Abstract
Background
Coronary artery disease (CAD) confers considerable morbidity and mortality in diabetes. However, the role of CAD in additive effect of left ventricular (LV) function has rarely been explored in type 2 diabetes mellitus (T2DM) patients. This study aimed to investigate how CAD affect LV systolic and diastolic function in T2DM patients.
Materials and methods
A total of 282 T2DM patients {104 patients with CAD [T2DM (CAD +)] and 178 without [T2DM (CAD −)]} and 83 sex- and age- matched healthy controls underwent cardiac magnetic resonance scanning. LV structure, function, global strains [including systolic peak strain (PS), peak systolic (PSSR) and diastolic strain rate (PDSR) in radial, circumferential and longitudinal directions] and late gadolinium enhancement (LGE) parameters were measured. T2DM (CAD +) patients were divided into two subgroups based on the median of Gensini score (60) which was calculated to assess the severity of CAD. Multivariable linear regression analyses were constructed to investigate the determinants of reduced LV function.
Results
Compared with normal controls, T2DM (CAD −) patients exhibited increased LV end-diastolic and end-systolic volume index and decreased LV global strains, while T2DM(CAD +) patients showed more marked increase and decrease than T2DM(CAD-) and healthy controls, except for longitudinal PDSR (PDSR-L) (all P < 0.017). All of LV global strains demonstrated a progressive decrease from normal controls, through Gensini score ≤ 60, to Gensini score > 60 group, except for PDSR-L (all P < 0.017). CAD was an independent predictor of reduced LV global circumferential PS (GCPS, β = 0.22, p < 0.001), PSSR (PSSR-C, β = 0.17, p = 0.005), PDSR (PDSR-C, β = 0.22, p < 0.001), global radial PS (GRPS, β = 0.19, p = 0.001), and global longitudinal PS (GLPS, β = 0.18, p = 0.003) in T2DM. The Gensini score was associated with decreased GCPS, PSSR-C, PDSR-C, GRPS, and GLPS in T2DM (CAD +) (all p < 0.05).
Conclusion
CAD has an additive deleterious effect on LV systolic and diastolic function in T2DM patients. Among T2DM (CAD +) patients, the Gensini score is associated with reduced LV contractile and diastolic function.
Trial registration Retrospectively registered
Similar content being viewed by others
Background
All forms of cardiovascular disease are common complications of diabetes mellitus that confers considerable morbidity and mortality [1, 2]. Mounting evidence suggest that type 2 diabetes mellitus (T2DM) can directly affect the myocardium, resulting in microvascular dysfunction, myocardial fibrosis, and left ventricular (LV) hypertrophy [3, 4]. Furthermore, it is well documented that T2DM associated with an exaggerated risk of macrovascular complication, such as coronary artery disease (CAD) [5]. People with T2DM have an almost two- to four- fold higher risk of CAD compared with those without [6]. Under the presence of ischemia, CAD may aggravate detrimental LV remodeling and dysfunction in patients with T2DM, which leads to advanced heart failure and poor clinical outcomes [7]. Therefore, a better understanding of the underlying influences of CAD on T2DM regarding cardiac function may be of paramount importance to improve our management efforts and reduce the incidence of long-term adverse events.
Cardiac magnetic resonance (CMR) tissue tracking is a novel method of measuring LV strain and strain rates, which has been applied to evaluate the LV systolic or diastolic function in diverse populations and shown high sensitivity and reproducibility [8,9,10]. To the best of our knowledge, several previous studies have focused on the additive effect of hypertension or valvular regurgitation on the LV function in T2DM patients [11, 12], the role of CAD on which has rarely been explored in those patients. [13] Accordingly, this study aimed to investigate how CAD affect LV systolic and diastolic function in T2DM patients and further to explore the independent determinants of decreased LV function.
