Abstract
Background
Recently, some studies reported the prognostic value of platelet-to-lymphocyte ratio (PLR) in patients with diffuse large B-cell lymphoma (DLBCL), however, the results varied from different studies. Therefore, we performed a meta-analysis to explore the prognostic value of PLR in DLBCL.
Methods
A comprehensive literature retrieval was conducted by using PubMed, Embase, Web of Science, the Cochrane Library, the China National Knowledge Infrastructure (CNKI), and Wanfang. Pooled hazard ratio (HR) and 95% confidence interval (CI) were used to evaluate the association of PLR and overall survival (OS) and progression-free survival (PFS). Odd ratios (ORs) and 95% CIs for clinicopathological characteristics were statistically analyzed.
Results
Eight studies with 1931 patients were included for meta-analysis. The pooled analysis indicated that elevated PLR was significantly associated with poor OS (HR = 1.73, 95% CI 1.29–2.31, p < 0.001), but not PFS (HR = 0.85, 95% CI 0.57–1.27, p = 0.438). Furthermore, elevated PLR was significantly associated with presentation of B symptoms (OR = 2.27, 95% CI 1.29–3.98, p = 0.004), elevated lactate dehydrogenase (LDH) (OR = 2.76, 95% CI 2.05–3.72, p < 0.001), higher tumor stage (OR = 2.22, 95% CI 1.66–2.98, p < 0.001), and Eastern Cooperative Oncology Group (ECOG) performance status (PS) ≥ 2 (OR = 1.71, 95% CI 1.09–2.69, p = 0.019). However, elevated PLR was not significantly correlated with gender, age or cell of origin.
Conclusion
This meta-analysis revealed that PLR may be an effective and noninvasive biomarker for poor prognosis and aggressive disease characteristics for patients with DLBCL.
Similar content being viewed by others
Background
Diffuse large B-cell lymphoma (DLBCL) is the most frequent type of non-Hodgkin lymphoma, accounting for approximately 30–40% of all malignant lymphomas worldwide [1, 2]. DLBCL presents heterogeneous and aggressive status with different biological and clinical features [3]. Since rituximab (R)-cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) regimen became the standard treatment over the past decade, over 60% of DLBCL patients are curable, whereas approximately 30% of patients experience primary refractory or relapsed disease [4]. Prognostic biomarkers are important for survival prediction and therapeutic strategies selection. International prognostic index (IPI) is widely used for prognosis of DLBCL, however, the prognostic efficiency still needs to be improved [5]. Therefore, search of cost-effective and easily available prognostic markers is of high importance for DLBCL treatment.
Inflammatory responses are involved in different steps of cancer development [6]. Inflammation activity plays an important role in prognostication. The indexes derived from hematological parameters are investigated for prognosis of cancer patients in recent years. Platelet-to-lymphocyte ratio (PLR) is calculated as platelet counts divided by lymphocyte counts. PLR was shown to be a significant prognostic marker in various solid tumors including esophageal cancer [7], head and neck squamous cell carcinoma [8], ovarian cancer [9], and breast cancer [10]. Previous retrospective studies also explored the prognostic effect of PLR in DLBCL, whereas the results were inconsistent even contrary [11,12,13,14,15,16]. Therefore, it is necessary to conduct a meta-analysis to comprehensively evaluate the prognostic and clinicopathological role of PLR in DLBCL patients.
Materials and methods
Search strategy
We performed the present meta-analysis based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement [17]. The databases including PubMed, Web of Science, Cochrane Library, Embase, CNKI (Chinese), and Wanfang were searched for relevant studies. The search strategies included the combination of MeSH terms and free-text terms: “platelet-to-lymphocyte ratio,” “platelet–lymphocyte ratio,” “PLR,” and “diffuse large B-cell lymphoma or DLBCL”. The last search was up to May, 2019. In addition, the references list of relevant researches was examined to identify relevant studies. Ethical approval was not required for this study because all data were from previous published studies.
Selection criteria
The inclusion criteria were following: (1) patients with DLBCL were diagnosed histologically; (2) studies reported the prognostic role of PLR on overall survival (OS) or/and progression-free survival (PFS) or provided sufficient data for calculation [18]; (3) a cut-off value of PLR was identified; (4) studies were published in English or Chinese; (5) the laboratory parameters including the blood counts were assessed prior to the start of first chemotherapy cycle. Studies did not meet the inclusion criteria were removed.
