Abstract
Background
Epicardial adipose tissue (EAT) is considered a novel diagnostic marker for cardiometabolic disease. This study aimed to evaluate whether EAT volume was associated with stress-induced myocardial ischemia in asymptomatic people living with diabetes—independently of confounding factors—and whether it could predict this condition.
Methods
We included asymptomatic patients with diabetes and no coronary history, who had undergone both a stress a myocardial scintigraphy to diagnose myocardial ischemia, and a computed tomography to measure their coronary artery calcium (CAC) score. EAT volume was retrospectively measured from computed tomography imaging. Determinants of EAT volume and asymptomatic myocardial ischemia were evaluated.
Results
The study population comprised 274 individuals, including 153 men. Mean (± standard deviation) age was 62 ± 9 years, and 243, 23 and 8 had type 2, type 1, or another type of diabetes, respectively. Mean body mass index was 30 ± 6 kg/m2, and mean EAT volume 96 ± 36 cm3. Myocardial ischemia was detected in 32 patients (11.7%). EAT volume was positively correlated with age, body mass index and triglyceridemia, but negatively correlated with HbA1c, HDL- and LDL-cholesterol levels. Furthermore, EAT volume was lower in people with retinopathy, but higher in men, in current smokers, in patients with nephropathy, those with a CAC score > 100 Agatston units, and finally in individuals with myocardial ischemia (110 ± 37 cm3 vs 94 ± 37 cm3 in those without myocardial ischemia, p < 0.05). The association between EAT volume and myocardial ischemia remained significant after adjustment for gender, diabetes duration, peripheral macrovascular disease and CAC score. We also found that area under the ROC curve analysis showed that EAT volume (AROC: 0.771 [95% confidence interval 0.683–0.858]) did not provide improved discrimination of myocardial ischemia over the following classic factors: gender, diabetes duration, peripheral macrovascular disease, retinopathy, nephropathy, smoking, atherogenic dyslipidemia, and CAC score (AROC 0.773 [0.683–0.862]).
Conclusions
EAT may play a role in coronary atherosclerosis and coronary circulation in patients with diabetes. However, considering EAT volume is not a better marker for discriminating the risk of asymptomatic myocardial ischemia than classic clinical data.
Similar content being viewed by others
Background
Despite improved multifactorial care, diabetes is still associated with an increased risk of cardiovascular disease [1, 2]. It has been suggested that the visceral fat tissues located adjacent to the coronary arteries—especially epicardial adipose tissue (EAT)—are one of the elements linking diabetes with cardiovascular disease [3, 4] for two primary reasons: first, diabetes is accompanied by an expansion of EAT and pericardial adipose tissue [4]. Second, these tissues secrete inflammatory factors and lipid metabolites, and may be determinants of accelerated atherosclerosis [3,4,5,6].
Some studies have shown that EAT amount is associated with myocardial ischemia and/or coronary stenosis in the general population [7,8,9,10,11]. However, only one study to date has explored this association specifically in asymptomatic persons living with type 2 diabetes (i.e., no personal cardiovascular history or symptoms) [12]. In that study, Kim et al. showed that increased EAT thickness was an independent risk factor for coronary stenosis but not for myocardial ischemia. However, the study’s power was limited as only 100 patients were included. Detecting diabetic patients with a very high risk of asymptomatic coronary disease is clinically relevant as they could benefit from specific prevention interventions [13,14,15].
In this context, using a large cohort of asymptomatic patients living with diabetes, the present study aimed to evaluate whether EAT volume was associated with asymptomatic myocardial ischemia, and whether it could help discriminate patients with this condition better than classic risk markers.
Methods
Inclusion criteria
This observational study retrospectively recruited consecutive patients consulted between 2010 and 2019 in the diabetes clinic in Jean Verdier Hospital, in Bondy, France. Data were extracted from the hospital’s files and were anonymized.
We selected individuals with diabetes who had no personal history of coronary artery disease or associated symptom, no heart failure, a normal 12-lead resting electrocardiogram (ECG), and both a stress myocardial scintigraphy and computed tomography (CT) measurement of their coronary artery calcium (CAC) score. The latter two examinations are routinely performed to evaluate cardiovascular risk in the hospital’s Diabetology–Endocrinology–Nutrition unit [13, 14]. The same CT scans were also used to measure EAT volume.
