Abstract
Background
No personalized prediction model or standardized algorithm exists to identify those at high risk of death among severe community-acquired pneumonia (SCAP) patients with chronic obstructive pulmonary disease (COPD). The aim of this study was to investigate the risk factors and to develop a useful nomogram for prediction of mortality in those patients.
Methods
We performed a retrospective, observational, cohort study in the intensive care unit (ICU) of West China Hospital, Sichuan University with all consecutive SCAP patients with COPD between December 2011 and December 2018. The clinical data within 24 h of admission to ICU were collected. The primary outcome was hospital mortality. We divided the patients into training and testing cohorts (70% versus 30%) randomly. In the training cohort, univariate and multivariate logistic regression analysis were used to identify independent risk factors applied to develop a nomogram. The prediction model was assessed in both training and testing cohorts.
Results
Finally, 873 SCAP patients with COPD were included, among which the hospital mortality was 41.4%. In training cohort, the independent risk factors for hospital mortality were increased age, diabetes, chronic renal diseases, decreased systolic blood pressure (SBP), and elevated fibrinogen, interleukin 6 (IL-6) and blood urea nitrogen (BUN). The C index was 0.840 (95% CI 0.809–0.872) in training cohort and 0.830 (95% CI 0.781–0.878) in testing cohort. Furthermore, the time-dependent AUC, calibration plots, DCA and clinical impact curves indicated the model had good predictive performance. Significant association of risk stratification based on nomogram with mortality was also found (P for trend < 0.001). The restricted cubic splines suggested that estimated associations between these predictors and hospital mortality were all linear relationships.
Conclusion
We developed a prediction model including seven risk factors for hospital mortality in patients with SCAP and COPD. It can be used for early risk stratification in clinical practice after more external validation.
Similar content being viewed by others
Background
Community-acquired pneumonia (CAP), caused by a large variety of microorganisms including bacteria, respiratory viruses and fungi, is a common acute respiratory infection with high morbidity in all age groups worldwide [1]. Meanwhile, it is reported to be responsible for substantial mortality, with a third of patients dying within 1 year after being discharged from hospital [2]. One multicenter, population-based study released that 21% of pneumonia patients required intensive care, who were often considered to be severe CAP (SCAP) patients [3]. Recent advances in rapid diagnosis, microbiological investigation, appropriate and individualized antibiotic therapy, and management of complications have contributed to improving the outcomes of patients with SCAP. However, the mortality still remains high and is reported to be 25–50% globally [4].
Chronic obstructive pulmonary disease (COPD), the fourth leading cause of death worldwide, has also imposed such a heavy burden on healthcare systems. It affects close to 400 million people around the world [5]. Similarly, despite huge progress in the prevention and treatment, only few advances have been made to ameliorate the mortality or improve the prognosis of COPD patients. It is estimated that more than 3 million people die of COPD worldwide every year. Furthermore, it is predicted that COPD will remain a major health-care related problem for the next few decades [6].
SCAP is one of the most common infections in COPD patients. COPD represents a relevant risk factor for development of CAP, and one of the most frequently reported comorbid conditions in SCAP patients. Compared with SCAP patients without COPD, SCAP patients with COPD might have some distinct characteristics, including structural disruptions in the lung parenchyma, abnormal lung immunity and pulmonary function, worse respiratory failure, different lung microbiome and pathogen virulence, and increased risk of infection by Gram-negative bacilli or development of invasive pulmonary aspergillosis, etc. [7]. Moreover, one recent meta-analysis also found a positive association between COPD and increased 30-days mortality in patients with CAP (OR 1.84; 95% CI 1.06, 2.62) [8]. Hence, there is growing need for more researches and investigations in patients with SCAP and COPD.
Accurate and timely evaluation of risk of death on the basis of various predictors or risk factors is of great importance for early and effective therapy and management. To date, only a few relatively small studies have reported the risk factors for poor outcomes in SCAP patients with COPD. For instance, one study with 211 patients with COPD and CAP requiring intensive care unit (ICU) admission reported that bilateral infiltration (OR 13.92; 95% CI 2.94–65.84) and longer duration of invasive mechanical ventilation (OR 1.11; 95% CI 1.01–1.22) were associated with increased in-hospital mortality [9]. However, no personalized prediction model or standardized algorithm exists to identify those at high risk of death among SCAP patients with COPD. The increasing rates of COPD in SCAP patients highlights the importance of a thorough assessment with an accurate and useful tool when managing those patients. The aim of this study was to investigate the risk factors and to develop a useful nomogram for prediction of hospital mortality in those patients.
