Abstract
Background
Reactive hyperemia-peripheral arterial tonometry (RH-PAT) is a noninvasive and simple test for evaluating the endothelial function. There has been sparse evidence on the usefulness of the RH-PAT index (RHI) in predicting future cardiovascular diseases among diabetic patients.
Methods
Asymptomatic diabetic patients with albuminuria were selected; their medical history and laboratory findings were evaluated every 3 to 4 months, respectively. The primary outcome was a composite of three-point major adverse cardiovascular events (3-point MACE): death from cardiovascular causes, acute coronary events, or nonfatal stroke. On the contrary, secondary outcomes included a composite of 3-point MACE, hospitalization for heart failure, or chronic kidney disease (CKD) progression. RHI was measured using the Endo-PAT2000 at the baseline. RHI < 1.67 was considered to indicate peripheral endothelial dysfunction (PED).
Results
In total, 149 subjects were included (mean age, 61.8 ± 9.2 years; duration of diabetes was 12 years). During the follow-up period (median, 49.7 months), of the 149 subjects, primary outcomes were detected in 12 (1 [2.3%] and 11 [10.5%] of those without and with PED, respectively). The presence of PED in baseline measurements significantly increased both primary and secondary outcomes, following adjustment for age, sex, hypertension, glycated hemoglobin, low-density lipoprotein cholesterol, triglyceride, systolic blood pressure, baseline estimated glomerular filtration rate, overt proteinuria, duration of diabetes, premedical history of ischemic events, anti-platelet agents, and smoking history (hazard ratio [HR]: 10.95; 95% confidence interval CI 1.00–119.91 for the primary outcome; HR, 4.12; 95% CI 1.37–12.41 for secondary outcome). In addition, PED could predict secondary outcomes independent of the risk score according to the American College of Cardiology/American Heart Association (HR: 3.24; 95% CI 1.14–9.17).
Conclusions
PED can independently predict future cardiovascular events among diabetic patients with albuminuria.
Similar content being viewed by others
Background
The leading cause of death in diabetic patients is atherosclerotic cardiovascular disease (ASCVD) [1]. However, intensive interventions targeting multifactorial ASCVD risk factors in the diabetic population have decreased vascular complications and mortality rates, [2] which weakened the prediction power of risk prediction based on traditional ASCVD risk factors [3, 4]. Currently, no risk scoring system has been developed based on diabetic patients on optimal medical treatment.
Reactive hyperemia-peripheral arterial tonometry (RH-PAT) is a simple, noninvasive, automatic test for evaluating the endothelial function [5, 6]. RH-PAT index (RHI) has been reported to be appropriately correlated with flow-mediated dilatation [5] and endothelin-1,[7] which are reliable markers of endothelial function. As RHI directly reflects endothelial function, it might estimate the residual ASCVD risk in diabetic subjects under appropriate medical treatment. Furthermore, endothelial dysfunction precedes atherosclerosis, [8] and RHI can predict the presence of ASCVD itself [9, 10]. Prospective studies confirmed that low levels of RHI could predict future cardiovascular events independently in the general population [11, 12]. However, there has been sparse evidence on the predictability of RHI in addition to conventional risk factors for future ASCVD among diabetic patients. Only a small-sized cross-sectional study [13] and a prospective study (less than 2 years) [14] reported no differences in RHI between the diabetic patients with and without coronary artery disease (CAD).
Diabetes itself is an important risk factor for ASCVD [14]. As albuminuria is a well-known risk factor for endothelial dysfunction [15] and ASCVD, [16] diabetic subjects with albuminuria consequently have a high risk of ASCVD. In this study, asymptomatic diabetic patients with albuminuria had their RHI levels evaluated, and future cardiovascular events were prospectively assessed. In addition, it was investigated whether RHI can provide any information alongside established ASCVD risk factors including Pooled Cohort Equations (PCE) for ASCVD according to the American College of Cardiology/American Heart Association [17].
Methods
Study subjects
This was a prospective cohort study of type 2 diabetic patients with albuminuria. Eligible patients with type 2 diabetes were: (i) ≥ 18 years of age, (ii) urinary albumin-to-creatinine ratio (ACR) ≥ 30 mg of albumin per gram of creatinine; and (iii) estimated glomerular filtration rate (eGFR) ≥ 30/min/1.73 m2 as recommended by the Modification of Diet in Renal Disease (MDRD) criteria [18]. Patients were excluded if they had (i) a recent history of myocardial infarction, cerebral infarction, or hospitalization due to heart failure less than 3 months before the enrollment, (ii) typical anginal pain aggravated by exercise, (iii) any chest discomfort accompanied with dyspnea, or (iv) grade 3 hypertension (systolic blood pressure (SBP) ≥ 180 mmHg or diastolic blood pressure (DBP) ≥ 110 mmHg) [19].
