Abstract
Background
High triglyceride-glucose index (TyG) is a major risk factor for heart failure, but the long-term effect of high TyG index on the risk of developing heart failure remains unclear. Therefore, we aimed to determine the relationship between the cumulative exposure to TyG index and the risk of heart failure.
Methods
A total of 56,149 participants from the Kailuan Study, who participated in three consecutive health examinations in 2006, 2008, and 2010 and had no history of heart failure or cancer were recruited for this study. The cumulative TyG index was calculated as the weighted sum (value × time) of the mean TyG index for each time interval. The participants were placed into quartiles based on their cumulative TyG index. The study ended on December 31, 2020, and the primary outcome was new-onset heart failure during the follow-up period. In addition, a Cox proportional hazards regression model and a restricted cubic spline analysis were used to further evaluate the relationship between cumulative TyG index and the risk of heart failure.
Results
During a median follow-up period of 10.04 years, a total of 1,312 new heart failure events occurred. After adjustment for potential confounding factors, the Cox regression analysis showed that the hazard ratios (95% confidence intervals) for the risk of heart failure in the Q2, Q3, and Q4 groups were 1.02 (0.83,1.25), 1.29 (1.07,1.56) and 1.40 (1.15,1.71), respectively, vs. the Q1 group. The subgroup analysis showed a significant interaction between cumulative TyG index and BMI or waist circumference, but there was no interaction between age, sex and cumulative TyG index. The restricted cubic spline analysis showed a dose-response relationship between cumulative TyG index and the risk of heart failure. In addition, the sensitivity analysis generated results that were consistent with the primary results.
Conclusions
High cumulative TyG index is associated with a higher risk of heart failure. Thus, the TyG index may be useful for the identification of individuals at high risk of heart failure. The present findings emphasize the importance of the long-term monitoring of the TyG index in clinical practice.
Similar content being viewed by others
Background
Heart failure (HF) is a common disease worldwide, with high incidence and mortality rates [1]. The prevalence of heart failure in developed countries is estimated to be 1–2%, and the number of people with HF worldwide increased from 33.5 million in 1990 to 64.3 million in 2017 [2, 3]. The American Heart Association has stated that as the prevalence of HF continues to rise, the associated economic and social burdens increase. In China, the prevalence rate of HF rose from 0.9% to 2000 to 1.3% in 2015 [4], and this rise has placed an enormous burden on the national healthcare system. Therefore, the risk factors for HF should be better understood to implement effective preventive measures [5].
Insulin resistance (IR) is an important mechanism for the development of type 2 diabetes [6] and has been shown in numerous studies to be an independent risk factor for cardiovascular disease (CVD) [7, 8]. The hyperinsulinemic-euglycemic clamp technique is considered to be the gold-standard method for the evaluation of insulin resistance [9], but its implementation requires complex equipment and skilled personnel; and it is time-consuming, expensive, requires multiple blood samples, and is not readily accepted by patients. Therefore, it cannot be used on a large scale in clinical practice [10]. In contrast, the triglyceride-glucose index (TyG), a reliable alternative index of IR, can be calculated using only the patient’s fasting blood glucose (FBG) and fasting triglyceride (TG) concentrations [11, 12]. A number of recent studies have shown that high TyG index is positively associated with the risk of CVD, which includes myocardial infarction, stroke, and atherosclerosis [13,14,15], while others have shown that high TyG index is a risk factor for HF [16]. However, most previous studies of the relationship between TyG index and HF have used single measurements, and therefore information on the relationship between the long-term change in TyG index and the risk of HF is limited. Consequently, in the present study, we used a large community-based prospective cohort from the Kailuan study to evaluate the relationship of cumulative TyG index with HF.