Methods
Study design and cohort
We performed a retrospective, observational, cohort study in the ICU with over 200 beds in a large tertiary-care teaching hospital in Chengdu city, Sichuan province, China in accordance with the amended Declaration of Helsinki. The study was approved by the West China Hospital of Sichuan University Biomedical Research Ethics Committee (No. 2021-828). The requirement to obtain informed consent in this analysis was waived due to the retrospective noninterventional design. All analyses were conducted in accordance with the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis statement [10].
For construction and validation of the nomogram, we divided the patients into training and testing cohorts (70% versus 30%) randomly to ensure comparability between the cohorts. With approximately 20 putative variables potentially related to mortality, the minimum sample size required 200 deaths to follow the principle of at least 10 outcome events per variable (EPV) in the regression analysis [11]. Considering that the mortality of SCAP was approximately 40% in previous reports [4], the sample size of training cohort was estimated to be approximately 500. And therefore, the overall sample size was at least 715. Hence, all consecutive SCAP patients with COPD admitted to ICU between December 2011 and December 2018 were included in the current study.
According to the Infectious Diseases Society of America (IDSA)/American Thoracic Society (ATS) guidelines, SCAP was defined as fulfilment of at least 1 major criterion (septic shock with need for vasopressors; respiratory failure requiring mechanical ventilation) or 3 minor criteria (respiratory rate ≥ 30 breaths/min; PaO2/FiO2 ratio ≤ 250; multilobar infiltrates; confusion/disorientation; blood urea nitrogen level ≥ 20 mg/dL; white blood cell count < 4000 cells/µL; platelet count < 100,000/µL; core temperature < 36 °C; hypotension requiring aggressive fluid resuscitation) [12]. COPD was diagnosed based on medical history, clinical manifestation and the presence of persistent airflow limitation with a post-bronchodilator FEV1/FVC less than 0.70 on spirometry according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) report [13].
The exclusion criteria were as follows: (1) residents of long-term care facilities and/or nursing homes; (2) prior hospitalization within 30 days of study enrollment; (3) unclear outcomes; (4) severe immunosuppression defined according to a consensus statement [14], including active solid or hematological malignancy; HIV infection with a CD4 T-lymphocyte count < 200 cells/mL; receiving corticosteroid therapy with a dose ≥ 20 mg prednisone or equivalent daily for ≥ 14 days or a cumulative dose > 600 mg of prednisone; receiving cancer chemotherapy, biological immune modulators, disease-modifying antirheumatic drugs or other immunosuppressive drugs; (5) only the first admission was included if the patient had repeated admission.
All patients received standard care and antibiotic therapy to the discretion of the ICU attending physician and based on the CAP guidelines [12].
Study outcomes and measurements
The following clinical data within 24 h of admission to the ICU were collected anonymously from electronic medical records: demographic characteristics, comorbidities, vital signs, and laboratory examinations including hematological data, biochemical parameters, inflammatory markers, coagulation indicators, etc. All patients’ data were anonymized and de-identified. The first value was recorded for analysis if any laboratory examination was repeated more than once within 24 h of admission.
Two experienced physicians reviewed the medical records and completed the data collection by using a standardized data collection form independently. Data were checked by a third reviewer if there was any disagreement.
Patient follow-up was until hospital discharge. The primary outcome established for this study was hospital mortality.
Statistical analysis
Data were analyzed using IBM SPSS Statistical version 23.0 (SPSS, Chicago, IL, USA) and R software 4.1.2 (R Foundation for Statistical Computing). For standard analyses, a two-sided p < 0.05 was considered to indicate statistical significance. Data are presented as median (interquartile range, IQR) for continuous variables and number (percentage) for categorical variables as appropriate. The nonparametric Kruskal–Wallis test, chi-square analysis and Fisher’s exact test were used to test for differences between groups as appropriate. All baseline clinical data were compared between training cohort and testing cohort. Multiple imputation (MI) was used to account for missing data by using Bayesian methods in SPSS.