Materials and methods
Study population
Between January 2015 and July 2021, 488 patients with T2DM undergoing CMR at our institution were retrospectively enrolled in this study. Among them, those patients with chest pain and suspected CAD were selected to undergo invasive coronary angiography (ICA) examination. T2DM was defined according to the current American Diabetes Association guidelines [14]. Obstructive CAD was defined when the luminal diameter stenosis was estimated as ≥ 50% in at least one major epicardial coronary artery [15]. Smoking was defined as current or previous smoking of at least one cigarette per day for at least 1 year [16]. Exclusion criteria were: (1) patients with prior percutaneous or surgical revascularization procedures, (2) congenital or valvular heart disease, (3) primary cardiomyopathy, (4) severe renal failure (estimated glomerular filtration rate < 30 mL/min), (5) the maximum percentage of luminal stenosis < 50% in any segment of major coronary arteries with patients who were diagnosed with CAD, (6) contradictions to CMR imaging, (7) and poor image quality. Finally, 282 T2DM patients (mean age, 59.00 ± 11.52 years; 183 male) who met above criteria were included in this study and these patients were categorized into two groups: T2DM with CAD [T2DM (CAD +), n = 104] and T2DM without CAD [T2DM (CAD −), n = 178]. In addition, 83 age- and sex-matched healthy individuals (mean age, 56.45 ± 10.05 years; 55 male) who underwent CMR examination were recruited to serve as the normal control group with no history of cardiovascular or systematic disease or diabetes mellitus. This study protocol was approved by the Biomedical Research Ethics Committee of our hospital and conducted in accordance with the ethical guidelines of the Declaration of Helsinki. Written informed consent was obtained from all subjects.
Invasive coronary angiography
Selective ICA was performed through the radial or femoral artery approach by interventional cardiologists who were blinded to the clinical data using a standard Judkins technique. T2DM patients with CAD were classified into one-, two-, or three-vessel disease according to the number of diseased coronary arteries. The luminal diameter narrowing of left main coronary artery ≥ 50% was considered as three-vessel disease [17]. According to the method described in the literature [18], the Gensini score was calculated to assess the severity of CAD by two independent experienced cardiologists who were blinded to the clinical and procedural data.
CMR protocol
All participants underwent CMR examination using a 3.0T whole-body scanner (MAGNETOM Skyra; Siemens Medical Solutions, Erlangen, Germany) in the supine position. Continuous data acquisition was performed during the end-inspiratory breath-holding period using the manufacturer’s standard ECG-triggering device which monitored dynamic changes in each subject’s ECG findings. A balanced steady-state free precession (bSSFP) sequence (TR/TE 3.4/1.2 ms, field of view 340 × 280.5 mm, flip angle 38°, slice thickness 8 mm, and matrix size 192 × 162) was performed to obtain a stack of contiguous cine images covering the whole LV from the base to the apex in the short-axis slices, as well as the four-, three-, and two-chamber in the long-axis views. Subsequently, a dose of 0.2 mL/kg body weight gadobenate dimeglumine (MultiHance 0.5 mmol/mL; Bracco, Milan, Italy) was intravenously injected at a flow rate of 2.5–3.0 mL/s, then a 20-mL saline flush immediately was injected at a rate of 3.0 mL/s. Segmented − turbo − FLASH − phase − sensitive inversion recovery (PSIR) sequence (TR/TE 598 /3.31 ms, field of view 340 × 255 mm, flip angle 40°, slice thickness 8 mm, and matrix size 256 × 162) was used to acquire LGE images after 10–15 min of contrast administration.
CMR image analysis
CMR images of all participants were evaluated offline using commercial software (cvi42, Circle Cardiovascular Imaging Inc., Calgary, Alberta, Canada) by two radiologists, each of whom had more than 5 years of CMR experience and were blinded to clinical data.
The epicardial and endocardial borders of the LV myocardium on a stack of short-axis cine images were manually outlined at the end-systolic and end-diastolic phases using the afore-mentioned software. Then, cardiac geometry and function parameters including LV mass (LVM) at end-diastole, LV end-diastolic volume (LVEDV), LV end-systolic volume (LVESV), LV stroke volume (LVSV), and LV ejection fraction (LVEF) were automatically computed. According to the Mosteller formula, LVM, LVEDV, and LVESV indexed for body surface area (BSA) were calculated and represented as LVMI, LVEDVI, and LVESVI, retrospectively [19]. LV papillary muscles and moderate bands were included in the measures of LV volume and excluded from the LVM.
A set of LV short-axis cine images in combination with two- and four- chamber long-axis images were loaded into the tissue tracking module to evaluate three-dimensional (3D) strain of LV myocardial. The LV global strain parameters including systolic peak strain (PS), peak systolic strain rate (PSSR), and peak diastolic strain rate (PDSR) in the three directions (radial, circumferential, and longitudinal) were obtained automatically using the above software. By convention, the radial strains were positive during systolic phase with radial thickening. While the longitudinal and circumferential strains were negative during systole with longitudinal and circumferential shortening respectively.
In addition, the presence or absence of LGE was analyzed by those above radiologists. A threshold- defined as 5 standard deviations (SDs) above the signal of the remote normal myocardial region-was used to measure the extent of LGE [20].
