Abstract
Background
Risk stratification of cardiovascular events in patients with type 2 diabetes mellitus (T2DM) has not been established. Coronary artery calcium score (CACS) and non-alcoholic fatty liver disease (NAFLD) are independently associated with cardiovascular events in T2DM patients. This study examined the incremental prognostic value of NAFLD assessed by non-enhanced computed tomography (CT) in addition to CACS and Framingham risk score (FRS) for cardiovascular events in T2DM patients.
Methods
This prospective pilot study included 529 T2DM outpatients with no history of cardiovascular disease who underwent CACS measurement because of suspected coronary artery disease. NAFLD was defined on CT images as a liver:spleen attenuation ratio < 1.0. Cardiovascular events were defined as cardiovascular death, nonfatal myocardial infarction, late coronary revascularization, nonfatal stroke, or hospitalization for heart failure.
Results
Among 529 patients (61% men, mean age 65 years), NAFLD was identified in 143 (27%). Forty-four cardiovascular events were documented during a median follow-up of 4.4 years. In multivariate Cox regression analysis, NAFLD, CACS, and FRS were associated with cardiovascular events (hazard ratios and 95% confidence intervals 5.43, 2.82–10.44, p < 0.001; 1.56, 1.32–1.86, p < 0.001; 1.23, 1.08–1.39, p = 0.001, respectively). The global χ2 score for predicting cardiovascular events increased significantly from 27.0 to 49.7 by adding NAFLD to CACS and FRS (p < 0.001). The addition of NAFLD to a model including CACS and FRS significantly increased the C-statistic from 0.71 to 0.80 (p = 0.005). The net reclassification achieved by adding CACS and FRS was 0.551 (p < 0.001).
Conclusions
NAFLD assessed by CT, in addition to CACS and FRS, could be useful for identifying T2DM patients at higher risk of cardiovascular events.
Similar content being viewed by others
Background
The prevalence of type 2 diabetes mellitus (T2DM) has been increasing rapidly worldwide [1]. T2DM is associated with a two- to four-fold increased risk of cardiovascular events compared with non-T2DM subjects [2, 3]. The prevention of cardiovascular events in T2DM patients has thus become a major concern. Although several clinical risk scores for predicting cardiovascular events have been proposed, there is currently no widely used risk stratification for T2DM patients. Previous studies showed that coronary artery calcium score (CACS) determined by coronary computed tomography (CT) provided additional information on cardiovascular events in T2DM patients beyond that provided by the commonly used Framingham risk score (FRS) [4, 5]. The latest American Heart Association and American College of Cardiology (AHA/ACC) guidelines for the primary prevention of atherosclerotic cardiovascular disease allowed the use of CACS in intermediate-risk patients if the risk level was uncertain [6]. Thus, CACS could be a useful factor for determining cardiovascular risk in patients with T2DM.
Growing evidence suggests that non-alcoholic fatty liver disease (NAFLD) is associated with cardiovascular events independently of established cardiovascular risk factors [7,8,9]. NAFLD is a frequent comorbidity of metabolic syndrome and T2DM [10]. Previous studies showed that metabolic syndrome and T2DM might be predictors of vascular damage [11, 12], and complex and bidirectional associations have been demonstrated between NAFLD and metabolic syndrome and T2DM [13]. We recently reported on the prognostic value of NAFLD assessed by non-enhanced CT in patients with suspected coronary artery disease who underwent coronary CT angiography [14], highlighting the benefits of concomitant assessment of liver fat content during the acquisition of coronary CT angiography to detect patients at higher risk of cardiovascular events.
We therefore hypothesized that the assessment of NAFLD using non-enhanced CT, in addition to CACS and FRS, might improve risk stratification for cardiovascular events in T2DM patients. We tested this hypothesis in a cohort of patients with suspected coronary artery disease who underwent CACS measurement, with the aim of evaluating the additional prognostic value of NAFLD compared with CACS and FRS in T2DM patients.