In the training cohort, the potential variables with P < 0.05 in univariate logistic regression analysis were included in the multivariate analysis with stepwise forward selection to identify independent risk factors for hospital mortality. The results were reported as odds ratios (ORs) and 95% confidence intervals (95% CIs). A simple nomogram based on independent risk factors was developed to predict individual probability of death. The prediction model was assessed using the concordance index (C index), area under receiver-operating characteristic (ROC) curve (AUC), area under time-dependent ROC curve (time-dependent AUC), calibration curves, decision curve analysis (DCA) and clinical impact curves in both training and testing cohorts [15,16,17].
Then, all patients were divided into three groups with different risks of mortality (low, moderate and high risk) according to nomogram to increase its clinical utility. The P values and the P for trend through the groups were calculated to further evaluate the nomogram. A Spearman correlation analysis was carried out to test the correlations of the continuous variables among the predictors. Finally, we also applied restricted cubic splines to estimate the possible non-linear associations between risk factors as continuous variables and mortality [18]. It was performed using the Regression Modeling Strategies (rms) package in R. The locations of the knots were set at the 10th, 50th and 90th percentiles with three knots. Analyses were multivariate-adjusted for all independent risk factors.
Results
Characteristics of SCAP patients with COPD
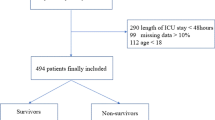
In total, 959 patients with SCAP and COPD between December 2011 and December 2018 were retrospectively screened. Then, 86 patients were excluded according to the exclusion criteria (Fig. 1). Among the remaining 873 SCAP patients with COPD, the median age was 77 years old (IQR 69,83) and 619 (70.9%) of patients were male. The patients’ comorbidities were summarized in Fig. 2. Hypertension, cancer history, chronic cardiovascular diseases, diabetes, chronic cardiovascular diseases and diabetes, and chronic renal diseases were the six most common coexisting medical conditions. The ICU mortality and hospital mortality was 36.5% (319 patients) and 41.4% (361 patients), respectively.
Finally, 611 patients were randomized to training cohort and 262 were assigned into testing cohort. Detailed comparison of clinical data between training cohort and testing cohort was shown in Additional file 1: Table S1 and Table S2. There were no significant differences in the features of demographic characteristics, comorbidities, vital signs, laboratory examinations and clinical outcomes.
Construction of nomogram
In training cohort, 17 variables were identified in the univariate logistics regression model. After that, multivariate analysis revealed that the independent risk factors for hospital mortality were increased age, diabetes, chronic renal diseases, decreased systolic blood pressure (SBP), and elevated fibrinogen, interleukin 6 (IL-6) and blood urea nitrogen (BUN). The detailed ORs and 95%CIs in univariate and multivariate analysis were summarized in Table 1.
Therefore, the above seven factors were used to construct the prediction model. To calculate individual patient scores and corresponding risk of death, a simple nomogram is available (Fig. 3A). According to the nomogram, each predictor corresponded to a point at each value. The total point was the sum of the points of seven predictors for each patient. The relationship between the total point and the probability of death was shown on the bottom of the nomogram.
A The nomogram for hospital mortality in SCAP patients with COPD. Age (years old); Diabetes and Chronic renal diseases (1: yes; 0: no); SBP (Systolic blood pressure, mmHg); Fibrinogen (g/L); IL-6 (interleukin-6, pg/mL) BUN (blood urea nitrogen, mmol/L). B Calibration curve of nomogram in training set. C Calibration curve in testing set. SCAP severe community-acquired pneumonia; COPD chronic obstructive pulmonary disease
Assessment of nomogram
The C index was 0.840 (95% CI 0.809–0.872) in training cohort and 0.830 (95% CI 0.781–0.878) in testing cohort, which indicated that the prediction model had good predictive discrimination. The ROC curves and AUCs for training cohort and testing cohort were displayed in Fig. 4A and B. Furthermore, the time-dependent AUC of model in training cohort and testing cohort were shown in Fig. 4C and D, respectively. The time-dependent AUC was around 0.80 for the prediction of death within 90 days after admission in both the training cohort and testing cohort, indicating favorable and robust discrimination of the model.