The cohort subjects were prospectively enrolled, and their RHI levels were measured within 3 months of enrollment. Their medical history and laboratory findings were followed every 3 or 4 months; cardiovascular and renal outcome events and deaths were prospectively monitored. The protocol was approved by the Institutional Review Board of the Seoul National University Boramae Medical Center, and written informed consent was obtained from all participants.
Measurement of reactive hyperemic index
RHI was measured using the Endo-PAT2000 (Itamar Medical Ltd., Caesarea, Israel) similar to other previous studies [20, 21]. Briefly, after resting for at least 15 min, the pressure cuff on the forearm was inflated and maintained at 50 mmHg above the SBP to occlude the brachial artery. The cuff was deflated 5 min later, and RHI was automatically calculated by an internal algorithm based on pulse wave amplitude at the baseline and 1 min after deflation. RHI < 1.67 was considered to indicate peripheral arterial endothelial dysfunction (PED) [20, 21].
Study outcomes
The primary outcome was a composite of three major adverse cardiovascular events (3-point MACE) which were defined as follows: death from cardiovascular causes, acute coronary events, or nonfatal stroke. Secondary outcomes included a composite of 3-point MACE, hospitalization for heart failure, or chronic kidney disease (CKD) progression.
An acute coronary event was defined as hospitalization for unstable angina or nonfatal myocardial infarction. The onset or worsening of CKD was defined as follows: (i) a decrease from baseline in eGFR by 30% or more to an eGFR < 60 mL/min per 1.73 m2, (ii) an eGFR < 30 mL/min per 1.73 m2, (iii) the initiation of renal-replacement therapy, or (iv) death from renal disease.
Evaluation for ASCVD risk factors
Plasma glucose and lipid concentrations were measured enzymatically using a Hitachi Automatic Analyzer B2400 (Hitachi, Tokyo, Japan), and glycated hemoglobin (HbA1c) levels were measured using a 200FR chemistry analyzer (Toshiba, Tokyo, Japan). Serum creatinine levels were measured every 3–6 months using an assay based on isotope dilution mass spectrometry. The patients’ eGFR was calculated using the MDRD Study equation [18].
Sex-specific PCE for non-Hispanic whites that estimates the 10-year risk of ASCVD according to the American College of Cardiology/American Heart Association [17] was also used to adjust conventional ASCVD risk, as no specific equation exists for Koreans.
Statistical analysis
All data were analyzed using IBM SPSS Statistic 20.0 for Windows (IBM Inc., Chicago, IL, USA). Demographic and clinical data between those with and without PED were compared with the Mann–Whitney test, an independent t test, and a Chi square test. The Cox proportional hazards model was used to investigate the predicting factors for primary or secondary outcomes with adjustments for sex, age, hypertension, HbA1c, low-density lipoprotein (LDL) cholesterol, triglyceride, overt proteinuria (ACR ≥ 300 mg of albumin per gram of creatinine), baseline e-GFR, premedical history of ischemic events, duration of diabetes, anti-platelet agents, and smoking history. The independent determining factors for PED (RHI < 1.67) were investigated using backward multivariable logistic regression. The level of significance was set at P < 0.05.
In the previous study, 16% of diabetic subjects with albuminuria experienced MACE during 3.1 years of follow-up [22]; and previous studies based on general population reported approximately 20% difference in ASCVD event according to the absence or presence of PED [11, 12]. With 0.05, 0.20 and 0.80 of α error, β error, and power, respectively, 148 subjects were needed for the study.
