Abstract
Background
The diagnosis of diabetes has important clinic implications for the prevention and management of cardiometabolic disorders. We aimed to investigate the awareness, treatment and control of hypertension and dyslipidemia in previously-diagnosed and newly-diagnosed diabetes in Chinese adult population.
Methods
We conducted a cross-sectional survey in a nationally representative sample of 98658 Chinese adults aged 18 years or older in 2010, using a complex, multistage, probability sampling design. Glycemic status were defined according to the 2010 American Diabetes Association criteria. Hypertension was diagnosed by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Dyslipidemia was diagnosed by the 2004 National Cholesterol Education Program Adult Treatment Panel III.
Results
The weighted prevalence of hypertension and dyslipidemia gradually increased in adults with normal glucose regulation, prediabetes, newly-diagnosed diabetes and previously-diagnosed diabetes. Compared to newly-diagnosed diabetes patients, previously-diagnosed diabetes patients were more likely to be aware of hypertension (weighted percentage [95% confidence interval]: 55.2% [52.9%-57.5%] vs 37.6% [35.9%-39.3%]) and dyslipidemia (33.9% [31.8%-36.1%] vs 12.8% [11.7%-13.9%]), to receive blood pressure-lowing (43.7% [41.5%-46.0%] vs 27.5% [26.0%-29.0%]) and lipid-lowering (18.9% [17.2%-20.7%] vs 5.4% [4.6%-6.2%]) therapies, and to have controlled blood pressure (4.7% [3.5%-6.2%] vs 3.5% [2.6%-4.8%]) and lipid (15.9% [12.3%-20.3%] vs 9.5% [6.4%-13.8%]) levels.
Conclusions
Detection and control of hypertension and dyslipidemia is far from optimal in Chinese adults, especially in newly-diagnosed diabetes. Improved screening for diabetes is required to promote a better prevention, treatment and control of hypertension and dyslipidemia in China.
Similar content being viewed by others
Background
Hypertension and dyslipidemia are established risk factors for cardiovascular disease morbidity and mortality [1]. Worldwide, 7.6 million premature deaths were attributed to high blood pressure in 2001 [2], and 4.4 million deaths each year were caused by raised cholesterols [3-6]. Most of the attributable burden caused by hypertension and dyslipidemia is borne by low-income and middle-income countries [2,7], where the coverage of screening and treatment of hypertension and dyslipidemia is low [6,8]. The awareness, treatment and control of hypertension and dyslipidemia have been discussed in several general populations [7,9,10]. Knowledge of the current magnitude of hypertension and dyslipidemia epidemic is key to ameliorating health care resource allocation, chronic disease management and education [11].
The China Noncommunicable Disease Surveillance 2010 is a nationally representative study [12], in which we have reported that 11.6% of Chinese adults aged 18 years or older had diabetes in 2010, while less than one-third (30.3%) of diabetes patients were aware of their condition [12]. Our data suggested that diabetes have reached an alert level in China, with the potential for a major epidemic of diabetes-related metabolic disorders, such as hypertension and dyslipidemia, which act as independent contributors to cardiovascular disease especially in patients with diabetes [13-15]. One previous study has indicated that newly-diagnosed diabetes tended to be associated with higher prevalence of uncontrolled hypertension and dyslipidemia [16]. Data from the United States National Health and Nutrition Examination Survey (NHANES) have revealed that newly-diagnosed diabetes was associated with a lack of awareness, treatment and control of high low-density lipoprotein cholesterol (LDL-C) [17]. Until recently, there are limited data concentrated on the awareness, treatment and control of hypertension and dyslipidemia in previously-diagnosed diabetes versus newly-diagnosed diabetes.
We sought to report a cross-sectional analysis of the influence of previously-diagnosed diabetes versus newly-diagnosed diabetes on the awareness, treatment and control of hypertension and dyslipidemia in a nationally representative sample from the China Noncommunicable Disease Surveillance 2010.
Methods
Study population
The China Noncommunicable Disease Surveillance 2010 included 162 study sites, based on the Chinese Center for Disease Control and Prevention’s National Disease Surveillance Point System, which guaranteed a nationally representative sample of the general population, covering major geographic areas of all 31 provinces, autonomous regions, and municipalities in mainland China [12,18]. The Surveillance Point System includes approximately 1% of the total Chinese population [18]. The first sampling level was stratified by 7 geographic regions including Northeast, North, East, South, Southeast, Northwest and Central areas, and 3 municipalities including Beijing, Tianjin, and Shanghai. The second level was stratified by urban and rural locations. The third level was stratified by 4 socioeconomic strata in rural areas and 3 population size strata in urban areas.
