Abstract
Background
Vitamin D has been suggested to influence the immune system, and vitamin D metabolites and the vitamin D receptor (VDR) are generated and expressed in white blood cells (WBC). Moreover, vitamin D status has been associated with incidence and prognosis of some respiratory tract infections (RTI). Therefore, we investigated the effect of vitamin D3 supplementation on WBC, acute phase reactants (APR), and the risk of developing RTIs.
Methods
A double-blinded, randomized, placebo-controlled clinical trial of 307 infertile men with multiple secondary immunological endpoints. The vitamin D3 group (n = 151) initially received 300,000 IU (7,500 µg) cholecalciferol once - followed by 1,400 IU (35 µg) daily for 150 days. The placebo group (n = 156) did not receive active ingredients.
Results
At baseline, stratification into clinically relevant groups of vitamin D status (< 25; 25–50; 50–75; >75 nmol/L), showed an inverse association with total leucocyte concentrations (7.0 vs. 6.0 vs. 6.0 vs. 5.5 (109/L); p = 0.007), lymphocytes (2.4 vs. 2.1 vs. 2.0 vs. 2.0 (109/L); p = 0.048), CRP (2.0 vs. 1.7 vs. 1.2 vs. 1.2 (mg/L); p = 0.037), and orosomucoid (0.82 vs. 0.77 vs. 0.76 vs. 0.70 (g/L); p = 0.015). After 150 days, no differences were detected in WBC counts or APRs between the vitamin D3 and the placebo group. However, vitamin D3 treated men had a higher prevalence of self-reported RTIs compared with the placebo group (55% vs. 39%; p = 0.005).
Conclusions
High-dose vitamin D3 supplementation did not alter WBCs or APRs, but a higher prevalence of respiratory infections was observed in the vitamin D3 group. Serum 25(OH)D3 was negatively correlated with most WBCs, indicating that vitamin D status may be linked with inflammation and WBC turnover, but not an important determinant of developing RTIs.
Trial registration
NCT01304927 (ClinicalTrials.gov). Registered February 20, 2011.
Similar content being viewed by others
Introduction
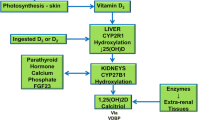
Vitamin D is a steroid hormone with several effects outside the classical regulation of bone health and calcium homeostasis [1,2,3]. Vitamin D is absorbed either through supplementation, diet, or de novo synthesized after ultraviolet-B radiation (UVB). Following UVB exposure of the skin, 7-dehydrocholesterol is converted into the inactive vitamin D3 – cholecalciferol [1]. Cholecalciferol undergoes a two-step hydroxylation before the active vitamin D metabolite 1α,25-dihydroxy-cholecalciferol (1,25(OH)2D3) binds to the vitamin D-receptor (VDR) where it can down- or upregulate genes [4]. The hepatic 25-hydroxylation enzyme CYP2R1 converts cholecalciferol into 25-hydroxy-cholecalciferol (25(OH)D3), which the kidneys converts into 1,25(OH)2D3, also known as calcitriol [1]. Both 25(OH)D3 and 1,25(OH)2D3 are catabolized into the inactive vitamin D metabolites (24,25-dihydroxyvitamin D3 and 1,24,25 trihydroxyvitamin D3, respectively) by the 24-hydroxylase enzyme CYP24A1 in the target tissue [1]. Vitamin D is mainly known for the regulation of bone and mineral homeostasis, but VDR is expressed in many other organs in the human body e.g., in the lungs, the reproductive tract, and in the immune system [2, 3, 5]. VDR is found in immune cells such as monocyte, leucocytes, and T lymphocytes [6,7,8]. Furthermore 1,25(OH)2D3 can be synthesized locally in monocytes as they express the enzyme CYP27B1 and vitamin D metabolites are of importance for the immune system [8].
In the innate immune system, Toll Like Receptors (TLR) exert a large role in detecting pathogenic organisms. In macrophages, activation of TLRs initiates an increase in VDR and CYP27B1 expression, and an intranuclear transcription of cathelicidin and beta-defensin genes – antimicrobial peptides [9]. Cathelicidin and beta-defensin are both present in airway epithelial cells [10] and are essential for regulating the inflammatory response in addition to eliminating the pathogens [11]. Sufficient vitamin D status is required for an adequate transcription of cathelicidin and beta-defensin [12]. Furthermore, neutrophils express VDRs and an abundant amount of cathelicidin but do not express the enzyme CYP27B1 [13]. Nonetheless, the function of vitamin D on neutrophils has not yet been fully characterized [14]. In the adaptive immune system, antigen-presenting cells (APC) present the pathogens to the naive T cells. This leads to either a proinflammatory response through Th1 (T-helper cell) development or an anti-inflammatory response through Th2 development [9, 15]. If the vitamin D levels are insufficient and if naive T cells are exposed to pathogens, Th1 development increases, which can lead to a cytokine storm where the secretion of proinflammatory cytokines IL-2 and IL-21 increases [15, 16]. Th1 will also release interferon gamma (IFN-γ) to stimulate the APC to secrete IL-6 which will activate Th17. Hence, Th17 is stimulated to secrete IL-17, another proinflammatory cytokine [17]. In contrast, sufficient vitamin D status can promote a Th2 development and IL-10 secretion and inhibit the expression of MHC-II, CD40, CD80, and CD86 in monocytes [15] and inflammatory signals influence vitamin D metabolism directly in granulomatous diseases [18].
