital Institutional Committee. Signed informed consent was provided by the parents or guardians of each pediatric patient.
Immunophenotyping
Patient mononuclear cells were isolated from pretreatment bone marrow aspirate samples by centrifugation on Ficoll-Hypaque density gradients, and stained with combinations of fluorochrome-conjugated monoclonal antibody panel (see Additional file 2: Table S2). Value of 20% was chosen as threshold of positivity for surface marker and 10% for intracytoplasmic antigen. Patients were classified as pro-B, common-B, pre-B, mature-B, T-cell and AML according to the criteria of the European Group for the Immunological Characterization of Acute Leukemias (EGIL) classification system [1]. Expression of CD19 and absence of CD10 surface antigen were required for the diagnosis of pro-B ALL and the immunophenotyping of one pro-B patient is shown in Additional file 3: Figure S2.
Molecular and Fluorescence in situ hybridization (FISH) analysis
Fusion transcript analysis was performed by a multiplex reverse transcription polymerase chain reaction (RT-PCR), as described previously [11, 14]. This system was able to simultaneously detect 29 fusion transcripts associated with B-ALL including BCR/ABL1, E2A-PBX1, E2A-HLF, ETV6/RUNX1, KMT2A/AFF1, KMT2A-MLLT1, KMT2A-MLLT3 and KMT2A-MLLT10 which are related to B-ALL. Patients were also investigated by interphase FISH for KMT2A rearrangements using LSI KMT2A Dual-color Break-Apart Rearrangement Probe (Abbott Laboratories, Dallas, TX, USA). The detailed FISH procedure has been documented in a previous study [15]. FISH images of one KMT2A rearrangement-positive patient are presented in Additional file 4: Figure S3.
Analysis of minimal residual disease
MRD was tested by flow cytometry and/or PCR quantitative method for immunoglobulin and T-cell receptor antigen gene rearrangements. Details of the performance and analysis of MRD by PCR were documented previously [11]. Leukemia-associated immunophenotypes were determined by multiparameter flow cytometry, using 11 panels of monoclonal antibodies conjugated to fluorescein isothiocyanate (FITC), phycoerythirin (PE), allophycocyanin (APC) and perdinin chlorophyII protein (PerCP). The immunophenotypic markers of MRD monitoring were shown in Additional file 2: Table S3 and one patient screening at diagnosis is shown in Additional file 5: Figure S4. For each patient, the marker combination of MRD was determined at diagnosis, identifying at least one leukemic cell per 104 normal nucleated bone marrow cells. The procedures for cell collection, separation, staining and protocol for flow cytometric detection of MRD followed the guidelines of St. Jude Children’s Research Hospital, as described previously [16]. At least 1 × 105 mononuclear cells were added into each MRD test tube. Bone marrow aspirates were collected at day 33 at the end of induction remission and day 78 before consolidation therapy. The leukemic involvement of < 0.01% of nucleated bone marrow cells was regarded as MRD negative [17]. Isotypical immunoglobulins were used as negative controls.
Statistical analysis
The reference date for the end of data collection for the purpose of statistical analysis was December 31, 2018. Comparisons between patients with or without distinct immunological marker, KMT2A gene rearrangements and associations of pretreatment characteristics and response to treatment were evaluated by nonparametric tests. EFS was defined from the date of diagnosis to the date of relapse, death, or induction failure, whichever came first, or the last contact with patients in continuous hematologic complete remission. EFS distribution of patients with different clinical and biological features was estimated using the Kaplan–Meier procedure; comparisons between groups were performed using the log-rank test. The Cox proportional hazards regression model was used to determine significant differences in associations between patients’ biological/clinical indicators and outcomes. All tests were two-sided and P < 0.05 was considered statistically significant. SPSS 16.0 software (SPSS, Chicago IL, USA) was used for all statistical analyses.