Only persons who had been living in their current residence for 6 months or longer were eligible to participate. At each site, a complex, multistage, probability sampling design was used to select participants who were representative of civilian, non-institutionalized Chinese adults. In stage one, 4 subdistricts in each urban area and 4 townships in each rural area were selected with probability proportional to population size. In stage two, 3 neighborhood communities or administrative villages were selected with probability proportional to population size. In stage three, households within each neighborhood community or administrative village were listed, and 50 households were randomly recruited. In stage four, 1 person aged 18 years or older was randomly selected from each household using a Kish selection table. When the selected individual was unable to participate, a similar household in the same or in a nearby neighborhood or village was randomly selected as a replacement. A total of 98658 adults (45143 men and 53515 women) participated in the survey. The overall response rate was 90.5%.
The study protocol was approved by the Ethical Review Committee of the Chinese Center for Disease Control and Prevention and other participating institutes. All study participants provided written informed consent.
Data collection
Data were collected in examination centers at local health stations or community clinics in the participants’ residential area by investigators and staff, who were trained according to a standard protocol and were required to pass a performance test in order to be qualified for data collection. A questionnaire including demographic characteristics, medical history, and lifestyle factors was administered by trained interviewers with face-to-face interviews. Current smoking was defined as having smoked 100 cigarettes in one’s lifetime and currently smoking cigarettes. Current drinking was defined as consuming alcohol more than once per month during the past 12 months. Physical activity was assessed by the Global Physical Activity Questionnaire and was measured by the metabolic equivalent hours per week [19]. Body mass index (BMI) was calculated as body weight in kilograms divided by body height squared in meters (kg/m2). Waist circumference was measured on standing participants midway between the lower edge of the costal arch and the upper edge of the iliac crest. Overweight was defined as a BMI of 25.0-29.9 kg/m2, and obesity was defined as BMI ≥30.0 kg/m2. Central obesity was defined as waist circumference ≥90 cm in men and ≥80 cm in women. Participants were advised to avoid alcohol, coffee, tea, smoking and exercise at least 30 minutes before blood pressure measurement. Blood pressure was measured at the non-dominant arm 3 times consecutively with a 1-minute interval between the measurements of seated participants using a calibrated automatic electronic device (OMRON Model HEM-7071, Omron Co.) in a separate examination room after a 5-minute rest. The three readings were averaged for analysis.
Blood samples were collected in all participants after an overnight fast of 10 hours or more. Participants without a self-reported history of diabetes undertook a 75-g oral glucose tolerance test (OGTT), and plasma glucose was measured at 0 and 2 hours after glucose administration during the OGTT. Plasma glucose was measured locally using glucose oxidase or hexokinase methods within 24 hours. All study laboratories successfully completed a standardization and certification program. The Hemoglobin Capillary Collection System (Bio-Rad Laboratories) was used to collect capillary blood samples strictly according to the manufacturer’s instructions. The capillary blood specimens were shipped and stored at 2°C to 8°C until hemoglobin A1c (HbA1c) was measured within 4 weeks after collection by high-performance liquid chromatography using the VARIANT II Hemoglobin Testing System (Bio-Rad Laboratories) at the central laboratory in the Shanghai Institute of Endocrine and Metabolic Diseases, which was certificated by the National Glycohemoglobin Standardization Program. Capillary HbA1c was converted to venous values using a validated formula [12].
Serum samples were aliquoted and frozen at −80°C within 2 hours of collection and shipped by air in dry ice to the central laboratory, which was accredited by the College of American Pathologists. Serum total cholesterol, LDL-C, HDL-C, and triglycerides were measured using an autoanalyser (Abbott Laboratories).