Reproducibility of LV global strains
To analyze intra-observer variability, the same observer with more than 5 years of CMR experience compared the LV global strains in 40 randomly selected participants including 30 T2DM patients and 10 healthy individuals with 2-month interval. Inter-observer variability was also obtained from the same population and was assessed by comparing the independent measurements by a second observer who is independent and double-blinded with more than 5 years of CMR experience.
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows version 24.0 (IBM Corporation, Armonk, NY, USA) and GraphPad Prism version 7.0a (GraphPad Software, San Diego, California, USA). The Shapiro–Wilk test was performed to evaluate data for normality and Levene’s test for homogeneity of continuous variables. The continuous normally distributed data were expressed as mean ± SD and non-normally distributed variables were expressed as the median (interquartile range, 25–75%). Discrete data were presented as number (percentage) and compared with Fisher’s exact test. Parameters among T2DM (CAD −), T2DM (CAD +) and normal controls groups were compared by one-way analysis of variance (One-way ANOVA) followed by Bonferroni’s post hoc-test or the Kruskal–Wallis rank test, where appropriate. The same methods were also applied to compare the parameters among T2DM (CAD +) patients with different Gensini score groups and normal controls group. Univariable linear regression analyses were constructed to identify the correlations of LV global strains with multiple clinical risk factors and other imaging parameters. Variables with an absence of collinearity and p values < 0.1 in the univariable analyses were selected in stepwise multivariable linear regression models to evaluate the independent effect of CAD on LV function in T2DM patients or identify the determinants of reduced LV function among T2DM (CAD +) patients. Inter- and intra-observer agreements were assessed using the intra-class correlation coefficient (ICC). A two-tailed p value of < 0.05 was considered to indicate statistical significance.
Results
Baseline characteristics
The baseline characteristics of the study cohort are presented in Table 1. Compared to T2DM(CAD-) patients and normal controls, T2DM(CAD +) patients were older, more often men and smokers, as well as had larger body mass index (BMI) and BSA, and had higher levels of fasting blood glucose, HbA1c, and N-terminal pro-brain natriuretic peptide (all p < 0.017). T2DM (CAD +) patients had longer disease duration than those T2DM (CAD −) [4.5 (0.63, 10) vs. 2 (0, 7.5) years, p < 0.05). The levels of blood pressure, triglycerides and renal function were similar in both subgroups of T2DM patients with and without CAD (all p > 0.05).
Among 104 T2DM (CAD +) patients, the median (IQR) Gensini score was 60 (39, 97) and the number (%) of patients for one-, two-, and three-vessel disease were 34 (32.69%), 30 (28.85%), and 40 (38.46%) respectively. Regarding the location of CAD, 95 (91.35%) patients had left ascending artery stenosis, 52 (50%) patients had left circumflex artery stenosis, and 66 (63.46%) patients had right coronary stenosis. No significant differences in management of antidiabetic drugs were observed between the T2DM (CAD −) and T2DM(CAD +) groups (all p > 0.05) (Table 2).
Comparison of CMR-derived indices among T2DM patients with and without CAD, and normal controls
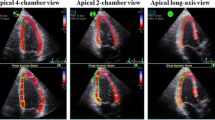
The CMR findings are shown in Table 3 and Fig. 1. In contrast to the normal controls, both T2DM patients with and without CAD exhibited increased LVMI and enlarged LVEDV and LVESV (all p < 0.017). LVEF, as preserved in those without CAD, showed a significant progressive decrease from normal controls, through T2DM (CAD −), to T2DM (CAD +) patients [63.1 (58, 67.8) vs. 55.1 (40.5, 63.5) vs. 37.2 (27, 52.4), p < 0.017]. T2DM (CAD +) patients showed a higher presence [104 (100%) vs. 56 (31.5%), p < 0.05] and extent of LGE [22.6 (12.9, 46.3) % vs. 7.7 (4.1, 16.8) %, p < 0.05) than those T2DM (CAD −).
Representative CMR pseudo-color images at the end-systole and global PS curves in a normal control, T2DM (CAD −) patient, and T2DM (CAD +) patient. A1–C1 pseudo-color images of LV radial PS in short-axis; A3–C3 three-dimensional pseudo-color maps of LV circumferential PS; A5, B5, C5 pseudo-color images of LV longitudinal PS in four-chamber long-axis; A2–C2 LV global PS curve in radial direction; A4, B4, C4 LV global PS curve in circumferential direction; A6, B6, C6 LV global PS curve in longitudinal direction. CMR cardiac magnetic resonance, PS peak strain, LV left ventricle, T2DM type 2 diabetes mellitus, CAD coronary artery disease
Regarding the LV global myocardial strains, T2DM patients even absence of CAD had evidence of decreased systolic and diastolic function, with a significant more impaired PS, PSSR, and PDSR in all of three directions than normal controls (all p < 0.017). Compared with the T2DM (CAD −) patients and normal controls, the decrease in all of LV global strains (PS, PSSR, and PDSR in the radial, circumferential, and longitudinal directions) among those T2DM (CAD +) was more marked, except for longitudinal PDSR (PDSR-L) (all p < 0.017).