Methods
Study population
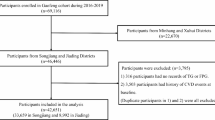
The Kailuan study is a large community-based prospective cohort study that is being conducted in Tangshan, China and aims to identify the risk factors for chronic non-communicable diseases. The research design and methods of the Kailuan study have been described previously [17, 18]. In brief, the Kailuan study started in 2006–2007, a total of 101,510 participants were recruited for the baseline survey, and they were followed up every 2 years. Comprehensive surveys were conducted on each occasion that comprised the completion of a questionnaire, a physical examination, and biochemical evaluation, including of FBG, and serum TG, high-density lipoprotein-cholesterol (HDL-C), and low-density lipoprotein-cholesterol (LDL-C). To date, eight rounds of health assessments have been completed. Participants who met the following conditions were included in the present study: (1) the completion of three health check-ups between 2006 and 2010; (2) complete data for blood glucose and TG from at least three check-ups; and (3) the provision of written informed consent. Participants with a history of HF or tumor prior to the third check-up (2010–2011) were excluded. Data from a total of 56,149 participants were ultimately included (Fig. 1). The study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Ethics Committee of Kailuan General Hospital (200,605).
Data collection and definitions
The participants completed the survey at 11 hospitals in Kailuan community. Trained staff used structured questionnaires to collect the demographic information (such as their age, sex, and education), medical history (such as of hypertension, diabetes, arrhythmia and myocardial infarction), and lifestyle factors (such as smoking status, alcohol consumption, and physical activity) of the participants, and their anthropometric measurements were reported previously [19].
Hypertension was defined as a systolic blood pressure (SBP) of ≥ 140 mmHg and/or diastolic blood pressure (DBP) of ≥ 90 mmHg, and/or a clear history of hypertension and/or the use of antihypertensive medication [20]. Diabetes was defined as a fasting plasma glucose (FPG) concentration of ≥ 7.0 mmol/L, and/or a clear history of diabetes, and/or the use of hypoglycemic drugs [21]. A normal waist circumference (WC) was defined as < 90 cm for men and < 80 cm for women [22]. Smoking and drinking habits were recorded as present or absent; physical activity was defined as exercising at least 4 times/week, with each session lasting at least 20 min; and body mass index (BMI) was calculated as body mass in kilograms divided by height in meters, squared.
Biochemical measurements and TyG index
Blood samples were collected after fasting for 8–12 h. On the day of the physical examination, 5 ml of venous blood was drawn from an elbow by a laboratory technician between 07:00 and 09:00 and analyzed using a Hitachi 747 automatic analyzer (Hitachi, Tokyo, Japan). The serum TC, HDL-C, LDL-C, FBG, TG, and high-sensitivity C-reactive protein (hs-CRP) concentrations were measured. Creatinine levels were measured by a creatine oxidase assay (Creatine Kit, BioSino BioTechnology and Science Inc, Beijing, China) [23]. Estimated glomerular filtration rate (eGFR) was calculated using the modified four-variable Chronic Kidney Disease Epidemiology Collaboration formula, with an adjustment factor of 1.1 for the Chinese population [24].
The TyG index was calculated as ln [TG (mg/dL) × FBG (mg/dL)/2] [25], and the cumulative TyG index (cumTyG) was calculated as the weighted sum of the mean TyG index values obtained at each visit as: (TyG index2006 + TyG index2008)/2 × time 1–2 + (TyG index2008 + TyG index2010)/2 × time 2–3, where the TyG index in 2006, TyG index in 2008, and TyG index in 2010 are the TyG indices calculated at the first, second, and third visits, respectively, and times 1–2 and 2–3 are the specific time intervals in years between consecutive examinations [26].
Assessment of heart failure
The health examination in 2010 was regarded as the start of the follow-up period and the first identification of an HF event was regarded as the endpoint of follow-up. An HF assessment was performed annually during the follow-up period. Potential HF was identified using hospital discharge summaries, death certificates, and social medical insurance records. The diagnostic criteria for HF were the Chronic Heart Failure Diagnosis Guidelines of the European Society of Cardiology [27]. The following conditions were identified by reviewing the participants’ medical records: (1) clinical symptoms of heart failure, including dyspnea, fatigue, fluid retention, New York Heart Association (NYHA) functional classification II, III, or IV, and Killip functional classification II, III, and IV; (2) left ventricular ejection fraction, measured on two-dimensional and Doppler echocardiography using the modified Simpson’s method, of ≤ 50%; and (3) high plasma natriuretic peptide (NT-proBNP) concentration. A diagnosis of HF was made if condition (1) and either condition (2) or condition (3) were fulfilled. For participants who experienced two or more episodes of HF, the timing and nature of the first episode were used as the outcomes; and for those who did not experience any HF events during the follow-up period, December 31, 2020 or the date of death was recorded as the endpoint, as appropriate.