Methods
Study population and data collection
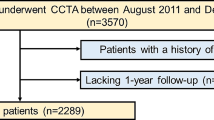
Patient enrollment in this study is shown in Fig. 1. This prospective study enrolled 529 Japanese outpatients with T2DM from August 2011 to December 2016. The patients had no history of cardiovascular disease but had been referred to our hospital with suspected coronary artery disease. CACS was measured in 172 asymptomatic patients for risk stratification by evaluating coronary atherosclerosis, and in the remaining 357 patients with atypical symptoms [n = 44] or no symptoms [n = 313] because of abnormalities in rest or stress electrocardiograms. No patients had any history of cardiovascular diseases, including coronary artery disease, heart failure, or cerebrovascular disease. Patients were excluded if they consumed > 20 g of alcohol per day, had known liver disease, were using oral corticosteroids or amiodarone, or had a coexisting active tumor. All the patients underwent blood tests, measurement of CACS, and abdominal CT on the same day.
Assessment of coronary calcification
CT imaging was performed using a Somatom Definition Flash scanner (Siemens Medical Solutions, Erlangen, Germany). CACS was measured using the following parameters: 120 kV, 150 mA, and 3-mm thickness. CACS was calculated using an automated computerized system (Virtual Place, Raijin; AZE Inc., Tokyo, Japan) and the Agatston method, which involved multiplying the area of each calcified plaque by a density factor determined by the peak pixel intensity within the plaque. The plaque-specific scores for all the slices were added together. The density factor was 1, 2, 3, or 4 for plaques with peak intensities of 130–199, 200–299, 300–399, and ≥ 400 Hounsfield units (HU), respectively [15]. In addition, patients were divided into three groups according to CACS: CACS 0, CACS (1–99), and CACS (≥ 100).
Assessment of visceral adipose tissue and NAFLD
Abdominal non-contrast CT scans were carried out alongside cardiac CT, at a level including the liver, spleen, and umbilicus. The visceral adipose tissue area was assessed using a semi-automatic segmentation technique at the umbilical level [16]. Hepatic and splenic Hounsfield attenuations were measured using the maximum circular regions of interest in the liver and spleen (at least 1 cm2) [17]. Regions of interests in the liver were located at two segments (right anterior and right posterior) by avoiding the inclusion of large vessels or biliary structures [17]. The liver:spleen attenuation ratio was calculated using the mean HU measurement of the two right liver lobe regions of interest. In this study, we defined hepatic steatosis as a liver:spleen attenuation ratio < 1.0 [18]. NAFLD was finally diagnosed after other causes of hepatic steatosis were ruled out.
Assessment of other risk factors
Hypertension was defined as a seated blood pressure > 140/90 mmHg or current treatment with antihypertensive medication. Dyslipidemia was defined as one or more of the following: serum triglycerides ≥ 150 mg/dL, high-density lipoprotein cholesterol < 40 mg/dL, low-density lipoprotein cholesterol ≥ 140 mg/dL, or current treatment with a lipid-lowering drug. Smoking status was defined as currently smoking or not smoking. Obesity was defined as a body mass index ≥ 25 kg/m2. FRS was calculated according to the algorithm presented by Wilson et al. to estimate the 10-year risk of a coronary heart disease event [19]. In addition, patients were classified into three groups according to the European Society of Cardiology recommendations as very-high, high, or moderate risk [20].