Data extraction and quality evaluation
Two experienced investigators (Y.C. and Z.Z.) independently extracted the data. Any discrepancies were resolved by discussion with the third investigator (H.J.). The main characteristics of eligible studies were: name of first author, year of publication, country, sample size, patients’ age, gender, treatment regimen, stage, cut-off value of PLR, study period, and survival outcomes. The quality assessment of included studies were performed according to Newcastle–Ottawa Scale (NOS) [19]. The NOS consists of three parts: selection (0–4 points), comparability (0–2 points), and outcome (0–3 points). The studies of highest quality scored 9 points and studies ≥ 6 points indicated a high quality.
Statistical analysis
All statistical analyses were performed by using Stata version 12 (STATA, College Station, TX). Pooled hazard ratio (HR) and 95% confidence interval (CI) were used to evaluate the association of PLR and OS and PFS. HR and 95% CI were extracted from included studies if reported, or were calculated from Kaplan–Meier curves by Tierney’s method [18]. The heterogeneity across studies was assessed by Cochran’s Q test and I-squared test [20, 21]. A random-effect model was employed when the heterogeneity was significant (p < 0.10 or I2 > 50%), otherwise, a fixed model was applied. Odd ratios (ORs) and 95% CIs for clinicopathological characteristics were statistically analyzed. Sensitivity was performed by sequential omitting of each study to test the credibility of the results. The potential publication bias was examined by Begg’s funnel plot and Egger’s test. A two-tailed p-value < 0.05 was defined as statistically significant.
Results
Search results
A total of 49 studies were identified after initial literature search. After duplicate records were removed, 20 studies remained. Seven records were excluded by title/abstract screening and 13 studies were left for full-text evaluation. Five full-text articles were removed for reasons: no available data, not on PLR, and overlapped patients. At last, eight studies [11,12,13,14,15,16, 22, 23] were included in the current meta-analysis. The detailed process of literature retrieval was depicted in Fig. 1.
Study characteristics
The eight studies were published from 2015 to 2019. Six studies were conducted in China [12, 14,15,16, 22, 23], one in Austria [11] and one in Croatia [13]. Five studies were published in English [11, 13, 14, 16, 22] and three in Chinese [12, 15, 23]. The total sample size was 1931, ranging from 59 to 515. The cut-off values of PLR ranged from 143 to 435. Five studies [11,12,13, 16, 22] employed R-CHOP regimen and three studies [14, 15, 23] used R-CHOP/CHOP regimen. All eight studies [11,12,13,14,15,16, 22, 23] reported the prognostic value of PLR on OS and seven studies [12,13,14,15,16, 22, 23] showed the association of PLR and PFS. All included studies had a NOS score ≥ 6. The baseline characteristics of included studies were summarized in Table 1.
PLR and OS
All eight studies [11,12,13,14,15,16, 22, 23] with 1931 patients showed the correlation between PLR and OS. The random-effect model was used due to significant heterogeneity (Ph = 0.018, I2 = 58.6%; Table 2, Fig. 2). The pooled analysis showed that a high PLR was significantly correlated to worse OS (HR = 1.73, 95% CI 1.29–2.31, p < 0.001) (Fig. 2, Table 2). To yield a further investigation, the subgroup analyses were conducted. The pooled data indicated that PLR was still a significant prognostic marker in Asian patients (HR = 1.95, 95% CI 1.34–2.84, p < 0.001), in studies with sample size ≤ 200 (HR = 1.88, 95% CI 1.32–2.67, p < 0.001), in studies with sample size > 200 (HR = 1.63, 95% CI 1.09–2.45, p = 0.018), and cut-off > 150 (HR = 1.76, 95% CI 1.25–2.49, p = 0.001) (Table 2). However, the prognostic value was non-significant for PLR in Caucasian patients (HR = 1.32, 95% CI 0.95–1.84, p = 0.103) or cut-off value ≤ 150 (HR = 1.74, 95% CI 0.92–3.28, p = 0.088) (Table 2).
PLR and PFS
Seven studies [12,13,14,15,16, 22, 23] including 1416 patients reported the association of PLR and PFS. Because of significant heterogeneity (Ph < 0.001, I2 = 77.8%; Table 2, Fig. 3), a random-effect model was applied. The combined results were HR = 0.85, 95% CI 0.57–1.27, p = 0.438 (Table 2, Fig. 3), indicating that PLR was not a prognostic factor for PFS. Subgroup analysis demonstrated that PLR was not correlated to PFS irrespective of ethnicity, sample size, or cut-off value of PLR.
