Abstract
Background
A series of studies has investigated the prognostic role and clinical significance of programmed death ligand 1 (PD-L1) in hepatocellular carcinoma (HCC). However, the results were inconsistent. We aimed to clarify the prognostic role of PD-L1 and relationship between PD-L1 expression and several important clinicopathological features.
Methods
PubMed, EMBASE and the Science Citation Index Expanded were systematically searched. All cohort or case–control studies comparing the prognosis and clinical features between the high PD-L1 and low PD-L1 groups were included. Publication bias was evaluated using funnel plots and Begg’s test. Subgroup analysis, sensitivity analysis and meta-regression analysis were performed.
Results
Seventeen studies including 2979 patients were eligible. The overall survival (OS) was not significantly different between the high and low PD-L1 groups (hazard ratio [HR]: 1.27; 95% confidence interval [CI] 0.98–1.65: P = 0.07) with significant heterogeneity (P < 0.001; I2 = 81%). The recurrence-free survival (RFS) was not significantly different between the high and low PD-L1 groups (HR: 1.22; 95% CI 0.97–1.53; P = 0.09) with significant heterogeneity (P < 0.001; I2 = 78%). The expression of PD-L1 was found to be significantly correlated with alpha-fetoprotein, hepatitis history, and tumour-infiltrating lymphocytes. Begg’s test found no significant publication bias for OS and RFS. Sensitivity analysis established the robustness of our results. Subgroup analysis and meta-regression analysis found the region of research as a significant contributor to inter-study heterogeneity in RFS, indicating some racial differences in the prognostic role of PD-L1.
Conclusions
Our study found no significant prognostic role of PD-L1 in HCC patients after potential curative hepatectomy based on our included studies. The expression of PD-L1 was significantly correlated with AFP, hepatitis history, and TILs. The prognostic role of PD-L1 in HCC warrants further investigation.
Similar content being viewed by others
Background
Hepatocellular carcinoma (HCC) remains one of the most common cancers worldwide. It is ranked as the fifth leading cancer and is the second leading cause of cancer-related mortality [1]. Despite great advances in the past decade, the long-term survival of HCC is low, considering that surgical resection of HCC is only applicable to a small proportion of patients and that the rate of tumour recurrence after surgery of curative intent is high.
The predominant risk factor for HCC in epidemic regions is hepatic inflammatory response following chronic hepatitis B virus (HBV) or hepatitis C virus (HCV) infection [2]. Evidence has suggested that chronic inflammation in the liver creates an immunosuppressive microenvironment that permits HCC tumourigenesis and progression, providing a rationale for targeting the dysregulated tumour microenvironment to improve HCC treatment [3]. Currently, most studies on the mechanisms of HCC immune evasion have focused on the programmed death receptor 1 (PD-1)/programmed death ligand 1 (PD-L1) pathway. PD-1 is an immunoinhibitory receptor expressed in activated T and B cells and natural killer T cells. PD-L1, the major ligand of PD-1, is expressed in various immune cells such as antigen-presenting cells, as well as in endothelial cells. PD-1/PD-L1 ligation suppresses the activation of immune cells as well as the production of certain cytokines such as IFN-γ, thereby inducing immune suppression and peripheral tolerance [4]. Cancer cells hijack this pathway by over-expressing PD-L1 via various mechanisms to protect themselves from the host immune response. Immunotherapies targeting PD-1/PD-L1 immune checkpoints have shown promising efficacy in different malignancies, including HCC [5]. However, the response rate of the PD-1 inhibitor in advanced HCC is far from satisfying [6]. An urgent need exists in the field to further understand the mechanisms of aberrant PD-1/PD-L1 signalling by which HCC forms an immune-evasive tumour microenvironment and for leveraging anti-PD1 immune checkpoint blockade therapies against HCC.
Data on the prognostic role of PD-L1 expression in HCC remain inconsistent. Some studies [7,8,9,10,11] and a meta-analysis [12] have shown that the expression of PD-L1 is correlated with a poor prognosis after hepatectomy, whereas other studies have reported non-homogeneous results [13,14,15]. To further clarify the prognostic role of PD-L1, the relationship of PD-L1 expression with several important clinicopathological features and tumour-infiltrating T lymphocytes, we conducted this meta-analysis.
Methods
Inclusion and exclusion criteria
The inclusion criteria were as follows: (i) study design: cohort studies or case–control studies; (ii) participants: all patients received potential curative hepatectomy for HBV-related HCC; (iii) group: immunohistochemical (IHC) assay of PD-L1 expression in tumour tissues (especially tumour cells); and (iv) sufficient information regarding the role of PD-L1 in recurrence-free survival (RFS) or overall survival (OS) of HCC and/or correlation with clinical features and tumour-infiltrating T lymphocytes (TILs).