Results
Genetic abnormalities in pro-B-ALL
Specific fusion transcripts were detected in 40 patients, with an incidence rate of 33.06% (40/121), involving KMT2A rearrangements, BCR-ABL1, ETV6-RUNX1 and E2A-PBX1. The description of the incidence of each fusion transcript is shown in Additional file 2: Table S4. KMT2A gene rearrangements, accounting for one-quarter of pediatric pro-B-ALL patients, were the most frequent translocation. Compared with patients with BCR-ABL1, ETV6-RUNX1 and without fusion, KMT2A gene-rearranged patients had a significantly higher proportion of infants and higher WBC counts. However, no differences were found in prednisone response and early treatment MRD between fusion subgroups (see Table 1). Furthermore, no differences were found in clinical and biological characteristics between patients with KMT2A-AFF1 and other KMT2A rearrangements (see Additional file 2: Table S5).
Immunophenotypic characteristics of pro-B ALL
All patients with pro-B-ALL were positive for CD19, cyCD79a and HLA-DR. 63.64%, and 6.31% of patients expressed B cell markers CD22 and CD20, respectively. T cell markers, including CD2, CD5 and CD7, were detected in fewer than 10% of patients, and no cytoplasmic CD3 antigen was detected. Myeloid lineage markers CD13 and CD33 were expressed in 20.66% and 50.41% of patients, respectively. Approximately four-fifths of patients demonstrated CD34 and cyTdT expression. Over one-third of patients expressed primitive cell antigen CD133, and only 2.48% patients expressed hematopoietic progenitor CD117. Aberrantly expressed CD15, CD56 and CD58 were detected in 21.05%, 15.79% and 12.40% of patients, respectively. Carcinoembryonic antigen CD66c was found in 6.58% and NG2 was detected in 39.47% of patients (see Additional file 2: Table S6). Further analysis of correlations between the expression of specific immunological markers and clinical features revealed that the frequency of NG2 expression was significantly higher in patients younger than 1 year old. Patients with CD15 expression had a higher ratio of MRD ≥ 1% at day 33 and ≥ 0.1% at day 78, while patients with CD34 expression had a lower proportion of MRD ≥ 1% at day 33 than those without (see Table 2). Meanwhile, no correlations were found between other immunological markers and clinical features (Additional file 2: Table S7).
Associations between immunophenotypic markers and genetic abnormalities
Patients with KMT2A rearrangements showed a statistically significant lower frequency of CD13, CD33, CD22 and CD34 expression, and higher frequency of CD7, NG2, CD15 and CD133 expression. The high frequency of CD15 and CD133 in KMT2A-rearranged subgroup was found to be due to the expression in patients with KMT2A-AFF1+, and was not found in other KMT2A-rearranged patients. Frequency in the latter was similar to that in non-KMT2A-rearranged patients. Also, CD2, CD5 and CD66c expression was not detected in any of the KMT2A-rearranged patients, although no statistically significant differences were found (see Table 3). In addition, no correlations were found between immunological markers and other genetic abnormalities, including BCR-ABL1, ETV6-RUNX1 and IKZF1 deletion (see Additional file 2: Table S8).
Outcomes and prognostic factors analysis
Follow-up of these 121 pediatric pro-B-ALL patients ranged from 0.5 to 184.0 months (median, 66.0 months), with a 5-year EFS of 75.1 ± 4.1%. During follow-up, one patient had induction failure, twenty-three patients experienced bone marrow relapse, four patients experienced isolated extramedullary relapse, three patients died of severe infections during induction, one patient died of severe toxicity from high-dose methotrexate (HD-MTX) and 89 patients were in first remission. Because the CCLG-2008 protocol introduced MRD evaluation to modify treatment intensity, comparison of outcomes revealed no significant differences between protocols: 5-year EFS was 73.9 ± 6.5% for BCH-2003 and 76.1 ± 5.3% for CCLG-2008, P = 0.975. However, the EFS rates varied significantly between clinical-biological subgroups. Favorable outcomes were found in patients older than 1 year, those with absence of CD20 expression and with KMT2A rearrangements, and with an MRD lower than 1% at day 33 and 0.1% at day 78, as shown in Table 4. However, other clinical and biological factors were not associated with patients’ outcomes (see Additional file 2: Table S8). Cox proportional hazards regression analysis identified MRD ≥ 0.1% at day 78 and presence of KMT2A gene rearrangements as independent adverse prognostic factors (OR 9.424 [95% CI 3.210, 27.662; P < 0.001); and (OR 4.142 CI 1.535, 11.715; P = 0.005); respectively (see Table 4 and Fig. 1). In the analysis of the outcomes of patients without any fusion, MRD at day 33 and day 78 were also found to be associated with patients’ outcomes, but only MRD at day 78 was an independent prognostic factor; the other biological characteristics were not associated with outcomes. (see Additional file 2: Tables S9, S10 and Additional file 6: Figure S5).