In Fig. 3B and C, the calibration plots suggested a high consistency, which demonstrated that the model’s predicted probabilities were close to the observed actual probabilities. The bias corrected C index was 0.834 and 0.813 in training cohort and testing cohort, respectively.
The DCA compared the net benefit of each score across different thresholds and showed that the majority of the threshold probabilities had great net benefit (Fig. 5A, B). In addition, we further plotted clinical impact curves to predict improved probability stratification for a population size of 1000. It showed that the predicted probability coincided well with the actual probability in both training cohort and testing cohort (Fig. 5C, D).
Clinical utility of nomogram and predictors
To further investigate the clinical utility of prediction model, all patients were divided into three groups according the total points calculated from nomogram: low risk (total points: under 150), moderate risk (from 150 to 200) and high risk (above 200). Compared with patients in low-risk group, the ORs (95% CIs) for hospital mortality of patients in moderate-risk and high-risk group were 4.102 (2.893, 5.815) and 22.130 (13.266, 36.919), respectively (P for trend < 0.001). (Table 2).
In Fig. 6A, the fibrinogen, IL-6 and BUN were positively correlated with each other. Meanwhile, the systolic blood pressure was negatively correlated with them (P for Spearman correlation analysis < 0.05). However, the correlations of age with them were not significant.
A Spearman correlation analysis. B–F The restricted cubic splines with three knots. The horizontal dashed line represents the reference OR of 1.0. The model was multivariate-adjusted for age, diabetes, chronic renal diseases, systolic blood pressure (SBP), fibrinogen, interleukin 6 (IL-6) and blood urea nitrogen (BUN). OR odds ratio; 95% CI 95% confidence interval
As shown in Fig. 6B–F, the estimated associations between these predictors and hospital mortality were all linear relationships (P for non-linear > 0.05), which further demonstrated the predictive performances and prognostic accuracies of these predictors as continuous variables.
Discussion
To the best of our knowledge, this is the first practical prediction model to identify patients at risk of death in those with SCAP and COPD specifically. Our model integrates various basic clinical characteristics, including age, comorbidities, vital signs and laboratory examinations, indicating that the comprehensive evaluation based on these predictors is essential. The C indices and time-dependent AUCs of the nomogram when applied to the training and testing cohorts were similar and both approximately 0.8, which demonstrated the performance was relatively ideal. The score can be calculated by hand according to nomogram with routine parameters tested in the laboratory. Hence, it is rapid, cost-effective and can be easily implemented in clinical practice.
The independent risk factors of death in CAP patients with COPD varied widely in the existing literature. For example, Bonnesen et al. included 243 CAP patients with COPD and found that the factors related to mortality were age, premorbid condition, CURB-65 score, pleural effusion and multi-lobular infiltrate [19]. In another research, aspiration (OR 5.203; 95% CI 1.443, 18.757), D-dimer > 2.0 µg/mL (OR 5.026; 95% CI 1.395, 18.108) and CURB-65 ≥ 3 (OR 23.299; 95% CI 6.246, 86.903) were risk factors of in-hospital mortality in 230 CAP patients comorbid with COPD [20]. Multilobar pneumonia (OR 2.883; 95% CI 1.299–6.399), Pseudomonas aeruginosa pneumonia (OR 19.091; 95% CI 4.326–84.256) and high-risk PSI classes (OR 10.316; 95% CI 1.691–62.946) were also found to be independent risk factors for case-fatality rate in a prospective cohort of CAP patients with COPD [21]. Moreover, Shin et al. found the serum hemoglobin concentration (HR 0.759; 95% CI 0.616, 0.936) and albumin level (HR 0.429; 95% CI 0.185, 0.995) were significantly associated with 180-day mortality in 134 acute exacerbation of COPD (AECOPD) patients with CAP [22]. The inconsistency regarding diverging results across prior studies could be attributable to a combination of factors such as study design, population, severity of CAP and treatments. The study from Cilli et al. only included CAP patients in the ICU [9]. However, researchers did not assess the prediction performances of risk factors. Besides, few prior studies focused on the weight of each risk factors for outcomes. Therefore, it is likely that this study has several advantages or more important clinical implications compared with previous studies. First, we had a larger population with only SCAP patients in ICU enrolled, which is representative of the real-world pneumonia patient cohort that has the highest mortality. Then, it has been suggested that the biomarkers are a cornerstone in the management of SCAP to decrease treatment failure [23]. Considering that the combination of biomarkers would be of greater use than individual predictor, we developed a prediction model. Afterwards, we also evaluated and validated the model with several statistical methods. Third, there is no consensus on the optimal cut-off values of these predictors in SCAP patients. Therefore, they were included in the model as continuous variables. Moreover, we carefully investigated the prognostic accuracies and clinical utilities of them via correlation analysis and restricted cubic splines.