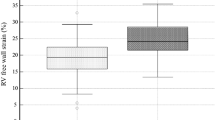
Comparison of LV global strains among T2DM (CAD +) patients with different Gensini score and normal controls
According to the median value (60) of the Gensini score, T2DM (CAD +) patients were divided into two subgroups: T2DM (CAD +) patients with Gensini score ≤ 60 (n = 51) and those with Gensini score > 60 (n = 53). The CMR-derived LV global strain parameters for the observed groups are demonstrated in Fig. 2. All of the LV global strains declined progressively from normal controls, through T2DM (CAD +) patients with Gensini score ≤ 60, to those with Gensini score > 60 (all p < 0.017), whereas the PDSR-L showed no significant difference between subgroups of T2DM (CAD +) patients with different Gensini score (p > 0.05).
Comparison of LV global strains among T2DM (CAD +) patients with different Gensini score and normal controls. The absolute values of LV global strains were used to avoid the influence of directional sign. PS peak strain, GRPS global radial peak strain, GCPS global circumferential peak strain, GLPS global longitudinal peak strain, PSSR peak systolic strain rate, PDSR peak diastolic strain rate, R radial, C circumferential, L longitudinal, T2DM type 2 diabetes mellitus, CAD coronary artery disease. *P < 0.017
Independent effect of CAD on LV systolic and diastolic function in T2DM patients
Multivariable linear regression analyses were performed to evaluate the independent effect of CAD on LV systolic and diastolic function in T2DM patients (Table 4). After controlling for sex, age, BSA, BMI, systolic and diastolic blood pressure, heart rate, and diabetes duration, CAD was independently associated with LV global circumferential PS (GCPS, β = 0.22, p < 0.001), PSSR (PSSR-C, β = 0.17, p = 0.005), PDSR (PDSR-C, β = 0.22, p < 0.001), global radial PS (GRPS, β = 0.19, p = 0.001) and global longitudinal PS (GLPS, β = 0.18, p = 0.003).
Determinants of impaired LV systolic and diastolic function in T2DM (CAD +) patients
The univariable analyses in T2DM (CAD +) patients exhibited that the Gensini score was negatively associated with GCPS (r = − 0.44, p < 0.001), PSSR-C (r = − 0.50, p < 0.001), PDSR-C (r = − 0.48, p < 0.001) (Fig. 3 A-C), GRPS (r = − 0.43, p < 0.001), and GLPS (r = − 0.43, p < 0.001). In addition, there were negative correlations between the extent of LGE and GCPS (r = − 0.46, p < 0.001), PSSR-C (r = − 0.46, p < 0.001), and PDSR-C (r = − 0.46, p < 0.001) (Fig. 3D–F), GRPS (r = − 0.44, p < 0.001), and GLPS (r = − 0.37, p < 0.001). Increasing NT-proBNP level was also significantly associated with worsening GRPS (r = − 0.49, p < 0.001), GCPS (r = − 0.52, p < 0.001), and GLPS (r = − 0.55, p < 0.001).
The associations of LV global circumferential strains with Gensini score and LGE in T2DM (CAD +) patients. The absolute values of LV circumferential global peak strains were used to avoid the influence of directional sign. GCPS global circumferential peak strain, PSSR-C the global circumferential peak systolic strain rate, PDSR-C the global circumferential peak diastolic strain rate, T2DM type 2 diabetes mellitus, CAD coronary artery disease. *P < 0.001
After adjusting for confounding factors, the Gensini score remained the independent determinant of impaired GCPS (β = − 0.34, p < 0.001), PSSR-C (β = − 0.35, p < 0.001), PDSR-C (β = − 0.34, p < 0.001), GRPS (β = − 0.29, p = 0.001) and GLPS (β = − 0.35, p < 0.001) (Table 5).
Inter-observer and intra-observer variability of LV strain parameters
As shown in Table 6, there were significantly high inter-observer and intra-observer agreements of LV global myocardial strains measured with CMR tissue tracking. The coefficient of variation of inter-observer variability for LV global PS, PSSR, and PDSR were 0.905–0.960, 0.893–0.909, and 0.895–0.944 respectively. The coefficient of variation of intra-observer variability for PS, PSSR, and PDSR were 0.900–0.969, 0.901–0.939, and 0.908–0.951 respectively.