Vitamin D deficiency is a global health issue and has been associated with inflammatory and infectious diseases [19, 20]. Vitamin D3 supplementation can reduce the risk of autoimmune diseases [21], and it has been suggested that impaired levels of vitamin D may negatively influence respiratory tract infections (RTI) such as asthma [22], tuberculosis [23, 24], and SARS-CoV-2 (COVID-19) [25]. Furthermore, a recent study found that COVID-19 hospitalized patients co-treated with high-dose 25(OH)D3 had a reduced risk of being admitted to an intensive care unit (ICU) compared to placebo treated patients [26]. However, regarding pneumonia and upper respiratory tract infections (URTI) such as the common cold and influenza, some studies suggest beneficial effects of vitamin D3 supplementation [27, 28], whereas other studies show no effects [29]. In this exploratory analysis from a randomized placebo-controlled clinical study, we investigated the effect of high-dose vitamin D3 supplementation on WBCs, acute phase reactants (APR), and self-reported RTIs.
Materials and methods
Trial design and intervention
The Copenhagen Bone-Gonadal Study (NCT01304927) is a single-centre, double-blinded, randomized clinical trial conducted at the Department of Growth and Reproduction, Rigshospitalet, Denmark and was approved by the Danish Health and Medicines authority, the local committee of Danish National Center for Ethics, and the data protection agency (approval no. 2010- 024588-42, H-4-2010-138, and 2,010,124,801). A thorough description of the study design has already been published [30]. In short, the study included 307 infertile men with impaired semen quality, vitamin D insufficiencies (< 50 nmol/L) at the day of screening, and no serious comorbidities. All participants were on average included in the study 2 months after the screening day. The primary endpoint was to determine if vitamin D3 supplementation modified the semen quality in infertile men. All participants signed a declaration of consent. The vitamin D3 group received an oral bolus of cholecalciferol (300,000 IU/7,500 µg) at day 1 (baseline) and vitamin D3 tablets containing cholecalciferol (1,400 IU/35 µg) and calcium (500 mg) for a single daily intake during each of the following 150 days. The placebo group received an oral bolus of oil and placebo tablets (without vitamin D3 and calcium). Written informed consent was obtained from all participants before enrolment. The treatment regime was selected to minimize the effect of compliance issues and since all men had vitamin D deficiency from the start (threshold 50 nmol/L). The study was designed to obtain an expected increase in serum 25(OH)D3 of 50 nmol/L. Blood samples were collected on day 1 and day 150, and participants were questioned about signs of RTIs on days 28, 90, and 150 as they were all considered incidents and therefore carefully asked for. Flow and safety outcome of the primary data concerning semen quality and changes in glucose and lipid homeostasis have been published [30, 31]. From January 2011 to August 2014 a total of 1,427 men were referred with impaired semen quality and screened for vitamin D insufficiency and comorbidities. A total of 1,002 men did not meet the criteria and were excluded, whereas 95 did not wish to participate. Furthermore, 15 men withdrew their consent and eight met an unforeseen exclusion criterion before day 1. Ultimately, 307 men were included in the study. Of the included men, 38 were lost to follow-up. In total, 269 men completed the study. No serious adverse effects were reported. The secondary outcome measures did not explicitly reference URTI. Instead, infectious disease such as pneumonia, common cold, and tonsillitis were listed as secondary outcomes. Alongside the CBG study, secondary endpoints related to metabolism [31], obesity [32], and reproductive hormones [33, 34] have been published using the dataset.
Biochemical analysis
Leucocyte levels were conducted on a Sysmex SE9000 with a coefficient of variation (CV) of 5%. Neutrophil, eosinophil, basophil, lymphocyte, and monocyte levels on a Sysmex XE-2100 with a CV of 6%, 12%, 6%, 6%, and 15%, respectively. CRP was measured on a Cobas 8000, c702 modul with a CV of 6%, whereas orosomucoid was measured on a Cobas 8000, c502 modul with a CV of 9%. Ferritin was measured on a Modular E-modul with a CV of 7% and PTH was measured on a Cobas 8000 (Roche) with a CV of 7%. Measurements of hemoglobin (CV2%) and thrombocytes were both conducted on a Sysmex XE-2100. The vitamin D measurements of 25(OH)D3 (CV < 10%) and 1,25(OH)2D3 (< 18%) levels were measured with an isotope-dilution liquid chromatography-tandem mass spectrometry (LC-MS/MS).
Statistical analysis
Tables 1, 2 and 3 are conducted as descriptive statistics and presented as mean with standard deviation (SD). The subgroups of vitamin D status in Table 2 are presented with p-values calculated with the Kruskal-Wallis test. P-values in Table 3 are calculated with a Student’s t-test. Furthermore, a correlation with a two-tailed test of significance and Pearson’s correlation coefficient between 25(OH)D3 and WBCs and APRs were completed on day 1, as seen in Fig. 1, and on day 150, as seen in Fig. 2. Moreover, Figs. 1 and 2 are presented with 95% confidence intervals for the regression lines and regression p-values in Fig. 2 were calculated with Student’s t-test. The self-reported RTIs (Fig. 3) were assembled as a whole number and expressed in the legend as a percentage for the vitamin D3 group and the placebo group. P-values were conducted with Pearson’s chi-squared test. All observations were included. All statistical analyses were conducted in the statistical software SPSS version 25. Vitamin D groups were defined as: Deficiency < 25 nmol/L, insufficiency 25–50 nmol/L, sufficiency 50–75 nmol/L, and adequate > 75 nmol/L.
