Abstract
Objective
Iron and steel industry workers are exposed to high levels of inhalable dust particles that contain various elements, including metals, and cause occupational lung diseases. We aim to assess the relationship between occupational dust exposure, systemic inflammation, and spirometric decline in a cohort of Chinese iron and steel workers.
Methods
We studied 7513 workers who participated in a Health Surveillance program at Wugang Institute for Occupational Health between 2008 and 2017. Time-weighted exposure intensity (TWEI) of dust was quantified based on self-reported dust exposure history, the experience of occupational hygienists, and historical data of dust exposure for workers with certain job titles. A linear mixed-effects model was used for association analyses.
Results
The average annual change of lung function was − 50.78 ml/year in forced expiratory volume in 1 s (FEV1) and − 34.36 ml/year in forced vital capacity (FVC) in males, and − 39.06 ml/year in FEV1 and − 26.66 ml/year in FVC in females. Higher TWEI prior to baseline was associated with lower longitudinal measurements of FEV1 and FVC but not with their decline rates. Higher WBC and its differential at baseline were associated with lower longitudinal measurements and a more rapid decline of FEV1 and FVC in a dose-dependent monotonically increasing manner. Moreover, the increase of WBC and its differential post-baseline was also associated with a more rapid decline of FEV1 and FVC.
Conclusions
Our findings support the important role of systemic inflammation in affecting the temporal change of lung function in iron and steel industry workers.
Similar content being viewed by others
Introduction
The iron and steel industry as a fundamental component of modern industrial infrastructure for the entire human society has employed millions of workers who were exposed to many chemical and physical hazards, workplace activities, or conditions [1]. Workers are exposed to high levels of inhalable dust particles containing various elements such as metals, silica, carbon, and polycyclic aromatic hydrocarbon, which could cause chronic occupational diseases such as chronic obstructive pulmonary disease (COPD) [2,3,4,5]. The International Agency for Research on Cancer has classified iron and steel founding processes as Group 1 human carcinogens based on sufficient evidence for lung cancer in humans [6]. Cross-sectional studies have established strong associations between dust exposure and lung function impairment in iron and steel workers [1, 7, 8]. However, the association between dust exposure in the working environment and lung function decline is inadequately studied.
Inhalation of dust particles containing metals and their compounds causes impairment to both pulmonary surfactant and respiratory function [4]. Occupational exposure to respirable dust in an iron foundry played a significant role in decreasing lung function and in increasing the risk of chronic airway obstruction in exposed workers [1, 2, 9]. In a longitudinal study from the Norwegian, the association of steel dust exposure with accelerated lung function decline was observed and smokers had stronger associations. A dose–response relationship between total dust exposure and the annual decline in FEV1 has been found among employees in smelters producing ferromanganese, silicomanganese, ferrochromium and silicon carbide [10].
White blood cell (WBC) counts and its differential (i.e., neutrophils, lymphocytes, monocytes, eosinophils, and basophils) are established systemic inflammatory markers and have been identified to be associated with lower FEV1 and airflow obstruction in occupational cohorts and general populations [11,12,13,14,15,16]. After the September 11, 2001 World Trade Center attacks, rescue and recovery workers were exposed to a high level of dust mixture and were later found to have high rates of airway injury, including excessive loss of lung function, airflow obstruction, and airway hyper-reactivity. Elevated blood neutrophil and eosinophil counts were independently associated with an accelerated FEV1 decline (64 mL/year or more), a well-established risk factor for COPD development [17]. Mechanisms underlying the observed associations may involve increased lung tissue damage due to the release of destructive enzymes or highly reactive oxygen species from neutrophils [18,19,20,21] or the generation of eosinophilia/Th2 inflammation in airways [14, 22].
Few studies have evaluated the associations between WBC counts and longitudinal changes of lung function in iron and steel workers. We hypothesized baseline WBC as a systemic inflammatory biomarker is associated with a lower lung function and a more rapid decline in a cohort of 7513 iron and steel industry workers. We also assessed the increase of WBC counts post-baseline and its association with the longitudinal change of spirometry.
Methods
A detailed description is available in supplemental materials.