PLR and clinicopathological characteristics
The correlation of PLR and several clinicopathological characteristics were analyzed. The clinicopathological features included: B symptoms (yes vs no), lactate dehydrogenase (LDH) level (> normal vs < normal), tumor stage (III–IV vs I–II), gender (male vs female), age (≥ 60 vs < 60), Eastern Cooperative Oncology Group (ECOG) performance status (PS) (≥ 2 vs < 2), and cell of origin [germinal center B cell (GCB) vs non-GCB]. As shown in Table 3, the pooled analysis showed that PLR was significantly associated with presentation of B symptoms (OR = 2.27, 95% CI 1.29–3.98, p = 0.004), elevated LDH (OR = 2.76, 95% CI 2.05–3.72, p < 0.001), higher tumor stage (OR = 2.22, 95% CI 1.66–2.98, p < 0.001), and ECOG PS ≥ 2 (OR = 1.71, 95% CI 1.09–2.69, p = 0.019). However, PLR was not significantly correlated with gender, age or cell of origin.
Sensitivity analysis
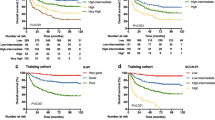
To evaluate the influence of each single study of the pooled results, sensitivity analysis was carried out. As shown in Fig. 4, the pooled HRs were not significantly altered by any individual study, which indicated the stability of the results.
Publication bias
The results of Begg’s funnel plot (OS, p = 0.536; PFS, p = 0.548) and Egger’s test (OS, p = 0.489; PFS, p = 0.808) indicated no publication bias in the present meta-analysis (Fig. 5).
Discussion
Inflammation plays a pivotal role in tumor progression [24]. PLR was widely investigated for prognosis of DLBCL patients with distinct results. Previous studies reported the prognostic value of PLR in DLBCL patients [11,12,13,14,15,16, 22, 23], whereas the results were inconsistent. For example, some studies [22, 23] demonstrated that PLR was a significant prognostic factor for DLBCL patients, whereas other studies failed to find the prognostic value of PLR [11, 13, 14]. As meta-analysis can aggregate data from a series of studies and make quantitative analysis, therefore, the results of meta-analysis are objective and credible.
In the present meta-analysis, we aggregated data from eight studies with 1931 patients to shed light on this issue. The results showed that a high PLR was a significant prognostic marker for poorer OS (HR = 1.73, 95% CI 1.29–2.31, p < 0.001). Furthermore, the prognostic efficiency enhanced for Asian patients (HR = 1.95, 95% CI 1.34–2.84, p < 0.001) and with a cut-off value > 150 (HR = 1.76, 95% CI 1.25–2.49, p = 0.001). However, PLR was not associated with PFS in DLBCL, regardless of ethnicity, sample size, or cut-off value of PLR. We also found that PLR was significantly correlated to presentation of B symptoms, elevated LDH, higher tumor stage, and ECOG PS ≥ 2. The results suggested that PLR was positively connected with clinical features reflecting high aggressiveness of the disease. Taken together, this study revealed that PLR was a significant prognostic factor for poor OS and invasiveness in DLBCL patients. To our knowledge, this is the first meta-analysis investigating the prognostic and clinicopathological value of PLR in DLBCL. Notably, the eight included studies are retrospective study design and recruited patients with one ethnicity. In the present meta-analysis, we collected the data and conducted subgroup analysis to investigate the prognostic value of PLR in different ethnicity, sample size, and cut-off values populations. We also investigated the correlation of PLR and clinical features with enlarged sample size compared with included studies. The current meta-analysis provides more comprehensive and systemic analysis than any single included study. Those factors were strengths of this meta-analysis.
Recent evidence suggests that inflammation response is involved in the processes of tumor angiogenesis, tumor growth, and metastasis [25]. However, the mechanism underlying the correlation between high PLR and poor prognosis in DLBCL patients has not been determined. The increasing of platelet counts and/or decreasing of lymphocyte counts can result in a high PLR. On the one hand, activated platelets were involved in early and advanced stages of tumor angiogenesis [26]. Platelets could secrete various biological molecules to facilitating angiogenesis in tumor microenvironment [27]. In addition, platelets derive transforming growth factor-β1 (TGF-β1), work together with the direct interaction of platelets and tumor cells to activate epithelial–mesenchymal transition (EMT) related pathways and induce subsequent metastasis [28]. On the other hand, lymphocytes exert critical roles in antitumor immune responses. Tumor-infiltrating lymphocytes (TILs) including CD3+ T cells, CD8+ T cells, Th1 CD4+ T cell could inhibit tumor cell proliferation and metastases [29, 30]. Therefore, it is reasonable to apply PLR as an easily available immunological parameter to predict survival outcomes in cancer patients.