Scatterplots of inflammatory markers at baseline with 95% confidence intervals for the regression lines, as a function of serum vitamin D of all men irrespective of randomization in a pooled linear regression model. a Leucocytes. b Neutrophils. c Eosinophils. d Lymphocytes. e Monocytes. f Orosomucoid. r-values: Pearson’s correlation coefficient. P-values: Pearson’s correlation with a two-tailed test of significance. * p < 0.05, ** p < 0.01, and *** p < 0.001. Abbreviations: S-25OHD3, serum 25-hydroxyvitamin D3
Scatterplots of inflammatory markers in the vitamin D3 group and placebo group after 150 days of treatment. Vitamin D3 group presented as red dots with red trend line and 95% confidence intervals for the regression lines. Placebo group presented as blue dots with a blue trend line and 95% confidence intervals for the regression lines, both as a function of serum 25(OH)D3 in a pooled linear regression model. (a) Leucocytes. (b) Neutrophils. (c) Eosinophils. (d) Lymphocytes. (e) Monocytes. (f) Orosomucoid. r-values: Pearson’s correlation coefficient. P-values: Pearson’s correlation with a two-tailed test of significance. * p < 0.05, ** p < 0.01, and *** p < 0.001. Regression p-values for leucocytes and monocytes were 0.016 and 0.013, respectively. Neutrophils and lymphocytes were borderline significant, 0.059 and 0.077, respectively. Regression p-values were calculated with Student’s t-test. Abbreviations: S-25(OH)D3, serum 25-hydroxyvitamin D3
Respiratory infections after 150 days of treatment between the vitamin D3 group and placebo group. The data are presented as numbers of cases of RTI. The Vitamin D3 group had 83 cases (55%) of RTI, while 68 cases (45%) had no RTI. The placebo group had 61 cases (39%) of RTI, while 95 cases (61%) had no RTI, during the trial. Cases of common cold infections vitamin D3 group 61%, placebo group 45%. Influenza cases (28% and 20%, respectively). Tonsilitis cases (6% and 6%, respectively). Pneumonia (5% and 0%, respectively). **P-value: <0.01, conducted with Pearson’s Chi-squared test. Abbreviation: RTI, Respiratory tract infections
Results
Baseline characteristics
Table 1 illustrates the baseline characteristics of the participants on day 1. On day 1, both the vitamin D3 and the placebo groups were on average vitamin D insufficient (< 50 nmol/L), with a serum 25(OH)D3 of 46 nmol/L (SD 20) and 45 nmol/L (SD 20), respectively. The concentration of leucocytes and lymphocytes, CRP, ferritin, and orosomucoid were within the reference interval with no differences between the vitamin D3 group and the placebo. The concentration of basophile granulocytes were higher in the vitamin D3 group (0.035 109/L; SD 0.021) compared to the placebo group (0.030 109/L; SD 0.019) on day 1 (p = 0.038) (data not shown).
At baseline, negative correlations were found between leucocytes (r = -0.207; p < 0.001), neutrophils (r = -0.151; p = 0.009), eosinophils (r = -0.158; p = 0.007), lymphocytes (r = -0.191; p < 0.001), monocytes (r = -0.160; p = 0.006), and serum 25(OH)D3, (Fig. 1). Additionally, a negative correlation between orosomucoid (r = -0.156; r = 0.008) and serum 25(OH)D3 was found. The baseline values were divided into groups according to serum 25(OH)D3 levels (< 25 nmol/L; 25–50 nmol/L; 50–75 nmol/L; >75 nmol/L). Leucocytes (7.0 vs. 6.0 vs. 6.0 vs. 5.5 (109/L); p = 0.007), eosinophils (0.25 vs. 0.22 vs. 0.20 vs. 0.17 (109/L); p = 0.026), and lymphocytes (2.4 vs. 2.1 vs. 2.0 vs. 2.0 (109/L); p = 0.048) were higher in men with low vitamin D status compared to men with normal/high vitamin D status (Table 2). Neutrophils (3.8 vs. 3.2 vs. 3.3 vs. 2.9 (109/L); p = 0.068) and monocytes (0.51 vs. 0.47 vs. 0.44 vs. 0.44 (109/L); p = 0.063) showed a similar pattern, though not significant. Additionally, CRP and orosomucoid were significantly higher in men with low vitamin D status compared to men with normal/high vitamin D status (2.0 vs. 1.7 vs. 1.2 vs. 1.2 (mg/L); p = 0.037) (0.82 vs. 0.77 vs. 0.76 vs. 0.70 (g/L); p = 0.015).