The exclusion criteria were as follows: (i) abstracts, letters, editorials, expert opinions, reviews and meta-analyses lacking original data; (ii) studies including patients receiving other curative or palliative therapy (ablation, systemic chemotherapy, radiation, or transarterial chemoembolization) or transplantation; (iii) including data from other cancer types; (iv) other detection methods of PD-L1 expression (non-IHC assays such as ELISA, and/or investigating the expression of PD-L1 in peritumoural tissues or plasma other than tumour tissues).
Search strategy
PubMed, EMBASE and the Science Citation Index Expanded were searched without language restrictions (the most recent published report search date: December 20, 2018). The search terms used were “hepatocellular carcinoma” and “PD-L1”. The detailed search strategies are described in Additional file 1: Table S1. To identify relevant trials, we also searched the reference lists of related articles. Grey literature (reports and papers that were not published in PubMed, EMBASE and the Science Citation Index Expanded) were not included in this study.
Data collection and assessment of bias
Two authors (GML and XGL) independently extracted the data concerning the first author’s name, year of publication, country, clinicopathological features of included patients, expression pattern of PD-L1 (sample uses, detection method, cut-off value, positive or high expression rate of PD-L1), and outcomes (survival outcomes and adverse events). For studies including several subgroups, only patients without adjuvant therapy were included. For studies investigating PD-L1 in tumour cells or in immune cells separately, only data from tumour cells were included. When the data were not available in the published reports, additional information was retrieved via correspondence with the primary investigators. Any disagreement between the investigators was resolved via discussion.
Data pooling and analysis
Pair-wise meta-analyses were conducted using a random-effects models in consideration of inter-study heterogeneity. All analyses were performed using Review Manger 5.3 (Revman, the Cochrane Collaboration) and Stata V.12 software (StataCorp, College Station, Texas, USA) according to the recommendations of the Cochrane Handbook [16] and were reported in line with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement [17] (Additional file 2: Table S2). The prognostic role of PD-L1 was expressed as hazard ratios (HRs) and 95% confidence intervals (CIs) and was extracted using a spreadsheet developed by Tierney et al. [18]. ORs with 95% CIs were calculated to assess the correlation of PD-L1 expression with clinicopathological features and TILs. The between-study heterogeneity was assessed using Higgins’ I2 statistic. Publication bias was evaluated using funnel plots and Begg’s test. Subgroup analysis and sensitivity analysis by omitting one study in each turn were used to evaluate the reliability of the results. To evaluate the effects of covariates on the pooled estimates and heterogeneity across studies, meta-regression analysis was conducted with covariates including publication year, sample size, positive rate of PD-L1, region of research, proportion of males, proportion of HBV, proportion of single tumours, proportion of vascular invasion and proportion of poor differentiation. P < 0.05 was regarded as significant.
Results
Description of the studies
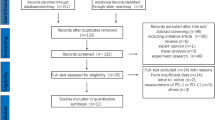
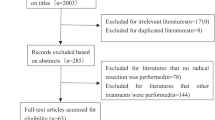
The literature searches identified 1754 potentially relevant records (Fig. 1). After excluding 683 duplicated studies, 1071 studies were screened by title and abstract. Thirty-six articles were left for full-text assessment for eligibility. Nineteen records were excluded due to insufficient data (n = 3), including patients receiving adjuvant postoperative therapy (n = 1), including patients receiving other curative or palliative therapy (n = 1), including data from other cancer type (n = 1), employing another detection method of PD-L1 (n = 6) and lacking original data (n = 7). Seventeen studies [7,8,9,10,11, 13,14,15, 19,20,21,22,23,24,25,26,27] including 2979 patients were eligible as listed in Table 1. Fifteen studies reported the effect of PD-L1 expression on overall survival [8,9,10,11, 13,14,15, 20,21,22,23,24,25,26,27], while 14 studies reported the effect of PD-L1 expression on recurrence-free survival [7,8,9, 13, 15, 19,20,21,22,23,24,25,26,27]. Detailed clinicopathological features and data on TILs are listed in Additional file 3: Table S3. Thirteen studies [7,8,9, 11, 13, 14, 20,21,22, 24,25,26,27] were conducted in Asia, whereas only four studies [10, 15, 19, 23] were performed in the USA and Europe. PD-L1 expression was characterized as positive or high in 938 patients with a positive ratio ranging from 16.7 to 82.9%.