Discussion
In previous studies, Pro-B immunophenotype was regarded as an unfavorable outcome indicator in both pediatric and adult ALL [2, 4], and patients with pro-B-ALL were considered as candidates for allogeneic hematopoietic stem cell transplantation (allo-HSCT) [3]. However, after gaining an impressive understanding of the associations between genetic abnormalities and treatment effects for ALL, pro-B-ALL was shown to be a heterogeneous malignancy with clinical and biological diversity [3, 18]. In the present study, we investigated the genetic and immunological characteristics of pro-B-ALL and their correlation with outcomes in a large cohort of Chinese pediatric pro-B-ALL patients treated using two consecutive protocols. Four common genetic alterations, including ETV6-RUNX1, E2A-PBX1, BCR-ABL1 and KMT2A rearrangements, were all present in pro-B-ALL. KMT2A rearrangement was the most frequent (~ 26%) translocation, and was lower than those reported previously in childhood (~ 50%) and adult (~ 64–75%) pro-B-ALL patients with Caucasian origins [5, 18,19,20]. However, the proportion (81.82%, 9/11) of KMT2A-rearranged infant pro-B-ALL was similar to that in previous findings [21, 22]. These results suggest that the KMT2A gene abnormality plays a leading role in the leukemogenesis mechanism of infant leukemia, regardless of racial differences, whereas the gene profile of Chinese pediatric patients with pro-B-ALL differs in part from those in western countries. In line with other reports [2, 5], KMT2A-rearranged patients in the present study also presented with adverse clinical features, including high leukocyte counts and younger age at diagnosis.
In the present study, the detailed analysis of immunological markers showed them to be associated with treatment response, KMT2A rearrangements and patients’ outcomes. Patients with KMT2A rearrangements were disclosed as having typical immunological profiles, with a lower proportion of CD33+, CD13+, CD22+ and CD34+ expression and a higher proportion of CD7+, CD15+, CD133+ and NG2+ expression, in which the higher rates of CD15 and CD133 expression were mostly due to KMT2A-AFF1+ rather than other KMT2A abnormalities. These results are similar to those of previous reports [6,7,8]. The blasts of KMT2A-rearranged leukemia are commonly regarded as being derived from an immature precursor. In their converse correlation with stem cell marker CD34 expression, KMT2A-rearranged blasts are shown to be arrested at a very early stage of stem cell differentiation before CD34 expression. A recent study identified the presence of CD34− leukemia-initiating cells (LIC) in primary KMT2A-rearranged ALL samples [23], which may partly explain the clinical findings of the present study. Moreover, CD34+ patients had more favorable MRD at day 33 in our study and a good prognosis in other studies [24], which also supports this presumption.
In the present study, we also found that an extremely high rate (90%) of KMT2A-AFF1+ patients had CD133 and CD15 expression. CD133 is documented as a more specific marker of hematopoietic stem cells than CD34, and a marker of cancer stem cells (CSC) discovered in many tumors [25, 26]. Furthermore, Mak et al. [27] reported that AFF1 is a promoter of CD133 transcription and CD133 is required for KMT2A-AFF1+ leukemia cell survival. The correlation between CD15 expression and KMT2A-AFF1 has also been reported [6], but the potential mechanisms have still not been described. In addition, CD15+ patients in the present study were associated with high MRD at day 33 and day 78, indicating that the mechanism of CD15 expression in the KMT2A-AFF1 subset must be clarified in order to improve treatment for these patients.