Study subjects
This longitudinal study was conducted in 7575 employees from Wuyang Iron and Steel Company Limited (Hangang Group in Henan, China). The employees were required to participate in the Worker Health Surveillance program at the Wugang Institute for Occupational Health between 2008 and 2017. This company has been using the electric arc furnace technique to manufacture steel from scrap or direct reduced iron, melted by electric arcs, and mainly has steel making, continuous casting, rolling, and oxygen-making plants. According to the Reports of Occupational Hazard Control Assessment conducted by Henan Institute of Occupational Medicine in 2006 and 2007, inhalable dust and noise are the two occupational hazards that have samples exceeding the national standards (the permissible concentration time-weighted average of 8 mg/m3 for inhalable dust and 85 dB(A) for noise in China). This cohort was dynamic with workers entering and leaving the cohort at different times. In general, individual participants in this program received medical assessments every other year with medical surveillance workouts recommended by the China Ministry of Health. The de-identified data were obtained from the Wugang Institute for Occupational Health. The Research Ethics Committee of the Qingdao University School of Medicine approved the study protocol with a waiver of subject consent (QYFYWZLL25933).
Occupational dust exposure assessment
Employment history including occupation, length of employment, and occupational dust exposure (yes or no) for three consecutive jobs or positions were self-reported at study entry. Because no cohort members were newly employed at the baseline visit, we focused on detailed employment history including plant, workshop, and post at the Wuyang Iron and Steel Company prior to baseline visit to quantify occupational dust exposure. All study subjects belonged to 79 workshops from seven plants and the population was divided into three groups by tertiles based on the percentage of subjects reporting dust exposure. Combined with the consultation of occupational hygienists, historical personal air sampling data in 2006 and 2007 (Additional file 1: Table S1), and epidemiological consideration of sample size within each exposure category, the workshops were classified into low (n = 43, person-posts = 4034), medium (n = 20, person-posts = 3816), and high (n = 16, person-posts = 2562) exposure categories to maximize the statistical power of the study. We calculated time-weighted exposure intensity (TWEI) using the sum of exposure unit (coded as 0, 1, 2 for low, medium, and high) years divided by total years prior to the baseline of dust exposure for each individual.
Lung function paraments
Spirometry was performed for each individual without a bronchodilator every other year by a certified respiratory technician using a portable calibrated electronic spirometer (CHESTGRAPH HI-701, Japan) in accordance with the American Thoracic Society (ATS)/European Respiratory Society standards(ERS) [23]. The spirometer was checked every day for leaks by a calibrated syringe. Persons were in the standing position with a nose clip used. After two or more practice blows, FEV1 and FVC were determined as the highest value from the results of measurements. Standing height and body weight were measured and recorded at each test occasion. Forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), and FEV1/FVC ratio were used in this study. Percent predicted values were calculated using the equations for Asian adults supplied in the user’s manual.
Complete blood count with differential
Peripheral venous blood samples were drawn from the antecubital veins of patients after overnight fasting. The blood samples were collected into lithium heparin-containing tubes to avoid pseudo thrombocytopenia. The number of red blood cells (including red blood cells, hemoglobin and hematocrit, etc.), white blood cells (WBC), platelets, and WBC differential counts (i.e., neutrophils, lymphocytes, monocytes, basophils, and eosinophils) were measured by a hematology analyzer (Sysmex. XS-500ix, China). Mid-range absolute counts (MID) include monocytes, eosinophils, basophils, blasts and other precursor white cells that fall in a particular size range. Absolute cell counts were used in the analyses. Baseline and follow-up blood samples were analyzed using the same machine operated by trained technicians.
Data analysis
Workers with airway obstruction (defined as FEV1/FVC < 0.7) at baseline (n = 20) or without spirometry data (n = 42) were excluded from this study, thus leaving 7513 workers with at least one spirometry measurement for data analyses. The sample size evolution for different analyses was summarized in Fig. 1. Females were more likely to conduct less physically intensive assignments, thus had less exposure to occupational hazards (Table 1). Therefore, all data analyses were conducted in males and females separately because of the division of labor by sex in heavy industry. A prudent analytical plan was developed to analyze the relationship among dust exposure, WBC count, and longitudinal spirometric decline with a careful assessment of important covariates, dose–response relationship, and potential confounding effects by linear mixed-effects model. First, a linear mixed-effects model with a subject-specific random intercept was used to assess the associations between occupational dust exposure (i.e., TWEI and years of dust exposure) prior to baseline and longitudinal spirometry with adjustment of important covariates. An interaction term between time-in-cohort (TIC) and prior occupational dust exposure was included in the model to assess whether lung function decline varied by previous occupational dust exposure. Baseline spirometry and its interaction with TIC were included in the models to minimize its effect on the association between occupational dust exposure and lung function decline. Second, similar approaches were taken to assess the association of prior occupational dust exposure on longitudinal measurements of WBC count and differential. Third, we also used linear mixed-effects models to assess the association of WBC count and differential at baseline with longitudinal measurements of lung function and its decline. WBC count and differential were included in the model as continuous variables first, then converted into categorical variables to assess their dose–response relationship. Using WBC count and differential collected at the same visits of spirometry in the model did not change the associations observed in models using baseline data for WBC count and differential. We further analyzed the elevation of WBC and its differential post-baseline and their association with lung function decline. Finally, three-way interactions (e.g., current smoker × TWEI × TIC or current smoker × WBC × TIC) with their two-way interactions and main effects were included in the models to analyze the potential effect modification of cigarette smoking on the associations of longitudinal lung function with occupational dust exposure or WBC count and differential. Data analyses were performed using SAS version 9.4 (site 70239492).