Outcomes and follow-up
The patients were followed up prospectively from the date of CT. Clinical follow-up information was obtained by review of medical records or telephone interviews by attending physicians. The study endpoint was cardiovascular events defined as cardiovascular death, nonfatal myocardial infarction, late coronary revascularization, nonfatal stroke, or hospitalization due to heart failure. The diagnosis of myocardial infarction was based on the criteria of typical acute chest pain and persistent ST-segment elevation or positive cardiac enzymes. Late coronary revascularization was defined as percutaneous coronary intervention or coronary artery bypass grafting as indicated by the treating physician due to stable angina with a newly positive functional test. Patients with scheduled revascularization within 90 days of the CACS measurement were not counted as events and were censored at the time of first revascularization. Hospitalization for heart failure was defined as any unplanned stay overnight or longer in a hospital environment, for which heart failure was the principal reason for admission. Nonfatal stroke was defined as sudden-onset non-convulsive and focal neurological deficit persisting for > 24 h.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation or median with interquartile range. Dichotomous variables were expressed as number and percentage. Differences in continuous variables between two groups were analyzed by Student’s t-test or Mann–Whitney U-test, as appropriate. Categorical data were compared by χ2 tests. In subsequent analysis, triglyceride data were log-transformed because they did not show a normal distribution. Similarly, the distribution of Agatston score data was also highly skewed, and CACS was therefore log-transformed after adding 1 to all calcium scores to manage values of 0 (log[CACS + 1]). Kaplan–Meier curves were used to estimate cumulative rates of cardiovascular events. Differences between time-to-event curves were compared by log-rank tests. Annual event rates were calculated by dividing the 4-year Kaplan–Meier event rates by 4 and comparing them. The effects of variables on cardiovascular events were analyzed by Cox proportional hazard analysis, and the results were reported as hazard ratios (HR) with 95% confidence intervals (CI). The incremental value of NAFLD was assessed by global χ2 tests and receiver operating characteristic (ROC) curve analysis. C-statistics were calculated from the ROC curves and compared using the Delong test. The category-free net reclassification improvement was also calculated. All reported p values were two-sided and p < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS statistical software (version 24; IBM Corp., Armonk, NY, USA) and the R statistical package (version 3.5.2; R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
The mean age of the study population was 65 years, 324 (61%) patients were men, and the median CACS was 63. Overall, 143 (27%) patients had CT evidence of NAFLD. The baseline characteristics of patients with and without NAFLD are shown in Table 1. Patients with NAFLD were younger (p < 0.001) and had a higher body mass index (p < 0.001) and visceral adipose tissue area (p < 0.001), and higher prevalences of dyslipidemia (p = 0.021) and obesity (p < 0.001) compared with patients without NAFLD. The proportion of very-high-risk patients was greater in patients with NAFLD than in patients without NAFLD (p = 0.003). Oral anti-hyperglycemic drugs were more frequent among patients with NAFLD. Patients with NAFLD also had higher levels of liver enzymes (p < 0.001) and triglycerides (p < 0.001), and lower levels of high-density lipoprotein cholesterol (p < 0.001). There was a significant difference in CACS between the two groups with higher CACS among non-NAFLD patients (p = 0.002). The mean dose-length product for abdominal CT was 251 mGy cm, and the effective dose for each imaging modality was 3.77 mSv, using a conversion coefficient of 0.015.
Outcome data
Forty-six patients (11 NAFLD, 35 non-NAFLD) with scheduled revascularization within 90 days of the index CT were censored at the time of revascularization. Forty-four cardiovascular events were documented during a median follow-up of 4.4 years (23 events in NAFLD patients: 1 cardiovascular death, 5 stroke, 5 myocardial infarction, 10 late revascularization, 2 heart failure; 21 events in non-NAFLD patients: 3 stroke, 7 myocardial infarction, 8 late revascularization, 3 heart failure). Kaplan–Meier curves showed the cumulative event-free survivals for cardiovascular events in patients stratified by CACS (0, 1–100 or ≥ 100), with or without NAFLD. The annual cardiovascular event rate in patients with NAFLD was significantly higher than that in patients without NAFLD (2.95% vs. 0.98%; p < 0.001) (Fig. 2a). In addition, patients were divided into three groups according CACS and compared in relation to the presence or absence of NAFLD (Fig. 2b–d). Patients with NAFLD and CACS ≥ 100 had a significantly higher incidence of cardiovascular events. The annual rates of cardiovascular events in patients with CACS 0 with and without NAFLD were very low and similar in both groups (0.00% vs. 0.30%; p = 0.513) (Fig. 2b). The annual rates of cardiovascular events in patients with CACS 1–99 and ≥ 100 were significantly higher in NAFLD compared with non-NAFLD patients (2.25% vs. 0.33%; p = 0.024, Fig. 2c; and 6.40% vs. 1.78%; p < 0.001, Fig. 2d, respectively). As shown in Table 2, univariate Cox regression analysis identified presence of NAFLD, CACS, and FRS as factors associated with cardiovascular events. Furthermore, multivariate Cox regression analysis identified the presence of NAFLD, CACS, and FRS as associated with cardiovascular events (HR, 95% CI 5.43, 2.82–10.44, p < 0.001; 1.56, 1.32–1.86, p < 0.001; 1.23, 1.08–1.39, p = 0.001, respectively).