Prognostic role of PD-L1 expression after hepatectomy for HCC
By pooling the data of 15 studies [8,9,10,11, 13,14,15, 20,21,22,23,24,25,26,27], the OS was not found to be significantly different between the high and low PD-L1 groups (HR: 1.27; 95% CI 0.98–1.65; P = 0.07) with significant heterogeneity (P < 0.001; I2 = 81%) (Fig. 2a).
By pooling the data of 14 studies [7,8,9, 13, 15, 19,20,21,22,23,24,25,26,27], the RFS was not found to be significantly different between the high and low PD-L1 groups (HR: 1.22; 95% CI 0.97–1.53; P = 0.09) with significant heterogeneity (P < 0.001; I2 = 78%) (Fig. 2b).
Correlation between PD-L1 expression and clinicopathological features
We elevated the correlation between PD-L1 expression and clinicopathological features using the OR and 95% CI (Table 2). At least three studies were included in the analyses. The clinicopathological features included age, gender, hepatitis history, AFP, tumour size, tumour stage, tumour differentiation, vascular invasion, tumour multiplicity, encapsulation, and liver cirrhosis. As shown in Fig. 3a, b, alpha-fetoprotein (AFP) and hepatitis history were found to be significantly correlated with the expression of PD-L1 (P = 0.04 and P = 0.04, respectively). No significant association was found between the expression of PD-L1 and other clinicopathological features above.
Correlation between PD-L1 expression and TILs
Limited data have shown the correlation between PD-L1 expression and TILs in our included studies. By pooling the data of four studies [7, 10, 15, 23], high PD-L1 expression was correlated with high CD8+ TILs (OR: 3.76; 95% CI 1.42–9.93; P = 0.008) with significant heterogeneity (P = 0.0005; I2 = 83%) (Fig. 3c). Gabrielson et al. reported that PD-L1 expression was correlated with high CD3+ TILs (OR: 3.95; 95% CI 1.20–13.06; P = 0.02). Chang et al. reported that PD-L1 expression was correlated with high PD1+ TILs (OR: 6.89; 95% CI 2.50–19.02; P = 0.0002).
Publication bias
Begg’s funnel plot was used to evaluate publication bias. As shown in Fig. 4a, b, the results showed no publication bias for OS and RFS, with P values of 1.000 and 0.728, respectively. Publication bias was not analysed for the correlation of PD-L1 expression and clinicopathological features or TILs because the number of included studies was less than 10 in most groups due to the low sensitivity of the qualitative and quantitative tests [28].
Subgroup analyses and sensitivity analysis
We conducted subgroup analyses according to publication year (before 2015 and after 2015), the origin of research (Asian and non-Asian), sample size (> 100 and < 100) and rate of positive or high PD-L1 (≤ 30% and > 30%). As shown in Fig. 5a, high PD-L1 was significantly correlated with poorer OS when combing data published before 2015, or with a sample size smaller than 100, or data from Asian populations, or studies reporting ≤ 30% of positive PD-L1. As shown in Fig. 5b, high PD-L1 was significantly correlated with poorer RFS when combining data published before 2015, or a cell membrane or cytoplasm PD-L1 staining pattern. Particularly, a significant difference was found in the prognostic role of PD-L1 between data from the Asian and non-Asian subgroups (P = 0.008). In the Asian subgroup, high PD-L1 indicated a significantly poor RFS (HR: 1.38; 95% CI 1.11–1.71; P = 0.003). However, in the non-Asian subgroup, high PD-L1 indicated an almost but not significant better RFS (HR: 0.44; 95% CI 0.19–0.99; P = 0.05). Additionally, the between-study heterogeneity was decreased to some degree in some subgroups. To further examine the robustness of the prognostic role of PD-L1 by sensitivity analyses, we applied a random effects model, omitting one study in each turn. No study exerted a significant influence on the overall pooling result, indicating that our estimates were robust and reliable (Fig. 5c–g, Additional file 4: Figure S1).