Results
Demographics of study subjects
This study included 6188 male and 1325 female workers with an average age of 34.5 years at study entry (Table 1). On average, workers reported 13 years of occupational dust exposure at the Wuyang Iron and Steel Company, concordant with the fact that the Company was the first employer for most cohort members. The median follow-up duration in the cohort (TIC) was 6 years, which allowed for three to four spirometry measurements. In total, 25,164 spirometry measurements were obtained from 7513 workers. The average percent predicted values of FEV1 and FVC at baseline were over 100%. Airflow obstruction was identified in 22 subjects during follow-up evaluations, resulting in an incidence of 2.9 cases per 1000 person-years.
Occupational dust exposure
Median inhalable dust concentrations (8-h time-weighted average [TWA]) for workshops classified in medium and high exposure categories were 0.91–1.45 and 7.45–10.35 mg/m3, between 2006 and 2007, respectively. Ninety percent of dust mass was non-silica (potentially as metal dust). Size distribution analysis found over 80% of particles had sizes less than 5 μm. No occupational monitoring data was available for the low exposure category. However, PM2.5 levels ranged 33 to 108 μg/m3 in non-heating seasons and 73 to 203 μg/m3 in heating seasons reported by the national air quality monitoring stations closest to Wugang city (about 30 miles away) between 2013 and 2017. The entire company area could be polluted by industrial dust due to its location in a small valley, which is 5 km long and 1.9 km wide with north and west sides surrounded by mountains. The median TWEI was 1.0 units for male workers and 0.19 units for female workers, supporting male workers having much higher occupational dust exposure.
Occupational dust exposure and spirometry
The average annual change of FEV1, FVC, and FEV1/FVC ratio during follow-up were 50.78 ml, 34.36 ml, and 0.49 in males (Table 2, model 1) and 39.06 ml, 26.66 ml, and 0.50 in females (Additional file 1: Table S2, model 1), respectively. Higher TWEI prior to baseline was associated with lower longitudinal measurements of FEV1 and FVC in either sexes and with females more vulnerable to the adverse effect of occupational dust exposure (e.g., − 21.76 ml in males versus − 41.96 ml in females for FEV1 and − 28.71 ml in males versus − 36.67 ml in females for FVC, per unit increase of TWEI, Table 2 and Additional file 1: Table S2, model 1), but had no effect on FEV1/FVC ratio. The most probable reason for lower spirometry in workers with higher past occupational dust exposure may be their more rapid initial decline of lung function or inadequate ongoing lung growth and development after the initiation of exposure. However, occupational dust exposure prior to baseline was associated with a slower annual decline of FEV1 and FVC in either sexes (Table 2 and Additional file 1: Table S2, model 2). We hypothesized a slower decline of FEV1 and FVC associated with higher TWEI could be due to the “healthy worker effect” and certain worker characteristics could mediate such associations. Univariate analyses identified workers with higher TWEI were younger and taller, and had shorter years of dust exposure for either sexes at baseline (Additional file 1: Table S3). Age and years of dust exposure were highly correlated with Spearman correlation coefficients > 0.93 for either sexes and could not be the factors mediating the observed associations because occupational dust exposure history and its interaction with TIC had been included in the model (Table 2 and Additional file 1: Table S2). Taller workers had a slower decline of FEV1 and FVC and a faster decline of FEV1/FVC ratio for either sexes and inclusion of interaction term of height and TIC in model 2 completely nullified the significance of interaction term of TWEI and TIC (Additional file 1: Tables S4 and S5), suggesting that height may be the healthy worker characteristic that mediates the association between higher TWEI and slower decline of spirometry. Moreover, the inclusion of any additional interaction terms with TIC (e.g., smoking status, HGB, packyears, and BMI) had no impact on the estimate and significance for the interaction term of TWEI and TIC (data not shown).