Previous studies also demonstrated the prognostic value of PLR in various tumors [31]. A recent meta-analysis showed that a high NLR was significantly associated with decreased OS and PFS in ovarian cancer [9]. Another work suggested that higher PLR was an indicator of poor progress in oral cancer [32]. Those findings were in accordance with our results in DLBCL. In addition, in the present meta-analysis, we found that PLR was a significant prognostic factor for OS, especially in Asian patients and PLR > 150. Those results suggest that PLR may have enhanced prognostic role when the cut-off value > 150, which provides implications for clinical use. An elevated PLR was also correlated to aggressive tumor characteristics, which may imply that DLBCL patients with high PLR should be treated with strong therapeutic strategies. However, we did not observe significant prognostic impact of PLR on PFS, which may be explained by the relative short follow-up of PFS, compared to OS. In addition, the results suggested that cell of origin had non-significant association with PLR. However, because only two studies were included for analysis, which may lead to the negative results, therefore, more large-scale studies are still needed.
There are several limitations to this study. First, significant heterogeneity was observed in the analysis, although we applied random-effect model accordingly. Because the included studies recruited patients with different ethnicity, disease stage, cut-off values and treatment strategies, which could result in heterogeneity in the meta-analysis. The subgroup analysis showed that significant heterogeneity still exists in different sample size and cut-off values groups. These indicated that the heterogeneity could be inherent among included studies and various cut-off values may be a source of heterogeneity. According to the heterogeneity, we selected corresponding effects model (random effects model or fixed effects model) to pool the data. Second, the cut-off values of PLR were different in included studies, which may influence the distribution of low and high PLR groups and cause heterogeneity. Third, we only included studies published in English and Chinese, therefore, relevant studies published in other languages may be unavailable.
Conclusion
Our study shows that high PLR was a significant prognostic marker for poorer OS in DLBCL. Furthermore, PLR was associated with presentation of B symptoms, elevated LDH, higher tumor stage, and ECOG PS ≥ 2. Considering the above-mentioned limitations, large-scale prospective studies with uniform cut-off value of PLR are needed to validate our findings.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- CI:
-
confidence interval
- HR:
-
hazard ratio
- NOS:
-
Newcastle–Ottawa Scale
- OS:
-
overall survival
- PLR:
-
platelet-to-lymphocyte ratio
- PFS:
-
progression-free survival
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- DLBCL:
-
diffuse large B-cell lymphoma
- R-CHOP:
-
rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone
- LDH:
-
lactate dehydrogenase
- ECOG PS:
-
Eastern Cooperative Oncology Group performance status
References
Fuchs D. Diffuse large B-cell lymphoma. Memo-Mag Eur Med Oncol. 2019;12(1):7–11.
Li SY, Young KH, Medeiros LJ. Diffuse large B-cell lymphoma. Pathology. 2018;50(1):74–87.
Al-Hamadani M, Habermann TM, Cerhan JR, Macon WR, Maurer MJ, Go RS. Non-Hodgkin lymphoma subtype distribution, geodemographic patterns, and survival in the US: a longitudinal analysis of the National Cancer Data Base from 1998 to 2011. Am J Hematol. 2015;90(9):790–5.
Li S, Wang Z, Lin LM, Wu ZX, Yu QF, Gao FQ, et al. BCL6 rearrangement indicates poor prognosis in diffuse large B-cell lymphoma patients: a meta-analysis of cohort studies. J Cancer. 2019;10(2):530–8.
Miyazaki K. Treatment of diffuse large B-cell lymphoma. J Clin Exp Hematopathol. 2016;56(2):79–88.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99.
Deng JH, Zhang P, Sun Y, Peng P, Huang Y. Prognostic and clinicopathological significance of platelet to lymphocyte ratio in esophageal cancer: a meta-analysis. J Thorac Dis. 2018;10(3):1522.
Takenaka Y, Oya R, Kitamiura T, Ashida N, Shimizu K, Takemura K, et al. Platelet count and platelet–lymphocyte ratio as prognostic markers for head and neck squamous cell carcinoma: meta-analysis. Head Neck. 2018;40(12):2714–23.
Zhao Z, Zhao XR, Lu JJ, Xue J, Liu PS, Mao HL. Prognostic roles of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in ovarian cancer: a meta-analysis of retrospective studies. Arch Gynecol Obstet. 2018;297(4):849–57.