Data collection
Data were extracted from patients’ medical records and collected anonymously in a secure health database. For the present study, we focused on:
-
General data: current tobacco consumption, diagnosed premature (before 55 years of age for men; before 65 years for women) coronary artery disease in first degree relatives.
-
Medical history: routine treatments before admission, history of peripheral macrovascular disease (history of stroke, peripheral artery occlusive disease, 50% or greater stenosis measured by ultrasound examination). Hypertension and dyslipidemia were self-reported and/or inferred from prescriptions for antihypertensive and lipid-lowering agents, respectively. Additionally, we collected data to measure possible obesity (body mass index (BMI) ≥ 30 kg/m2). BMI was calculated using the formula: weight (kg)/height2 (m2). Weight and height were measured within 24 h of hospital admission.
-
Biomarkers: HbA1c (high performance liquid chromatography variant); total and HDL-cholesterol (colorimetric assay on homogenous phase and cholesterol dosage by cholesterol oxidase), triglycerides (colorimetric assay), and LDL-cholesterol (calculated using the Friedewald formula). All these measurements were performed on plasma from fasting individuals using a Cobas 6000 analyzer (Roche diagnostics, Meylan, France). Atherogenic dyslipidemia was defined as triglycerides ≥ 2.26 mmol/L and HDL-cholesterol ≤ 0.88 mmol/L [16]. Serum creatinine was measured (colorimetry, Kone Optima, Thermolab System, Paris La Défense, France) and the glomerular filtration rate estimated (using the Chronic Kidney Disease-Epidemiology Collaboration equation). Furthermore, the urinary albumin excretion rate was measured (immunoturbidimetry, Cobas c501, Roche Diagnostics, Meylan, France), with levels between 30 and 299 mg/24 h defining microalbuminuria, and higher levels defining macroalbuminuria.
-
Diabetes-related complications: retinopathy (detected by fundus photography or ophthalmoscopy), nephropathy (defined as renal failure (i.e., an estimated glomerular filtration rate < 60 mL/min) and/or micro or macroalbuminuria), neuropathy (defined as any sign or symptom of polyneuropathy), and peripheral macrovascular disease.
Stress myocardial scintigraphy
Patients underwent a dual-isotope rest 201thallium/stress 99mTc-sestamibi protocol or a stress/rest protocol using 99mTc-sestamibi [17]. The stress test consisted in an exercise using either a calibrated bicycle ergometer or a pharmacological stress test (dipyridamole injection), or both. The former was performed when a patient was able to exercise on a bicycle ergometer and was expected to have an interpretable exercise-based ECG. The latter was performed when a patient was unable to exercise or when the exercise-based ECG stress test result was indeterminate. Asymptomatic myocardial ischemia was defined as having an abnormal ECG stress test and/or abnormal myocardial scintigraphy (i.e., defects in at least three of the 17 segmental regions).
CT imaging
CAC scores and EAT volume were calculated using ECG-gated cardiac CT without contrast injection. All CT scans were performed with GE (Healthcare Digital, France) or Siemens (Healthineers, France) scanners. CAC scores were calculated following manufacturers’ guidelines [18] using a dedicated tool available on Picture Archiving and Communication Systems (PACS) platforms (either from Carestream Health, Rochester, NY or Philips Healthcare, Best, the Netherlands). EAT volume was quantified with the software package AW VolumeShare 7 (GE Healthcare Digital) and was measured using a semi-automatic segmentation technique on every axial slice from the thoracic inlet to the beginning of the abdomen. The software automatically measured EAT volume (in cm3) by summing appropriate pixels using a CT Hounsfield unit, range − 150 to − 50 HU. The software user could readjust the delimitation manually when necessary [19, 20].
Statistical analyses
Continuous variables were expressed as means ± standard deviation and compared using one-way ANOVA or the Mann–Whitney’s U test as appropriate. No data replacement procedure was used for missing data. Pearson’s and/or Spearman’s correlations were performed to identify the parameters associated with EAT. The χ2 test was used to measure significant differences between the proportion of patients with or without asymptomatic myocardial ischemia.