Statistical analysis
Normally distributed continuous data are described as mean ± standard deviation, non-normally distributed continuous data are described as median and interquartile range, and categorical data are described using frequency and percentage. To compare the characteristics of the cumulative TyG index groups, the chi-square test was used for categorical data, and one-way ANOVA or the Kruskal–Wallis test was used for continuous data. The cumulative incidence was calculated using Kaplan–Meier method, and groups were compared using the log-rank test. Missing data for covariates were imputed using the multiple imputation method. The incidence density of the event is expressed as the number of events per 1,000 person-years, and was calculated by dividing the number of events by the total number of person-years of follow-up.
To evaluate the independent risk correlation between the cumulative TyG index and HF, multivariate Cox proportional hazards regression analysis was performed, with adjustment for age, sex, heart rate, WC, BMI, LDL-C, HDL-C, hs-CRP, eGFR, current smoking status (yes or no), current alcohol consumption (yes or no), physical activity status (yes or no), the presence of hypertension (yes or no), the presence of diabetes (yes or no), history of myocardial infarction (yes or no), history of arrhythmia (yes or no), the use of anti-hypertensive drugs (yes or no), the use of hypoglycemic drugs (yes or no), and the use of lipid-lowering drugs (yes or no). Subgroup analyses was performed after stratification of the participants by age (< 60 years vs. ≥60 years), sex (male vs. female), BMI (normal weight: <25 kg/m2vs. overweight or obesity: ≥25 kg/m2) [28] and WC (men < 90 cm or women < 80 cm vs. men ≥ 90 cm or women ≥ 80 cm). In addition, to evaluate the long-term risk of exposure to TyG index with respect to HF, we used the American College of Cardiology (ACC)/American Heart Association (AHA) model for the prediction of HF risk [29].
Finally, several sensitivity analyses were performed to test the robustness of the results. First, to account for the risk of reverse causality, participants who had experienced an HF event within the first year were excluded. Second, to account for the potential effect of the post-infarction condition on HF, participants with a history of myocardial infarction were excluded. Third, the incident HF analysis was repeated with the Fine-Gray model, considering death from non-HF as a competing risk [30]. Finally, to account for the effects of drug use on HF outcomes, three sensitivity analyses were performed separately with respect to the use of anti-hypertensive drugs, hypoglycemic agents, and lipid-lowering drugs. Statistical analyses were performed using SAS v.9.4 (SAS Institute, Inc, Cary, NC, USA). A two-sided P-value < 0.05 was considered to represent statistical significance.
Results
Baseline characteristics of the participants
A total of 57,927 participants attended all three of the medical examinations in 2006, 2008, and 2010. Of these, 1,149 individuals with missing FBG and TG data were excluded, as were 629 with a history of HF or cancer at the 2006 medical examination or who developed one of these between 2006 and 2010. Therefore, data from 56,149 participants were analyzed. These participants comprised 43,013 (76.6%) men and 13,136 (23.4%) women, with a mean age of 49.42 ± 11.93 years. The baseline characteristics of the participants, categorized according to the cumTyG quartile, are shown in Table 1. Compared with the lowest quartile group, participants with higher cumTyG indices were more likely to be male; were older; had lower eGFR; had higher BMI, SBP and DBP; had higher FBG, TG, LDL, and hs-CRP concentrations; and were more likely to have diabetes, hypertension, history of myocardial infarction and history of arrhythmia.