NG2 was reported to be expressed in malignant hematopoietic cells and absent in normal hematopoietic cells, thus it could possibly be used as a marker for monitoring MRD and as a potential therapeutic target [28]. A recent study demonstrated that NG2 expression was associated with CNS disease and relapse in KMT2A-rearranged infant B-ALL [29]. Also, the combination of anti-NG2-specific monoclonal antibody and chemotherapy improved the prognosis of NSG mice [30]. In the present study, we also found a close association between NG2 expression and KMT2A rearrangements, which implies that anti-NG2 antibody may be a potential component in the combination treatment of KMT2A-rearranged patients.
In the prognostic analysis of the present study, CD20 expression was found to be associated with unfavorable outcomes in the pro-B-ALL cohort. Although the prognostic impact of CD20 expression on patients’ outcomes remains controversial [31,32,33,34,35,36,37,38], our data suggest that the combination of rituximab with current chemotherapy may be necessary for these patients. In addition, carrying KMT2A rearrangement and high MRD at day 78 were shown to be independent prognostic factors of pro-B-ALL in the present study. This emphasizes that genetic detection and MRD monitoring are essential in the prediction of patients’ prognosis. However, we noted that the EFS did not increase, even though we applied the high-risk chemotherapy regimen on KMT2A-rearranged patients and enhanced the treatment intensity based on MRD analysis in patients on the CCLG-2008 protocol. Thus, to further improve the treatment outcomes of pro-B-ALL patients, it appears to be necessary to apply new target drugs in combination with current therapy.
Conclusions
Results of the present study conducted in a large cohort of Chinese pediatric patients treated in a single institution confirm and extend previous reports of the heterogeneity of pro-B-ALL. Moreover, our results demonstrated the importance of genetic investigation and MRD monitoring in prognostic evaluation. However, conventional intensive chemotherapy alone did not improve patients’ long-term outcomes, thus further investigation is necessary to better elucidate the effects of combination therapy with targeted agents or HSCT for KMT2A-rearranged in a large cohort of high-risk patients.
Availability of data and materials
The datasets used and/or analyzed during this study are available from the corresponding authors on reasonable request.
Abbreviations
- Pro-B-ALL:
-
B cell precursor acute lymphoblastic leukemia
- CNS:
-
central nervous system
- MRD:
-
minimal residual disease
- EFS:
-
event free survival
- BCH-2003:
-
Beijing Children’s Hospital-2003
- CCLG-2008:
-
Chinese Childhood Leukemia Group-2008
- SR:
-
standard risk
- IR:
-
intermediate risk
- HR:
-
high risk
- EGIL:
-
European Group for the Immunological Characterization of Acute Leukemia
- FISH:
-
fluorescence in situ hybridization
- RT-PCR:
-
reverse transcription polymerase chain reaction
- HD-MTX:
-
high dose methotrexate
- CI:
-
confidence interval
- allo-HSCT:
-
allogeneic hematopoietic stem cell transplantation
- LIC:
-
leukemia initiating cell
- CSC:
-
cancer stem cell
References
European Group for the Immunological Characterization of Leukemias (EGIL), Bene MC, Castoldi G, Knapp W, et al. Proposals for the immunological classification of acute leukemias. Leukemia. 1995;9(10):1783–6.
Pui CH, Rivera GK, Hancock ML, et al. Clinical significance of CD10 expression in childhood acute lymphoblastic leukemia. Leukemia. 1993;7(1):35–40.
Cimino G, Elia L, Mancini M, et al. Clinico-biologic features and treatment outcome of adult pro-B-ALL patients enrolled in the GIMEMA 0496 study: absence of the ALL1/AF4 and of the BCR/ABL fusion genes correlates with a significantly better clinical outcome. Blood. 2003;102(6):2014–20.
Hoelzer D, Thiel E, Löffler H, et al. Prognostic factors in multicenter study for treatment of acute lymphoblastic leukemia in adults. Blood. 1988;71(1):123–31.
Attarbaschi A, Mann G, König M, et al. Mixed lineage leukemia-rearranged childhood pro-B and CD10-negative pre-B acute lymphoblastic leukemia constitute a distinct clinical entity. Clin Cancer Res. 2006;12(10):2988–94.