Discussion
The present study highlights evidence supporting the viewpoint that CAD has a deleterious effect on LV function in T2DM patients. The key findings were as follows: (1) even in absence of CAD, T2DM patients displayed an adverse LV remodeling and reduced LV systolic and diastolic function, (2) when coexisting CAD, T2DM patients demonstrated a significantly more severe impairment of systolic and diastolic function, with a more marked reduction in nearly all of the LV strains than those without CAD and normal controls, (3) after adjusting for confounding factors, CAD was an independent predictor of reduced LV systolic and diastolic function in T2DM patients. (4) among T2DM (CAD +) patients, LV strains declined progressively along with the increase of Gensini score, in addition, the Gensini score was the independent determinant of decreased LV systolic and diastolic function.
Previous trials have suggested that adverse LV remodeling and dysfunction can occur even in absence of CAD in diabetes, as demonstrated by increased LVMI, with diastolic dysfunction, either alone or combined with depressed systolic function [21, 22]. The present study showed similar changes in cardiac structure and exhibited reduced both systolic and diastolic function in T2DM (CAD −) patients, despite with preserved LVEF. Besides, the presence of LGE indicating myocardial fibrosis was also observed in these patients. Therefore, detection of early changes in the LV myocardium allows for early intervention and instigating preventative strategies in T2DM patients.
Available data regarding the CAD-related influence on LV function in T2DM patients remain limited [13]. In this study, our data exhibited that T2DM (CAD +) patients had a more significantly marked decreased in nearly all of LV global strains, larger LVESVI, and lower LVEF than those T2DM (CAD −) and normal individuals, which suggest that CAD exacerbate the impairment of systolic and diastolic function. The precise underlying mechanisms of the adverse impact of CAD on LV systolic and diastolic function are not fully understood but are likely to be multifactorial. The potential mechanistic explanations for this finding are as follows: on the one hand, hyperglycemia, metabolic-related disorders, and insulin resistance induce states of pro-thrombotic, pro-inflammatory, and pro-oxidant in the context of DM, which contribute to calcium handing altered, excitation–contraction coupling impairment, myocardium interstitial fibrosis, and microvasculature abnormalities [23, 24]. Some of above-mentioned changes in molecular signal pathways also exist in a milieu of CAD [25, 26]. When T2DM comorbid with CAD, we speculate that those superimposed factors in myocardium might be amplified, thereby promoting the aggravation of myocardial contractility and relaxation impairment.
On the other hand, the association between myocardium ischemia and obstructive coronary stenosis was well established [27]. In addition, the presence and extent of LGE in our T2DM (CAD +) patients was higher than that in T2DM (CAD −) patients. Those above suggested the potential pathophysiological mechanisms of myocardium ischemia and increased international fibrosis [28] which result in more severe impairment of systolic and diastolic function in T2DM(CAD +) patients than those in T2DM (CAD −) patients. Future researches will be encouraged to explore the exact molecular mechanisms of these two stimuli (CAD and DM) interaction regarding affecting myocardial contractile and diastolic dysfunction.
Gensini score is one of the angiographic scoring systems which is widely used for quantifying the severity of CAD [29]. Accumulating studies indicated that CAD was associated with poor clinical outcomes (such as myocardial infarction, death) in T2DM patients [30, 31]. Importantly, our results add additional information by showing that LV systolic and diastolic function (nearly all of the LV global strains) decreased progressively along with the aggravation of CAD (increase of Gensini score) among T2DM(CAD +) patients. In addition, the Gensini score was the independent determinant of reduced LV contractile and diastolic function. These results emphasized the significance of CAD management in patients with T2DM. Currently, coronary revascularization either with percutaneous coronary intervention (PCI) or with coronary artery bypass graft (CABG) is acceptable option in individuals with DM and more extensive CAD [32, 33]. A recent large study based on the ISCHEMIA Trials [34] demonstrated that patients with chronic coronary disease and diabetes did not derive incremental benefit from routine coronary revascularization in contrast to the initial medical therapy alone. It is highly stimulating the exploration of future targeted medicine therapy in order to improve management and prognosis of high-risk patients with DM and CAD.