Effect of vitamin D on WBCs, APRs and RTIs
At day 150, the concentration of 25(OH)D3 was higher in the vitamin D3 group compared to the placebo treated group. No differences in WBCs or APRs were detected between the vitamin D3 and the placebo group (Table 3). Moreover, no differences within the vitamin D3 group for WBCs or APRs were found, when comparing changes in WBCs or APRs according to vitamin D status at day 1 (Supplementary Table 1). The intervention induced an increase in serum 25(OH)D3 (46 to 89 nmol/L, p < 0.001) and 1,25(OH)2D3 levels (83 to 102 nmol/L, p < 0.001) in the vitamin D3 group that differed from the placebo group. There was no significant correlation between serum 25(OH)D3 and WBCs or APRs in the vitamin D3 treated group at day 150, as seen in Fig. 2. We did establish a significant difference of the regression lines between the two groups for leucocytes (p = 0.016) and monocytes (0.013), and borderline significant for neutrophils (p = 0.059) and lymphocytes (p = 0.077). In the placebo group, there was a significant correlation between serum 25(OH)D3 and leucocytes (r = -0.268, p = 0.002), neutrophils (r = -0.185, p = 0.033), eosinophils (r = -0.201, p = 0.021), lymphocytes (r = -0.197, p = 0.023), monocytes (r = -0.296, p < 0.001) at day 150, as seen in Fig. 2. In the vitamin D3 group, 83 participants reported at least one episode of a RTI corresponding to 55% of all men in the vitamin D3 group. Noteworthy, men in the vitamin D3 treated group reported more respiratory infections (common cold, influenza virus, tonsilitis, and pneumonia) during the trial period compared to the placebo group (61 participants, 39% of placebo group; p = 0.005), (Fig. 3). The etiological factors contributing to RTIs were common cold and influenza virus based on questionnaire, but not confirmed by serological testing. In men, who had self-reported RTIs in the vitamin D3 treated group, the common cold was reported by 61% (51 participants) whereas in the placebo group, it was reported by 74% (45 participants). Furthermore, 28% (23 participants) of the RTIs in the vitamin D3 treated group and 20% (12 participants) of RTIs in the placebo group reported influenza. Baseline characteristics such as smoking status, age, and BMI were compared to cases of RTIs between the vitamin D3 group and placebo group and showed no significant differences (data not shown).
Discussion
This study shows no significant effects of vitamin D3 supplementation on white blood cells (WBC) or acute phase reactants (APR) in infertile men. Although at baseline negative associations between serum 25(OH)D3 and WBCs and orosomucoid were found. Moreover, men with low vitamin D status (< 25 nmol/L; 25–50 nmol/L) had significantly higher levels of WBCs and APRs compared to normal/high vitamin D status (50–75 nmol/L; >75 nmol/L). After 150 days of intervention, there was a significantly higher prevalence of RTIs in the vitamin D3 group compared to the placebo group despite no differences in WBCs. The existing literature on how vitamin D insufficiency affects WBCs and APRs, as well as URTIs and pneumonia in young men, who despite infertility can be considered, is limited. The negative associations with leucocytes, neutrophils, eosinophils, monocytes, lymphocytes, and orosomucoid are similar to the study by Laird et al. [35] who investigated the link between vitamin D status and inflammatory markers such as CRP and IL-6 in an elderly population (> 60 years of age). They discovered significant associations in CRP and IL-6 levels compared to vitamin D levels. Specifically, individuals with lower levels of serum vitamin D had higher levels of CRP and IL-6, though within reference levels. The significant negative correlations found in both studies suggest that the link with inflammation is not age dependent. At day 150, we found a similar negative correlation between serum 25(OH)D3 and the inflammatory markers in the placebo group (Fig. 2), but no significant correlation in the vitamin D3 group. This could indicate that vitamin D influences inflammatory markers, even when within reference levels, but vitamin D3 supplementation and vitamin D status are not strong determinants of the risk of acquiring a RTI. Vitamin D has been the subject of discussions regarding a potential U-shaped pattern concerning health risks and immune function [36, 37]. The U-shaped relationship of vitamin D suggests that vitamin D3 supplementation may only influence inflammatory markers up to a certain threshold. This could potentially explain why no further effects in the vitamin D3 group were observed after 150 days. Moreover, it is possible that the high-dose bolus of 300,000 IU is the cause of the potential harmful effect on the incidence of RTI.
The lack of benefit of high dose vitamin D3 supplementation on RTIs was consistent with other studies [38, 39]. Subsequently, more recent research has found contradictory results. Several studies using bolus dosing such as the ViDA study [40] with monthly doses of 100,000 IU showed no benefit for respiratory infections, while 60,000 IU monthly showed similar results but reduced the burden of symptoms [41, 42]. A recent meta-analysis [43] showed a 20% reduction in RTI in patients receiving daily or weekly dosing, but not in patients treated with bolus dosing.
Laaksi et al. [44] and Urashima et al. [45] showed that participants who ingested daily low-dose vitamin D3 (400 IU and 1,200 IU, respectively) had a positive effect on URTI. Mechanistic insight into the difference between high bolus versus daily intake was provided by Vieth et al. [46] suggesting that high-dose vitamin D3 intake could induce substantial fluctuations in the concentration of serum 25(OH)D3, differently than daily low-dose vitamin D3 intake, through an imbalance in the vitamin D regulating enzymes (CYP27B1 and CYP24A1). This results in a decreased level of active vitamin D (1,25(OH)2D3) needed to assist the immune system against pathogens in respiratory infections and in this way, high-dose bolus vitamin D may impair immune function.
It is plausible that vitamin D insufficiency is of less relevance in milder infections, particularly if the person does not have vitamin D deficiency but may play a more essential role when exposed to severe respiratory tract infections. This hypothesis is supported by a study from Castillo et al. [26], which showed that high-dose 25(OH)D3 supplementation was associated with reduced intensive care unit (ICU) cases in SARS-CoV-2 hospitalized patients. Additionally, a study from Nielsen et al. [25] found that vitamin D deficiency was significantly correlated with severe SARS-CoV-2 infections. Nonetheless, Nielsen et al. [25] also found significant differences between vitamin D and age as well as vitamin D and comorbidity, which may explain why we did not observe any differences between vitamin D insufficiency and inflammatory markers or for that matter URTI. Except for their known infertility, our study participants were young and healthy, and none were hospitalized during the trial. But hypothetically, in the event participants had been hospitalized with a RTI during the trial, the results would likely have been akin.