Definitions
Participants were categorized into one of the four mutually exclusive categories based on diabetes status: normal glucose regulation, prediabetes, newly-diagnosed diabetes, and previously-diagnosed diabetes, according to the American Diabetes Association 2010 criteria [20]. Diabetes was defined as a self-reported previous diagnosis by health care professionals, fasting plasma glucose level of 7.0 mmol/L (126 mg/dL) or higher, 2-hour plasma glucose level of 11.1 mmol/L (200 mg/dL) or higher, or HbA1c concentration of 6.5% or more. Among all diabetes patients, participants who reported a history of physician-diagnosed diabetes were considered to have previously-diagnosed diabetes, and those without a history of physician-diagnosed diabetes were considered to have newly-diagnosed diabetes. Prediabetes was defined as fasting plasma glucose levels between 5.6 mmol/L (100 mg/dL) and 6.9 mmol/L (125 mg/dL), 2-hour plasma glucose levels between 7.8 mmol/L (140 mg/dL) and 11.0 mmol/L (199 mg/dL), or HbA1c concentrations between 5.7% and 6.4% in participants without a prior diabetes diagnosis. Normal glucose regulation was defined as fasting plasma glucose levels less than 5.6 mmol/L (100 mg/dL), 2-hour plasma glucose levels less than 7.8 mmol/L (140 mg/dL), and HbA1c concentrations less than 5.7% in participants without a prior diabetes diagnosis.
The diagnosis and categorization of hypertension were based on the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure [21]. Hypertension was defined as a systolic blood pressure of 140 mm Hg or higher, a diastolic blood pressure of 90 mmHg or higher or taking blood pressure-lowering medications within the previous 2 weeks. Awareness was defined as the proportion of participants who reported a history of physician-diagnosed hypertension among all patients with hypertension. Treatment was defined as the proportion of participants taking blood pressure-lowering medications among all patients with hypertension. Control was defined as the proportion of participants who had systolic blood pressure and diastolic blood pressure of less than 140/90 mmHg for non-diabetes participants, or of less than 130/80 mmHg for diabetes patients among all hypertension patients with blood pressure-lowering medications.
According to the 2004 National Cholesterol Education Program Adult Treatment Panel III [22], dyslipidemia was defined as taking lipid-lowering medications or increased lipid levels as total cholesterol ≥240 mg/dL, triglycerides ≥200 mg/dL, HDL-C <40 mg/dL, or high LDL-C. Framingham risk score was calculated to estimate the 10-year risk of coronary heart disease [23]. Coronary heart disease risk factors included older age (55 years or older for women and 45 years or older for men), current smoking, hypertension, and low HDL-C (less than 40 mg/dL). Participants were assigned to one of the four risk categories: 1) low risk, having 0 to 1 risk factor, 2) intermediately low risk, having 2 or more risk factors and a 10-year risk of coronary heart disease less than 10%, 3) intermediately high risk, having 2 or more risk factors and a 10-year risk of coronary heart disease between 10% and 20%, and 4) with diabetes or a 10-year risk of coronary heart disease greater than 20% [24]. High LDL-C was defined according to the group-specific threshold recommended in National Cholesterol Education Program Adult Treatment Panel III as ≥190, 160, 130 and 130 mg/dL for risk categories 1 through 4, respectively. Awareness was defined as the proportion of participants who reported a history of physician-diagnosed dyslipidemia among all patients with dyslipidemia. Treatment was defined as the proportion of participants taking lipid-lowering medications among all patients with dyslipidemia. Control was defined as the proportion of participants who had total cholesterol <240 mg/dL, triglycerides <150 mg/dL, HDL-C ≥40 mg/dL in men and ≥50 mg/dL in women, and LDL-C <160, 130, 100, and 100 mg/dL for risk categories 1 through 4, respectively, among all patients with lipid-lowering medications.
Statistical analysis
All calculations were weighted to represent the overall Chinese adult population aged 18 years or older. Weight coefficients were derived from China population census data in 2010 and the sampling scheme of the present survey to obtain national estimates. Each one of the 162 study sites was categorized into underdeveloped, intermediately developed or developed region according to their gross domestic product per capita in 2009.
Demographic and metabolic features were described in overall population and in diabetes categories, using percentages (95% confidence intervals [CIs]) for categorical variables and means (95% CIs) for continuous variables. Weighted percentages (95% CIs) for prevalence, awareness, treatment and control of hypertension and dyslipidemia were estimated in overall population and in different diabetes categories.
Data were analyzed using the SAS system, version 9.3 (SAS Institute Inc, Cary, NC) and SUDAAN software, version 10.0 (Research Triangle Institute, Research Triangle Park, NC). All statistical analyses were 2-sided, and a P-value less than 0.05 was considered statistically significant.