We used the C-statistic to determine whether EAT volume and CAC score [13, 14, 21]—separately or combined—improved the prediction of the risk of myocardial ischemia over the risk predicted when using classic factors associated with asymptomatic myocardial ischemia (i.e., male gender, diabetes duration, peripheral macrovascular disease, retinopathy, nephropathy, smoking, and atherogenic dyslipidemia [16, 22, 23]). Finally, to evaluate the independent relationship between EAT volume and myocardial ischemia, we performed logistic regressions for the multivariable analyses, which included the classic variables listed above—at first separately and then all together—as well as EAT volume, the CAC score and BMI. We also evaluated the independent relationship between EAT volume and additional parameters that were associated with EAT volume, i.e. age, HbA1c, systolic blood pressure, triglycerides, HDL- and LDL-cholesterol levels. Odds ratios (OR) with 95% confidence intervals (95CI) for the risk of myocardial ischemia were calculated.
Results
Patient characteristics
The characteristics of the 274 included patients, including 153 men, are shown in Table 1. In summary, mean (± standard deviation) age was 62 ± 9 years, and 243, 23 and 8 had type 2, type 1, or another type of diabetes, respectively. Mean diabetes duration was 17 ± 10 years and 55.5% of the patients were treated with insulin. The percentage of obese participants was 48.1%. Mean EAT volume 96 ± 36 cm3 and 32 patients (11.7%) had asymptomatic myocardial ischemia.
Parameters associated with EAT volume
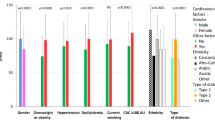
EAT volume was positively correlated with age, BMI and triglyceridemia, but negatively correlated with HbA1c, HDL- and LDL-cholesterol level (Table 2). Furthermore, it was lower in people with retinopathy than in those without (87 ± 34 vs 103 ± 38 cm3, p < 0.001), but higher in men than in women (107 ± 38 vs 83 ± 31 cm3, p < 0.01), in current smokers (107 ± 43 vs 95 ± 35 cm3, p < 0.05), in patients with nephropathy (101 ± 37 vs 91 ± 36 cm3, p < 0.05), in those with a CAC score > 100 AU (103 ± 38 vs 90 ± 34 cm3, p < 0.01), and finally in individuals with myocardial ischemia (94 ± 37 vs 110 ± 37 cm3, p < 0.05) (Figs. 1 and 2).
Parameters associated with asymptomatic myocardial ischemia
Individuals with myocardial ischemia (versus without) were more likely to be male (OR 3.2 [95CI 1.3–7.6]), to have peripheral macrovascular disease (OR 2.8 [95 CI 1.3–6.1]), a CAC score > 100 Agatston units (AU) (OR 3.0 [95 CI 1.3–6.7]), and to be treated with aspirin (OR 2.6 [95 CI 1.2–5.7]). Furthermore, they had diabetes for a longer time (Table 1).
In the multivariable analyses, the association between EAT volume and myocardial ischemia remained statistically significant after adjustment for each of the following variables: gender, diabetes duration, peripheral macrovascular disease, and CAC score (Table 3).
Additionally, neither EAT volume nor CAC score—separately or combined—were better at discriminating the risk of myocardial ischemia over classic risk factors (Fig. 3). Specifically, the areas under the ROC curve (AROC [95CI]) were 0.770 [0.680–0.860] for classic risk factors, 0.767 [0.679–0,856] for classic risk factors and EAT volume, 0.773 [0.683–0.862] for classic risk factors and CAC score, and finally 0.771 [0.683–0.858] for classic risk factors and both EAT volume and CAC score.
Area under the curve to predict asymptomatic myocardial ischemia. Model 1 (classic risk factors: male gender, diabetes duration, peripheral macrovascular disease, retinopathy, nephropathy, atherogenic dyslipidemia, smoking): area under the ROC curve (AROC [95% confidence interval]) 0.770 [0.680–0.860]). Model 2 (Model 1 + epicardial adipose tissue (EAT) volume): AROC 0.767 [0.679–0;856]. Model 3 (Model 1 + coronary artery calcium score (CAC) score): AROC 0.773 [0.683–0.862]. Model 4 (Model 1 + EAT volume + CAC score): AROC 0.771 [0.683–0.858]
Discussion
Our cohort study results show that EAT volume was significantly associated with stress-induced myocardial ischemia in asymptomatic people with diabetes, and that this association remained significant after controlling for gender, diabetes duration, peripheral macrovascular disease, and CAC score. However, EAT volume did not improve discrimination of ischemia over these classic risk factors.