Results
Baseline characteristics
In total, 149 subjects were included; the median follow-up period was 49.7 months (range: 3–69 months). At the baseline, mean age was 61.8 ± 9.2 years, and median duration of diabetes was 12 years (interquartile range [IQR], 7–17 years) (Table 1). Among them, 105 subjects (70.5%) had PED. These subjects were significantly older than those without PED (62.8 ± 8.7 years vs. 59.4 ± 9.9; P = 0.043). Despite no difference in the prevalence of hypertension or the proportion of subjects on angiotensin receptor blocker (ARB) or angiotensin-converting enzyme inhibitor (ACEI) between the two groups, subjects with PED experienced low SBP and DBP compared to those without PED (Table 1). The proportion of subjects taking statin at a moderate dose or more [23] was 67.6% and 75.0% in those with and without PED, respectively (no difference between groups; P = 0.371). Overall, only 9 subjects took sodium-glucose cotransporter 2 (SGLT2) inhibitors, whereas no subject took glucagon-like peptide 1 receptor analogue (GLP1-RA) at the baseline (Table 1). No difference was observed in body mass index (BMI), HbA1c, lipid profile, eGFR, or ACR. The presence or absence of PED was not an indicator of previous vascular events; however, subjects with PED more frequently used anti-platelet agents than subjects with RHI ≥ 1.67 (52.4% vs. 31.8%; P = 0.022).
Determinants of the baseline RHI
To investigate the independent determinant of PED at the baseline, backward multivariable logistic regression was performed incorporating age, sex, BMI, HbA1c, SBP, DBP, hypertriglyceridemia, hypertension, smoking history, anti-platelet agents, and prescriptions of cilostazol or statin. In the final model, only age, SBP, hypertriglyceridemia, and smoking history showed a correlation (Additional file 1: Table S1). Age and current smoking were significantly associated with PED (odds ratio [OR], 1.06; 95% CI 1.02–1.11; P = 0.008; and OR, 2.97; 95% CI 1.15–7.63; P = 0.024, respectively). On the contrary, SBP showed a negative association with the risk of PED (OR 0.96; 95% CI 0.94–0.99; P = 0.006).
Future cardiorenal events according to RHI
During the follow-up period (median 49.7 months), primary outcomes were detected in 12 of 149 subjects (1 [2.3%] and 11 [10.5%] in those without and with PED, respectively; P = 0.093; Table 2). No mortality was associated with cardiovascular causes. Secondary outcomes were detected in 37 of 149 subjects (4 [9.1%] vs. 33 [31.4%] in those without and with PED, respectively; P = 0.004).
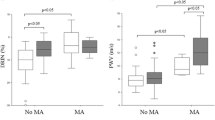
In unadjusted Cox-regression analysis, the presence of PED at the baseline did not increase the risk of the primary outcomes significantly (hazard ratio [HR], 4.62; 95% CI 0.60–35.79; P = 0.143). Subjects with PED experienced secondary outcomes more frequently than those without PED (HR, 3.45; 95% CI 1.22–9.75; P = 0.019; Table 2). After adjusting for age, sex, hypertension, HbA1c, LDL cholesterol, triglyceride, proteinuria, duration of diabetes, and premedical history of ischemic events, presence of PED increased both primary and secondary outcomes (Model 1 in Table 2). This trend persisted following additional adjustments for SBP, baseline e-GFR, anti-platelet agents, and smoking history for both primary (HR, 10.95; 95% CI 1.00–119.91; P = 0.050; Fig. 1a) and secondary outcomes (HR, 4.12; 95% CI 1.37–12.41; P = 0.012; Fig. 1b; Model 2 in Table 2).
Cumulative probability of primary and secondary outcomes according to peripheral arterial endothelial dysfunction (PED). Cox proportional hazards model was used to investigate the effect of PED (RHI < 1.67) on the primary and secondary outcome event rates during the follow-up period with adjustment for sex, age, hypertension, glycated hemoglobin (HbA1c), low density lipoprotein (LDL) cholesterol, triglyceride, overt proteinuria, baseline estimated glomerular filtration rate (e-GFR), premedical history of ischemic events, duration of diabetes, anti-platelet agents, and smoking history. Solid and dashed lines represent cumulative probability of a primary outcome composed of 3-point major adverse cardiovascular events (MACE), b secondary outcome composed of 3-point MACE, hospitalization for heart failure, or chronic kidney disease (CKD) progression, c acute coronary events, and d CKD progression in those with and without PED, respectively. RHI, reactive hyperemia index; MACE, major adverse cardiovascular event; CKD, chronic kidney disease; e-GFR, estimated glomerular filtration rate; CAC, coronary artery calcification; ASCVD, atherosclerotic cardiovascular disease; CAD, coronary artery disease; SBP, systolic blood pressure; DBP, diastolic blood pressure; MDRD, Modification of Diet in Renal Disease; PED, peripheral endothelial dysfunction; PCE, pooled Cohort Equations
Subsequent Cox-regression analysis incorporating PCE and PED confirmed PED as an independent risk factor for secondary outcomes (HR, 3.24; 95% CI 1.14–9.17; P = 0.027; Additional file 1: Table S2).