Kaplan–Meier curves showing cumulative incidence of cardiovascular events. Kaplan–Meier curves of cardiovascular events presented according to a presence or absence of NAFLD, and b–d presence or absence of NAFLD according to CACS categories. a All patietnts. b Patients wigh CACS 0. c Patients with CACS 1–99. d Patients with CACS ≥ 100. CACS coronary artery calcium score, NAFLD non-alcoholic fatty liver disease
Comparison of predictive performances for cardiovascular events
We investigated the incremental value of adding NAFLD compared with CACS and FRS alone for predicting cardiovascular events. The global χ2 score and ROC curve analysis were calculated to assess the incremental predictive value of NAFLD. Adding NAFLD to log (CACS + 1) and FRS significantly increased the global χ2 score from 27.0 to 49.7 (p < 0.001) (Fig. 3a). The results of ROC analysis comparing the area under the curve for each group are shown in Fig. 3b. Adding NAFLD significantly increased the C-statistic of Model 1 (FRS + log [CACS + 1]) from 0.71 to 0.80 (p = 0.005). The net reclassification index achieved by adding log (CACS + 1) and FRS was 0.551 (p < 0.001). The addition of NAFLD to CACS and FRS thus improved the predictability of cardiovascular events.
Discussion
This study demonstrated that the presence of NAFLD in non-enhanced CT images, in addition to CACS and FRS, improved the risk classification of cardiovascular events in T2DM patients. However, this study was conducted in a cohort of T2DM patients with suspected coronary artery disease, and further studies are needed to determine if the results apply to all T2DM patients.
Several lines of evidence have shown that NAFLD is associated with an increased risk of cardiovascular events in T2DM patients. Lee et al. showed that NAFLD was independently associated with progression of carotid intima-media thickness, as a well-established surrogate marker of subclinical atherosclerosis, in T2DM patients [21]. In an observational study of 2103 T2DM patients, NAFLD was associated with an increased incidence of cardiovascular events after adjustment for multiple risk factors (HR 1.96, 95% CI 1.4–2.7) [22]. However, the mechanisms by which NAFLD increases the risk of cardiovascular events are complex and not fully understood. A previous study showed that the histological severity of NAFLD was associated with increased arterial stiffness and endothelial dysfunction [23]. In addition, inflammatory cytokines increased in line with the severity of liver disease in NAFLD patients [24]. The presence of systemic inflammation promoted by cytokines secreted from the liver leads to endothelial dysfunction, altering vascular tone and enhancing vascular plaque formation. This mechanism was supported by a clinical study that found a significant association between the severity of NAFLD and both surrogate markers of atherosclerosis and an increased risk of cardiovascular mortality in NAFLD patients [25,26,27,28].
CACS is a well-established surrogate marker of subclinical coronary artery atherosclerotic plaque burden, which can predict risk beyond the established cardiovascular risk score. Budoff et al. reported that CACS was independently and strongly associated with cardiovascular events, and CACS > 100 signified at least a 7.5% 10-year risk of cardiovascular events regardless of age, sex, or ethnicity among 6814 subjects from the general population [29]. CACS is also used to predict cardiovascular risk in T2DM patients, with elevated CACS in T2DM compared with non-T2DM subjects [30]. The Diabetes Heart Study comprising 1123 T2DM patients demonstrated that CACS predicted cardiovascular events more accurately than FRS [4]. In addition, the 2019 AHA/ACC guidelines for the primary prevention of atherosclerotic cardiovascular disease included the measurement of CACS for patients in intermediate-risk groups [6]. These data support the possible use of CACS as a means of assessing risk for cardiovascular outcomes in T2DM patients.