Patients with advanced age, chronic renal diseases, decreased systolic blood pressure, elevated BUN are also classified as high-risk population when conventional score calculations are applied in SCAP patients, such as CURB-65, pneumonia severity index (PSI), Sequential Organ Failure Assessment (SOFA) score and Acute Physiology and Chronic Health Evaluation (APACHE) II tool. As observed clinically and previously reported, our nomograms show that diabetes, a common comorbidity of COPD, is associated with worse prognosis. Several factors might be responsible for the mechanisms. Previous evidence suggested that both COPD and impaired lung function, especially restricted ventilation dysfunction, could increase the risk of diabetes as a consequence of systemic inflammatory processes [24]. In addition, treatment with corticosteroids in COPD could possibly lead to a variety of side effects, such as worsening hyperglycemia and deterioration of diabetes control [25]. And reversely, diabetes can worsen the prognosis of COPD due to the direct effects of hyperglycemia on lung physiology, inflammation and susceptibility to bacterial infection [26]. Moreover, diabetes is potentially associated with a wide spectrum of complications which negatively affect the prognosis of COPD, such as pulmonary hypertension [27]. Therefore, careful evaluation and management should be conducted in SCAP patients with COPD and diabetes due to the possible poor prognosis. IL-6 is involved in various hematopoietic, immune, and inflammatory responses. Therefore, it has been widely used as an early sensitive prognostic biomarker and a predictor of treatment failure and mortality in CAP [28]. He et al. found that IL-6 (hazard ratio [HR] 1.001; p = 0.001) could serve as independent predictors of 30-day mortality for CAP after adjusting for clinical data, including age, bilateral lung infection, procalcitonin, CURB-65, PSI, etc. [29]. Similarly, as an inflammatory marker and coagulation factor which is synthesized by hepatocytes and circulating in the bloodstream, the concentrations of fibrinogen are rapidly elevated in tissue injury, infection, inflammation, etc. It could also be used in the CAP severity evaluation [30]. Their prognostic values have also been investigated in COPD. In a meta-analysis with 61 studies in COPD, increased levels of IL-6 were associated with hospitalization (standardized mean difference [SMD] 0.12, 95%CI 0.04–0.20) and higher levels of fibrinogen were also associated with exacerbation (SMD 0.23 g/dL, 95%CI 0.14–0.33) and mortality (HR 3.13 per twofold increase, 95%CI 2.14–4.57) [31]. Zhou et al. conducted another meta-analysis with 45 studies and found a graded, concentration-dependent, significant relation between higher circulating fibrinogen and more severity of COPD [32]. Hence, it is plausible that elevated admission IL-6 and fibrinogen both are associated with hospital mortality in SCAP patients with COPD.
Some factors, such as increased creatinine and Troponin T, were associated with the mortality in univariate analysis. Nonetheless, the associations disappeared when adjusting for other risk factors. However, we should be cautious when explaining this conclusion because results from the existing literature on patients with SCAP or COPD are inconsistent with regard to whether they are associated with survival [33,34,35,36]. Future studies should address whether they could improve the evaluation and prediction of outcomes in SCAP patients with COPD.