Relationship between cumulative TyG index and the risk of heart failure
During a median follow-up of 10.04 years (interquartile range, 9.70–10.32), 1,312 participants experienced HF events. According to the cumulative TyG quartiles, the incidences of HF in the Q1, Q2, Q3, and Q4 groups were 1.19, 1.57, 2.80, and 4.03 per 1,000 person-years, respectively (Table 2). The Kaplan–Meier curve showed that the incidence of HF gradually increased from the Q1 to the Q4 group. The cumulative incidence of HF in each group was significantly different among the groups (P < 0.01, Fig. 2), according to the log-rank test. After adjustment for potential confounding factors, the fully adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) in Model 4 for the Q2–Q4 groups vs. the Q1 group were 1.02 (0.83,1.25), 1.29 (1.07,1.56) and 1.40 (1.15,1.71), respectively. In addition, restricted cubic spline analysis showed that there was a dose-response relationship between the cumulative TyG index and the risk of HF (P for non-linearity = 0.0208) (Fig. 3).
The associations of cumTyG index with risk of heart failure
Caption: Cox regression models with restricted cubic splines were fitted to the data with 3 knots at the 25th, 50th and 75th percentiles of the cumTyG index. TyG index, triglycerides-glucose index, HR hazard ratio, CI confidence interval. The solid line represents the point estimate of cumTyG index correlation with the risk of heart failure, and the shaded part represents the 95% CI estimate. Covariates in the model include age, sex, heart rate, HDL-C, LDL-C, WC, hs-CRP, eGFR, current smoker, current drinker, physical activity, hypertension, diabetes mellitus, history of myocardial infarction, history of arrhythmia, hypoglycemic drugs, anti-hypertensive drugs, lipid-lowering drugs and the TyG index2010 at baseline
Relationship between baseline TyG index and the risk of heart failure
The incident rate presented an increas-ing trend in four groups divided by the quartiles of baseline TyG index, which were 1.57, 2.00, 2.69, and 3.21 per 1000 person-years, respectively (Additional file 1, Table S1). The Kaplan–Meier curve showed that the incidence of HF gradually increased from the Q1 to the Q4 group. The cumulative incidence of HF in each group was significantly different among the groups (P < 0.01) (Additional File 2, Fig. S1), according to the log-rank test. After adjustment for potential confounding factors, the fully adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) in Model 3 for the Q2–Q4 groups vs. the Q1 group were 1.08 (0.91,1.30), 1.23 (1.04,1.46) and 1.24 (1.04,1.47), respectively.
Results of the subgroup and sensitivity analyses
The relationship between the cumulative TyG index and HF was stratified according to age, sex, BMI, and WC (Table 3), and we found a significant interaction between cumulative TyG index and both BMI and WC, but not between age, sex and cumulative TyG index. The sensitivity analysis, in which we adjusted for covariates and excluded participants who experienced an HF event within 1 year and those with a history of myocardial infarction (Additional file 1, Tables S2 and S3), generated results that were consistent with the main findings. Considering the competing risks of non-heart failure death, we used the Fine-Gray model to assess the association of cumulative TyG index with new-onset heart failure, and the results remained stable (Additional file 1, Table S4). Furthermore, the results were unaffected by the exclusion of participants who were using anti-hypertensive drugs, hypoglycemic drugs, and lipid-lowering drugs (Additional file 1, Table S5).
Incremental predictive value of the change in the cumTyG index
In turn, we added TyG index2006, TyG index2010, and cumTyG to the original ACC/AHA prediction model and evaluated its efficacy. Of these, the addition of cumTyG was associated with the highest predictive value for the risk of HF, with a C-index of 76.13%, compared with the original ACC/AHA prediction model (C-index of 75.93%), the 2006 prediction model (C-index of 76.04%), and the 2010 prediction model (C-index of 76.01%), its C-indexes were 0.2%, 0.09%, and 0.12% higher, respectively, and the continuous NRIs were 25.37%, 10.72%, and 17.61% higher, respectively (Additional file 1, Table S6).
Discussion
The main finding of the present study is that a high cumulative TyG index is a risk factor for new-onset HF. A high cumulative TyG index increases the risk of heart failure development independently of traditional risk factors and exhibits a dose-response relationship. In addition, the risk of HF is BMI- and WC-dependent, such that individuals with a normal BMI and with a normal WC have a higher risk of developing HF. Compared with single TyG index, cumulative TyG index is more likely to be a better predictor of the risk of HF.