The significant difference in respiratory infections in the vitamin D3 group compared to the placebo group, 55% vs. 39% cannot be explained by this study setup. Moreover, URTIs were not a predefined secondary endpoint, and this observation should therefore be considered as an explorative endpoint that needs confirmation in future trials. Furthermore, the CBG (Copenhagen Bone-Gonadal Study) has several secondary endpoints, which is an important limitation because the likelihood of chance finding increases with numerous secondary endpoints. To our knowledge, no studies have shown an increased prevalence of RTIs and vitamin D3 supplementation. This could be due to the self-reported procedure following interview for potential incidents during GCP (Good clinical practice) monitored follow up. No tests were done when participants reported RTIs over the 150 days to confirm the diagnosis. On average, healthy men experience a URTI 1–2 times a year [47], which correlates with the cohort, as 46% of the participants experienced a URTI within 150 days. From the respiratory infections, the vitamin D3 group had a higher percentage (5%) of pneumonia cases compared to the placebo group (0%). However, pneumonia is a lower respiratory tract infection. Similarly, to our study, Remmelts et al. [48] explored three case-control studies of a total of 33,726 cases of pneumonia and found that vitamin D3 supplementation in adults showed no preventive effect against pneumonia when adjusted for confounders. One of the studies even reported an increased risk of pneumonia in the vitamin D3 group. When exploring respiratory infections, we found that vitamin D3 did not protect against influenza. Influenza was detected in 28% of the RTIs in the vitamin D3 group, whereas 20% were in the placebo group. We assume that high-dose vitamin D3 intake does not influence mild, non-hospitalized URTI, as opposed to low-dose vitamin D3 supplementation.
This study has notable strengths. All participants were vitamin D insufficient at the day of screening, and the serum 25(OH)D3 was analysed on a LC-MS/MS. Additionally, participants in the vitamin D3 group achieved the expected increase in serum 25(OH)D3 after 150 days [30]. However, while valid, it is not without limitations. We investigated 307 men, who were healthy besides being infertile and having vitamin D insufficiencies. This population may not be suitable to represent healthy men in general. Furthermore, after 150 days of intervention, the placebo group had an average vitamin D status above 50 nmol/L. This observation raises the possibility that the outcome of WBC and APR levels between the vitamin D3 group and placebo group may be influenced by inclination. In retrospect, using a higher daily dosage rather than the initial bolus of 300,000 IU would have been preferable. The decision to opt for the initial bolus of 300,000 IU was driven by concerns about non-compliance within the vitamin D3 group, potentially resulting in negligible differences in the vitamin D status between the two groups. While the chosen dosage regimen guaranteed a pronounced divergence in vitamin D status, the utility of the initial 300,000 IU bolus remains uncertain, introducing the possibility of underestimating the positive effects associated with correcting vitamin D insufficiency. The high bolus dosage has later shown to induce harm and may lead to high CYP24A1 activity in many tissues.
In conclusion, this exploratory analysis from a randomized clinical trial did not show any impact of vitamin D3 supplementation in infertile men regarding WBCs and APRs. However, serum 25(OH)D3 was significantly negative correlated with leucocytes, neutrophils, eosinophils, monocytes lymphocytes, and orosomucoid at baseline. In our cohort, vitamin D3 has no preventive effect against non-hospital required RTIs and high-dose vitamin D3 supplementation cannot be routinely recommended for individuals with insufficient vitamin D levels to prevent respiratory tract infections.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 1,25(OH)2D3 :
-
1,25-dihydroxyvitamin D3
- 25(OH)D3 :
-
25-hydroxyvitamin D3
- APC:
-
Antigen presenting cell
- APR:
-
Acute phase reactant
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- CV:
-
Coefficient of variation
- ICU:
-
Intensive care unit
- IFN-γ:
-
Interferon gamma
- PTH:
-
Parathyroid hormone
- RTI:
-
Respiratory tract infection
- Th1:
-
T-helper cell 1
- Th2:
-
T-helper cell 2
- TLR:
-
Toll like receptor
- URTI:
-
Upper respiratory tract infections
- UVB:
-
Ultraviolet-B
- VDR:
-
Vitamin D receptor
- WBC:
-
White blood cell
References
Prosser D, Jones G. Enzymes involved in the activation and inactivation of vitamin D. Trends Biochem Sci [Internet]. 2004;29(12):664–73. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0968000404002701.
Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B et al. Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions. Endocr Rev [Internet]. 2019 Aug 1 [cited 2023 May 10];40(4):1109–51. Available from: https://academic.oup.com/edrv/article/40/4/1109/5126915.
Blomberg Jensen M, Nielsen JE, Jørgensen A, Rajpert-De Meyts E, Kristensen DM, Jørgensen N et al. Vitamin D receptor and vitamin D metabolizing enzymes are expressed in the human male reproductive tract. Hum Reprod [Internet]. 2010;25(5):1303–11. Available from: https://pubmed.ncbi.nlm.nih.gov/20172873/.
