Abstract
Background
Acute respiratory distress syndrome (ARDS) is characterized by alveolar epithelial disruption. Lipoxins (LXs), as so-called “braking signals” of inflammation, are the first mediators identified to have dual anti-inflammatory and inflammatory pro-resolving properties.
Methods
In vivo, lipoxinA4 was administrated intraperitoneally with 1 μg/per mouse after intra-tracheal LPS administration (10 mg/kg). Apoptosis, proliferation and epithelial–mesenchymal transition of AT II cells were measured by immunofluorescence. In vitro, primary human alveolar type II cells were used to model the effects of lipoxin A4 upon proliferation, apoptosis and epithelial–mesenchymal transition.
Results
In vivo, lipoxin A4 markedly promoted alveolar epithelial type II cells (AT II cells) proliferation, inhibited AT II cells apoptosis, reduced cleaved caspase-3 expression and epithelial–mesenchymal transition, with the outcome of attenuated LPS-induced lung injury. In vitro, lipoxin A4 increased primary human alveolar epithelial type II cells (AT II cells) proliferation and reduced LPS induced AT II cells apoptosis. LipoxinA4 also inhibited epithelial mesenchymal transition in response to TGF-β1, which was lipoxin receptor dependent. In addition, Smad3 inhibitor (Sis3) and PI3K inhibitor (LY294002) treatment abolished the inhibitory effects of lipoxinA4 on the epithelial mesenchymal transition of primary human AT II cells. Lipoxin A4 significantly downregulated the expressions of p-AKT and p-Smad stimulated by TGF-β1 in primary human AT II cells.
Conclusion
LipoxinA4 attenuates lung injury via stimulating epithelial cell proliferation, reducing epithelial cell apoptosis and inhibits epithelial–mesenchymal transition.
Similar content being viewed by others
Background
Acute respiratory distress syndrome (ARDS), an acute inflammatory pulmonary process, causes intense and diffuse alveolar architecture damage and the development of interstitial and alveolar protein-rich edema, leading to acute hypoxemic respiratory failure [1, 2]. In ARDS, the alveolar epithelium is the primary target where cell damage occurs. The degree of alveolar epithelial damage can predict the outcome of ARDS [3, 4]. Consequently, the repair of the alveolar epithelium plays a crucial role in the resolution of ARDS [4]. Recent literatures have demonstrated that apoptosis of alveolar epithelial cells contributed to the loss of alveolar epithelial cells and the development of ARDS [5,6,7]. Inhibiting apoptosis has been shown to attenuate lung injury in animal models [6].
Epithelial-mesenchymal transition (EMT) is the process in which epithelial cells differentiate into mesenchymal (fibroblast-like) cells expressing mesenchymal biomarkers such as α-Smooth muscle actin (α-SMA), and N-cadherin [8]. The EMT was associated with lung injury and could lead to the prognosis of ARDS [9]. Furthermore, inflammation stimulated by HCL can also lead to EMT in HCL-induced ARDS models [10, 11]. Another study demonstrated that trichostatin A attenuated ventilation augmented-EMT playing a role in the reparative phase of ARDS [12]. Both EMT and apoptosis of the alveolar epithelium are crucial for the progression of ARDS.
Lipoxins (LXs), as so-called “braking signals” of inflammation, are endogenous lipid mediators derived from arachidonic acid [13]. They were the first mediators identified to have dual anti-inflammatory and inflammatory pro-resolving properties [14]. Lipoxin A4 (LXA4) was shown to inhibit neutrophil and eosinophil recruitment [15], promote macrophage clearance of apoptotic neutrophils [16], and increase survival in a rat CLP model [17]. Our previous studies showed that LXA4 inhibited inflammation following inhaled LPS-induced lung injury [18]. LXA4 increased alveolar fluid clearance in rat lung injury model [19], and LXA4 promoted alveolar epithelial repair by stimulating epithelial cell wound repair, proliferation, and reducing apoptosis in vitro [20].
The alveolar epithelial cells may either undergo apoptosis or EMT in ARDS. In this study, we aimed to investigate whether LXA4 could promote type II alveolar lung epithelial cells proliferation, whilst inhibiting apoptosis in vivo and in vitro. Furthermore, we also investigated if LXA4 inhibited EMT in vivo and reduced TGF-β1 induced EMT in human primary type II alveolar epithelial cells.