Schwartz S, Rieder H, Schläger B, et al. Expression of the human homologue of rat NG2 in adult acute lymphoblastic leukemia: close association with MLL rearrangement and a CD10(−)/CD24(−)/CD65s(+)/CD15(+) B-cell phenotype. Leukemia. 2003;17(8):1589–95.
Marks DI, Moorman AV, Chilton L, et al. The clinical characteristics, therapy and outcome of 85 adults with acute lymphoblastic leukemia and t(4;11)(q21;q23)/MLL-AFF1 prospectively treated in the UKALLXII/ECOG2993 trial. Haematologica. 2013;98(6):945–52.
Raponi S, De Propris MS, Intoppa S, et al. Flow cytometric study of potential target antigens (CD19, CD20, CD22, CD33) for antibody-based immunotherapy in acute lymphoblastic leukemia: analysis of 552 cases. Leuk Lymphoma. 2011;52(6):1098–107.
Campana D, Pui CH. Minimal residual disease-guided therapy in childhood acute lymphoblastic leukemia. Blood. 2017;129(14):1913–8.
Cui L, Li ZG, Chai YH, et al. Outcome of children with newly diagnosed acute lymphoblastic leukemia treated with CCLG-ALL 2008: the first nation-wide prospective multicenter study in China. Am J Hematol. 2018;93(7):913–20.
Gao C, Zhao XX, Li WJ, et al. Clinical features, early treatment responses, and outcomes of pediatric acute lymphoblastic leukemia in China with or without specific fusion transcripts: a single institutional study of 1004 patients. Am J Hematol. 2012;87(11):1022–7.
Gao C, Liu SG, Zhang RD, et al. NOTCH1 mutations are associated with favourable long-term prognosis in paediatric T-cell acute lymphoblastic leukaemia: a retrospective study of patients treated on BCH-2003 and CCLG-2008 protocol in China. Br J Haematol. 2014;166(2):221–8.
Gao C, Zhang RD, Liu SG, et al. Low CREBBP expression is associated with adverse long-term outcomes in paediatric acute lymphoblastic leukaemia. Eur J Haematol. 2017;99(2):150–9.
Pallisgaard N, Hokland P, Riishøj DC, et al. Multiplex reverse transcription-polymerase chain reaction for simultaneous screening of 29 translocations and chromosomal aberrations in acute leukemia. Blood. 1998;92(2):574–88.
Yue ZX, Huang C, Gao C, et al. MYCN amplification predicts poor prognosis based on interphase fluorescence in situ hybridization analysis of bone marrow cells in bone marrow metastases of neuroblastoma. Cancer Cell Int. 2017;31(17):43.
Campana D, Coustan-Smith E. Detection of minimal residual disease in acute leukemia by flow cytometry. Cytometry. 1999;38(4):139–52.
Coustan-Smith E, Sancho J, Hancock ML, et al. Clinical importance of minimal residual disease in childhood acute lymphoblastic leukemia. Blood. 2000;96(8):2691–6.
Ludwig WD, Rieder H, Bartram CR, et al. Immunophenotypic and genotypic features, clinical characteristics, and treatment outcome of adult pro-B acute lymphoblastic leukemia: results of the German multicenter trials GMALL 03/87 and 04/89. Blood. 1998;92(6):1898–909.
Burmeister T, Meyer C, Schwartz S, et al. The MLL recombinome of adult CD10-negative B-cell precursor acute lymphoblastic leukemia: results from the GMALL study group. Blood. 2009;113(17):4011–5.
Gleissner B, Goekbuget N, Rieder H, et al. CD10- pre-B acute lymphoblastic leukemia (ALL) is a distinct high-risk subgroup of adult ALL associated with a high frequency of MLL aberrations: results of the German Multicenter Trials for Adult ALL (GMALL). Blood. 2005;106(13):4054–6.
van der Linden MH, Valsecchi MG, De Lorenzo P, et al. Outcome of congenital acute lymphoblastic leukemia treated on the Interfant-99 protocol. Blood. 2009;114(18):3764–8.
Bueno C, Montes R, Catalina P, et al. Insights into the cellular origin and etiology of the infant pro-B acute lymphoblastic leukemia with MLL-AF4 rearrangement. Leukemia. 2011;25(3):400–10.