In contrast, in their Korean cohort, Kim et al. did not report a significant association between EAT thickness and asymptomatic myocardial ischemia or infarction (with vs. without: 12.8 ± 2.1 vs 11.7 ± 2.3 mm, respectively, p = 0.11) [12]. This discrepancy with our results may be due to better statistical power in our study than theirs (274 vs 100 participants, respectively), the different type of EAT measurement (volume vs thickness), the different method used to screen for myocardial ischemia (scintigraphy vs magnetic resonance acquired during adenosine stress and at rest), and different patient profiles (ethnicity, BMI 30 vs 25 kg/m2, diabetes duration 17 vs 8 years, and HbA1c level 8 vs 7%) [12].
There are arguments for a causal relationship between EAT and myocardial ischemia. First, increased EAT volume/thickness has been associated with other markers of subclinical atherosclerosis patients with diabetes including high CAC score [19], arterial stiffness [24] and cardiac dysfunction [3]. Second, prospective studies have shown that high EAT volume/thickness is predictive of a higher incidence of cardiovascular events in the general population [25] and in patients with type 2 diabetes [26, 27]. Third, the positive association between EAT and myocardial ischemia may reflect pathophysiological effects of EAT on coronary circulation. This hypothesis is supported by other studies reporting a similar association [7,8,9,10,11]. However, inclusion criteria in those studies differed from ours as they considered only between 7% [11] and 36% [9] of patients with diabetes, persons in secondary prevention [9], and/or persons with chest pain [7,8,9,10,11]. More specifically, several pathophysiological pathways may be involved in the association. First, EAT volume has been reported to be higher in patients with coronary stenoses [9, 10, 12, 28] and is associated with plaque vulnerability, which may contribute to acute coronary syndrome [29]. It also distinguishes patients with vs without myocardial infarction [30]. Second, it has been suggested that EAT is an important source of energy for the myocardium during periods of increased energy demand through lipolysis and fat oxidation, leading to putative lipotoxicity in cardiomyocytes and disruption of fatty acid beta oxidation [3]. Third, in patients without significant coronary stenosis, ischemia may result from functional disorders, such as abnormal coronary reserve and endothelial dysfunction [31,32,33]. It has been shown that abnormal increases in EAT volume are proinflammatory and that EAT secretes vasoactive factors that regulate coronary endothelial function and facilitate free fatty acid influx [3,4,5,6]. However, some studies have suggested that no association exists between EAT and microvascular function [34] or coronary vasomotor dysfunction in patients with diabetes [35] (although the same studies did find such associations in individuals without diabetes).
The association between EAT volume and ischemia in our study population may be partially due to confounding factors. EAT volume and asymptomatic myocardial ischemia share similar risk factors, such as male gender, age, diabetes duration, lipid disorders, nephropathy, peripheral macrovascular disease, and a high CAC score [3, 12, 16, 19, 22, 23]. We found that EAT was associated with myocardial ischemia independently of gender, diabetes duration, peripheral macrovascular disease and CAC score, but not independently of the other confounders listed above. This means that control of cardiovascular risk factors, including BMI, lipid, glucose, blood pressure and smoking may explain a higher risk of both myocardial ischemia and higher EAT volume. Specific mechanistic studies are therefore needed to fully understand how EAT could foster ischemia in the diabetic population. Finally, our results showed that EAT volume did not improve discrimination of predicted risk of asymptomatic myocardial ischemia over classic factors, suggesting that the screening strategies currently proposed [13, 14] would not be improved if EAT volume were measured concurrently with CAC score.