CKD progression was observed in 27 subjects during the follow-up period, which was associated with PED at the baseline in the fully adjusted model (HR, 3.26; 95% CI 1.01–10.50; P = 0.048; Model 2 in Table 2; Fig. 1). Among subjects experiencing secondary outcomes, those with CKD progression had significantly higher SBP (134.9 ± 15.6 mmHg vs. 118.9 ± 12.6 mmHg; P = 0.006) and lower eGFR (median eGFR, 61.2 vs. 82.1 mL/min/1.73 m2; P = 0.023) at the baseline than those without CKD progression. Notably, no difference in RHI at baseline was observed between them (Table 3).
Discussion
In this study, 149 diabetic patients with albuminuria (median duration of diabetes was 12 years) were followed for 49.7 months, and the primary outcomes, defined as 3-point MACE, were detected in 8.1% of study subjects. PED (RHI < 1.67) was an independent risk factor for developing primary outcomes following adjustments for age, sex, hypertension, HbA1c, LDL cholesterol, triglyceride, SBP, baseline e-GFR, overt proteinuria, duration of diabetes, premedical history of ischemic events, anti-platelet agents, and smoking history. Subjects with PED at baseline had 10.95 times higher incidence of primary outcomes during the follow-up period in the fully adjusted model.
Similarly, PED was an independent risk factor for CKD progression in this study; subjects with PED showed 3.26 times higher risk of CKD progression. CKD shares common risk factors and pathophysiological mechanisms with ASCVD [24,25,26]. The combined risk of ASCVD and CKD was increased 4.12 times by PED at the baseline.
Traditionally, diabetes is regarded as a CAD equivalent [14]. However, intensive interventions targeting multifactorial ASCVD risk factors in the diabetic population have decreased vascular complications and mortality rates [2]. This resulted in a substantial reduction in death from cardiovascular causes, [27, 28] and weakened the prediction power of risk prediction based on traditional ASCVD risk factors [3, 4]. The estimation of the 10-year risk of ASCVD according to the American College of Cardiology/American Heart Association by PCE [17] was developed based on subjects enrolled in the 1970s-1990s; before the 1990s, statin therapy was not available. Accordingly, PCE overestimates ASCVD risk in modern cohorts [29]. In this study, 69.8% of the study subjects took statin with moderate intensity or more [23] at the baseline, and their baseline LDL cholesterol was 81.0 mg/dL. Currently, there is no risk scoring system developed based on diabetic patients under multifactorial treatment.
As the RHI directly reflects endothelial function regardless of the presence or absence of traditional ASCVD risk factors [11, 12], it could estimate the residual ASCVD risk independent of well-known ASCVD risk factors in diabetic subjects. In this study, PED could predict primary outcome only after adjusting ASCVD risk factors, which might be a supporting evidence for the possible estimation of the residual ASCVD risk by RHI. However, Venuraju S et al. recently reported that RHI could not predict MACE in diabetic patients [30]. Similarly, no difference was reported in coronary artery calcification (CAC) according to PED [30]. However, only a total of 18 MACE was observed in < 2 years of follow-up, and too small number of events for a short period might weaken the statistical significance. In addition, a wide distribution of baseline CAC observed in the study subjects reflects heterogeneity in ASCVD risk at the baseline among subjects. This might result not only in no association between CAC and RHI but also in no difference in MACE rate during the study period according to the PED status. However, considering that CAC reflects subclinical atherosclerosis and is useful for predicting ASCVD in asymptomatic diabetic patients along with the established cardiovascular risk factors, [31, 32], the determination of ASCVD risk by PED in addition to CAC should be further investigated [33,34,35].
Low RHI was reported not only in diabetes [13, 36,37,38] but also in metabolic syndrome [39] and nonalcoholic fatty liver disease [40]. Diabetic patients demonstrated lower RHI levels than the general population [13, 36, 37]. In this study, low RHI was detected in approximately 70% of the study subjects (105 out of 149 subjects), which was relatively higher than previous studies based on the general population where this was observed in 23–27% of the study subjects [20, 21]. In previous studies including diabetic patients, the mean RHI was 1.69; [13] a finding similar to ours. This study included subjects with albuminuria. Albuminuria is a well-known risk factor of endothelial dysfunction [15] and ASCVD, [16] which might result in a prevalent low RHI in this study.