We found that cumulative exposure to a high TyG index is an independent risk factor for new-onset HF. In previous studies of the relationship between TyG index and the risk of HF, similar conclusions have been reached. In a prospective study of 138,620 participants, Xu et al. [31]. found that after a median follow-up of 8.78 years, the risk of HF was 24% higher in those with the highest quartile of TyG index than in those with the lowest quartile. Similarly, Li et al. [32]. analyzed 95,996 and 19,345 participants in the Kailuan and Hong Kong cohort studies, and found that a higher TyG index was an independent risk factor for the risk of HF in the general population, with the risk of HF being 22% higher in the highest quartile of TyG index than in the lowest quartile. However, in these studies, TyG was measured once, and therefore the change in TyG over time was not assessed. In the present study, we found that participants with a high cumulative TyG index are at a higher risk of HF and that those in the highest quartile group are at the highest risk, with a multifactor-adjusted HR (95% CI) of 1.40 (1.15,1.71), and therefore cumulative exposure to a high TyG index may be associated with a higher risk of HF than a single exposure. In the present study, we evaluated the effect of a 6-year TyG index assessment on HF, and generated more reliable results.
We also found that the risk of HF is bmi- and waist circumference-dependent. The association between the cumulative TyG index and the risk of HF appears to be stronger in normal BMI, normal waist circumferences. Previous studies have found that individuals with a normal BMI or WC and metabolic abnormalities tend to have a higher risk of cardiovascular disease, which may be the reason why a high TyG index in the normal BMI or WC group leads to a higher risk of heart failure than in the large BMI or WC group [33]. In contrast, in individuals with a large BMI or WC, other risk factors, such as abnormal blood lipid concentrations, may mask the effects of TyG index on the risk of HF [34, 35]. Thus, in summary, exposure to high TyG index is associated with a higher risk of HF in individuals with normal BMI or WC.
This study also found that high baseline tyg index was associated with a higher risk of heart failure, and participants in the highest quartile had the highest risk of heart failure, with a multivariate adjusted HR (95%CI) of 1.24 (1.04,1.47). However, compared with the high cumulative TyG index, baseline high TyG exposure may have a lower risk of heart failure than high cumulative exposure to TyG. In addition, previous cohort studies have shown that the cumulative exposure to risk factors such as TyG index, blood pressure, and adverse lipid profile have more marked effects on outcomes such as cardiovascular disease than a single exposure [36,37,38], which is consistent with the present findings. We constructed HF risk prediction models that incorporated conventional risk factors and the cumTyG or TyG in 2006 or 2010, and found that the predictive ability of the first was significantly better than those that included single TyG values, which suggests that cumTyG may be a better predictor of the risk of HF.
The mechanisms underpinning the long-term changes in TyG index and its relationship with the risk of HF are not yet clear; IR is likely to be involved. IR increases the risk of many chronic metabolic diseases, such as hypertension, diabetes mellitus, and dyslipidemia, which happen to be risk factors for heart failure [39, 40], and the combined effects of IR and these conditions may further increase the risk of HF. In addition, some previous pathophysiological findings may also explain the relationship between IR and HF. For example, a previous meta-analysis suggested that sodium retention, sympathetic nervous system activation, hyperinsulinemia, IR-related metabolic alterations, and greater sensitivity to angiotensin II may be involved; that higher IR is associated with higher risk of HF; and that there may be a causal relationship between IR and HF, according to the results of a Mendelian randomization study [41,42,43]. Finally, further evidence of the connection between IR and HF lies in the association between IR and structural abnormalities of the heart, such as left ventricular hypertrophy and greater left ventricular mass, which are associated with a higher risk of developing diastolic HF [44, 45].
The present findings have important clinical implications. IR is a major risk factor for cardiovascular events, including HF, but the gold-standard methods for the assessment of IR are the hyperinsulinemic-euglycemic clamp and the homeostatic model assessment of insulin resistance (HOMA-IR) [46], which are difficult to use in clinical and epidemiological investigations. However, the TyG index, as a reliable alternative marker of IR, is easy to calculate in a clinical setting and is highly sensitive and cheap. Furthermore, the use of electronic medical records has made cumTyG easily accessible, and therefore readily applicable for use as a means of identifying individuals at high risk of HF in the general population.