Our study has several limitations. First, it was observational in design, which prevented us from being able to draw conclusions about causal relationships between EAT volume and myocardial ischemia. Second, we only included patients who had been admitted to our hospital department and who had both a myocardial scintigraphy and a CAC score measurement. Therefore, our results may not be representative of all patients with diabetes. Third, we did not have data on ethnicity, which is a determinant of EAT volume in the diabetic population [19]. Fourth, we did not include an invasive angiography to assess potential coronary stenosis in patients with myocardial ischemia. Fifth, we explored global but not regional EAT volume in the heart [10, 11, 36], and EAT volume but not its density. Having said that, density was not associated with myocardial ischemia in a previous study [11]. Finally, we did not have any data on EAT function [3, 37], such as inflammation or brown fat activity.
The main strength of our study is that we measured EAT and not pericardial (or total cardiac) adipose tissue. EAT lies between the myocardium and the visceral layer of the pericardium and is different from pericardial fat, which is located externally to the myocardium. As no fascia separates EAT from the myocardium, they are in direct contact [3,4,5,6]. To date, EAT is the only type of cardiac adipose tissue which has been observed to predict incident cardiovascular events in people with type 2 diabetes [26]. Furthermore, we applied a robust methodology—CT acquisition and assessment following standard methods—and used specific cardiac software to automatically quantify EAT. CT scans are considered the gold standard for EAT as, unlike echography, they measure EAT volume not thickness [5, 27].
Conclusions
We showed that EAT volume was significantly higher in asymptomatic individuals with myocardial ischemia—specifically stress-induced myocardial ischemia—who had diabetes, and that this association remained significant after adjustment for gender, diabetes duration, peripheral macrovascular disease and CAC score. Finally, EAT volume did not improve the prediction of the risk of ischemia over these classic risk factors in this population.
Availability of data and materials
Data for the present analysis can be provided from the first author on reasonable request.
Abbreviations
- 95CI:
-
95% Confidence interval
- AROC:
-
Area under the operating curve
- BMI:
-
Body mass index
- CAC:
-
Coronary artery calcium
- CT:
-
Computed tomography
- EAT:
-
Epicardial adipose tissue
- ECG:
-
Electrocardiogram
- PACS:
-
Picture Archiving and Communication Systems
- OR:
-
Odds ratio
References
Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370:1514–23.
Vergès B. Cardiovascular disease in type 1 diabetes: a review of epidemiological data and underlying mechanisms. Diabetes Metab. 2020;46:442–9.
Christensen RH, von Scholten BJ, Lehrskov LL, Rossing P, Jørgensen PG. Epicardial adipose tissue: an emerging biomarker of cardiovascular complications in type 2 diabetes? Ther Adv Endocrinol Metab. 2020;11:2042018820928824.
Li Y, Liu B, Li Y, Jing X, Deng S, Yan Y, et al. Epicardial fat tissue in patients with diabetes mellitus: a systematic review and meta-analysis. Cardiovasc Diabetol. 2019;18:3.
Villasante Fricke AC, Iacobellis G. Epicardial adipose tissue: clinical biomarker of cardio-metabolic risk. Int J Mol Sci. 2019;20:5989.
Iacobellis G, Barbaro G. Epicardial adipose tissue feeding and overfeeding the heart. Nutrition. 2019;59:1–6.
Tamarappoo B, Dey D, Shmilovich H, Nakazato R, Gransar H, Cheng VY, et al. Increased pericardial fat volume measured from noncontrast CT predicts myocardial ischemia by SPECT. JACC Cardiovasc Imaging. 2010;3:1104–12.
Janik M, Hartlage G, Alexopoulos N, Mirzoyev Z, McLean DS, Arepalli CD, et al. Epicardial adipose tissue volume and coronary artery calcium to predict myocardial ischemia on positron emission tomography-computed tomography studies. J Nucl Cardiol. 2010;17:841–7.
Nakazato R, Dey D, Cheng VY, Gransar H, Slomka PJ, Hayes SW, et al. Epicardial fat volume and concurrent presence of both myocardial ischemia and obstructive coronary artery disease. Atherosclerosis. 2012;221:422–6.
Khawaja T, Greer C, Thadani SR, Kato TS, Bhatia K, Shimbo D, et al. Increased regional epicardial fat volume associated with reversible myocardial ischemia in patients with suspected coronary artery disease. J Nucl Cardiol. 2015;22:325–33.