Hepatic steatosis has been reportedly associated with the presence of coronary artery calcium in some studies [31,32,33]. In addition, Sung et al. reported that hepatic steatosis was independently associated with coronary artery calcium progression [34]. However, the association between NAFLD and CACS has been inconsistent across studies, especially in T2DM patients. In a study of 213 participants with T2DM, NAFLD was not associated with CACS in patients with glycated hemoglobin A1c (HbA1c) < 7%, but was significantly associated with CACS in patients with HbA1c ≥ 7% [35]. In contrast, McKimme et al. reported no significant association between hepatic steatosis and CACS in T2DM patients [36]. Kim et al. reported an association between NAFLD and the prevalence of CACS, but this association was attenuated and was no longer significant after adjusting for insulin resistance [37]. The current study also found no association between NAFLD and higher CACS. Given that our results indicated that NAFLD and CACS were independent factors, the combination of NAFLD and CACS might improve the identification of T2DM patients at higher risk of cardiovascular events.
Ultrasonography is commonly used to assess liver fat infiltration in clinical practice; however, non-enhanced CT can also be useful for diagnosing liver fat. Previous studies showed that a liver:spleen ratio < 1.0 could be used effectively to diagnose the presence of liver fat with high reproducibility [18, 38, 39]. However, the prevalence of NAFLD in T2DM in this study was lower than that reported in other studies [40], in which NAFLD was mostly diagnosed by ultrasonography and magnetic resonance imaging. On the other hand however, our study applied CT, which was reported to have a lower sensitivity for diagnosing hepatic steatosis compared with ultrasonography and magnetic resonance imaging, especially in cases with mild steatosis (< 30% steatosis) [41]. The present study may thus have included patients with moderate to severe hepatic steatosis.
NAFLD is closely associated with obesity [22], and the prevalence of NAFLD has been reported to increase in parallel with increasing severity of obesity [42]. Recently, severe obesity among children and adolescents has recently become a significant public health concern [43]. Furthermore, pediatric fatty liver disease clustered with cardiometabolic risk factors, associated with an increase in subsequent adult cardiovascular mortality among adolescents with severe obesity [44]. A healthier diet and physical activity should thus be promoted among adolescents with obesity to mitigate the cardiometabolic risk.
This study had several limitations that need to be addressed. First, the number of patients and cardiovascular events were relatively small. In addition, our study population only consisted of Japanese patients with suspected coronary artery disease, and the results therefore cannot be applied directly to the T2DM population or to other ethnic groups. Second, the histological severity of liver damage was not confirmed in this study. However, CT is a useful tool for diagnosing NAFLD, without the complications associated with invasive methods. The association between CACS and histologic findings of NAFLD, such as ballooning grade, need to be evaluated in future studies. Third, we have no data about the duration of T2DM, which has been reported to increase the risk of cardiovascular events [45]. Fourth, longitudinal information on changes in medications, risk factor control, and changes in body mass index and lifestyle during the follow-up period was not available. Finally, FRS was originally developed in Western societies and is therefore not accurate in Asians. The Suita score has been proposed and validated as an alternative score for predicting coronary heart disease in Japanese populations [46]. The application of the Suita score instead of FRS did not affect the findings of this study (data not shown).
Conclusions
This study demonstrated the potential incremental prognostic value of NAFLD assessed by non-enhanced CT, in addition to CACS, for risk stratification of cardiovascular events in T2DM patients with suspected coronary artery disease. Further studies are needed to validate the applicability of NAFLD and CACS examination by non-enhanced CT to all T2DM patients.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CACS:
-
Coronary artery calcium score
- CT:
-
Computed tomography
- FRS:
-
Framingham risk score
- HbA1c:
-
Glycated hemoglobin A1c
- HU:
-
Hounsfield unit
- NAFLD:
-
Non-alcoholic fatty liver disease
- ROC:
-
Receiver operating characteristic
- T2DM:
-
Type 2 diabetes mellitus
References
Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414(6865):782–7.