Haussler MR, Jurutka PW, Mizwicki M, Norman AW. Vitamin D receptor (VDR)-mediated actions of 1α,25(OH)2vitamin D3: genomic and non-genomic mechanisms. Best Pract Res Clin Endocrinol Metab [Internet]. 2011 [cited 2023 May 10];25(4):543–59. Available from: https://pubmed.ncbi.nlm.nih.gov/21872797/.
Jensen MB. Vitamin D and male reproduction. Nat Rev Endocrinol [Internet]. 2014;10(3):175–86. Available from: http://www.nature.com/articles/nrendo.2013.262.
Chun RF, Liu PT, Modlin RL, Adams JS, Hewison M. Impact of vitamin D on immune function: lessons learned from genome-wide analysis. Front Physiol [Internet]. 2014;5. Available from: https://pubmed.ncbi.nlm.nih.gov/24795646/.
Mahon BD, Wittke A, Weaver V, Cantorna MT. The targets of vitamin D depend on the differentiation and activation status of CD4 positive T cells. J Cell Biochem [Internet]. 2003;89(5):922–32. Available from: https://pubmed.ncbi.nlm.nih.gov/12874827/.
Zhang Y, Leung DYM, Richers BN, Liu Y, Remigio LK, Riches DW et al. Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1. J Immunol [Internet]. 2012 Mar 1 [cited 2023 Apr 4];188(5):2127–35. Available from: https://pubmed.ncbi.nlm.nih.gov/22301548/.
Ismailova A, White JH. Vitamin D, infections and immunity. Rev Endocr Metab Disord [Internet]. 2022;23(2):265–77. Available from: https://link.springer.com/article/10.1007/s11154-021-09679-5.
Bartley J. Vitamin D: emerging roles in infection and immunity. https://doi.org/10.1586/eri10102 [Internet]. 2014;8(12):1359–69. Available from: https://www.tandfonline.com/doi/abs/10.1586/eri.10.102.
Allen-Hoffmann BL, Rooney PJ. Current innovations for the treatment of chronic wounds. Ski Tissue Eng Regen Med. 2016;265–87.
Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science [Internet]. 2006;311(5768):1770–3. Available from: https://pubmed.ncbi.nlm.nih.gov/16497887/.
Szymczak I, Pawliczak R. The Active Metabolite of Vitamin D3 as a Potential Immunomodulator. Scand J Immunol [Internet]. 2016 Feb 1 [cited 2023 May 11];83(2):83–91. Available from: https://pubmed.ncbi.nlm.nih.gov/26678915/.
Quesada-Gomez JM, Entrenas-Castillo M, Bouillon R. Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166. J Steroid Biochem Mol Biol [Internet]. 2020;202. Available from: https://pubmed.ncbi.nlm.nih.gov/32535032/.
Boonstra A, Barrat FJ, Crain C, Heath VL, Savelkoul HFJ, O’Garra A. 1α,25-Dihydroxyvitamin D3 Has a Direct Effect on Naive CD4 + T Cells to Enhance the Development of Th2 Cells. J Immunol [Internet]. 2001;167(9):4974–80. Available from: https://journals.aai.org/jimmunol/article/167/9/4974/42755/1-25-Dihydroxyvitamin-D3-Has-a-Direct-Effect-on.
Mattner F, Smiroldo S, Galbiati F, Muller M, Lucia P, Di, Poliani PL et al. Inhibition of Th1 development and treatment of chronic-relapsing experimental allergic encephalomyelitis by a non-hypercalcemic analogue of 1,25-dihydroxyvitamin D 3. [cited 2023 May 11]; Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1002/1521-4141.
Jeffery LE, Burke F, Mura M, Zheng Y, Qureshi OS, Hewison M et al. 1,25-Dihydroxyvitamin D3 and IL-2 combine to inhibit T cell production of inflammatory cytokines and promote development of regulatory T cells expressing CTLA-4 and FoxP3. J Immunol [Internet]. 2009;183(9):5458–67. Available from: https://pubmed.ncbi.nlm.nih.gov/19843932/.
Yahyavi SK, Theilade S, Hansen D, Berg JO, Andreassen CH, Lorenzen M et al. Treatment options for hypercalcemia after cosmetic oil injections: Lessons from human tissue cultures and a pilot intervention study. Bone [Internet]. 2022;154. Available from: https://pubmed.ncbi.nlm.nih.gov/34757214/.
Amrein K, Scherkl M, Hoffmann M, Neuwersch-Sommeregger S, Köstenberger M, Tmava Berisha A et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr 2020 7411 [Internet]. 2020;74(11):1498–513. Available from: https://www.nature.com/articles/s41430-020-0558-y.
Charoenngam N, Holick MF. Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients [Internet]. 2020 Jul 1 [cited 2023 Apr 13];12(7):1–28. Available from: https://pubmed.ncbi.nlm.nih.gov/32679784/.
Hahn J, Cook NR, Alexander EK, Friedman S, Walter J, Bubes V et al. Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease: VITAL randomized controlled trial. BMJ [Internet]. 2022;376. Available from: https://pubmed.ncbi.nlm.nih.gov/35082139/.
Korn S, Hübner M, Jung M, Blettner M, Buhl R. Severe and uncontrolled adult asthma is associated with vitamin D insufficiency and deficiency. Respir Res [Internet]. 2013 Feb 22 [cited 2023 Apr 4];14(1). Available from: https://pubmed.ncbi.nlm.nih.gov/23432854/.