Results of subgroup analysis and sensitivity analysis. Forest plot of the subgroup analysis according to publication year (before 2015 and after 2015), origin of research (Asian and non-Asian), sample size (> 100 and < 100), and PD-L1 positive or high expression rate (< 30% and ≥ 30%) for the prognostic role of PD-L1 in a overall survival (OS) and b recurrence-free survival (RFS) in HCC. Sensitivity analysis revealed that no study exerted a significant influence on the overall pooling result of OS (c) and RFS (d). Sensitivity analysis revealed that no study exerted a significant influence on the overall pooling correlation of PD-L1 and AFP (e), hepatitis history (f), and CD8+ TILs (g). AFP alpha-fetoprotein, CI confidence interval, HR hazard ratio, OR odds ratio, PD-L1 programmed death ligand 1, HCC hepatocellular carcinoma, TIL tumour-infiltrating lymphocyte
Meta-regression analysis
For OS, meta-regression analysis showed a trend for a positive rate of PD-L1, region of research, proportion of male, proportion of HBV, proportion of single tumours, proportion of vascular invasion and proportion of poor differentiation, but the trend was not statistically significant (all P > 0.05, Fig. 6a–d, Additional file 5: Table S4). Given the significant heterogeneity in the overall effect estimates, the contribution of different study characteristics to the level of heterogeneity was calculated (Additional file 5: Table S4). No significant factors contributed to the level of heterogeneity, and the proportion of heterogeneity ranged from − 8.73% to 11.16% (all P > 0.05). The remaining heterogeneity was large (τ2 range from 0.187 to 0.628). For RFS, meta-regression analysis found that the region of research could explain 51.86% of the between-study variance (Fig. 6g, Additional file 5: Table S4, P 0.013). No other significant factors contributed to the level of heterogeneity, and the proportion of heterogeneity ranged from − 13.61% to 15.06% (all P > 0.05); the remaining heterogeneity was large (τ2 range from 0.172 to 0.407) (Fig. 6e, f, h; Additional file 5: Table S4). The meta-regression analysis categorized by age, AFP, proportion of cirrhosis, proportion of larger tumour size, proportion of tumour encapsulation, and TNM stage was not achieved and was attributed to the lack of data in the included studies.
Meta-regression analysis for overall survival and recurrence-free survival in HCC. Bubble plot with a fitted meta-regression line of the log hazard ratio for a, e publication year, b, f sample size, c, g region of research, and d, h positive rate of PD-L1 (%). a–d Represent overall survival; e–h represent recurrence-free survival. The size of circles is proportional to the weight of each study in the fitted random-effects meta-regression. PD-L1 programmed death ligand 1, HCC hepatocellular carcinoma
Discussion
While numerous studies have established that aberrant expression of PD-L1 in cancer promoted cancer immune escape and blockade of the PD-L1-enhanced anti-tumour response [4, 5], the prognostic role of PD-L1 in HCC has remained inconsistent. Several previous studies [8, 11, 21] and meta-analyses [29,30,31] have shown that high PD-L1 indicates a poorer OS and RFS, which could be explained by innate immune resistance. The innate immune resistance implies the constitutive expression of PD-L1, which is driven by intrinsic cellular oncological signalling in tumour cells and can lead to tumour-infiltrating immune cell inhibition [32, 33]. In this sense, PD-L1 expression reflects a lack of anti-tumour immunity and is reasonable to correlate with a significantly poorer prognosis [7,8,9,10,11, 21]. Meanwhile, a few recent studies failed to confirm the negative prognostic effect of PD-L1 and even showed the opposite [13,14,15, 23, 24]. For instance, Sideras et al. [15] reported that high PD-L1 in tumour cells indicated a significant better survival in HCC. The adaptive immune resistance was used to explain the inconsistency. The adaptive immune resistance implied a specific state of immune privilege of tumour cells acquired by the induced expression of PD-L1 to inhibit the pre-existing anti-tumour T cell response. The state can be reversed easily by blocking the PD1/PD-L1 interaction [34, 35]. From this point of view, the upregulation of PD-L1 represents the existence of immune-surveillance and could be correlated with a better prognosis [13,14,15]. Both mechanisms may co-exist, and the predominant mechanism may shift from one to the other at different times depending on the cancer immunogenicity [36]. The prognostic role of PD-L1 tends to be the combined effect of these two mechanisms. In the present meta-analysis based on 17 studies with 2979 patients, we found no significant prognostic role of PD-L1 in HCC after potential curative hepatectomy. Additionally, the expression of PD-L1 was correlated with AFP, hepatitis history, and CD8+ TILs but not with other clinicopathological features. The robustness and reliability of these results was further validated by sensitivity analysis.