Aoki Y, Watanabe T, Saito Y, et al. Identification of CD34+ and CD34- leukemia-initiating cells in MLL-rearranged human acute lymphoblastic leukemia. Blood. 2015;125(6):967–80.
Jiang Z, Wu D, Lin S, et al. CD34 and CD38 are prognostic biomarkers for acute B lymphoblastic leukemia. Biomark Res. 2016;16(4):23.
Toren A, Bielorai B, Jacob-Hirsch J, et al. CD133-positive hematopoietic stem cell “stemness” genes contain many genes mutated or abnormally expressed in leukemia. Stem Cells. 2005;23(8):1142–53.
Hong D, Gupta R, Ancliff P, et al. Initiating and cancer-propagating cells in TEL-AML1-associated childhood leukemia. Science. 2008;319(5861):336–9.
Mak AB, Nixon AM, Moffat J, et al. The mixed lineage leukemia (MLL) fusion-associated gene AF4 promotes CD133 transcription. Cancer Res. 2012;72(8):1929–34.
Smith FO, Rauch C, Williams DE, et al. The human homologue of rat NG2, a chondroitin sulfate proteoglycan, is not expressed on the cell surface of normal hematopoietic cells but is expressed by acute myeloid leukemia blasts from poor-prognosis patients with abnormalities of chromosome band 11q23. Blood. 1996;87(3):1123–33.
Prieto C, López-Millán B, Roca-Ho H, et al. Correction: NG2 antigen is involved in leukemia invasiveness and central nervous system infiltration in MLL-rearranged infant B-ALL. Leukemia. 2018;32(10):2306.
Lopez-Millan B, Sanchéz-Martínez D, Roca-Ho H, et al. NG2 antigen is a therapeutic target for MLL-rearranged B-cell acute lymphoblastic leukemia. Leukemia. 2019. https://doi.org/10.1038/s41375-018-0353-0 (Epub ahead of print).
Esteban RE, Christianne B, Alvaro A, et al. Prognostic effect of CD20 expression in adult B-cell acute lymphoblastic leukemia. Clin Lymphoma Myeloma Leuk. 2018;18(5):361–7.
Yang S, Wang J, Zhao T, et al. CD20 expression sub-stratifies standard-risk patients with B cell precursor acute lymphoblastic leukemia. Oncotarget. 2017;8(62):105397–406.
Isshiki Y, Ohwada C, Sakaida E, et al. CD20 positivity and white blood cell count predict treatment outcomes in Philadelphia chromosome-negative acute lymphoblastic leukemia patients ineligible for pediatric-inspired chemotherapy. Jpn J Clin Oncol. 2017;47(11):1047–54.
Solano-Genesta M, Tarín-Arzaga L, Velasco-Ruiz I, et al. CD20 expression in B-cell precursor acute lymphoblastic leukemia is common in Mexicanpatients and lacks a prognostic value. Hematology. 2012;17(2):66–70.
Mannelli F, Gianfaldoni G, Intermesoli T, et al. CD20 expression has no prognostic role in Philadelphia-negative B-precursor acute lymphoblastic leukemia: new insights from the molecular study of minimal residual disease. Haematologica. 2012;97(4):568–71.
Bachanova V, Sandhu K, Yohe S, et al. Allogeneic hematopoietic stem cell transplantation overcomes the adverse prognostic impact of CD20 expression in acute lymphoblastic leukemia. Blood. 2011;117(19):5261–3.
Maury S, Huguet F, Leguay T, et al. Adverse prognostic significance of CD20 expression in adults with Philadelphia chromosome-negative B-cell precursor acute lymphoblastic leukemia. Haematologica. 2010;95(2):324–8.
Thomas DA, O’Brien S, Jorgensen JL, et al. Prognostic significance of CD20 expression in adults with de novo precursor B-lineage acute lymphoblastic leukemia. Blood. 2009;113(25):6330–7.
Acknowledgements
We gratefully thank all staff of the Hematology & Oncology Center of Beijing Children’s Hospital, Capital Medical University, for their help in sampling.