Aibana O, Huang CC, Aboud S, Arnedo-Pena A, Becerra MC, Bellido-Blasco JB et al. Vitamin D status and risk of incident tuberculosis disease: A nested case-control study, systematic review, and individual-participant data meta-analysis. PLoS Med [Internet]. 2019;16(9). Available from: https://pubmed.ncbi.nlm.nih.gov/31509529/.
Martineau AR, Wilkinson KA, Newton SM, Floto RA, Norman AW, Skolimowska K et al. IFN-γ- and TNF-Independent Vitamin D-Inducible Human Suppression of Mycobacteria: The Role of Cathelicidin LL-37. J Immunol [Internet]. 2007;178(11):7190–8. Available from: https://journals.aai.org/jimmunol/article/178/11/7190/42971/IFN-and-TNF-Independent-Vitamin-D-Inducible-Human.
Nielsen NM, Junker TG, Cohen AS, Munger KL, Stenager E, Ascherio A et al. Vitamin D status and severity of COVID-19. Sci Rep [Internet]. 2022;12(1). Available from: https://pubmed.ncbi.nlm.nih.gov/36396686/.
Entrenas Castillo M, Entrenas Costa LM, Vaquero Barrios JM, Alcalá Díaz JF, López Miranda J, Bouillon R et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. J Steroid Biochem Mol Biol [Internet]. 2020 Oct 1 [cited 2023 May 12];203. Available from: https://pubmed.ncbi.nlm.nih.gov/32871238/.
Nanri A, Nakamoto K, Sakamoto N, Imai T, Akter S, Nonaka D et al. Association of serum 25-hydroxyvitamin D with influenza in case-control study nested in a cohort of Japanese employees. Clin Nutr [Internet]. 2017 Oct 1 [cited 2023 Apr 5];36(5):1288–93. Available from: https://pubmed.ncbi.nlm.nih.gov/27595379/.
Cannell JJ, Vieth R, Umhau JC, Holick MF, Grant WB, Madronich S et al. Re: epidemic influenza and vitamin D. Epidemiol Infect [Internet]. 2007 Oct [cited 2023 Apr 5];135(7):1097–8. Available from: https://pubmed.ncbi.nlm.nih.gov/17352842/.
Li-Ng M, Aloia JF, Pollack S, Cunha BA, Mikhail M, Yeh J et al. A randomized controlled trial of vitamin D3 supplementation for the prevention of symptomatic upper respiratory tract infections. Epidemiol Infect [Internet]. 2009 Oct [cited 2023 Apr 5];137(10):1396–404. Available from: https://pubmed.ncbi.nlm.nih.gov/19296870/.
Blomberg Jensen M, Gerner Lawaetz J, Petersen JH, Juul A, Jørgensen N. Effects of Vitamin D Supplementation on Semen Quality, Reproductive Hormones, and Live Birth Rate: A Randomized Clinical Trial. J Clin Endocrinol Metab [Internet]. 2018 [cited 2023 Apr 5];103(3):870–81. Available from: https://pubmed.ncbi.nlm.nih.gov/29126319/.
Holt R, Petersen JH, Dinsdale E, Knop FK, Juul A, Jørgensen N et al. Vitamin D Supplementation Improves Fasting Insulin Levels and HDL Cholesterol in Infertile Men. J Clin Endocrinol Metab [Internet]. 2022 Jan 1 [cited 2023 Jun 5];107(1):98–108. Available from: https://academic.oup.com/jcem/article/107/1/98/6368653.
Holt R, Jorsal MJ, Yahyavi SK, Qin S, Juul A, Jørgensen N et al. High-dose cholecalciferol supplementation to obese infertile men is sufficient to reach adequate vitamin D status. Br J Nutr. 2023;(9).
Holt R, Yahyavi SK, Kooij I, Poulsen NN, Juul A, Jørgensen N et al. Effects of vitamin D on sex steroids, luteinizing hormone, and testosterone to luteinizing hormone ratio in 307 infertile men. Andrology. 2023;(May):1–8.
Holt R, Yahyavi SK, Kooij I, Andreassen CH, Andersson A-M, Juul A et al. Low serum anti-Müllerian hormone is associated with semen quality in infertile men and not influenced by vitamin D supplementation. [cited 2023 Nov 13]; Available from: http://creativecommons.org/licenses/by/4.0/.TheCreativeCommonsPublicDomainDedicationwaiver.
Laird E, McNulty H, Ward M, Hoey L, McSorley E, Wallace JMW et al. Vitamin D Deficiency Is Associated With Inflammation in Older Irish Adults. J Clin Endocrinol Metab [Internet]. 2014 May 1 [cited 2023 Apr 29];99(5):1807–15. Available from: https://academic.oup.com/jcem/article/99/5/1807/2537572.
Grant WB, Karras SN, Bischoff-Ferrari HA, Annweiler C, Boucher BJ, Juzeniene A et al. Do studies reporting ’U’-shaped serum 25-hydroxyvitamin D-health outcome relationships reflect adverse effects? Dermatoendocrinol [Internet]. 2016 Jan [cited 2023 Aug 4];8(1):e1187349. Available from: https://pubmed.ncbi.nlm.nih.gov/27489574/.