Hell MM, Ding X, Rubeaux M, Slomka P, Gransar H, Terzopoulos D, et al. Epicardial adipose tissue volume but not density is an independent predictor for myocardial ischemia. J Cardiovasc Comput Tomogr. 2016;10:141–9.
Kim HM, Kim KJ, Lee H-J, Yu HT, Moon JH, Kang ES, et al. Epicardial adipose tissue thickness is an indicator for coronary artery stenosis in asymptomatic type 2 diabetic patients: its assessment by cardiac magnetic resonance. Cardiovasc Diabetol. 2012;11:83.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
Valensi P, Henry P, Boccara F, Cosson E, Prevost G, Emmerich J, et al. Risk stratification and screening for coronary artery disease in asymptomatic patients with diabetes mellitus: Position paper of the French Society of Cardiology and the French-speaking Society of Diabetology. Diabetes Metab. 2021;47:101185.
Valensi P, Cosson E. It is not yet the time to stop screening diabetic patients for silent myocardial ischaemia. Diabetes Metab. 2010;36:91–6.
Valensi P, Avignon A, Sultan A, Chanu B, Nguyen MT, Cosson E. Atherogenic dyslipidemia and risk of silent coronary artery disease in asymptomatic patients with type 2 diabetes: a cross-sectional study. Cardiovasc Diabetol. 2016;15:104.
Cosson E, Nguyen MT, Chanu B, Banu I, Chiheb S, Balta C, et al. Cardiovascular risk prediction is improved by adding asymptomatic coronary status to routine risk assessment in type 2 diabetic patients. Diabetes Care. 2011;34:2101–7.
Hecht HS, Cronin P, Blaha MJ, Budoff MJ, Kazerooni EA, Narula J, et al. 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncontrast noncardiac chest CT scans: a report of the Society of Cardiovascular Computed Tomography and Society of Thoracic Radiology. J Thorac Imaging. 2017;32:W54-66.
Cosson E, Nguyen MT, Rezgani I, Tatulashvili S, Sal M, Berkane N, et al. Epicardial adipose tissue volume and coronary calcification among people living with diabetes: a cross-sectional study. Cardiovasc Diabetol. 2021;20:35.
Bihan H, Heidar R, Beloeuvre A, Allard L, Ouedraogo E, Tatulashvili S, et al. Epicardial adipose tissue and severe Coronavirus Disease 19. Cardiovasc Diabetol. 2021;20:147.
Bavishi C, Argulian E, Chatterjee S, Rozanski A. CACS and the frequency of stress-induced myocardial ischemia during MPI: a meta-analysis. JACC Cardiovasc Imaging. 2016;9:580–9.
Cosson E, Attali JR, Valensi P. Markers for silent myocardial ischemia in diabetes. Are they helpful? Diabetes Metab. 2005;31:205–13.
Cosson E, Nguyen MT, Chanu B, Balta S, Takbou K, Valensi P. The report of male gender and retinopathy status improves the current consensus guidelines for the screening of myocardial ischemia in asymptomatic type 2 diabetic patients. Nutr Metab Cardiovasc Dis. 2013;23:557–65.
Al-Talabany S, Mordi I, Graeme Houston J, Colhoun HM, Weir-McCall JR, Matthew SZ, et al. Epicardial adipose tissue is related to arterial stiffness and inflammation in patients with cardiovascular disease and type 2 diabetes. BMC Cardiovasc Disord. 2018;18:31.
Mahabadi AA, Berg MH, Lehmann N, Kälsch H, Bauer M, Kara K, et al. Association of epicardial fat with cardiovascular risk factors and incident myocardial infarction in the general population: the Heinz Nixdorf Recall Study. J Am Coll Cardiol. 2013;61:1388–95.
Christensen RH, von Scholten BJ, Hansen CS, Jensen MT, Vilsbøll T, Rossing P, et al. Epicardial adipose tissue predicts incident cardiovascular disease and mortality in patients with type 2 diabetes. Cardiovasc Diabetol. 2019;18:114.
Christensen RH, von Scholten BJ, Hansen CS, Heywood SE, Rosenmeier JB, Andersen UB, et al. Epicardial, pericardial and total cardiac fat and cardiovascular disease in type 2 diabetic patients with elevated urinary albumin excretion rate. Eur J Prev Cardiol. 2017;24:1517–24.