Occupational dust exposure and longitudinal data of WBC count and its differential
Current smokers, packyears and years of dust exposure in males (Table 3), and BMI in either sexes (Table 3 and Additional file 1: Table S6) were associated with higher WBC count and all differential cell counts (neutrophils, lymphocytes. and mid-range absolute counts), consistent with the fact that cigarette smoking, higher BMI, and years of dust exposure increased systemic inflammation. However, age and TIC were associated with lower levels of WBC count and most differential counts in either sexes, suggesting aging may reduce general immunity. Interestingly, there was no evidence supporting TWEI associated with increased WBC count and differential cell counts in either sexes. In opposite, TWEI was associated with lower lymphocyte count in males (Table 3) and with lower mid-range absolute count (MID) count in either sexes (Table 3 and Additional file 1: Table S6). Self-reported exposure to toxic gases (e.g., carbon monoxide, nitrogen monoxide and dioxide, and benzene and its derivatives) was not associated with WBC count and its differential (data not shown).
Associations of WBC count and its differential with a spirometric decline
Higher baseline WBC count and differential (neutrophil and lymphocyte) counts were associated with lower longitudinal measurements and a more rapid decline of FEV1 and FVC in male workers only (Table 4). The MID count was associated with a more rapid decline of FEV1 and FVC in male workers only (Table 4). Lymphocyte count was associated with lower longitudinal measurements of FEV1 and FVC but not with a decline in females (Table 4). We further stratified workers into quartiles based on WBC count or differential counts to characterize their dose–response relationship with longitudinal lung function measurements and their declines (Additional file 1: Table S7). Higher WBC count and differential (neutrophil and lymphocyte count) were monotonically associated with lower longitudinal measurements and a more rapid decline of FEV1 and FVC in males only (Additional file 1: Table S7 and Additional file 1: Figure S1). MID was monotonically associated with a more rapid decline of FEV1 and FVC in male workers only (Additional file 1: Table S7 and Figure S1). Lymphocyte count was associated with lower longitudinal measurements of FEV1 and FVC in a dose–response manner in females (Additional file 1: Table S7).
We further tested whether elevation of WBC count and its differential post-baseline, as an indicator for the elevation of systemic inflammation over time was associated with a more rapid decline of lung function. Change in WBC and its differential for each visit relative to baseline level were calculated and were included in the linear mixed-effects models together with its interaction of TIC. Interestingly, the elevation of WBC and its differential (e.g., neutrophil and MID) was associated with a more rapid decline of FEV1 and FVC in either sexes (Table 5). Moreover, the magnitude of association seems to be more robust in female than male workers. Elevation of lymphocyte count was associated with a more rapid FEV1 decline in male workers only, resulted in a more rapid decline of FEV1/FVC ratio.
Sensitivity analyses
We are concerned that the associations between occupational dust exposure or WBC count and differential and lung function decline could be potentially confounded by cigarette smoking. None of these three-way interaction terms on current smoker × TWEI × TIC or current smoker × WBC × TIC were statistically significant (data not shown). We also repeated the main analyses in subjects (n = 6735) with two or more visits, findings similar to that seen in the entire 7513 workers were identified. In addition, we calculated the time-weighted exposure intensity (TWEI) based on self-reported dust exposure history up to every medical surveillance and observed the same trend for the associations between dust exposure, WBCs and spirometric decline. (data not shown).
Discussion
In this longitudinal cohort of 7513 workers, occupational exposure to inhalable particles containing metal elements prior to baseline evaluation was inversely associated with longitudinal measurements of FEV1 and FVC over a follow-up period of 10 years. We observed that cohort members with high levels of baseline WBC counts and differential had lower longitudinal measurements and a more rapid decline of FEV1 and FVC in male workers in a dose-dependent manner. Moreover, the elevation of WBC counts and its differential count post-baseline as an indicator of increasing systemic inflammation over time was associated with a more rapid decline of FEV1 and FVC in either sexes. Finally, sex disparity of the associations between dust exposure, WBC, and lung function was identified with stronger adverse effects of dust exposure or change of WBC seen in females as well as stronger effects of baseline WBC seen in males. The mechanisms underlying the sex disparity may be attributed to differences in dust exposure level [24], inherited differences in lung structure [25], or differences in sex hormones regulating lung homeostasis upon the challenge of dust exposure.