Gu K, Cowie CC, Harris MI. Mortality in adults with and without diabetes in a national cohort of the U.S. population, 1971–1993. Diabetes Care. 1998;21(7):1138–45.
Emerging Risk Factors C, Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215–22.
Agarwal S, Cox AJ, Herrington DM, Jorgensen NW, Xu J, Freedman BI, Carr JJ, Bowden DW. Coronary calcium score predicts cardiovascular mortality in diabetes: diabetes heart study. Diabetes Care. 2013;36(4):972–7.
Mielke CH, Shields JP, Broemeling LD. Coronary artery calcium, coronary artery disease, and diabetes. Diabetes Res Clin Pract. 2001;53(1):55–61.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2019;140(11):e596-646.
Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363(14):1341–50.
Hamaguchi M, Kojima T, Takeda N, Nagata C, Takeda J, Sarui H, Kawahito Y, Yoshida N, Suetsugu A, Kato T, et al. Nonalcoholic fatty liver disease is a novel predictor of cardiovascular disease. World J Gastroenterol. 2007;13(10):1579–84.
Stepanova M, Younossi ZM. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin Gastroenterol Hepatol. 2012;10(6):646–50.
Non-alcoholic Fatty Liver Disease, Study G, Lonardo A, Bellentani S, Argo CK, Ballestri S, Byrne CD, Caldwell SH, Cortez-Pinto H, Grieco A, Machado MV, et al. Epidemiological modifiers of non-alcoholic fatty liver disease: focus on high-risk groups. Dig Liver Dis. 2015;47(12):997–1006.
Tuttolomondo A, Di Raimondo D, Di Sciacca R, Pecoraro R, Arnao V, Butta C, Licata G, Pinto A. Arterial stiffness and ischemic stroke in subjects with and without metabolic syndrome. Atherosclerosis. 2012;225(1):216–9.
Tuttolomondo A, Maida C, Pinto A. Diabetic foot syndrome: immune-inflammatory features as possible cardiovascular markers in diabetes. World J Orthop. 2015;6(1):62–76.
Lonardo A, Ballestri S, Guaraldi G, Nascimbeni F, Romagnoli D, Zona S, Targher G. Fatty liver is associated with an increased risk of diabetes and cardiovascular disease-evidence from three different disease models: NAFLD, HCV and HIV. World J Gastroenterol. 2016;22(44):9674–93.
Ichikawa K, Miyoshi T, Osawa K, Miki T, Nakamura K, Ito H. Prognostic Value of coronary computed tomographic angiography in patients with nonalcoholic fatty liver disease. JACC Cardiovasc Imaging. 2020;13(7):1628–30.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–32.
Yoshizumi T, Nakamura T, Yamane M, Islam AH, Menju M, Yamasaki K, Arai T, Kotani K, Funahashi T, Yamashita S, et al. Abdominal fat: standardized technique for measurement at CT. Radiology. 1999;211(1):283–6.
Ma X, Holalkere NS, Kambadakone RA, Mino-Kenudson M, Hahn PF, Sahani DV. Imaging-based quantification of hepatic fat: methods and clinical applications. Radiographics. 2009;29(5):1253–77.
Zeb I, Li D, Nasir K, Katz R, Larijani VN, Budoff MJ. Computed tomography scans in the evaluation of fatty liver disease in a population based study: the multi-ethnic study of atherosclerosis. Acad Radiol. 2012;19(7):811–8.
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–47.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, Federici M, Filippatos G, Grobbee DE, Hansen TB, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323.
Lee HH, Cho Y, Choi YJ, Huh BW, Lee BW, Kang ES, Park SW, Cha BS, Lee EJ, Lee YH, et al. Non-alcoholic steatohepatitis and progression of carotid atherosclerosis in patients with type 2 diabetes: a Korean cohort study. Cardiovasc Diabetol. 2020;19(1):81.