Results
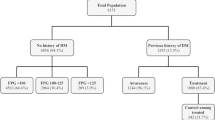
Among Chinese adults aged 18 years or older, the prevalence of diabetes was estimated to be 11.6% (95% CI: 11.3%, 11.8%), among which 3.5% (95% CI: 3.4%, 3.6%) were previously-diagnosed diabetes and 8.1% (95% CI: 7.9%, 8.3%) were newly-diagnosed diabetes. Characteristics of study population by glycemic status are depicted in Table 1. Compared with newly-diagnosed diabetes patients, previously-diagnosed diabetes patients were older, more likely to be women, or urban residents, live in economically developed areas, have parental diabetes history and higher educational achievement, have lower proportions of current smokers or drinkers, and have less physical activity. Additionally, previously-diagnosed diabetes patients had higher levels of BMI, waist circumference, fasting plasma glucose, HbA1c, and systolic blood pressure, and lower levels of OGTT-2 h plasma glucose, total cholesterol, triglycerides, LDL-C, and HDL-C than newly-diagnosed diabetes patients.
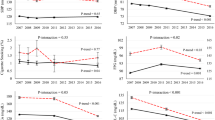
The weighted prevalence of hypertension and dyslipidemia gradually increased in adults with normal glucose regulation, prediabetes, newly-diagnosed diabetes and previously-diagnosed diabetes. Compared to those with newly-diagnosed diabetes, previously-diagnosed diabetes patients were more likely to be aware of hypertension (55.2% [95% CI: 52.9%, 57.5%] in previously-diagnosed diabetes and 37.6% [95% CI: 35.9%, 39.3%] in newly-diagnosed diabetes) and dyslipidemia (33.9% [95% CI: 31.8%, 36.1%] in previously-diagnosed diabetes and 12.8% [95% CI: 11.7%, 13.9%] in newly-diagnosed diabetes). Among participants who were aware of their conditions, those with previously-diagnosed diabetes were more inclined to receive treatment than those with newly-diagnosed diabetes (anti-hypertensive treatment, 43.7% [95% CI: 41.5%, 46.0%] in previously-diagnosed diabetes and 27.5% [95% CI: 26.0%, 29.0%] in newly-diagnosed diabetes; lipid-lowering treatment, 18.9% [95% CI: 17.2%, 20.7%] in previously-diagnosed diabetes and 5.4% [95% CI: 4.6%, 6.2%] in newly-diagnosed diabetes). The proportions of participants having controlled blood pressure and lipid levels were higher in those with previously-diagnosed diabetes (blood pressure control, 4.7% [95% CI: 3.5%, 6.2%]; lipid control, 15.9% [95% CI: 12.3%, 20.3%]) than in those with newly-diagnosed diabetes (blood pressure control, 3.5% [95% CI: 2.6%, 4.8%]; lipid control, 9.5% [95% CI: 6.4%, 13.8%]) (Table 2).
As shown in Table 3, the proportions of awareness and treatment of hypertension were higher in individuals who were older, women, urban residents, living in economically developed areas, and with higher BMI and abdominal obesity in both newly-diagnosed and previously-diagnosed diabetes. Compared with newly-diagnosed diabetes, previously-diagnosed diabetes had higher proportions of awareness and treatment of hypertension and dyslipidemia in each stratum, had higher proportions of controlled blood pressure in 45–64 years old individuals, and had higher proportions of controlled lipids in 45–64 years old individuals, men, urban residents, those with BMI less than 25 kg/m2, and those with waist circumference <90 cm in men and <80 cm in women (Table 4).
Among all participants, the proportion of participants who were aware of hypertension, in the meanwhile received anti-hypertensive medications and had their blood pressure controlled was 2.1% (95% CI: 1.5%, 2.7%) in previously-diagnosed diabetes patients vs newly-diagnosed diabetes (1.0% [95% CI: 0.7%, 1.3%]). Treatment and control of dyslipidemia were even worse than that of hypertension. The proportion of controlled lipids and treated dyslipidemia was higher in previously-diagnosed diabetes (3.0%, 95% CI: 2.3%, 3.9%) than newly-diagnosed diabetes (0.5%, 95% CI: 0.3%, 0.8%), as well as the proportion of treated but uncontrolled patients (Figure 1).