Occupational exposure to inhalable dust in the iron and steel industry has been shown to compromise lung function and increase the risk of chronic airflow obstruction in exposed workers [1, 2, 9, 10]. In this study, the decline rates of FEV1 and FVC are much faster than those observed in current and former cigarette smokers from a NM, USA-based Lovelace Smokers cohort with a median packyears of 36.0 and relatively healthy lung function, but comparable to smokers from Pittsburgh Lung Screening Study cohort with a median packyears of 59 and much-compromised lung function [26] and from Lung Health Study with all participants having mild to moderate airway obstruction [27], supporting the adverse effects of occupational dust exposure on the age-related decline of spirometry. A case–control study from New York City firefighters has shown that inhalable dust could remain in the lungs and be pro-inflammatory for up to 10 months after cessation of fire smoke exposure [28, 29]. However, we did not see an accelerated FEV1 and FVC decline associated with dust exposure prior to baseline. This finding was not altered even when dust exposure calculated up to each physical examination date was included in the model. Such patterns of results were supported by a most recent study in which prior airborne occupational exposures (e.g., biological dust, mineral dust, gases/fumes, insecticides, herbicides, fungicides, aromatic, chlorinated, other solvents, and metals) were associated with lower lung function measurements but not with annual decline using the Lifelines Cohort Study [30]. This could be explained by that most workers in our study have been working at a job title with occupational exposures for more than a decade prior to the baseline visit. Thus, workers may already develop resistance or saturation, a state of indifference or non-reactivity towards a substance that would normally be expected to excite a more exaggerated health effect [30]. A second reasonable explanation is that workers who are sensitive to dust-induced health effects could have switched their job with lower dust exposure or the pre-employment selection criteria could select subjects who are less likely to be affected by occupational dust exposure on lung function decline. Indeed, we did find that workers at occupational positions with higher dust exposure tend to be taller than workers from other positions and height is associated with better lung function and greater resilience for age-related lung function decline.
Higher WBC and its differential at baseline were associated with lower longitudinal measurements of lung function and a higher decline rate of FEV1 and FVC among the male workers. Baseline WBC counts implied the overall levels of inflammation and the post-baseline WBC counts change reflected the increase of system inflammation over time. Besides, this association is independent of occupational dust exposure. Furthermore, although on average WBC and its differential declined over time, the elevation of WBC and its differential post-baseline was associated with a more rapid decline of FEV1 and FVC in either sexes as well. These findings strongly support our hypothesis that elevated systemic inflammatory markers predict a more rapid decline of lung function in workers [11, 31, 32]. However, the temporal relationship between baseline WBC and its differential and subsequent lung function change and the compelling dose–response relationship does not directly support a causal relationship between systemic inflammation and lung function impairment. Instead, it may reflect a latent condition that workers with higher systemic inflammation are more vulnerable to dust exposure-induced health effects. The lack of a positive correlation between TWEI and WBC and its differential also suggested this latent inflammatory condition is more reflective of individual predisposition rather than an acquired trait due to chronic iron and steel dust exposure. Predisposition is an increased likelihood of developing a particular disease based on a person's genetic makeup rather than acquired character. The magnitude of associations of lung function or its decline with WBC and its differential is very comparable and this does not support a more dominant effect of certain leucocytes. Thus, all these suggest systemic inflammation as a holistic readout of individual predisposition that well predicts the severity of pulmonary toxicity caused by dust exposure containing metals in workers [8, 11].
We also found that elevation of post-baseline lymphocyte count was associated with a more rapid decline of FEV1/FVC ratio in male workers only. The ratio of FEV1 to FVC measures the amount of air a person can forcefully exhale in one second relative to the total amount of air individuality can exhale, which is the established index for diagnosing airway obstruction [33]. This ratio is decreased in obstructive lung disorders and normal in restrictive lung disorders. Research on COPD patients and healthy participants found higher levels of lymphocytes in COPD patients than the control group [34]. Chronic obstructive pulmonary disease is associated with inflammation of airway epithelium, including an increase in the number of intraepithelial T cells. Increased apoptosis of these T cells may result in unbalanced cellular homeostasis, defective clearance of apoptotic material by monocytes/macrophages, secondary necrosis, and prolongation of the inflammatory response. The increased T-cell death may be associated with the upregulation of apoptotic pathways, TGF-beta, TNF-alpha, and Fas in the peripheral blood [35].