Targher G, Bertolini L, Rodella S, Tessari R, Zenari L, Lippi G, Arcaro G. Nonalcoholic fatty liver disease is independently associated with an increased incidence of cardiovascular events in type 2 diabetic patients. Diabetes Care. 2007;30(8):2119–21.
Tuttolomondo A, Petta S, Casuccio A, Maida C, Corte VD, Daidone M, Di Raimondo D, Pecoraro R, Fonte R, Cirrincione A, et al. Reactive hyperemia index (RHI) and cognitive performance indexes are associated with histologic markers of liver disease in subjects with non-alcoholic fatty liver disease (NAFLD): a case control study. Cardiovasc Diabetol. 2018;17(1):28.
du Plessis J, Korf H, van Pelt J, Windmolders P, Vander Elst I, Verrijken A, Hubens G, Van Gaal L, Cassiman D, Nevens F, et al. Pro-inflammatory cytokines but not endotoxin-related parameters associate with disease severity in patients with NAFLD. PLoS ONE. 2016;11(12):e0166048.
Mangla N, Ajmera VH, Caussy C, Sirlin C, Brouha S, Bajwa-Dulai S, Madamba E, Bettencourt R, Richards L, Loomba R. Liver stiffness severity is associated with increased cardiovascular risk in patients with type 2 diabetes. Clin Gastroenterol Hepatol. 2020;18(3):744-6.e741.
Ekstedt M, Hagstrom H, Nasr P, Fredrikson M, Stal P, Kechagias S, Hultcrantz R. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61(5):1547–54.
Kim JH, Moon JS, Byun SJ, Lee JH, Kang DR, Sung KC, Kim JY, Huh JH. Fatty liver index and development of cardiovascular disease in Koreans without pre-existing myocardial infarction and ischemic stroke: a large population-based study. Cardiovasc Diabetol. 2020;19(1):51.
Idilman IS, Akata D, Hazirolan T, Doganay Erdogan B, Aytemir K, Karcaaltincaba M. Nonalcoholic fatty liver disease is associated with significant coronary artery disease in type 2 diabetic patients: a computed tomography angiography study 2. J Diabetes. 2015;7(2):279–86.
Budoff MJ, Young R, Burke G, Jeffrey Carr J, Detrano RC, Folsom AR, Kronmal R, Lima JAC, Liu KJ, McClelland RL, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the multi-ethnic study of atherosclerosis (MESA). Eur Heart J. 2018;39(25):2401–8.
Raggi P, Shaw LJ, Berman DS, Callister TQ. Prognostic value of coronary artery calcium screening in subjects with and without diabetes. J Am Coll Cardiol. 2004;43(9):1663–9.
Sung KC, Wild SH, Kwag HJ, Byrne CD. Fatty liver, insulin resistance, and features of metabolic syndrome: relationships with coronary artery calcium in 10,153 people. Diabetes Care. 2012;35(11):2359–64.
Chhabra R, O’Keefe JH, Patil H, O’Keefe E, Thompson RC, Ansari S, Kennedy KF, Lee LW, Helzberg JH. Association of coronary artery calcification with hepatic steatosis in asymptomatic individuals. Mayo Clin Proc. 2013;88(11):1259–65.
Kim D, Choi SY, Park EH, Lee W, Kang JH, Kim W, Kim YJ, Yoon JH, Jeong SH, Lee DH, et al. Nonalcoholic fatty liver disease is associated with coronary artery calcification. Hepatology. 2012;56(2):605–13.
Sung KC, Ryu S, Lee JY, Lee SH, Cheong ES, Wild SH, Byrne CD. Fatty liver, insulin resistance, and obesity: relationships with increase in coronary artery calcium over time. Clin Cardiol. 2016;39(6):321–8.