Zhang M, Huang XZ, Song YX, Gao P, Sun JX, Wang ZN. High platelet-to-lymphocyte ratio predicts poor prognosis and clinicopathological characteristics in patients with breast cancer: a meta-analysis. Biomed Res Int. 2017. https://doi.org/10.1155/2017/9503025.
Melchardt T, Troppan K, Weiss L, Hufnagl C, Neureiter D, Trankenschuh W, et al. Independent prognostic value of serum markers in diffuse large B-cell lymphoma in the era of the NCCN-IPI. J Natl Compr Cancer Netw. 2015;13(12):1501–8.
Ni J, Wang YQ, Zhang YP, Wu W, Zeng QS, Yang MZ, et al. Value of neutrophil/lymphocyte ratio and platelet/lymphocyte ratio for prognostic evaluation of diffuse large B-cell lymphoma. J Exp Hematol. 2016;24(2):427–32.
Periša V, Knezović A, Zibar L, Sinčić-Petričević J, Mjeda D, Periša I, et al. Comparison of the prognostic impact of neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, and glasgow prognostic score in diffuse large B-cell lymphoma. Shiraz E Med J. 2016;17(7–8):e38209.
Hao X, Wei Y, Wei X, Zhou L, Wei Q, Zhang Y, et al. Glasgow prognostic score is superior to other inflammation-based scores in predicting survival of diffuse large B-cell lymphoma. Oncotarget. 2017;8(44):76740–8.
Han Y, Qin Y, He X, Yang J, Liu P, Zhang C, et al. Prognostic significance of inflammatory indicators for advanced-stage diffuse large B-cell lymphoma. Natl Med J China. 2018;98(16):1250–5.
Wang S, Ma Y, Sun L, Shi Y, Jiang S, Yu K, et al. Prognostic significance of pretreatment neutrophil/lymphocyte ratio and platelet/lymphocyte ratio in patients with diffuse large B-cell lymphoma. Biomed Res Int. 2018;2018:9651254.
Moher D, Liberati A, Tetzlaff J, Altman DG, Grp P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Cochran W. The combination of estimates from different experiments. Biometrics. 1954;10:101–29.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Zhao P, Zang L, Zhang X, Chen Y, Yue Z, Yang H, et al. Novel prognostic scoring system for diffuse large B-cell lymphoma. Oncol Lett. 2018;15(4):5325–32.
Lin H, Xu Y, Chen F. Relationship between RDW, PLR and clinical features in patients with DLBCL and its impact on survival prognosis. J Clin Hematol. 2019;32(02):205–9.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Wojtukiewicz MZ, Sierko E, Hempel D, Tucker SC, Honn KV. Platelets and cancer angiogenesis nexus. Cancer Metastasis Rev. 2017;36(2):249–62.
Walsh TG, Metharom P, Berndt MC. The functional role of platelets in the regulation of angiogenesis. Platelets. 2015;26(3):199–211.
Labelle M, Begum S, Hynes RO. Direct signaling between platelets and cancer cells induces an epithelial–mesenchymal-like transition and promotes metastasis. Cancer Cell. 2011;20(5):576–90.
Kawai O, Ishii G, Kubota K, Murata Y, Naito Y, Mizuno T, et al. Predominant infiltration of macrophages and CD8(+) T cells in cancer nests is a significant predictor of survival in stage IV nonsmall cell lung cancer. Cancer. 2008;113(6):1387–95.
Rusakiewicz S, Semeraro M, Sarabi M, Desbois M, Locher C, Mendez R, et al. Immune infiltrates are prognostic factors in localized gastrointestinal stromal tumors. Cancer Res. 2013;73(12):3499–510.
Templeton AJ, Ace O, McNamara MG, Al-Mubarak M, Vera-Badillo FE, Hermanns T, et al. Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Cancer Epidemiol Biomark Prev. 2014;23(7):1204–12.
Zhang Y, Zheng L, Quan L, Du L. Prognostic role of platelet-to-lymphocyte ratio in oral cancer: a meta-analysis. J Oral Pathol Med. 2019. https://doi.org/10.1111/jop.12832.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception and design were by YC and ZZ. Provision of study materials was performed by QF. Collection and assembly of data were conducted by YC and ZZ. Data analysis and interpretation were done by YC, ZZ and HJ. Manuscript writing was performed by YC and HJ. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chen, Y., Zhang, Z., Fang, Q. et al. Prognostic impact of platelet-to-lymphocyte ratio on diffuse large B-cell lymphoma: a meta-analysis. Cancer Cell Int 19, 245 (2019). https://doi.org/10.1186/s12935-019-0962-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-019-0962-3