This present study benefits greatly from a large sample size, high-quality data for longitudinal measurements of lung spirometry and WBC, and a long follow-up period that together contributes to sufficient statistical power and a more precise assessment of the magnitude of associations. However, this study does have limitations. Due to the lack of reliable occupational monitoring data for all years except 2006 and 2007, for many job posts, and the low exposure category, the job-exposure matrix could not be established for studied subjects. Second, we do not have the resources to assess what has happened in the first ten years of employment of the enrolled workers. A cohort with careful and repeated assessment of occupational exposure would help to disentangle the relationship between dust exposure, systemic inflammation, and the initial decline of lung function.
Conclusion
In conclusion, we have shown that previous occupational exposure to inhalable dust-containing metals resulted in a reduction in FEV1 and FVC. Higher WBC and its differential at baseline or elevation post-baseline were associated with a more rapid decline of FEV1 and FVC. Future studies should focus on a more quantitative assessment of occupational exposure and its constituents, a cohort of new employees to detect early changes of health effects after exposure initiation, and novel local and systemic inflammation biomarkers [36].
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Abbreviations
- FEV1:
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- COPD:
-
Chronic obstructive pulmonary disease
- WBC:
-
White blood cell
- NEU:
-
Neutrophilic granulocyte
- LYM:
-
Lymphocyte
- MID:
-
Mid-range absolute count
- BMI:
-
Body mass index
- TWEI:
-
Time-weighted exposure intensity
- ATS:
-
American Thoracic Society
- ERS:
-
European Respiratory Society standards
- TIC:
-
Time in cohort
- TWA:
-
Time-weighted average
- SE:
-
Standard error of mean
- M:
-
Mean
- SD:
-
Standard deviation
- Q:
-
Quartile
References
Gomes J, Lloyd OL, Norman NJ, Pahwa P. Dust exposure and impairment of lung function at a small iron foundry in a rapidly developing country. Occup Environ Med. 2001;58(10):656–62.
Wang ML, McCabe L, Hankinson JL, Shamssain MH, Gunel E, Lapp NL, Banks DE. Longitudinal and cross-sectional analyses of lung function in steelworkers. Am J Respir Crit Care Med. 1996;153(6 Pt 1):1907–13.
Szram J, Schofield SJ, Cosgrove MP, Cullinan P. Welding, longitudinal lung function decline and chronic respiratory symptoms: a systematic review of cohort studies. Eur Respir J. 2013;42(5):1186–93.
Ruediger HW. Hard metal particles and lung disease: coincidence or causality? Respiration. 2000;67(2):137–8.
Hamzah N, Tamrin SBM, Ismail NH. Respiratory symptoms and pulmonary function among male steel workers in Terengganu, Malaysia. Malay J Public Health Med. 2014;14:10–8.
Loomis D, Guha N, Hall AL, Straif K. Identifying occupational carcinogens: an update from the IARC Monographs. Occup Environ Med. 2018;75(8):593–603.
Chen P-C, Doyle PE, Wang J-D. Respirable dust exposure and respiratory health in male Taiwanese steelworkers. Ind Health. 2006;44(1):190–9.
Hamzah NA, Mohd Tamrin SB, Ismail NH. Metal dust exposure and lung function deterioration among steel workers: an exposure-response relationship. Int J Occup Environ Health. 2016;22(3):224–32.
Girma F, Kebede Z. Dust exposure associations with lung function among ethiopian steel workers. Ann Glob Health. 2019. https://doi.org/10.5334/aogh.2422.
Johnsen HL, Hetland SM, Benth JS, Kongerud J, Søyseth V. Dust exposure assessed by a job exposure matrix is associated with increased annual decline in FEV1: a 5-year prospective study of employees in Norwegian smelters. Am J Respir Crit Care Med. 2010;181(11):1234–40.
Koo H-K, Kang HK, Song P, Park HK, Lee S-S, Jung H. Systemic white blood cell count as a biomarker associated with severity of chronic obstructive lung disease. Tuberc Respir Dis (Seoul). 2017;80(3):304–10.
Thomsen M, Ingebrigtsen TS, Marott JL, Dahl M, Lange P, Vestbo J, Nordestgaard BG. Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease. JAMA. 2013;309(22):2353–61.
Ray A, Kolls JK. Neutrophilic inflammation in asthma and association with disease severity. Trends Immunol. 2017;38(12):942–54.