The principal strength of the present study is that it was a large prospective cohort study with a long follow-up period. The relationship between cumTyG and the risk of HF was investigated by monitoring the long-term changes in TyG index. In addition, we performed subgroup and sensitivity analyses with adjustment for confounding factors, which has rendered the findings more reliable. However, the study also had certain limitations. First, although we adjusted for most potential confounding factors, some residual or unmeasured confounding factors that could have affected the results may remain. In addition, the majority of participants in our study were male coal miners, with female participants being underrepresented. Therefore, these findings may not be directly generalizable to other populations, there is still a need to further validate our results in the future in areas where there is a balanced representation of women and men. Last but not least, because we did not measure IR, such as by calculating HOMA-IR, we could not compare the differential effects of IR and TyG index on the risk of HF. Therefore, further studies are needed to compare the predictive values of the TyG index and HOMA-IR with respect to the risk of HF.
Conclusions
People with a high cumulative TyG index are at a higher risk of developing HF. This simple index may assist with the early identification of individuals who are at high risk of HF, and the present findings emphasize the importance of the long-term monitoring of TyG index in clinical practice.
Data Availability
The datasets used and/or analyzed during the present study are available from.
the corresponding author on reasonable request.
Abbreviations
- TyG index:
-
Triglyceride-glucose index
- IR:
-
Insulin resistance
- HF:
-
Heart failure
- CVD:
-
Cardiovascular disease
- TG:
-
Triglyceride
- FBG:
-
Fasting blood glucose
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- BMI:
-
Body mass index
- TC:
-
Total cholesterol
- HDL-C:
-
High-density lipoprotein-cholesterol
- LDL-C:
-
Low-density lipoprotein-cholesterol
- hsCRP:
-
High-sensitivity C-reactive protein
- eGFR:
-
Estimated glomerular filtration rate
- HR:
-
Hazard ratio
- CI:
-
Confidence interval. RCS:Restricted cubic spline
References
Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat Rev Cardiol. 2016;13(6):368–78.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Bragazzi NL, Zhong W, Shu J, Abu Much A, Lotan D, Grupper A, Younis A, Dai H. Burden of heart failure and underlying causes in 195 countries and territories from 1990 to 2017. Eur J Prev Cardiol. 2021;28(15):1682–90.
Wang H, Chai K, Du M, Wang S, Cai JP, Li Y, Zeng P, Zhu W, Zhan S, Yang J. Prevalence and incidence of heart failure among urban patients in China: A National Population-Based analysis. Circ Heart Fail. 2021;14(10):e008406.
Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–44.
Gerich JE. Contributions of insulin-resistance and insulin-secretory defects to the pathogenesis of type 2 diabetes mellitus. Mayo Clin Proc. 2003;78(4):447–56.
Laakso M, Kuusisto J. Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat Rev Endocrinol. 2014;10(5):293–302.
Hanley AJ, Williams K, Stern MP, Haffner SM. Homeostasis model assessment of insulin resistance in relation to the incidence of cardiovascular disease: the San Antonio Heart Study. Diabetes Care. 2002;25(7):1177–84.
DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237(3):E214–223.
Muniyappa R, Lee S, Chen H, Quon MJ. Current approaches for assessing insulin sensitivity and resistance in vivo: advantages, limitations, and appropriate usage. Am J Physiol Endocrinol Metab. 2008;294(1):E15–26.
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6(4):299–304.
Abbasi F, Reaven GM. Comparison of two methods using plasma triglyceride concentration as a surrogate estimate of insulin action in nondiabetic subjects: triglycerides × glucose versus triglyceride/high-density lipoprotein cholesterol. Metabolism. 2011;60(12):1673–6.
Zhao Y, Sun H, Zhang W, Xi Y, Shi X, Yang Y, Lu J, Zhang M, Sun L, Hu D. Elevated triglyceride-glucose index predicts risk of incident ischaemic stroke: the rural chinese cohort study. Diabetes Metab. 2021;47(4):101246.
Tian X, Zuo Y, Chen S, Liu Q, Tao B, Wu S, Wang A. Triglyceride-glucose index is associated with the risk of myocardial infarction: an 11-year prospective study in the Kailuan cohort. Cardiovasc Diabetol. 2021;20(1):19.