Discussion
In this nationally representative survey of Chinese adults aged 18 years or older, we found that previously-diagnosed diabetes was associated with a higher likelihood of awareness, treatment and control of hypertension and dyslipidemia compared to newly-diagnosed diabetes. Especially, a significant proportion of newly-diagnosed diabetes patients remained unaware of hypertension and dyslipidemia, and only a minority were treated and had their conditions effectively controlled.
The present study was conducted in a large nationally representative sample of the general population in China. In addition, the diagnosis of diabetes used all 3 glycemic indexes including fasting plasma glucose, 2-hour plasma glucose, and HbA1c concentrations, which provide a comprehensive estimation of diabetes status. Moreover, a strict quality assurance and quality control program was implemented at every phase of the study to ensure data validity and reliability. Several study limitations should be mentioned. First, type 1 and type 2 diabetes were not distinguished, although type 2 diabetes is the predominant diabetes in adults. Second, correlations may not infer causal relationships because of the cross-sectional nature and potential reverse causation bias. Also, the cross-sectional nature of the study prevents from seeking more deeply the reasons why subjects with previously diagnosed type 2 diabetes showed greater level of awareness of concomitant risk factors such as hypertension and dyslipidemia, compared to newly diagnosed subjects. In addition, due to a lack of family history of coronary heart disease (history of myocardial infarction or angina before age 50 years among first-degree relatives), we cannot precisely define the coronary heart disease risk categories.
Our data elaborated that not only in overall Chinese population, but also in traditional risk factors’ strata, previously-diagnosed diabetes patients were more likely to be aware of hypertension and dyslipidemia and to receive therapy. This result can be partially explained by the fact that compared to newly-diagnosed diabetic patients, previously-diagnosed patients are more frequently to have medical examinations by physicians. As a result of the diagnosis of diabetes, some hypertension and dyslipidemia could be prompted to have treated and get controlled. Thus, screening for diabetes would make for early diagnosis and prevention of hypertension and dyslipidemia, which would benefit the prevention and control of atherosclerotic cardiovascular diseases in general population [25-27].
The diagnosis of diabetes has important clinic implications for the prevention and management of cardiometabolic complications. The Ludwigshafen Risk and Cardiovascular Health study found that half of the patients scheduled for coronary angiography had newly-diagnosed diabetes, suggesting that for high-risk patients who had to schedule for coronary angiography, screening for diabetes should be performed routinely to initiate timely preventive efforts [28]. Besides, newly-diagnosed diabetes was common among high-risk non-ST-segment elevation acute coronary syndrome patients and associated with greater 30-day death or myocardial infarction [29], and was also associated with a higher death rate after coronary artery bypass grafting [30].
Hypertension and hyperlipidemia increase the risk of long-term cardiovascular disease in type 2 diabetes [31,32], which are disproportionally more harmful in low- and middle-income countries than in high-income countries [2,7]. In our study, urban location, developed economy, high education, and parental diabetes were associated with higher rate of hypertension control in both previously-diagnosed and newly-diagnosed diabetes. Urban location, high education, and parental diabetes were associated with higher proportion of controlled blood lipids in previously-diagnosed diabetes, but not in newly-diagnosed diabetes. Even in previously-diagnosed diabetes patients who were aware of their conditions and received treatments, the control rates for hypertension and dyslipidemia were still low. Several risk factors, including old age, women, rural location, under-developed economy, without parental history of diabetes, low education, less physical activity, high glucose or HbA1c associated with the worse control of hypertension in previously-diagnosed diabetes patients. These risk factors also impact the control of dyslipidemia, except that the developed economy was associated with lower control of dyslipidemia, and suggests that preventive interventions for dyslipidemia should be used at all levels of economic development (Additional file 1: Table S1 and S2). Interestingly, in each glycemic status, compared to non-obese individuals, general or abdominal obese individuals had higher prevalence of hypertension and dyslipidemia, and were more likely to be aware and treated, whereas were less likely to be adequately controlled (Additional file 1: Figure S1). The increased prevalence of obesity may have not only affected the metabolic characteristics of the population, but also impeded the pursuit of diseases control [33,34]. Thus, controlling obesity is important for an efficient and comprehensive management of multiple risk factors to prevent atherosclerotic cardiovascular diseases [35].