At the baseline, no difference was observed in HbA1c, according to RHI in this study. In diabetic subjects, low RHI level was reported to be associated with poor glycemic control status [13, 30, 38]; however, there has been some controversies regarding this [41]. In addition, the median HbA1c in this study was 7.2 (IQR, 6.7–7.8), a relatively fair level, which might result in a negative finding in the association between glycemic level and RHI. On the contrary, lower SBP, age, and smoking were independent risk factors for low RHI in this study. However, no difference was observed in the prevalence of hypertension or the use of antihypertensive medication according to RHI. There is supporting information for a positive correlation, [42, 43] and a negative correlation [39, 44] between blood pressure and RHI. Heterogeneity in clinical characteristics of study subjects among studies might cause a difference in the relationship between RHI and blood pressure. In addition, inconsistent correlations between RHI and well-known ASCVD risk factors have been reported not only in blood pressure [30, 39, 42, 44,45,46] but also in age [39, 47, 48]. Age is one of the most important risk factors for ASCVD; however, RHI has been reported to be positively correlated [39, 47] and negatively correlated [48] with age. The association between RHI and blood pressure and/or age should be further investigated in large sized independent studies.
Anti-diabetic medications such as SGLT2 inhibitors or GLP1-RA may influence the endothelial function, [49] which was not observed in this study. At the baseline, only a small number of patients enrolled in this study were taking SGLT2 inhibitors (5 of 105 and 4 of 44 in those with and without PED, respectively), whereas no subject was on GLP1-RA. This study enrolled subjects from March 2013 to January 2017; in addition, the prescription of SGLT2 inhibitors and dulaglutide (the only long-acting GLP1-RA available in Korea) commenced in the institution in 2015 and 2016, respectively.
Anti-platelet agents are similarly known to improve the endothelial function [50]. In this study, subjects in the PED group took anti-platelet medications more frequently than those without PED at the baseline. However, the cross-sectional nature of the comparison of the baseline characteristics according to the PED status cannot show causality, and older age might result in a greater rate of prescription in the PED group.
The main limitation of this study was a small sample size, which weakened the statistical significance in the analysis of each composite secondary endpoint. In addition, considering that the proportion of CKD progression in the secondary outcome was relatively large, the significant causal effect of PED on the secondary outcome should be interpreted with caution. Despite insufficient statistical significance, the trends of each composite secondary endpoint according to the baseline RHI were consistent. Future ASCVD risk associated with PED should be validated with larger studies. In addition, this result cannot be applied in diabetic subjects without albuminuria. Lastly, CAC has been recommended for ASCVD risk-stratification [31]. As the CAC was not measured, its clinical usefulness alongside that of RHI could not be evaluated.
Conclusions
RHI can independently predict future cardiovascular events among diabetic patients with albuminuria who are under treatment for conventional risk factors. Further studies encompassing a larger and diverse population are required for confirmation.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- ACR:
-
Albumin-to-creatinine ratio
- ACEI:
-
Angiotensin-converting enzyme inhibitor
- ARB:
-
Angiotensin receptor blocker
- ASCVD:
-
Atherosclerotic cardiovascular disease
- CAC:
-
Coronary artery calcification
- CAD:
-
Coronary artery disease
- CKD:
-
Chronic kidney disease
- DBP:
-
Diastolic blood pressure
- eGFR:
-
Estimated glomerular filtration rate
- GLP-1RA:
-
Glucagon-like peptide 1 receptor analogue
- LDL:
-
Low-density lipoprotein
- MACE:
-
Major adverse cardiovascular events
- PCE:
-
Pooled Cohort Equations
- PED:
-
Peripheral endothelial dysfunction
- RH-PAT:
-
Reactive hyperemia-peripheral arterial tonometry
- RHI:
-
Reactive hyperemia-peripheral arterial tonometry index
- SBP:
-
Systolic blood pressure
- SGLT2:
-
sodium-glucose cotransporter 2
References
Li S, Wang J, Zhang B, Li X, Liu Y. Diabetes mellitus and cause-specific mortality: a population-based study. Diabetes Metab J. 2019;43(3):319–41.
Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358(6):580–91.
Wackers FJ, Young LH, Inzucchi SE, Chyun DA, Davey JA, Barrett EJ, Taillefer R, Wittlin SD, Heller GV, Filipchuk N, et al. Detection of silent myocardial ischemia in asymptomatic diabetic subjects: the DIAD study. Diabetes Care. 2004;27(8):1954–61.
Scognamiglio R, Negut C, Ramondo A, Tiengo A, Avogaro A. Detection of coronary artery disease in asymptomatic patients with type 2 diabetes mellitus. J Am Coll Cardiol. 2006;47(1):65–71.
Kuvin JT, Patel AR, Sliney KA, Pandian NG, Sheffy J, Schnall RP, Karas RH, Udelson JE. Assessment of peripheral vascular endothelial function with finger arterial pulse wave amplitude. Am Heart J. 2003;146(1):168–74.
Nohria A, Gerhard-Herman M, Creager MA, Hurley S, Mitra D, Ganz P. Role of nitric oxide in the regulation of digital pulse volume amplitude in humans. J Appl Physiol (1985). 2006;101(2):545–8.
Nishiyama SK, Zhao J, Wray DW, Richardson RS. Vascular function and endothelin-1: tipping the balance between vasodilation and vasoconstriction. J Appl Physiol (1985). 2017;122(2):354–60.
Davignon J, Ganz P. Role of endothelial dysfunction in atherosclerosis. Circulation. 2004;109(23 Suppl 1):27–32.
Matsuzawa Y, Li J, Aoki T, Guddeti RR, Kwon TG, Cilluffo R, Widmer RJ, Gulati R, Lennon RJ, Lerman LO, et al. Predictive value of endothelial function by noninvasive peripheral arterial tonometry for coronary artery disease. Coron Artery Dis. 2015;26(3):231–8.
Matsuzawa Y, Sugiyama S, Sugamura K, Nozaki T, Ohba K, Konishi M, Matsubara J, Sumida H, Kaikita K, Kojima S, et al. Digital assessment of endothelial function and ischemic heart disease in women. J Am Coll Cardiol. 2010;55(16):1688–96.
Rubinshtein R, Kuvin JT, Soffler M, Lennon RJ, Lavi S, Nelson RE, Pumper GM, Lerman LO, Lerman A. Assessment of endothelial function by non-invasive peripheral arterial tonometry predicts late cardiovascular adverse events. Eur Heart J. 2010;31(9):1142–8.
Matsuzawa Y, Sugiyama S, Sumida H, Sugamura K, Nozaki T, Ohba K, Matsubara J, Kurokawa H, Fujisue K, Konishi M, et al. Peripheral endothelial function and cardiovascular events in high-risk patients. J Am Heart Assoc. 2013;2(6):e000426.
Gargiulo P, Marciano C, Savarese G, D’Amore C, Paolillo S, Esposito G, Santomauro M, Marsico F, Ruggiero D, Scala O, et al. Endothelial dysfunction in type 2 diabetic patients with normal coronary arteries: a digital reactive hyperemia study. Int J Cardiol. 2013;165(1):67–71.
Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339(4):229–34.
Pedrinelli R, Giampietro O, Carmassi F, Melillo E, Dell’Omo G, Catapano G, Matteucci E, Talarico L, Morale M, De Negri F, et al. Microalbuminuria and endothelial dysfunction in essential hypertension. Lancet. 1994;344(8914):14–8.
Mattock MB, Morrish NJ, Viberti G, Keen H, Fitzgerald AP, Jackson G. Prospective study of microalbuminuria as predictor of mortality in NIDDM. Diabetes. 1992;41(6):736–41.
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O’Donnell CJ, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S49–73.
Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F. Chronic kidney disease epidemiology C: using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145(4):247–54.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104.
Michelsen MM, Mygind ND, Pena A, Aziz A, Frestad D, Host N, Prescott E. Steering committee of the i PS: peripheral reactive hyperemia index and coronary microvascular function in women with no obstructive CAD: the iPOWER study. JACC Cardiovasc Imag. 2016;9(4):411–7.
Syvanen K, Korhonen P, Partanen A, Aarnio P. Endothelial function in a cardiovascular risk population with borderline ankle-brachial index. Vasc Health Risk Manag. 2011;7:97–101.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–28.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082–143.