Wu S, Xu L, Wu M, Chen S, Wang Y, Tian Y. Association between triglyceride-glucose index and risk of arterial stiffness: a cohort study. Cardiovasc Diabetol. 2021;20(1):146.
Guo W, Zhao L, Mo F, Peng C, Li L, Xu Y, Guo W, Sun A, Yan H, Wang L. The prognostic value of the triglyceride glucose index in patients with chronic heart failure and type 2 diabetes: a retrospective cohort study. Diabetes Res Clin Pract. 2021;177:108786.
Huang Z, Chen Z, Wang X, Ding X, Cai Z, Li W, Cai Z, Lan Y, Chen G, Fang W, et al. Association of Cardiovascular Health score trajectory with Incident Myocardial Infarction in Hypertensive Patients. Hypertension. 2022;79(11):2622–30.
Huang Z, Ding X, Yue Q, Wang X, Chen Z, Cai Z, Li W, Cai Z, Chen G, Lan Y, et al. Triglyceride-glucose index trajectory and stroke incidence in patients with hypertension: a prospective cohort study. Cardiovasc Diabetol. 2022;21(1):141.
Wang L, Lee Y, Wu Y, Zhang X, Jin C, Huang Z, Wang Y, Wang Z, Kris-Etherton P, Wu S, et al. A prospective study of waist circumference trajectories and incident cardiovascular disease in China: the Kailuan Cohort Study. Am J Clin Nutr. 2021;113(2):338–47.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, et al. The Seventh Report of the Joint National Committee on Prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72.
Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J, Knowler WC, Lebovitz H, Lernmark A, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26(11):3160–7.
Alberti KG, Zimmet P, Shaw J. The metabolic syndrome–a new worldwide definition. Lancet. 2005;366(9491):1059–62.
Ma C, Gurol ME, Huang Z, Lichtenstein AH, Wang X, Wang Y, Neumann S, Wu S, Gao X. Low-density lipoprotein cholesterol and risk of intracerebral hemorrhage: a prospective study. Neurology. 2019;93(5):e445–57.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Ramdas Nayak VK, Satheesh P, Shenoy MT, Kalra S. Triglyceride glucose (TyG) index: a surrogate biomarker of insulin resistance. J Pak Med Assoc. 2022;72(5):986–8.
Liu S, Zhao D, Wang M, Qi Y, Sun JY, Liu J, Li Y, Liu J. Association between cumulative blood pressure and long-term risk of cardiovascular disease: findings from the 26-year chinese multi-provincial cohort Study-Beijing Project. Chin Med J (Engl). 2021;134(8):920–6.
Swedberg K, Cleland J, Dargie H, Drexler H, Follath F, Komajda M, Tavazzi L, Smiseth OA, Gavazzi A, Haverich A, et al. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): the Task Force for the diagnosis and treatment of Chronic Heart failure of the European Society of Cardiology. Eur Heart J. 2005;26(11):1115–40.
Lin YP, Hsu YC, Tsai KZ, Kwon Y, Lin GM. Insulin resistance indices and carotid intima-media thickness in physically fit adults: CHIEF atherosclerosis study. Endocr Metab Immune Disord Drug Targets 2023.
Arshi B, van den Berge JC, van Dijk B, Deckers JW, Ikram MA, Kavousi M. Implications of the ACC/AHA risk score for prediction of heart failure: the Rotterdam Study. BMC Med. 2021;19(1):43.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509.
Xu L, Wu M, Chen S, Yang Y, Wang Y, Wu S, Tian Y. Triglyceride-glucose index associates with incident heart failure: a cohort study. Diabetes Metab. 2022;48(6):101365.
Li X, Chan JSK, Guan B, Peng S, Wu X, Lu X, Zhou J, Hui JMH, Lee YHA, Satti DI, et al. Triglyceride-glucose index and the risk of heart failure: evidence from two large cohorts and a mendelian randomization analysis. Cardiovasc Diabetol. 2022;21(1):229.