Kwak MS, Yim JY, Kim D, Park MJ, Lim SH, Yang JI, Chung GE, Kim YS, Yang SY, Kim MN, et al. Nonalcoholic fatty liver disease is associated with coronary artery calcium score in diabetes patients with higher HbA1c. Diabetol Metab Syndr. 2015;7:28.
McKimmie RL, Daniel KR, Carr JJ, Bowden DW, Freedman BI, Register TC, Hsu FC, Lohman KK, Weinberg RB, Wagenknecht LE. Hepatic steatosis and subclinical cardiovascular disease in a cohort enriched for type 2 diabetes: the Diabetes Heart Study. Am J Gastroenterol. 2008;103(12):3029–35.
Kim MK, Ahn CW, Nam JS, Kang S, Park JS, Kim KR. Association between nonalcoholic fatty liver disease and coronary artery calcification in postmenopausal women. Menopause. 2015;22(12):1323–7.
Piekarski J, Goldberg HI, Royal SA, Axel L, Moss AA. Difference between liver and spleen CT numbers in the normal adult: its usefulness in predicting the presence of diffuse liver disease. Radiology. 1980;137(3):727–9.
Bydder GM, Chapman RW, Harry D, Bassan L, Sherlock S, Kreel L. Computed tomography attenuation values in fatty liver. J Comput Tomogr. 1981;5(1):33–5.
Lee YH, Cho Y, Lee BW, Park CY, Lee DH, Cha BS, Rhee EJ. Nonalcoholic fatty liver disease in diabetes. Part I: epidemiology and diagnosis. Diabetes Metabol J. 2019;43(1):31–45.
Bohte AE, van Werven JR, Bipat S, Stoker J. The diagnostic accuracy of US, CT, MRI and 1H-MRS for the evaluation of hepatic steatosis compared with liver biopsy: a meta-analysis. Eur Radiol. 2011;21(1):87–97.
Anderson EL, Howe LD, Jones HE, Higgins JP, Lawlor DA, Fraser A. The prevalence of non-alcoholic fatty liver disease in children and adolescents: a systematic review and meta-analysis. PLoS ONE. 2015;10(10):e0140908.
Bendor CD, Bardugo A, Pinhas-Hamiel O, Afek A, Twig G. Cardiovascular morbidity, diabetes and cancer risk among children and adolescents with severe obesity. Cardiovasc Diabetol. 2020;19(1):79.
Twig G, Yaniv G, Levine H, Leiba A, Goldberger N, Derazne E, Ben-Ami Shor D, Tzur D, Afek A, Shamiss A, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med. 2016;374(25):2430–40.
Fox CS, Sullivan L, D’Agostino RB, Wilson PW, Framingham Heart S. The significant effect of diabetes duration on coronary heart disease mortality: the Framingham Heart Study. Diabetes Care. 2004;27(3):704–8.
Nishimura K, Okamura T, Watanabe M, Nakai M, Takegami M, Higashiyama A, Kokubo Y, Okayama A, Miyamoto Y. Predicting coronary heart disease using risk factor categories for a Japanese urban population, and comparison with the framingham risk score: the suita study. J Atheroscler Thromb. 2014;21(8):784–98.
Acknowledgements
We thank Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript.
Funding
No funding to declare.
Author information
Authors and Affiliations
Contributions
KI and TM designed the study, analyzed the data, and wrote the manuscript. KO, TM, HT, KE, MY, YN, MY and KN collected the data. MH and HI assisted in data interpretation and manuscript revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of Okayama University Hospital and conducted in accordance with the principles contained within the Declaration of Helsinki. All patients enrolled in the study provided written informed consent.
Consent for publication
Not applicable.
Competing interests
We declare that we have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ichikawa, K., Miyoshi, T., Osawa, K. et al. Prognostic value of non-alcoholic fatty liver disease for predicting cardiovascular events in patients with diabetes mellitus with suspected coronary artery disease: a prospective cohort study. Cardiovasc Diabetol 20, 8 (2021). https://doi.org/10.1186/s12933-020-01192-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-020-01192-4