Anderson et al. [35] reported that the presence of myocardial scar detected by CMR was significantly correlated with the LV circumferential deformation in patients with DM, which was in concordance with previous study by Jiang et al. [21] In the present study, we found there was also a significant association of LGE with LV longitudinal, circumferential, and radial deformation in T2DM (CAD +) patients, which was similar to those prior observations and extended those findings to patients with both DM and CAD.
Limitations
Our results should be interpreted in the context of several limitations. First, this study was a single-center and retrospective study, and the likelihood for selection bias cannot be disregarded. Besides, insulin levels, insulin resistance (HOMA-IR) and inflammatory markers (such as: CRP and IL-6) were not complete for all patients. Their role as possible predictors of CAD in T2DM patients will be explored in the future prospective study. Second, although multivariable adjustments were conducted to obtain significant confounders, we cannot exclude the existence of unmeasured covariates. Third, although not all of our T2DM (CAD −) patients underwent coronary angiography, including invasive coronary angiography or coronary computed tomography angiography, CAD was deemed to be unlikely according to the comprehensive assessment of the patients by clinical history, electrocardiography, laboratory results and echocardiography, subsequently supported by the CMR examinations [21]. Finally, it is a cross-sectional analysis of T2DM patients with CAD and the evolution of cardiac remodeling and function is not known over time as the CAD progression. Future longitudinal studies will be needed to address this question.
Conclusions
In summary, CAD had an additive deleterious effect on LV systolic and diastolic function in patients with T2DM. The Gensini score quantifying the severity of CAD was associated with reduced contractile and diastolic function among T2DM (CAD +) patients. Future studies should be encouraged to explore the underlying mechanisms by which the coexistence of these two stimuli (CAD and DM) affect the myocardium and how these effects could be prevented.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CAD:
-
Coronary artery disease
- T2DM:
-
Type 2 diabetes mellitus
- LV:
-
Left ventricular
- PS:
-
Peak strain
- PSSR:
-
Peak systolic strain rate
- PDSR:
-
Peak diastolic strain rate
- LGE:
-
Late gadolinium enhancement
- PDSR-L:
-
The longitudinal PDSR
- PSSR-C:
-
The circumferential PSSR
- PDSR-C:
-
The circumferential PDSR
- CMR:
-
Cardiac magnetic resonance
- ICA:
-
Invasive coronary angiography
- bSSFP:
-
Balanced steady-state free precession
- LVM:
-
LV mass
- LVEDV:
-
LV end-diastolic volume
- LVESV:
-
LV end-systolic volume
- LVSV:
-
LV stroke volume
- LVEF:
-
LV ejection fraction
- ICC:
-
Intra-class correlation coefficient
- GRPS:
-
Global radial peak strain
- GCPS:
-
Global circumferential peak strain
- GLPS:
-
Global longitudinal peak strain
References
Eckel RH, Bornfeldt KE, Goldberg IJ. Cardiovascular disease in diabetes, beyond glucose. Cell Metab. 2021;33:1519–45.
Ng ACT, Delgado V, Borlaug BA, Bax JJ. Diabesity: the combined burden of obesity and diabetes on heart disease and the role of imaging. Nat Rev Cardiol. 2020;18:291–304.
Skali H, Di Carli MF, Blankstein R, Chow BJ, Beanlands RS, Berman DS, Germano G, Min JK, Merhige M, Williams B, Veledar E, Shaw LJ, Dorbala S. Stress myocardial perfusion PET provides incremental risk prediction in patients with and patients without diabetes. Radiol Cardiothorac Imaging. 2019;1:e180018.
Levelt E, Rodgers CT, Clarke WT, Mahmod M, Ariga R, Francis JM, Liu A, Wijesurendra RS, Dass S, Sabharwal N, Robson MD, Holloway CJ, Rider OJ, Clarke K, Karamitsos TD, Neubauer S. Cardiac energetics, oxygenation, and perfusion during increased workload in patients with type 2 diabetes mellitus. Eur Heart J. 2016;37:3461–9.
Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287(19):2570–81.
Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H. Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia. 2001;44(Suppl 2):S14-21.
Bax JJ, Young LH, Frye RL, Bonow RO, Steinberg HO, Barrett EJ. Screening for coronary artery disease in patients with diabetes. Diabetes Care. 2007;30:2729–36.
Kammerlander AA, Dona C, Nitsche C, Koschutnik M, Schonbauer R, Duca F, Zotter-Tufaro C, Binder C, Aschauer S, Beitzke D, Loewe C, Hengstenberg C, Bonderman D, Mascherbauer J. Feature tracking of global longitudinal strain by using cardiovascular MRI improves risk stratification in heart failure with preserved ejection fraction. Radiology. 2020;296:290–8.