The existing reports believed that risk stratification and early identification might contribute to optimizing the management of SCAP, with potential reduction of mortality [37]. Early assessment via prediction model could be instrumental to quantify in advance an individual patient’s risk of death when planning the therapies. On the other hand, the identification of patients at highest risk is pivotal to implement early measures and improve prognosis. The nomograms could be utilized as a complementary tool for decision making in clinical practice, or for SCAP-COPD patient selection in future studies on the basis of their risk stratification using the risk grouping. However, we acknowledge that some issues remain to be addressed. First, in our study, the diagnosis of COPD may lack strictness. It was difficult to determine the severity of COPD patients or to stratify them according to exacerbation histories, lung functions and symptoms from the data available. Thus, the identified independent risk factors need to be confirmed in COPD patients with different clinical characteristics. In addition, the nomogram might also have decreased predicting value in some specific subgroups of COPD patients. Then, the patients in present study are a little older (median age: 77 years old) compared to those SCAP patients in previous observational studies [19,20,21,22]. One leading cause is that we only strictly included confirmed SCAP-COPD patients because COPD is considered as an age-related disease. However, it is worth noting that different baseline characteristics existing among studies could result in diverse conclusions. Thus, large-scale, multicenter, prospective studies are desirable to validate, recalibrate, improve discriminative capacity and increase the generalizability of our prediction model. Besides, further information is needed to shed light on deeper understanding of pathophysiological mechanisms of SCAP patients with COPD. For instance, more efforts could be dedicated to investigate the impacts of various coexisting medical conditions, such as chronic cardiovascular diseases and diabetes, on the mortality of SCAP patients with COPD. Future researches should also consider the prognostic effects of more pre-admission individual features, including smoking status, vaccination history, prior antibiotic treatment and corticosteroid use, etc. Meanwhile, it is still controversial whether identified pathogens or imaging findings are related to the severity or mortality in those patients.
The main limitation of the current study is the single-center, retrospective design with selection bias. Then, the missing data might have reduced the effective sample size, caused inevitable bias and threatened the validity of the study. Third, although a number of potential risk factors have been analyzed, we cannot exclude that some unadjusted confounders could have affected the results or some untested variables would further improve the model. The model can be updated when more multicentric data become available.
Conclusion
In conclusion, we developed a prediction model for hospital mortality in patients with SCAP and COPD. The nomogram including seven risk factors with favorable predictive accuracy, discrimination, and clinical utility allows simple and rapid individual patient risk estimates. It can be used at admission of ICU to predict mortality to prompt early risk stratification and actionable measures in clinical practice after more external validation.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SCAP:
-
Severe community-acquired pneumonia
- COPD:
-
Chronic obstructive pulmonary disease
- ICU:
-
Intensiv care unit
- OR:
-
Odds ratio
- 95% CI:
-
95% confidence interval
- SBP:
-
Systolic blood pressure
- IL-6:
-
Interleukin-6
- BUN:
-
Blood urea nitrogen
References
Torres A, Cilloniz C, Niederman MS, et al. Pneumonia. Nat Rev Dis Primers. 2021;7(1):25. https://doi.org/10.1038/s41572-021-00259-0.
Aliberti S, Dela Cruz CS, Amati F, Sotgiu G, Restrepo MI. Community-acquired pneumonia. Lancet. 2021;398(10303):906–19. https://doi.org/10.1016/S0140-6736(21)00630-9.
Jain S, Self WH, Wunderink RG, et al. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med. 2015;373(5):415–27. https://doi.org/10.1056/NEJMoa1500245.
Torres A, Chalmers JD, Dela Cruz CS, et al. Challenges in severe community-acquired pneumonia: a point-of-view review. Intensive Care Med. 2019;45(2):159–71. https://doi.org/10.1007/s00134-019-05519-y.
Labaki WW, Rosenberg SR. Chronic obstructive pulmonary disease. Ann Intern Med. 2020;173(3):ITC17-32. https://doi.org/10.7326/AITC202008040.
Rabe KF, Watz H. Chronic obstructive pulmonary disease. Lancet. 2017;389(10082):1931–40. https://doi.org/10.1016/S0140-6736(17)31222-9.
Cavallazzi R, Ramirez J. Community-acquired pneumonia in chronic obstructive pulmonary disease. Curr Opin Infect Dis. 2020;33(2):173–81. https://doi.org/10.1097/QCO.0000000000000639.