Armstrong MJ, Adams LA, Canbay A, Syn WK. Extrahepatic complications of nonalcoholic fatty liver disease. Hepatology. 2014;59(3):1174–97.
Lonardo A, Nascimbeni F, Mantovani A, Targher G. Hypertension, diabetes, atherosclerosis and NASH: cause or consequence? J Hepatol. 2018;68(2):335–52.
Kim HY, Kim JK, Shin GG, Han JA, Kim JW. Association between abdominal obesity and cardiovascular risk factors in adults with normal body mass index: based on the sixth Korea National Health and Nutrition Examination Survey. J Obes Metab Syndr. 2019;28(4):262–70.
Gregg EW, Cheng YJ, Saydah S, Cowie C, Garfield S, Geiss L, Barker L. Trends in death rates among U.S. adults with and without diabetes between 1997 and 2006: findings from the National Health Interview Survey. Diabetes Care. 2012;35(6):1252–7.
Kim KJ, Kwon TY, Yu S, Seo JA, Kim NH, Choi KM, Baik SH, Choi DS, Kim SG, Park Y, et al. Ten-Year mortality trends for adults with and without diabetes mellitus in South Korea, 2003 to 2013. Diabetes Metab J. 2018;42(5):394–401.
DeFilippis AP, Young R, McEvoy JW, Michos ED, Sandfort V, Kronmal RA, McClelland RL, Blaha MJ. Risk score overestimation: the impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association-American College of Cardiology-Atherosclerotic Cardiovascular Disease risk score in a modern multi-ethnic cohort. Eur Heart J. 2017;38(8):598–608.
Venuraju S, Jeevarethinam A, Mehta VS, Ruano S, Dumo A, Nair D, Rosenthal M, Darko D, Cohen M, Rakhit R, et al. Predicting severity of coronary artery disease in patients with diabetes using endothelial function measured with peripheral arterial tonometry: PROCEED study. Angiology. 2019;70(7):613–20.
Anand DV, Lim E, Hopkins D, Corder R, Shaw LJ, Sharp P, Lipkin D, Lahiri A. Risk stratification in uncomplicated type 2 diabetes: prospective evaluation of the combined use of coronary artery calcium imaging and selective myocardial perfusion scintigraphy. Eur Heart J. 2006;27(6):713–21.
Venuraju SM, Lahiri A, Jeevarethinam A, Cohen M, Darko D, Nair D, Rosenthal M, Rakhit RD. Duration of type 2 diabetes mellitus and systolic blood pressure as determinants of severity of coronary stenosis and adverse events in an asymptomatic diabetic population: PROCEED study. Cardiovasc Diabetol. 2019;18(1):51.
Esper RJ, Nordaby RA. Cardiovascular events, diabetes and guidelines: the virtue of simplicity. Cardiovasc Diabetol. 2019;18(1):42.
Bosevski M, Borozanov V, Tosev S, Georgievska-Ismail L. Is assessment of peripheral endothelial dysfunction useful tool for risk stratification of type 2 diabetic patients with manifested coronary artery disease? Int J Cardiol. 2009;131(2):290–2.
Naka KK, Papathanassiou K, Bechlioulis A, Pappas K, Tigas S, Makriyiannis D, Antoniou S, Kazakos N, Margeli A, Papassotiriou I, et al. Association of vascular indices with novel circulating biomarkers as prognostic factors for cardiovascular complications in patients with type 2 diabetes mellitus. Clin Biochem. 2018;53:31–7.
Hahad O, Wild PS, Prochaska JH, Schulz A, Hermanns I, Lackner KJ, Pfeiffer N, Schmidtmann I, Beutel M, Gori T, et al. Endothelial function assessed by digital volume plethysmography predicts the development and progression of type 2 diabetes mellitus. J Am Heart Assoc. 2019;8(20):e012509.
Tuttolomondo A, Di Raimondo D, Casuccio A, Guercio G, Del Cuore A, Puleo MG, Della Corte V, Bellia C, Caronia A, Maida C, et al. Endothelial function, adipokine serum levels and white matter hyperintesities in subjects with diabetic foot syndrome. J Clin Endocrinol Metab. 2019;104:3920–30.
Tuttolomondo A, Casuccio A, Guercio G, Maida C, Del Cuore A, Di Raimondo D, Simonetta I, Di Bona D, Pecoraro R, Della Corte V, et al. Arterial stiffness, endothelial and cognitive function in subjects with type 2 diabetes in accordance with absence or presence of diabetic foot syndrome. Cardiovasc Diabetol. 2017;16(1):2.