Considering the significant between-study heterogeneity, we conducted further subgroup analysis and meta-regression analysis. High PD-L1 predicted a poorer RFS in Asian studies, while high PD-L1 predicted a better RFS in non-Asian patients; the difference between the subgroups was significant, and meta-regression analysis further confirmed the results. Together, these results indicated some racial differences in the prognostic role of PD-L1. Theoretically, several factors might also help explain the great heterogeneity. First, the positive rate of PD-L1 varied greatly across the included studies due to the different tested tissue samples, IHC assay, detection antibody, staining pattern, analytic method, and cut-off value. For instance, PD-L1 can be expressed in both tumour cells and immune cells in the intra-tumoural area of HCC tissues, with different biological and prognostic roles. As Liu et al. [27] reported, PD-L1 expressed on tumour cells was negatively correlated with the prognosis, while PD-L1 expressed on macrophages was positively correlated with the prognosis in HCC. Some included studies investigated the overall expression in the intra-tumoural area [10] or simply classified PD-L1 expression on tumour cells or immune cells by IHC [19]. Additionally, by combining the data published before 2015 or data including PD-L1 staining both in the cell membrane and/or cytoplasm, we found high PD-L1 significantly predicted a poorer survival. However, earlier studies might have used an invalid PD-L1 antibody [8, 11], while more recent studies utilized an antibody that distinguished between cytoplasmic and membranous patterns of PD-L1 staining [9, 15, 20, 22]. As a type I transmembrane molecule [37], membranous PD-L1 was proposed to be the most functionally relevant, and cytoplasmic staining represents intracellular stores of PD-L1 ready to be transported to the cell membrane with appropriate stimulation [38]. Failing to distinguish the expression pattern of PD-L1 in HCC can potentially confound the positive rate of PD-L1 and prognostic role of HCC. Moreover, the analytic method varied extensively. Some studies have utilized imaging software [7, 8, 10, 11, 13, 14, 19, 20, 22, 24], while others were based on intensity and distribution [9, 15, 21, 23]. Finally, the cut-off value used to evaluate high and low PD-L1 expression varied from 1 to 75%. Second, the different baseline characteristics of included patients and different follow-up periods might be another contributing factor. For example, the study of Calderaro et al. [19] only evaluated the prognostic role of PD-L1 in early recurrence within 2 years, while some other studies performed a significant longer follow up (both longer than 80 months) [21, 22]. However, our meta-regression analysis did not find a factor other than the region of research that significantly contributed to the level of heterogeneity, and the roles of the abovementioned factors warrant further investigation. Further studies should make great efforts to establish standardization regarding the methodology of PD-L1 assessment, such as the method to distinguish between tumour cells and immune cells, to distinguish between the expression patterns of PD-L1, to accurately calculate PD-L1 staining cells, and to set optimal cut-off values. Additionally, critical baseline patient characteristics such as AFP must be considered when estimating the prognostic role of PD-L1.
There have been several meta-analyses to date [12, 29, 31, 39,40,41,42,43]. Most recently, Li et al. [43] finished a similar meta-analysis on the value of PD-L1 in HCC patients. The major difference between our study might be the included criteria. Li et al. included all studies that examined PD-L1 expression levels in clinical HCC tissues. They included the study from Zeng et al. [44] that evaluated most of the PD-L1 expression using flow cytometry, but not IHC, and the study from Dai et al. [45] that assessed the PD-L1 expression in peritumoural tissues. Additionally, they included the study from Finkelmeier et al. [46] that investigated soluble PD-L1 in serum. As pointed out in a previous study, using data from different assays or different tissue types would inevitably raise the heterogeneity more or less [12]. Therefore, our meta-analysis focused on only the immunohistochemical (IHC) assay of PD-L1 expression in tumour tissues (or tumour cells but not immune cells in the intra-tumoural area) and found some inconsistent results with previous meta-analyses. Although our results should be explained with great caution, our study possessed some strengths. To our knowledge, the present study is the largest meta-analysis to date with subgroup and meta-regression analyses providing extended evidence regarding the inter-study heterogeneity issues.
Several limitations existed in our study. First, most of the included studies were retrospective and of questionable quality, and data from the prospective high-quality study were lacking. Second, significant between-study heterogeneity was found. Nevertheless, we conducted these meta-analyses using random-effect models, and sensitivity analysis confirmed the reliability of our results. Third, we could not evaluate the prognostic role of PD-L1 based on critical prognostic factors such as TNM stage or HCC causes because most studies did not report sufficient data. For example, as Huang et al. [20] reported, high PD-L1 expression was correlated with a high HBV viral load. How the causes of HCC, such as hepatitis C virus or alcohol, influence the expression and prognostic role of PD-L1 remain unclear. Finally, our analysis indicated some racial differences exist in the prognostic role of PD-L1. However, data from non-Asian patients were limited, and the prognostic role of PD-L1 in these patients warrants further investigation.