Conclusions
The China Noncommunicable Disease Surveillance 2010 indicated that the detection and control of hypertension and dyslipidemia is far from optimal in Chinese adults, especially in newly-diagnosed diabetes. Our data suggest that improved screening for diabetes is required to be an important component of a national strategy to promote better prevention, treatment and control of hypertension and hyperlipidemia, and to ease the large and increasing societal burden of cardiovascular disease in China.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- HbA1c:
-
Hemoglobin A1c
- HDL:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- MET-h/wk:
-
Metabolic equivalent hours per week
- NHANES:
-
National Health and Nutrition Examination Survey
- OGTT:
-
Oral glucose tolerance test
References
Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, et al. Heart disease and stroke statistics–2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115(5):e69–171.
Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371(9623):1513–8.
Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, Halsey J, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370(9602):1829–39.
Zhang X, Patel A, Horibe H, Wu Z, Barzi F, Rodgers A, et al. Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Int J Epidemiol. 2003;32(4):563–72.
Erqou S, Kaptoge S, Perry PL, Di Angelantonio E, Thompson A, White IR, et al. Lipoprotein (a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. Jama. 2009;302(4):412–23.
Farzadfar F, Finucane MM, Danaei G, Pelizzari PM, Cowan MJ, Paciorek CJ, et al. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3.0 million participants. Lancet. 2011;377((9765):578–86.
Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. Jama. 2013;310(9):959–68.
Tolonen H, Keil U, Ferrario M, Evans A. Prevalence, awareness and treatment of hypercholesterolaemia in 32 populations: results from the WHO MONICA Project. Int J Epidemiol. 2005;34(1):181–92.
Goff Jr DC, Bertoni AG, Kramer H, Bonds D, Blumenthal RS, Tsai MY, et al. Dyslipidemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium. Circulation. 2006;113(5):647–56.
Joffres M, Falaschetti E, Gillespie C, Robitaille C, Loustalot F, Poulter N, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013;3(8):e003423.
Hogan P, Dall T, Nikolov P. Economic costs of diabetes in the US in 2002. Diabetes Care. 2003;26(3):917–32.
Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–59.
van Hoeven KH, Factor SM. A comparison of the pathological spectrum of hypertensive, diabetic, and hypertensive-diabetic heart disease. Circulation. 1990;82(3):848–55.
Querton L, Buysschaert M, Hermans MP. Hypertriglyceridemia and residual dyslipidemia in statin-treated, patients with diabetes at the highest risk for cardiovascular disease and achieving very-low low-density lipoprotein-cholesterol levels. J Clin Lipidol. 2012;6(5):434–42.
Sowers JR, Epstein M, Frohlich ED. Diabetes, hypertension, and cardiovascular disease: an update. Hypertension. 2001;37(4):1053–9.
Hunt KJ, Gebregziabher M, Egede LE. Racial and ethnic differences in cardio-metabolic risk in individuals with undiagnosed diabetes: National Health and Nutrition Examination Survey 1999–2008. J Gen Intern Med. 2012;27(8):893–900.
Brown TM, Tanner RM, Carson AP, Yun H, Rosenson RS, Farkouh ME, et al. Awareness, treatment, and control of LDL cholesterol are lower among U.S. adults with undiagnosed diabetes versus diagnosed diabetes. Diabetes Care. 2013;36(9):2734–40.
Yang G, Hu J, Rao KQ, Ma J, Rao C, Lopez AD. Mortality registration and surveillance in China: History, current situation and challenges. Popul Health Metrics. 2005;3(1):3.
Bull FC, Maslin TS, Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. 2009;6(6):790–804.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33 Suppl 1:S62–9.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. Jama. 2003;289(19):2560–72.
Grundy SM, Cleeman JI, Merz CN, Brewer Jr HB, Clark LT, Hunninghake DB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227–39.
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–47.
National Cholesterol Education Program (NCEP). Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). Circulation. 2002;106(25):3143–421.
Ford ES, Li C, Sniderman A. Temporal changes in concentrations of lipids and apolipoprotein B among adults with diagnosed and undiagnosed diabetes, prediabetes, and normoglycemia: findings from the National Health and Nutrition Examination Survey 1988–1991 to 2005–2008. Cardiovasc Diabetol. 2013;12:26.