Versteylen MO, Takx RAP, Joosen IAPG, Nelemans PJ, Das M, Crijns HJGM, et al. Epicardial adipose tissue volume as a predictor for coronary artery disease in diabetic, impaired fasting glucose, and non-diabetic patients presenting with chest pain. Eur Heart J Cardiovasc Imaging. 2012;13:517–23.
Nerlekar N, Brown AJ, Muthalaly RG, Talman A, Hettige T, Cameron JD, et al. Association of epicardial adipose tissue and high-risk plaque characteristics: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6:e006379.
Mahabadi AA, Balcer B, Dykun I, Forsting M, Schlosser T, Heusch G, et al. Cardiac computed tomography-derived epicardial fat volume and attenuation independently distinguish patients with and without myocardial infarction. PLoS ONE. 2017;12:e0183514.
Nguyen MT, Pham I, Valensi P, Rousseau H, Vicaut E, Laguillier-Morizot C, et al. Flow-mediated-paradoxical vasoconstriction is independently associated with asymptomatic myocardial ischemia and coronary artery disease in type 2 diabetic patients. Cardiovasc Diabetol. 2014;13:20.
Cosson E, Pham I, Valensi P, Pariès J, Attali J-R, Nitenberg A. Impaired coronary endothelium-dependent vasodilation is associated with microalbuminuria in patients with type 2 diabetes and angiographically normal coronary arteries. Diabetes Care. 2006;29:107–12.
Nitenberg A, Valensi P, Sachs R, Cosson E, Attali J-R, Antony I. Prognostic value of epicardial coronary artery constriction to the cold pressor test in type 2 diabetic patients with angiographically normal coronary arteries and no other major coronary risk factors. Diabetes Care. 2004;27:208–15.
Zobel EH, Christensen RH, Winther SA, Hasbak P, Hansen CS, von Scholten BJ, et al. Relation of cardiac adipose tissue to coronary calcification and myocardial microvascular function in type 1 and type 2 diabetes. Cardiovasc Diabetol. 2020;19:16.
Chen WJY, Danad I, Raijmakers PG, Halbmeijer R, Harms HJ, Lammertsma AA, et al. Effect of type 2 diabetes mellitus on epicardial adipose tissue volume and coronary vasomotor function. Am J Cardiol. 2014;113:90–7.
Gaborit B, Venteclef N, Ancel P, Pelloux V, Gariboldi V, Leprince P, et al. Human epicardial adipose tissue has a specific transcriptomic signature depending on its anatomical peri-atrial, peri-ventricular, or peri-coronary location. Cardiovasc Res. 2015;108:62–73.
Gaborit B, Sengenes C, Ancel P, Jacquier A, Dutour A. Role of epicardial adipose tissue in health and disease: a matter of fat? Compr Physiol. 2017;7:1051–82.
Acknowledgements
We thank Sylvain Guillaume and Adeline Digard from GE Healthcare, France, for providing the software to calculate EAT volume. Our thanks also to Jude Sweeney (Milan, Italy) for the English editing and revision of the manuscript.
Funding
Internal funding was provided by Assistance Publique-Hôpitaux de Paris and Paris 13 University.
Author information
Authors and Affiliations
Contributions
EC conceived and designed this study and had full access to all the study data. EC is responsible for the integrity of the data and the accuracy of the data analyses. IR, NB, SP and PYB collected the data. EC drafted the paper, with help from MTN, HB, PYB and PV. MTN performed the statistical analyses. All authors critically revised the manuscript for important intellectual content and gave final approval for publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In Jean Verdier hospital, and in general in the various Public Assistance Hospitals in Paris, all patients are informed at admission that their medical records may be used for research, unless they indicate their opposition. For the present study, no patient indicated opposition.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cosson, E., Nguyen, M.T., Rezgani, I. et al. Epicardial adipose tissue volume and myocardial ischemia in asymptomatic people living with diabetes: a cross-sectional study. Cardiovasc Diabetol 20, 224 (2021). https://doi.org/10.1186/s12933-021-01420-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-021-01420-5