Kojima G, Iliffe S, Tanabe M. Vitamin D supplementation as a potential cause of U-shaped associations between vitamin D levels and negative health outcomes: a decision tree analysis for risk of frailty. BMC Geriatr [Internet]. 2017 Oct 16 [cited 2023 Aug 4];17(1). Available from: https://www.pmc/articles/PMC5644251/.
Martineau AR, James WY, Hooper RL, Barnes NC, Jolliffe DA, Greiller CL et al. Vitamin D3 supplementation in patients with chronic obstructive pulmonary disease (ViDiCO): a multicentre, double-blind, randomised controlled trial. Lancet Respir Med [Internet]. 2015 Feb 1 [cited 2023 Apr 5];3(2):120–30. Available from: https://pubmed.ncbi.nlm.nih.gov/25476069/.
Murdoch DR, Slow S, Chambers ST, Jennings LC, Stewart AW, Priest PC et al. Effect of Vitamin D3 Supplementation on Upper Respiratory Tract Infections in Healthy Adults: The VIDARIS Randomized Controlled Trial. JAMA [Internet]. 2012 Oct 3 [cited 2023 Apr 5];308(13):1333–9. Available from: https://jamanetwork.com/journals/jama/fullarticle/1367547.
Scragg R. The Vitamin D Assessment (ViDA) study-Design and main findings. 2019 [cited 2023 Nov 12]; Available from: www.elsevier.com/locate/jsbmb.
Charoenngam N, Shirvani A, Holick MF. Vitamin D and Its Potential Benefit for the COVID-19 Pandemic. Endocr Pract [Internet]. 2021;27(5):484–93. Available from: https://pubmed.ncbi.nlm.nih.gov/33744444/.
Pham H, Waterhouse M, Baxter C, Romero B, McLeod D, Armstrong B, et al. 1378The effect of vitamin D supplementation on acute Respiratory Infection -analysis of the D-Health trial. Int J Epidemiol. 2021;50(Supplement1):1–2.
Mazess RB, Bischoff-ferrari HA, Dawson-hughes B. Vitamin D: Bolus is Bogus —. Narrative Rev. 2021;5(12):1–8.
Laaksi I, Ruohola JP, Mattila V, Auvinen A, Ylikomi T, Pihlajamäki H. Vitamin D Supplementation for the Prevention of Acute Respiratory Tract Infection: A Randomized, Double-Blinded Trial among Young Finnish Men. J Infect Dis [Internet]. 2010 Sep 1 [cited 2023 Apr 5];202(5):809–14. Available from: https://academic.oup.com/jid/article/202/5/809/1746565.
Urashima M, Segawa T, Okazaki M, Kurihara M, Wada Y, Ida H. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am J Clin Nutr [Internet]. 2010 May 1 [cited 2023 Apr 5];91(5):1255–60. Available from: https://pubmed.ncbi.nlm.nih.gov/20219962/.
Vieth R. How to optimize vitamin D supplementation to prevent cancer, based on cellular adaptation and hydroxylase enzymology. Anticancer Res. 2009;29(9):3675–84.
Heikkinen T, Järvinen A. The common cold. Lancet (London, England) [Internet]. 2003 Jan 1 [cited 2023 Apr 5];361(9351):51. Available from: https://www.pmc/articles/PMC7112468/.
Remmelts HHF, Spoorenberg SMC, Oosterheert JJ, Bos WJW, De Groot MCH, Van De Garde EMW. The role of vitamin D supplementation in the risk of developing pneumonia: three independent case-control studies. Thorax [Internet]. 2013 Nov [cited 2023 Apr 5];68(11):990–6. Available from: https://pubmed.ncbi.nlm.nih.gov/23892991/.
Funding
Open access funding provided by Copenhagen University. No influence from any sponsor on the study design, interpretation of results, or the decision to submit the manuscript for publication. This study was supported by FSS, Beckett foundation and Novo Nordisk foundation.
Open access funding provided by Copenhagen University
Author information
Authors and Affiliations
Contributions
GWG reviewed the literature, organized the writing, and wrote the initial draft. SKY, RH, MJJ, and MBJ designed the study and directed the analyses. In line with the mentioned authors, AJ and NJ participated in the discussion and interpretation of the results, critically revised the manuscript for intellectual content, and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from all participants before enrolment. The Copenhagen Bone-Gonadal Study (NCT01304927) was approved by the Danish Health and Medicines authority, the local committee of Danish National Center for Ethics, and the data protection agency (approval no. 2010-024588-42, H-4-2010-138, and 2010124801).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
: Table 1 Effect of treatment as Δ values divided into four groups of vitamin D levels. The effect of treatment presented as delta values after 150 days divided into four groups of vitamin D3 levels from day 1; <25 nmol/L; 25–50 nmol/L; 50–75 nmol/L; >75 nmol/L. The n highlights the number of participants in each group. The data are presented as means with a confidence interval of ± 95% (CI 95%) enclosed in parenthesis. P-values: t-test. Abbreviations: BMI, body mass index; 25(OH)D3, 25-hydroxyvitamin D3; CRP, C-reactive protein. Table 2 Season of inclusion. The season of inclusion during the trial. 46% of participants were included during the season of spring, 19% during summer, 10% during autumn, and 26% during winter.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wall-Gremstrup, G., Holt, R., Yahyavi, S.K. et al. High-dose vitamin D3 supplementation shows no beneficial effects on white blood cell counts, acute phase reactants, or frequency of respiratory infections. Respir Res 25, 11 (2024). https://doi.org/10.1186/s12931-023-02642-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-023-02642-9