Shen J, Poole JC, Topel ML, Bidulescu A, Morris AA, Patel RS, Binongo JG, Dunbar SB, Phillips L, Vaccarino V, et al. Subclinical vascular dysfunction associated with metabolic syndrome in African Americans and whites. J Clin Endocrinol Metab. 2015;100(11):4231–9.
Tuttolomondo A, Petta S, Casuccio A, Maida C, Corte VD, Daidone M, Di Raimondo D, Pecoraro R, Fonte R, Cirrincione A, et al. Reactive hyperemia index (RHI) and cognitive performance indexes are associated with histologic markers of liver disease in subjects with non-alcoholic fatty liver disease (NAFLD): a case control study. Cardiovasc Diabetol. 2018;17(1):28.
Heier M, Espeland CN, Brunborg C, Seljeflot I, Margeirsdottir HD, Hanssen KF, Fugelseth D, Dahl-Jorgensen K. Preserved endothelial function in young adults with type 1 diabetes. PLoS ONE. 2018;13(10):e0206523.
Kelly AS, Marlatt KL, Steinberger J, Dengel DR. Younger age is associated with lower reactive hyperemic index but not lower flow-mediated dilation among children and adolescents. Atherosclerosis. 2014;234(2):410–4.
Brant LC, Hamburg NM, Barreto SM, Benjamin EJ, Ribeiro AL. Relations of digital vascular function, cardiovascular risk factors, and arterial stiffness: the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) cohort study. J Am Heart Assoc. 2014;3(6):e001279.
Carnovale V, Paradis ME, Gigleux I, Ramprasath VR, Couture P, Jones PJ, Lamarche B, Couillard C. Correlates of reactive hyperemic index in men and postmenopausal women. Vasc Med. 2013;18(6):340–6.
Erqou S, Kip KE, Mulukutla SR, Aiyer AN, Reis SE. Endothelial dysfunction and racial disparities in mortality and adverse cardiovascular disease outcomes. Clin Cardiol. 2016;39(6):338–44.
Saito Y, Kitahara H, Nakayama T, Fujimoto Y, Kobayashi Y. Night-time blood pressure variability negatively correlated with reactive hyperemia index. Int J Cardiol. 2017;230:332–4.
Hamburg NM, Keyes MJ, Larson MG, Vasan RS, Schnabel R, Pryde MM, Mitchell GF, Sheffy J, Vita JA, Benjamin EJ. Cross-sectional relations of digital vascular function to cardiovascular risk factors in the Framingham Heart Study. Circulation. 2008;117(19):2467–74.
Yang WI, Park S, Youn JC, Son NH, Lee SH, Kang SM, Jang Y. Augmentation index association with reactive hyperemia as assessed by peripheral arterial tonometry in hypertension. Am J Hypertens. 2011;24(11):1234–8.
Kaur R, Kaur M, Singh J. Endothelial dysfunction and platelet hyperactivity in type 2 diabetes mellitus: molecular insights and therapeutic strategies. Cardiovasc Diabetol. 2018;17(1):121.
Husain S, Andrews NP, Mulcahy D, Panza JA, Quyyumi AA. Aspirin improves endothelial dysfunction in atherosclerosis. Circulation. 1998;97(8):716–20.
Acknowledgements
Not applicable.
Funding
This study was supported by Health Connect Research Fund (No. 16-2013-87).
Author information
Authors and Affiliations
Contributions
MKM designed the study and carried out subject recruitment. MKM and BKK analyzed the data and wrote the manuscript. WC assisted in study design, data interpretation and manuscript revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review board of the Seoul National University Boramae Medical Center (No.16-2013-87).
Consent for publication
The consent to publish was obtained from all participants in this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
Determinants for peripheral arterial endothelial dysfunction (PED). Table S2. Cox Proportional Hazards Analysis for Cardiovascular Events according to Peripheral Endothelial Dysfunction (PED).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Koo, B.K., Chung, WY. & Moon, M.K. Peripheral arterial endothelial dysfunction predicts future cardiovascular events in diabetic patients with albuminuria: a prospective cohort study. Cardiovasc Diabetol 19, 82 (2020). https://doi.org/10.1186/s12933-020-01062-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-020-01062-z