Ma H, Liu T, Zhang Y, Ye Z, Jia W, Li Y. Impact of chronic obstructive pulmonary disease on mortality in community acquired pneumonia: a meta-analysis. J Comp Eff Res. 2020;9(12):839–48. https://doi.org/10.2217/cer-2020-0061.
Cilli A, Erdem H, Karakurt Z, et al. Community-acquired pneumonia in patients with chronic obstructive pulmonary disease requiring admission to the intensive care unit: risk factors for mortality. J Crit Care. 2013;28(6):975–9. https://doi.org/10.1016/j.jcrc.2013.08.004.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. 2015;350:g7594. https://doi.org/10.1136/bmj.g7594.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9. https://doi.org/10.1016/s0895-4356(96)00236-3.
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45-67. https://doi.org/10.1164/rccm.201908-1581ST.
Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–82. https://doi.org/10.1164/rccm.201701-0218PP.
Ramirez JA, Musher DM, Evans SE, et al. Treatment of community-acquired pneumonia in immunocompromised adults: a consensus statement regarding initial strategies. Chest. 2020;158(5):1896–911. https://doi.org/10.1016/j.chest.2020.05.598.
Caetano SJ, Sonpavde G, Pond GR. C-statistic: a brief explanation of its construction, interpretation and limitations. Eur J Cancer. 2018;90:130–2. https://doi.org/10.1016/j.ejca.2017.10.027.
Alba AC, Agoritsas T, Walsh M, et al. Discrimination and calibration of clinical prediction models: users’ guides to the medical literature. JAMA. 2017;318(14):1377–84. https://doi.org/10.1001/jama.2017.12126.
Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making. 2006;26(6):565–74. https://doi.org/10.1177/0272989X06295361.
Harrell Jr FE. Regression modeling strategies, with applications to linear models, logistic and ordinal regression, and survival analysis. Cham: Springer; 2015.https://doi.org/10.1007/978-3-319-19425-7.
Bonnesen B, Baunbæk Egelund G, Vestergaard Jensen A, et al. Is chronic obstructive pulmonary disease a risk factor for death in patients with community acquired pneumonia? Infect Dis (Lond). 2019;51(5):340–7. https://doi.org/10.1080/23744235.2019.1565416.
Dai RX, Kong QH, Mao B, et al. The mortality risk factor of community acquired pneumonia patients with chronic obstructive pulmonary disease: a retrospective cohort study. BMC Pulm Med. 2018;18(1):12. https://doi.org/10.1186/s12890-018-0587-7.
Gómez-Junyent J, Garcia-Vidal C, Viasus D, et al. Clinical features, etiology and outcomes of community-acquired pneumonia in patients with chronic obstructive pulmonary disease. PLoS ONE. 2014;9(8):e105854. https://doi.org/10.1371/journal.pone.0105854.
Shin B, Kim SH, Yong SJ, et al. Early readmission and mortality in acute exacerbation of chronic obstructive pulmonary disease with community-acquired pneumonia. Chronic Respir Dis. 2019;16:1479972318809480. https://doi.org/10.1177/1479972318809480.
Martin-Loeches I, Torres A. New guidelines for severe community-acquired pneumonia. Curr Opin Pulm Med. 2021;27(3):210–5. https://doi.org/10.1097/MCP.0000000000000760.
Peng Y, Zhong GC, Wang L, et al. Chronic obstructive pulmonary disease, lung function and risk of type 2 diabetes: a systematic review and meta-analysis of cohort studies. BMC Pulm Med. 2020;20(1):137. https://doi.org/10.1186/s12890-020-1178-y.
Aldibbiat AM, Al-Sharefi A. Do benefits outweigh risks for corticosteroid therapy in acute exacerbation of chronic obstructive pulmonary disease in people with diabetes mellitus? Int J Chronic Obstr Pulm Dis. 2020;15:567–74. https://doi.org/10.2147/COPD.S236305.
Gläser S, Krüger S, Merkel M, Bramlage P, Herth FJ. Chronic obstructive pulmonary disease and diabetes mellitus: a systematic review of the literature. Respiration. 2015;89(3):253–64. https://doi.org/10.1159/000369863.