Sacks FM, Hermans MP, Fioretto P, Valensi P, Davis T, Horton E, et al. Association between plasma triglycerides and high-density lipoprotein cholesterol and microvascular kidney disease and retinopathy in type 2 diabetes mellitus: a global case–control study in 13 countries. Circulation. 2014;129(9):999–1008.
Wasem J, Bramlage P, Gitt AK, Binz C, Krekler M, Deeg E, et al. Co-morbidity but not dysglycaemia reduces quality of life in patients with type-2 diabetes treated with oral mono- or dual combination therapy–an analysis of the DiaRegis registry. Cardiovasc Diabetol. 2013;12:47.
Taubert G, Winkelmann BR, Schleiffer T, Marz W, Winkler R, Gok R, et al. Prevalence, predictors, and consequences of unrecognized diabetes mellitus in 3266 patients scheduled for coronary angiography. Am Heart J. 2003;145(2):285–91.
Giraldez RR, Clare RM, Lopes RD, Dalby AJ, Prabhakaran D, Brogan Jr GX, et al. Prevalence and clinical outcomes of undiagnosed diabetes mellitus and prediabetes among patients with high-risk non-ST-segment elevation acute coronary syndrome. Am Heart J. 2013;165(6):918–25. e912.
Lauruschkat AH, Arnrich B, Albert AA, Walter JA, Amann B, Rosendahl UP, et al. Prevalence and risks of undiagnosed diabetes mellitus in patients undergoing coronary artery bypass grafting. Circulation. 2005;112(16):2397–402.
Anderson RJ, Bahn GD, Moritz TE, Kaufman D, Abraira C, Duckworth W. Blood pressure and cardiovascular disease risk in the Veterans Affairs Diabetes Trial. Diabetes Care. 2011;34(1):34–8.
Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358(6):580–91.
Nagao H, Kashine S, Nishizawa H, Okada T, Kimura T, Hirata A, et al. Vascular complications and changes in body mass index in Japanese type 2 diabetic patients with abdominal obesity. Cardiovasc Diabetol. 2013;12:88.
Saydah S, Bullard KM, Cheng Y, Ali MK, Gregg EW, Geiss L, et al. Trends in cardiovascular disease risk factors by obesity level in adults in the United States, NHANES 1999–2010. Obesity (Silver Spring). 2014;22:1888–95.
Kones R, Rumana U. Prevention of cardiovascular disease: updating the immensity of the challenge and the role of risk factors. Hosp Pract (1995). 2014;42(1):92–100.
Acknowledgement
This work was supported by the grants 2013BAI09B13 from the National Clinical Research Center for Metabolic Diseases, 2012ZX09303006-001 from the National Key New Drug Creation and Manufacturing Program of Ministry of Science and Technology, 2012AA02A509 from the National High Technology Research and Development Program of China (863 Program) and 81321001, 81390350, 81222008, 81130016 from the National Natural Science Foundation of China. Dr. Yu Xu was supported by the Fogarty International Center of the National Institutes of Health under Award Number D43TW009107.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Drs TW, YX and MX contributed equally to this work. Dr N directed this work. Study concept and design: TW, YX, MX, B and N acquisition of data: TW, YX, Z, J, LW, YL, MZ, LW and N analysis and interpretation of data: TW, YX, MX, WW, B and N drafting of the manuscript: TW, YX and MX critical revision of the manuscript for important intellectual content: TW, YX, MX, WW, B, L and N statistical analysis: TW, YX and Lai administrative, technical, or material support: D, DZ, D, BX and S study supervision: WW, B, Z, LW and N. All authors read and approved the final manuscript.
Tiange Wang, Yu Xu and Min Xu contributed equally to this work.
Additional file
Additional file 1: Table S1.
Characteristics of Chinese adults with controlled vs. uncontrolled hypertension in newly-diagnosed and previously-diagnosed diabetes. Table S2. Characteristics of Chinese adults with controlled vs. uncontrolled dyslipidemia in newly-diagnosed and previously-diagnosed diabetes. Figure S1. Prevalence, awareness, treatment and control of hypertension and dyslipidemia by obesity status in each glycemic group.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wang, T., Xu, Y., Xu, M. et al. Awareness, treatment and control of cardiometabolic disorders in Chinese adults with diabetes: a national representative population study. Cardiovasc Diabetol 14, 28 (2015). https://doi.org/10.1186/s12933-015-0191-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-015-0191-6