Hastie AT, Martinez FJ, Curtis JL, Doerschuk CM, Hansel NN, Christenson S, Putcha N, Ortega VE, Li X, Barr RG, et al. Association of sputum and blood eosinophil concentrations with clinical measures of COPD severity: an analysis of the SPIROMICS cohort. Lancet Respir Med. 2017;5(12):956–67.
Sparrow D, Glynn RJ, Cohen M, Weiss ST. The relationship of the peripheral leukocyte count and cigarette smoking to pulmonary function among adult men. Chest. 1984;86(3):383–6.
Chan-Yeung M, Abboud R, Buncio AD, Vedal S. Peripheral leucocyte count and longitudinal decline in lung function. Thorax. 1988;43(6):462–6.
Zeig-Owens R, Singh A, Aldrich TK, Hall CB, Schwartz T, Webber MP, Cohen HW, Kelly KJ, Nolan A, Prezant DJ, et al. Blood leukocyte concentrations, FEV decline, and airflow limitation. A 15-year longitudinal study of world trade center-exposed firefighters. Ann Am Thorac Soc. 2018;15(2):173–83.
Wang J. Neutrophils in tissue injury and repair. Cell Tissue Res. 2018;371(3):531–9.
Janoff A. Biochemical links between cigarette smoking and pulmonary emphysema. J Appl Physiol Respir Environ Exerc Physiol. 1983;55(2):285–93.
Park HS, Kim SR, Lee YC. Impact of oxidative stress on lung diseases. Respirology. 2009;14(1):27–38.
Valko M, Rhodes CJ, Moncol J, Izakovic M, Mazur M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact. 2006. https://doi.org/10.1016/j.cbi.2005.12.009.
Bafadhel M, Pavord ID, Russell REK. Eosinophils in COPD: just another biomarker? Lancet Respir Med. 2017;5(9):747–59.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38.
Wang T, Wang H, Chen J, Wang J, Ren D, Hu W, Wang H, Han W, Leng S, Zhang R, et al. Association between air pollution and lung development in schoolchildren in China. J Epidemiol Community Health. 2020. https://doi.org/10.1136/jech-2020-214283.
Cao X, Lin L, Sood A, Ma Q, Zhang X, Liu Y, Liu H, Li Y, Wang T, Tang J, et al. Small airway wall thickening assessed by computerized tomography is associated with low lung function in Chinese carbon black packers. Toxicol Sci. 2020. https://doi.org/10.1093/toxsci/kfaa134.
Leng S, Diergaarde B, Picchi MA, Wilson DO, Gilliland FD, Yuan JM, Siegfried JM, Belinsky SA. Gene promoter hypermethylation detected in sputum predicts FEV1 decline and all-cause mortality in smokers. Am J Respir Crit Care Med. 2018;198(2):187–96.
Hansel NN, Ruczinski I, Rafaels N, Sin DD, Daley D, Malinina A, Huang L, Sandford A, Murray T, Kim Y, et al. Genome-wide study identifies two loci associated with lung function decline in mild to moderate COPD. Hum Genet. 2013;132(1):79–90.
Fireman EM, Lerman Y, Ganor E, Greif J, Fireman-Shoresh S, Lioy PJ, Banauch GI, Weiden M, Kelly KJ, Prezant DJ. Induced sputum assessment in New York City firefighters exposed to World Trade Center dust. Environ Health Perspect. 2004;112(15):1564–9.
Weiden MD, Naveed B, Kwon S, Segal LN, Cho SJ, Tsukiji J, Kulkarni R, Comfort AL, Kasturiarachchi KJ, Prophete C, et al. Comparison of WTC dust size on macrophage inflammatory cytokine release in vivo and in vitro. PLoS ONE. 2012;7(7): e40016.
Faruque MO, Vonk JM, Kromhout H, Vermeulen R, Bültmann U, Boezen HM. Airborne occupational exposures and lung function in the lifelines cohort study. Ann Am Thorac Soc. 2021;18(1):60–67.
Nerpin E, Jacinto T, Fonseca JA, Alving K, Janson C, Malinovschi A. Systemic inflammatory markers in relation to lung function in NHANES. 2007–2010. Respir Med. 2018;142:94–100.
McKeever T, Saha S, Fogarty AW. The association between systemic inflammatory cellular levels and lung function: a population-based study. PLoS ONE. 2011;6(7): e21593.
Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Criner GJ, Frith P, Halpin DMG, Han M, et al. global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019. https://doi.org/10.1183/13993003.00164-2019.