Takahashi T, Yoshihisa A, Sugimoto K, et al. Associations between diabetes mellitus and pulmonary hypertension in chronic respiratory disease patients. PLoS ONE. 2018;13(10):e0205008. https://doi.org/10.1371/journal.pone.0205008.
Karakioulaki M, Stolz D. Biomarkers in pneumonia-beyond procalcitonin. Int J Mol Sci. 2019;20(8):2004. https://doi.org/10.3390/ijms20082004.
He X, Luo Q, Zhao L, Shang Y, Gao Z. Prognostic value of histidine-rich glycoprotein for community-acquired pneumonia. Dis Markers. 2022;2022:4713045. https://doi.org/10.1155/2022/4713045.
Luo B, Sun M, Huo X, Wang Y. Two new inflammatory markers related to the CURB-65 score for disease severity in patients with community-acquired pneumonia: the hypersensitive C-reactive protein to albumin ratio and fibrinogen to albumin ratio. Open Life Sci. 2021;16(1):84–91. https://doi.org/10.1515/biol-2021-0011.
Fermont JM, Masconi KL, Jensen MT, et al. Biomarkers and clinical outcomes in COPD: a systematic review and meta-analysis. Thorax. 2019;74(5):439–46. https://doi.org/10.1136/thoraxjnl-2018-211855.
Zhou B, Liu S, He D, et al. Fibrinogen is a promising biomarker for chronic obstructive pulmonary disease: evidence from a meta-analysis. Biosci Rep. 2020;40(7):BSR20193542. https://doi.org/10.1042/BSR20193542.
Wang X, Jiao J, Wei R, et al. A new method to predict hospital mortality in severe community acquired pneumonia. Eur J Intern Med. 2017;40:56–63. https://doi.org/10.1016/j.ejim.2017.02.013.
Flattet Y, Garin N, Serratrice J, Perrier A, Stirnemann J, Carballo S. Determining prognosis in acute exacerbation of COPD. Int J Chronic Obstr Pulm Dis. 2017;12:467–75. https://doi.org/10.2147/COPD.S122382.
Pavasini R, d’Ascenzo F, Campo G, et al. Cardiac troponin elevation predicts all-cause mortality in patients with acute exacerbation of chronic obstructive pulmonary disease: systematic review and meta-analysis. Int J Cardiol. 2015;191:187–93. https://doi.org/10.1016/j.ijcard.2015.05.006.
Vestjens SMT, Spoorenberg SMC, Rijkers GT, et al. High-sensitivity cardiac troponin T predicts mortality after hospitalization for community-acquired pneumonia. Respirology. 2017;22(5):1000–6. https://doi.org/10.1111/resp.12996.
Leoni D, Rello J. Severe community-acquired pneumonia: optimal management. Curr Opin Infect Dis. 2017;30(2):240–7. https://doi.org/10.1097/QCO.0000000000000349.
Acknowledgements
None.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 82072156), the Science and Technology Department of Sichuan Province (Grant Nos. 2019YFS0443, 2018JY0389), the National Key Research and Development Program of China (Grant No. 2016YFC1304303), key program of Sichuan Provincial Health Commission (Grant No. 18ZD002), and the Fundamental Research Funds for the Central Universities (Grant No. 2022SCU12055).
Author information
Authors and Affiliations
Contributions
DH, DH, LG, RY, WW, YS and ZL gave the study concept and design; all authors acquired, analyzed, and interpreted the data, and critically revised the manuscript for important intellectual content; DH, DH and LG drafted the manuscript; DH carried out the statistical analysis; YS and ZL supervised the study; All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the West China Hospital of Sichuan University Biomedical Research Ethics Committee (No. 2021-828), with waiver of written informed consent due to retrospective non-interventional design. All patient data was maintained with confidentiality.
Consent for publication
Consent for publication was provided by all authors.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Baseline characteristics of SCAP-COPD individuals in training cohort and testing cohort. Table S2. Numbers and percentages of missing values for each variable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, D., He, D., Gong, L. et al. A prediction model for hospital mortality in patients with severe community-acquired pneumonia and chronic obstructive pulmonary disease. Respir Res 23, 250 (2022). https://doi.org/10.1186/s12931-022-02181-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-02181-9