Fan J, Song Y, Chen Y, Hui R, Zhang W. Combined effect of obesity and cardio-metabolic abnormality on the risk of cardiovascular disease: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;168(5):4761–8.
Clark AL, Fonarow GC, Horwich TB. Waist circumference, body mass index, and survival in systolic heart failure: the obesity paradox revisited. J Card Fail. 2011;17(5):374–80.
Rauchhaus M, Coats AJ, Anker SD. The endotoxin-lipoprotein hypothesis. Lancet. 2000;356(9233):930–3.
Tai S, Fu L, Zhang N, Yang R, Zhou Y, Xing Z, Wang Y, Zhou S. Association of the cumulative triglyceride-glucose index with major adverse cardiovascular events in patients with type 2 diabetes. Cardiovasc Diabetol. 2022;21(1):161.
Wang J, Zhang S, Jiao Y, Zheng L, Sun Y, Sun Z. Cumulative exposure to elevated blood pressure better predicts cardiovascular disease risk in rural chinese adults. Front Public Health. 2022;10:1006220.
Dai L, Xu J, Zhang Y, Wang A, Chen Z, Mo J, Li H, Meng X, Wu S, Wang Y. Cumulative burden of lipid profiles predict future incidence of ischaemic stroke and residual risk. Stroke Vasc Neurol. 2021;6(4):581–8.
Reaven GM. The insulin resistance syndrome. Curr Atheroscler Rep. 2003;5(5):364–71.
Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93(9):1137–46.
Erqou S, Adler AI, Challa AA, Fonarow GC, Echouffo-Tcheugui JB. Insulin resistance and incident heart failure: a meta-analysis. Eur J Heart Fail. 2022;24(6):1139–41.
Aroor AR, Mandavia CH, Sowers JR. Insulin resistance and heart failure: molecular mechanisms. Heart Fail Clin. 2012;8(4):609–17.
Mordi IR, Lumbers RT, Palmer CNA, Pearson ER, Sattar N, Holmes MV, Lang CC. Type 2 diabetes, metabolic traits, and risk of Heart failure: a mendelian randomization study. Diabetes Care. 2021;44(7):1699–705.
Verdecchia P, Reboldi G, Schillaci G, Borgioni C, Ciucci A, Telera MP, Santeusanio F, Porcellati C, Brunetti P. Circulating insulin and insulin growth factor-1 are independent determinants of left ventricular mass and geometry in essential hypertension. Circulation. 1999;100(17):1802–7.
Pagé A, Dumesnil JG, Clavel MA, Chan KL, Teo KK, Tam JW, Mathieu P, Després JP, Pibarot P. Metabolic syndrome is associated with more pronounced impairment of left ventricle geometry and function in patients with calcific aortic stenosis: a substudy of the ASTRONOMER (aortic stenosis Progression Observation Measuring Effects of Rosuvastatin). J Am Coll Cardiol. 2010;55(17):1867–74.
Vardeny O, Gupta DK, Claggett B, Burke S, Shah A, Loehr L, Rasmussen-Torvik L, Selvin E, Chang PP, Aguilar D, et al. Insulin resistance and incident heart failure the ARIC study (atherosclerosis risk in Communities). JACC Heart Fail. 2013;1(6):531–6.
Acknowledgements
We sincerely thank all the research participants and members of the Kailuan Research Group for their contributions.
Funding
This work has been supported by Science and Technology Innovation Strategy Special Project of Guangdong (No. 221117237489175).
Author information
Authors and Affiliations
Contributions
The study idea was designed by HCZ, SLW and YRC; HCZ, GZC, KYW, ZGH and XXW analyzed and interpreted the data; HCZ, GZC, ZFC, ZKC, YLL, WQW and ZWC were responsible for drafting the manuscript. The manuscript was reviewed by SLW and YRC. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of Kailuan General Hospital (approval number: 2006-05). All participants agreed to participate in the study and provided informed written consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, H., Chen, G., Wu, K. et al. Relationship between cumulative exposure to triglyceride-glucose index and heart failure: a prospective cohort study. Cardiovasc Diabetol 22, 239 (2023). https://doi.org/10.1186/s12933-023-01967-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-01967-5