Guiedem E, Ikomey GM, Nkenfou C, Walter PE, Mesembe M, Chegou NN, Jacobs GB, Okomo Assoumou MC. Chronic obstructive pulmonary disease (COPD): neutrophils, macrophages and lymphocytes in patients with anterior tuberculosis compared to tobacco related COPD. BMC Res Notes. 2018;11(1):192.
Hodge SJ, Hodge GL, Reynolds PN, Scicchitano R, Holmes M. Increased production of TGF-beta and apoptosis of T lymphocytes isolated from peripheral blood in COPD. Am J Physiol Lung Cell Mol Physiol. 2003;285(2):L492-499.
Wang H, Duan H, Meng T, Yang M, Cui L, Bin P, Dai Y, Niu Y, Shen M, Zhang L, et al. Local and systemic inflammation may mediate diesel engine exhaust-induced lung function impairment in a chinese occupational cohort. Toxicol Sci. 2018;162(2):372–82.
Acknowledgements
The authors would like to thank students from the School of Public Health Qingdao University (Yurong Li, Yangyang Ren, Pengyue Guo, Ning Wang, Yidan Hu, Jun Lian, Xiangming Yang, Lin Wang, and Yifei Gao) and staff from Wugang Institute for Occupational Health (Xiaohe Wu, Qiufeng Cheng, Xiaowei Guo, Yanqiu Wang, Zhen Guo, Xingpei Li, Ning Yang, and Ping Cao) for data input. The data collection, field survey, and majority of data analysis and result summary were completed during Dr. Leng’s affiliation with Qingdao University prior to 2020. Critical revision and submission of the manuscript were conducted during Dr. Leng’s employment at the University of New Mexico since 2020.
Funding
This study is funded by the National Natural Science Foundation of China (91643203, 81872600, 81872651, and 81973012) and the Guangdong Provincial Natural Science Foundation Team Project (2018B030312005).
Author information
Authors and Affiliations
Contributions
YZ and SL conceived of and designed the study; NK, HW, YL, and HZ performed the data collection and data input; NK conducted the data analyses, tabulated and interpreted the results, and drafted the first version of the manuscript; GC, HZ, and SY were occupational hygienists; SY was the certified pulmonary technician and conducted all spirometry; JL, XC, and TW assist with SAS programming; XL and JT edited the first version of the manuscript; AS, YZ, and SL critically edited the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The Research Ethics Committee of the Qingdao University School of Medicine approved the study protocol with a waiver of subject consent (QYFYWZLL25933, 16Sep2020).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
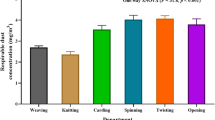
Inhalable dust concentration (mg/m3) for different exposure category. Table S2. The association betwwen dust exposure and spirometry in female workers using linear mixeds-effects model (n = 1295). Table S3. The univariate analyses assessing the associations between time-weighted exposure intensity and characteristic variables as the outcomes. Table S4. The influence of inclusion of height and TIC interaction on the estimates and P values for TWEI and TIC interaction in male workers using linear mixed-effects model (n = 6100). Table S5. The influence of inclusion of height and TIC interaction on the estimates and P values for TWEI and TIC interaction in female workers using linear mixed-effects model (n = 1295). Table S6. The association between dust exposure and white blood cell count and its differential in female workers using linear mixed-effects model (n = 1295). Table S7. The association between categorized white blood cell count and its differential at baseline on longitudinal spirometry using linear mixed-effects model to assess the dose–response relationship. Figure S1. Dose–response relationship between WBC count and its differential and FEV1 decline in workers by sex. Baseline WBC count and its differential were converted into categorical variables based on sex-specific 25th percentile, median, and 75th percentile (see Table S7 for range limits). Linear mixed-effects model assessed the of quartile group status and FEV1 decline with Q1 as the reference. Q1, Q2, Q3, and Q4 group status was coded as numerical 0, 1, 2, and 3 in the trend test. The detailed modeling strategy was introduced in the footnote of Table S7. A significant dose–response relationship was identified for WBC, NEU, LYM, and MID in male workers only. A more rapid FEV1 decline was identified in male workers with higher levels of WBC or its differential. Only three groups for MID in males were available due to the discrete distribution of the MID data. A statistically significant test results (*) means P < 0.05 compared to the Q1 group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kong, N., Chen, G., Wang, H. et al. Blood leukocyte count as a systemic inflammatory biomarker associated with a more rapid spirometric decline in a large cohort of iron and steel industry workers. Respir Res 22, 254 (2021). https://doi.org/10.1186/s12931-021-01849-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-021-01849-y