Conclusions
Despite the limitations listed above, our meta-analyses found no significant prognostic role of PD-L1 in HCC patients after potential curative hepatectomy based on the included studies. The expression of PD-L1 was significantly correlated with AFP, hepatitis history, and TIL. The prognostic role of PD-L1 in HCC warrants further investigation.
Abbreviations
- AFP:
-
alpha-fetoprotein
- CI:
-
confidence interval
- HBV:
-
hepatitis B virus
- HCC:
-
hepatocellular carcinoma
- HR:
-
hazard ratio
- IHC:
-
immunohistochemical
- OS:
-
overall survival
- OR:
-
odds ratio
- PD-L1:
-
programmed death ligand 1
- PD-1:
-
programmed death receptor 1
- RFS:
-
recurrence-free survival
- TNM:
-
tumour-node-metastasis
- TIL:
-
tumour-infiltrating T lymphocyte
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics 2012. CA: Cancer J Clin. 2015;65(2):87–108.
El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142(6):1264–73.
Makarovarusher OV, Medinaecheverz J, Duffy AG, Greten TF. The yin and yang of evasion and immune activation in HCC. J Hepatol. 2015;62(6):1420.
Keir ME, Butte MJ, Freeman GJ, Sharpe AH. PD-1 and its ligands in tolerance and immunity. Annu Rev Immunol. 2009;26(1):677–704.
Kudo M. Immune checkpoint inhibition in hepatocellular carcinoma: basics and ongoing clinical trials. Oncology. 2017;92(Suppl 1):50.
Melero I, Crocenzi TS, Welling TH, Yau TC, Yeo W, Chopra A, Grosso J, Lang L, Anderson J, Dela Cruz CM. Phase I/II safety and antitumor activity of nivolumab in patients with advanced hepatocellular carcinoma (HCC): CA209-040. J Clin Oncol. 2015;33(18_suppl):LBA101.
Chang H, Jung W, Kim A, Kim HK, Kim WB, Kim JH, Kim BH. Expression and prognostic significance of programmed death protein 1 and programmed death ligand-1, and cytotoxic T lymphocyte-associated molecule-4 in hepatocellular carcinoma. APMIS. 2017;125(8):690–8.
Gao Q, Wang XY, Qiu SJ, Yamato I, Sho M, Nakajima Y, Zhou J, Li BZ, Shi YH, Xiao YS, et al. Overexpression of PD-L1 significantly associates with tumor aggressiveness and postoperative recurrence in human hepatocellular carcinoma. Clin Cancer Res. 2009;15(3):971–9.
Jung HI, Jeong D, Ji S, Ahn TS, Bae SH, Chin S, Chung JC, Kim HC, Lee MS, Baek MJ. Overexpression of PD-L1 and PD-L2 is associated with poor prognosis in patients with hepatocellular carcinoma. Cancer Res Treat. 2017;49(1):246–54.
Semaan A, Dietrich D, Bergheim D, Dietrich J, Kalff JC, Branchi V, Matthaei H, Kristiansen G, Fischer HP, Goltz D. CXCL12 expression and PD-L1 expression serve as prognostic biomarkers in HCC and are induced by hypoxia. Virchows Archiv. 2017;470(2):185–96.
Wu K, Kryczek I, Chen L, Zou W, Welling TH. Kupffer cell suppression of CD8+ T cells in human hepatocellular carcinoma is mediated by B7-H1/programmed death-1 interactions. Can Res. 2009;69(20):8067–75.
Gu XB, Gao XS, Xiong W, Guo W, Han LJ, Bai Y, Peng C, Cui M, Xie M. Increased programmed death ligand-1 expression predicts poor prognosis in hepatocellular carcinoma patients. OncoTargets Ther. 2016;9:4805–13.
Chen CL, Pan QZ, Zhao JJ, Wang Y, Li YQ, Wang QJ, Pan K, Weng DS, Jiang SS, Tang Y, et al. PD-L1 expression as a predictive biomarker for cytokine-induced killer cell immunotherapy in patients with hepatocellular carcinoma. Oncoimmunology. 2016;5(7):e1176653.
Kan G, Dong W. The expression of PD-L1 APE1 and P53 in hepatocellular carcinoma and its relationship to clinical pathology. Eur Rev Med Pharmacol Sci. 2015;19(16):3063–71.
Sideras K, Biermann K, Verheij J, Takkenberg BR, Mancham S, Hansen BE, Schutz HM, de Man RA, Sprengers D, Buschow SI, et al. PD-L1, galectin-9 and CD8(+) tumor-infiltrating lymphocytes are associated with survival in hepatocellular carcinoma. Oncoimmunology. 2017;6(2):e1273309.