Funding
This work was partially supported by the National Natural Science Foundation of China (No. 81300432), Beijing Natural Science Foundation (No. 7192066), Major National Science and Technology Projects (No. 2017ZX09304029), Research on the application of clinical characteristics of the Beijing Municipal Science and Technology Commission (No. Z181100001718100).
Author information
Authors and Affiliations
Contributions
CG was the principal investigator and wrote the paper. SGL performed the experiments and analyzed the data. ZXY, YL, JL and JL performed some experiments. YYZ, JLY, YW, WL, and HYZ supplied the clinical data. RDZ reviewed the final manuscript and takes primary responsibility for the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was approved by the Beijing Children’s Hospital Institutional Ethics Committee. Signed informed consent was obtained from the parents or guardians of each patient according to the Declaration of Helsinki.
Consent for publication
All authors had full access to all of the data in the study and had final responsibility for the decision to submit for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Figure S1.
BCH-2003 and CCLG-2008 treatment protocol. (A) BCH-2003 treatment protocol. (B) CCLG-2008 treatment protocol. BCH, Beijing Children’s Hospital; CCLG, Chinese Childhood Leukemia Group; VDLP, vincristine, duanorubicin, l-asparaginase, prednisone; CAM, cyclophosphamide, cytarabine, 6-mercaptopurine; HD-MTX, high-dose methotrexate; VDLD, vincristine, daunorubicin, l-asparaginase, dexzmethasone; VD, vincristine, dexamethasone; IT, intrathecal injection with dexamethasone and methotrexate; VDLA, vincristine, cytarabine, l-asparaginase, dexamethasone; VM26, teniposide; HD-Ara-C, high-dose cytarabine; CA, cyclophosphamide, cytarabine; TIT, intrathecal injection with dexamethasone, methotrexate and cytarabine; I’, Berlin-Frankfürt-Münster (BFM) High Risk block-1’; II’, BFM High Risk block-2’; III’, BFM High Risk block-3’; TP1, minimal residual disease (MRD) time point 1 at the end of induction; TP2, MRD time point 2 before consolidation.
Additional file 2: Table S1.
Stratification criteria for BCH-2003 and CCLG-2008 treatment protocol. Table S2. Immunophenotyping Panel. Table S3. Immunophenotypic combinations used in MRD detection in B-ALL. Table S4. Incidence of fusion transcript of pro-B ALL. Table S5. Comparison of clinical features between KMT2A rearranged subgroups. Table S6. Expression frequency of immunological markers. Table S7. Correlation of immunological markers with clinical features of pro-B ALL. Table S8. Correlation of genetic abnormalities with immunological markers. Table S9. Associations between patient outcomes and clinical-biological characteristics. Table S10. Prognostic indicators of pro-B ALL without any fusion.
Additional file 3: Figure S2.
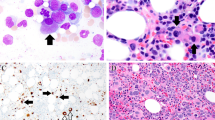
Immunophenotyping of a patient with pro-B ALL. Cells in the R2 region express: CD33, CD34, HLA-DR, CD19 and cyCD79a. Under the EGIL criteria, the immunophenotype is pro-B ALL with myeloid marker (CD33).
Additional file 4: Figure S3.
Representative FISH analysis of KMT2A rearrangement in a patient with pro-B ALL. KMT2A gene rearrangement is positive using a KMT2A break-apart probe.
Additional file 5: Figure S4.
Screening of immunophenotypic markers of minimal residual disease (MRD) monitoring of a patient with pro-B ALL. CyTdT, CD38, CD45, CD15, CD58, CD56, CD133 and NG2 were positive on the leukemic cells.
Additional file 6: Figure S5.
Event-free survival (EFS) for pediatric pro-B ALL without any fusion according to minimal residual disease (MRD). (A) EFS stratified by MRD at day 33. (B) EFS stratified by MRD at day 78.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gao, C., Liu, SG., Yue, ZX. et al. Clinical-biological characteristics and treatment outcomes of pediatric pro-B ALL patients enrolled in BCH-2003 and CCLG-2008 protocol: a study of 121 Chinese children. Cancer Cell Int 19, 293 (2019). https://doi.org/10.1186/s12935-019-1013-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-019-1013-9