Giusca S, Korosoglou G, Montenbruck M, Geršak B, Schwarz AK, Esch S, Kelle S, Wülfing P, Dent S, Lenihan D, Steen H. Multiparametric early detection and prediction of cardiotoxicity using myocardial strain, T1 and T2 mapping, and biochemical markers: a longitudinal cardiac resonance imaging study during 2 years of follow-up. Circ Cardiovasc Imaging. 2021;14(6):e012459.
Voigt JU, Cvijic M. 2- and 3-Dimensional myocardial strain in cardiac health and disease. JACC Cardiovasc imaging. 2019;12:1849–63.
Jiang L, Ren Y, Yu H, Guo YK, Liu X, Deng MY, Xie LJ, Gao Y, Shen MT, Han PL, Yang ZG. Additive effect of hypertension on left ventricular structure and function in patients with asymptomatic type 2 diabetes mellitus. J Hypertens. 2020;39:538.
Zhang Y, Yan WF, Jiang L, Shen MT, Li Y, Huang S, Shi K, Yang ZG. Aggravation of functional mitral regurgitation on left ventricle stiffness in type 2 diabetes mellitus patients evaluated by CMR tissue tracking. Cardiovasc diabetol. 2021;20:158.
Burgmaier M, Frick M, Liberman A, Battermann S, Hellmich M, Lehmacher W, Jaskolka A, Marx N, Reith S. Plaque vulnerability of coronary artery lesions is related to left ventricular dilatation as determined by optical coherence tomography and cardiac magnetic resonance imaging in patients with type 2 diabetes. Cardiovasc Diabetol. 2013;12:102.
Chamberlain JJ, Rhinehart AS, Shaefer CF Jr, Neuman A. Diagnosis and management of diabetes: synopsis of the 2016 American Diabetes Association Standards of medical care in diabetes. Ann Intern Med. 2016;164(8):542–52.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD. Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–64.
Pongrac Barlovic D, Harjutsalo V, Gordin D, Kallio M, Forsblom C, King G, Groop PH, FinnDiane Study Group. The association of severe diabetic retinopathy with cardiovascular outcomes in long-standing type 1 diabetes: a longitudinal follow-up. Diabetes Care. 2018;41(12):2487–94.
Wang XB, Cui NH, Liu X, Liu X. Mitochondrial 8-hydroxy-2’-deoxyguanosine and coronary artery disease in patients with type 2 diabetes mellitus. Cardiovasc diabetol. 2020;19:22.
Rampidis GP, Benetos G, Benz DC, Giannopoulos AA, Buechel RR. A guide for Gensini score calculation. Atherosclerosis. 2019;287:181–3.
Schulz-Menger J, Bluemke DA, Bremerich J, Flamm SD, Fogel MA, Friedrich MG, Kim RJ, von Knobelsdorff-Brenkenhoff F, Kramer CM, Pennell DJ, Plein S, Nagel E. Standardized image interpretation and post-processing in cardiovascular magnetic resonance—2020 update: society for cardiovascular magnetic resonance (SCMR): board of trustees task force on standardized post-processing. J Cardiovasc Magn Reson. 2020;22:19.
Bondarenko O, Beek AM, Hofman MB, Kuhl HP, Twisk JW, van Dockum WG, Visser CA, van Rossum AC. Standardizing the definition of hyperenhancement in the quantitative assessment of infarct size and myocardial viability using delayed contrast-enhanced CMR. J Cardiovasc Magn Reson. 2005;7:481–5.
Jiang L, Wang J, Liu X, Li ZL, Xia CC, Xie LJ, Gao Y, Shen MT, Han PL, Guo YK, Yang ZG. The combined effects of cardiac geometry, microcirculation, and tissue characteristics on cardiac systolic and diastolic function in subclinical diabetes mellitus-related cardiomyopathy. Int J Cardiol. 2020;320:112–8.
Daniels A, Linz D, van Bilsen M, Rutten H, Sadowski T, Ruf S, Juretschke HP, Neumann-Haefelin C, Munts C, van der Vusse GJ, van Nieuwenhoven FA. Long-term severe diabetes only leads to mild cardiac diastolic dysfunction in Zucker diabetic fatty rats. Eur J Heart Fail. 2012;14:193–201.
Kawamura M, Paulsen MJ, Goldstone AB, Shudo Y, Wang H, Steele AN, Stapleton LM, Edwards BB, Eskandari A, Truong VN, Jaatinen KJ, Ingason AB, Miyagawa S, Sawa Y, Woo YJ. Tissue-engineered smooth muscle cell and endothelial progenitor cell bi-level cell sheets prevent progression of cardiac dysfunction, microvascular dysfunction, and interstitial fibrosis in a rodent model of type 1 diabetes-induced cardiomyopathy. Cardiovasc diabetol. 2017;16:142.