Higgins JPTGS, editor. Cochrane handbook for systematic reviews of interventions version 5.1.0. Oxford: The Cochrane Collaboration; 2011 (updated March 2011).
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Calderaro J, Rousseau B, Amaddeo G, Mercey M, Charpy C, Costentin C, Luciani A, Zafrani ES, Laurent A, Azoulay D, et al. PD-L1 expression in hepatocellular carcinoma: relationship with clinical and pathological features. Hepatology. 2016;64:624A.
Huang CY, Wang Y, Luo GY, Han F, Li YQ, Zhou ZG, Xu GL. Relationship between PD-L1 expression and CD8+ T-cell immune responses in hepatocellular carcinoma. J Immunother. 2017;40(9):323–33.
Umemoto Y, Okano S, Matsumoto Y, Nakagawara H, Matono R, Yoshiya S, Yamashita YI, Yoshizumi T, Ikegami T, Soejima Y, et al. Prognostic impact of programmed cell death 1 ligand 1 expression in human leukocyte antigen class I-positive hepatocellular carcinoma after curative hepatectomy. J Gastroenterol. 2014;50(1):65–75.
Chang B, Shen L, Wang K, Jin J, Huang T, Chen Q, Li W, Wu P. High number of PD-1 positive intratumoural lymphocytes predicts survival benefit of cytokine-induced killer cells for hepatocellular carcinoma patients. Liver Int. 2018;38(8):1449–58.
Gabrielson A, Wu YN, Wang HK, Jiang JJ, Kallakury B, Gatalica Z, Reddy S, Kleiner D, Fishbein T, Johnson L, et al. Intratumoral CD3 and CD8 T-cell densities associated with relapse-free survival in HCC. Cancer Immunol Res. 2016;4(5):419–30.
Xie QK, Zhao YJ, Pan T, Lyu N, Mu LW, Li SL, Shi MD, Zhang ZF, Zhou PH, Zhao M. Programmed death ligand 1 as an indicator of pre-existing adaptive immune responses in human hepatocellular carcinoma. Oncoimmunology. 2016;5(7):e1181252.
Dai X, Pi G, Yang SL, Chen GG, Liu LP, Dong HH. Association of PD-L1 and HIF-1α coexpression with poor prognosis in hepatocellular carcinoma. Transl Oncol. 2018;11(2):559–66.
Hu K, Wang ZM, Li JN, Zhang S, Xiao ZF, Tao YM. CLEC1B expression and PD-L1 expression predict clinical outcome in hepatocellular carcinoma with tumor hemorrhage. Transl Oncol. 2018;11(2):552–8.
Liu CQ, Xu J, Zhou ZG, Jin LL, Yu XJ, Xiao G, Lin J, Zhuang SM, Zhang YJ, Zheng L. Expression patterns of programmed death ligand 1 correlate with different microenvironments and patient prognosis in hepatocellular carcinoma. Br J Cancer. 2018;119(1):80–8.
Ioannidis JPA, Trikalinos TA. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ. 2007;176(8):1091–6.
Xiang X, Yu PC, Long D, Liao XL, Zhang S, You XM, Zhong JH, Li LQ. Prognostic value of PD-L1 expression in patients with primary solid tumors. Oncotarget. 2018;9(4):5058–72.
Wang X, Teng FF, Kong L, Yu JM. PD-L1 expression in human cancers and its association with clinical outcomes. OncoTargets Ther. 2016;9:5023–39.
Dai C, Wang M, Lu J, Dai ZM, Lin S, Yang PT, Tian T, Liu XH, Min WL, Dai ZJ. Prognostic and predictive values of PD-L1 expression in patients with digestive system cancer: a meta-analysis. OncoTargets Ther. 2017;10:3625–34.
Coelho MA, Trécesson SDC, Rana S, Zecchin D, Moore C, Molina-Arcas M, East P, Spencer-Dene B, Nye E, Barnouin K. Oncogenic RAS signaling promotes tumor immunoresistance by stabilizing PD-L1 mRNA. Immunity. 2017;47(6):1083–99.
Zhou J, Liu M, Sun H, Feng Y, Xu L, Chan AWH, Tong JH, Wong J, Chong CCN, Lai PBS, et al. Hepatoma-intrinsic CCRK inhibition diminishes myeloid-derived suppressor cell immunosuppression and enhances immune-checkpoint blockade efficacy. Gut. 2018;67(5):931–44.
Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJ, Robert L, Chmielowski B, Spasic M, Henry G, Ciobanu V. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515(7528):568.
Ribas A, Wolchok JD. Cancer immunotherapy using checkpoint blockade. Science. 2018;359(6382):1350–5.
Schumacher TN, Schreiber RD. Neoantigens in cancer immunotherapy. Science. 2015;348(6230):69–74.
Haynes D. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med. 1999;5(12):1365–9.
Taube JM, Anders RA, Young GD, Xu H, Sharma R, McMiller TL, Chen S, Klein AP, Pardoll DM, Topalian SL, et al. Colocalization of inflammatory response with B7-h1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Sci Transl Med. 2012;4(127):127ra137.
He J, Zhang Y, Kang S, Shen J, He J, Jiang L, Wang W, Guo Z, Peng G, Chen G, et al. Prognostic significance of programmed cell death 1 (PD-1) or PD-1 ligand 1 (PD-L1) expression in epithelial-originated cancer: a meta-analysis. Medicine. 2015;94(6):e515.
Pyo JS, Kang G, Kim JY. Prognostic role of PD-L1 in malignant solid tumors: a meta-analysis. Int J Biol Mark. 2017;32(1):e68–74.
Wang Q, Liu F, Liu L. Prognostic significance of PD-L1 in solid tumor: an updated meta-analysis. Medicine. 2017;96(18):e6369.
Zhong JH, Luo CP, Zhang CY, Li LQ. Strengthening the case that elevated levels of programmed death ligand 1 predict poor prognosis in hepatocellular carcinoma patients. J Hepatocell Carcinoma. 2017;4:11–3.
Li JH, Ma WJ, Wang GG, Jiang X, Chen X, Wu L, Liu ZS, Zeng XT, Zhou FL, Yuan YF. Clinicopathologic significance and prognostic value of programmed cell death ligand 1 (PD-L1) in patients with hepatocellular carcinoma: a meta-analysis. Front Immunol. 2018;9:2077. https://doi.org/10.3389/fimmu.2018.02077.
Zeng Z, Shi F, Zhou L, Zhang MN, Chen Y, Chang XJ, Lu YY, Bai WL, Qu JH, Wang CP, et al. Upregulation of circulating PD-L1/PD-1 is associated with poor post-cryoablation prognosis in patients with HBV-related hepatocellular carcinoma. PLoS ONE. 2011;6(9):e23621.
Dai XM, Xue J, Hu JL, Yang SL, Chen GG, Lai PBS, Yu C, Zeng C, Fang XF, Pan XL, et al. Positive expression of programmed death ligand 1 in peritumoral liver tissue is associated with poor survival after curative resection of hepatocellular carcinoma. Transl Oncol. 2017;10(4):511–7.
Finkelmeier F, Canli Ö, Tal A, Pleli T, Trojan J, Schmidt M, Kronenberger B, Zeuzem S, Piiper A, Greten FR, et al. High levels of the soluble programmed death-ligand (sPD-L1) identify hepatocellular carcinoma patients with a poor prognosis. Eur J Cancer. 2016;59:152–9.
Authors’ contributions
G-ML conceptualized the study, reviewed the literature, summarized and analysed the data and was a major contributor in the writing of the manuscript. X-GL and Y-MZ reviewed the literature, summarized and analysed the data and revised the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Data sharing is not applicable to this article because no datasets were generated or analysed during the current study.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
This work was supported by the Medical Scientific Research Foundation of Guangdong Province, China (2016102120351019).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1: Table S1.
Search strategy.
Additional file 2: Table S2.
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) checklist.
Additional file 3: Table S3.
Association of PD-L1 and clinicopathological features and tumour-infiltrating lymphocytes of the included studies.
Additional file 4: Figure S1.
Results of sensitivity analysis for the correlation of PD-L1 and several clinicopathological features. Sensitivity analysis revealed that no study exerted a significant influence on the overall pooling correlation of PD-L1 and gender (A), tumour differentiation (B), tumour stage (C), vascular invasion (D), tumour size (E), age (F), tumour multiplicity (G), cirrhosis (H), and tumour encapsulation (I). PD-L1: programmed death ligand 1; HCC, hepatocellular carcinoma.
Additional file 5: Table S4.
Meta-regression analysis for overall survival and recurrence-free survival.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Liu, GM., Li, XG. & Zhang, YM. Prognostic role of PD-L1 for HCC patients after potentially curative resection: a meta-analysis. Cancer Cell Int 19, 22 (2019). https://doi.org/10.1186/s12935-019-0738-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-019-0738-9