Zhao CT, Wang M, Siu CW, Hou YL, Wang T, Tse HF, Yiu KH. Myocardial dysfunction in patients with type 2 diabetes mellitus: role of endothelial progenitor cells and oxidative stress. Cardiovasc Diabetol. 2012;11:147.
Agrawal H, Choy HK, Liu J, Auyoung M, Albert MA. Coronary artery disease. Arterioscler Thromb Vasc Biol. 2020;40:e185–92.
Sechtem U, Brown D, Godo S, Lanza GA, Shimokawa H, Sidik N. Coronary microvascular dysfunction in stable ischaemic heart disease (non-obstructive coronary artery disease and obstructive coronary artery disease). Cardiovasc Res. 2020;116:771–86.
Nguyen MT, Cosson E, Valensi P, Poignard P, Nitenberg A, Pham I. Transthoracic echocardiographic abnormalities in asymptomatic diabetic patients: association with microalbuminuria and silent coronary artery disease. Diabetes Metab. 2011;37(4):343–50.
Ng ACT, Delgado V, Borlaug BA, Bax JJ. Diabesity: the combined burden of obesity and diabetes on heart disease and the role of imaging. Nat Rev Cardiol. 2021;18(4):291–304.
Kadoglou NPE, Korakas E, Lampropoulos S, Maratou E, Kassimis G, Patsourakos N, Plotas P, Moutsatsou P, Lambadiari V. Plasma nesfatin-1 and DDP-4 levels in patients with coronary artery disease: Kozani study. Cardiovasc diabetol. 2021;20:166.
Cho E, Rimm EB, Stampfer MJ, Willett WC, Hu FB. The impact of diabetes mellitus and prior myocardial infarction on mortality from all causes and from coronary heart disease in men. J Am Coll Cardiol. 2002;40(5):954–60.
Berry C, Tardif JC, Bourassa MG. Coronary heart disease in patients with diabetes: part II: recent advances in coronary revascularization. J Am Coll Cardiol. 2007;49:643–56.
Authors/Task Force m, Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Juni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541–619.
Myers GR, Weintraub WS. Coronary artery disease: revascularization strategies for patients with CAD and diabetes. Nat Rev Cardiol. 2010;7:364–6.
Newman JD, Anthopolos R, Mancini GBJ, Bangalore S, Reynolds HR, Kunichoff DF, Senior R, Peteiro J, Bhargava B, Garg P, Escobedo J, Doerr R, Mazurek T, Gonzalez-Juanatey J, Gajos G, Briguori C, Cheng H, Vertes A, Mahajan S, Guzman LA, Keltai M, Maggioni AP, Stone GW, Berger JS, Rosenberg YD, Boden WE, Chaitman BR, Fleg JL, Hochman JS, Maron DJ. Outcomes of participants with diabetes in the ISCHEMIA trials. Circulation. 2021;144(17):1380–95.
Armstrong AC, Ambale-Venkatesh B, Turkbey E, Donekal S, Chamera E, Backlund JY, Cleary P, Lachin J, Bluemke DA, Lima JA, DCCT/EDIC Research Group. Association of cardiovascular risk factors and myocardial fibrosis with early cardiac dysfunction in type 1 diabetes: the diabetes control and complications trial/epidemiology of diabetes interventions and complications study. Diabetes Care. 2017;40(3):405–11.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (81771887, 81471722, 821201080, 81971586), the Fellowship of China Postdoctoral Science Foundation (2021M692287) and the 1·3·5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYGD18013).
Author information
Authors and Affiliations
Contributions
JW designed the study, analyzed the data, and drafted the manuscript. YKG, ZGY and YL was responsible for guiding the study, editing and review of the manuscript. WLQ and GXH collected the data. SH, RS and WFY analyzed the data and gave advice on data presentation. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study complied with the Declaration of Helsinki and was approved by the Biomedical Research Ethics Committee of our hospital. Written informed consent was obtained from all participants and patient-sensitive data were protected with full confidentiality and used only for the purposes of this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, J., Li, Y., Guo, YK. et al. The adverse impact of coronary artery disease on left ventricle systolic and diastolic function in patients with type 2 diabetes mellitus: a 3.0T CMR study. Cardiovasc Diabetol 21, 30 (2022). https://doi.org/10.1186/s12933-022-01467-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-022-01467-y