Materials and methods
Materials
LXA4 and LY294002 (PI3K inhibitor) were obtained from Cayman Chemical Company (Ann Arbor, MI, USA). LPS (Escherichia coli serotype 055: B5), Sis3 (smad3 inhibitor) and SP-C antibody were purchased from Sigma (St Louis, MO, USA), BOC-2 (N-t- BOC-PHE-LEU-PHE-LEU-PHE; Gene Script USA Inc., Piscataway, NJ, USA) and BML-111 (Enzo Life Sciences, NY, United States) were purchased from Shang Hai Bo Yun. Antibody against anti-alpha smooth muscle actin (α-SMA) antibody, Vimentin and the secondary antibodies were obtained from Abcam Company (Cambridge, UK). Antibodies against E-cadherin and N-cadherin were from Cell Signaling Technology Company (Boston, USA). Recombinant Human TGF-β1 (HEK293 derived) was purchased from Peprotech Company (Rocky Hill, USA). DMEM and FBS were purchased from Life Technologies BRL (Grand Island, NY). Protein levels were determined using a Bicinchoninic acid kit (Thermo Scientific).
Primary human lung alveolar type II (HAT II) cell culture
Human alveolar type II (HAT II) cells were isolated from lungs of grossly normal appearance after lung tumor resection. The cells were isolated in accordance with approval from the local research ethics committees at the University of Wenzhou Medical University (Wen Zhou, China). Primary human AT II cells were extracted according to the methods described previously (see online supplement) [20].
Stimuli and inhibitors
HAT II cells were treated with LXA4 (0, 0.1, 1, 10, 100 nM, Cayman Chemical Company, USA) with or without LPS (1 μg/ml, Escherichia coli serotype 055:B5). Appropriate vehicle controls were used for all experiments with inhibitors. Inhibitors were used at the following concentrations according to manufacturers’ instructions: LY294002, a PI3-kinase inhibitor (Calbiochem, Nottingham, UK); Sis3 (smad3 inhibitor), Boc-2 (N-t-Boc-Phe-Leu-Phe-Leu-Phe; GenScript USA Inc., the ALXR antagonist) and BML-111(Enzo Life Sciences, NY, United States, the ALXR agonist), all at 10 μM. Inhibitors were added to cells 30 min before every treatment.
Animal model of ALI/ARDS
C57BL/6 J mice at 6–8 weeks of age were purchased from the Shanghai SLAC Laboratory Animal Co. Ltd. The animals were acclimatized for 7 days prior to experimental use. Mice were caged with free access to food and fresh water in a temperature-controlled room (22–24 °C) on a 12-h light/dark cycle. Mice (male; ethics code: 2015048) were randomized into 5 groups of 6 mice per group: control group, LPS group (24 h, 48 h, 72 h), LPS + LXA4 group. For the induction of ARDS, mice were anaesthetised and instilled by intra-tracheal (IT) route as a model of direct lung injury with LPS (10 mg/kg dissolved in 30ul N.S) for 24 h, 48 h or 72 h. No treatment control mice were anaesthetised and instilled by intra-tracheal (IT) route with physiological saline. In LPS + LXA4 group, LXA4 was administrated by intraperitoneal injection at 1 μg/per mouse 10 min after intra-tracheal (IT) LPS administration. Mice were subsequently sacrificed by using cervical dislocation, lungs were removed and washed with sterile PBS and stored in 4% paraformaldehyde for HE and immunofluorescence, or at − 80 °C for Western blot, in tube for wet/dry ratio.
Immunofluorescence
Lung tissue were fixed and stained as the method described in the online Supplementary Information.
Quantitative real-time PCR and reverse transcriptase-PCR
Total RNA samples in HAT II cells were isolated using TRIzol reagent (Invitrogen, Carlsbad, California, USA) according to the manufacturer’s protocol. The cDNA of mRNA was synthesized using the reverse transcription kit (Bio-Rad, USA). The expression of mRNA was detected using SYBR green super-mix PCR kit (Bio-Rad) by qPCR (ABI7500, Applied Biosystems). The gene-specific primers used are listed in Table 1 and mRNA normalized to GAPDH, was calculated using the 2-ΔΔCt method.
Protein extraction and Western blot analysis
Cells or lung sections were washed in ice-cold PBS and harvested using RIPA buffer supplemented with protease inhibitors. The resulting supernatant fraction was homogenized in 1x SDS–PAGE sample buffer and boiled for 5 min at 99 °C. For the immunoblotting, protein lysates were electrophoresed via 10% SDS-PAGE gel and then transferred to to polyvinylidene difloride membranes. Membranes were blocked and incubated with the indicated primary antibody (Ab) overnight at 4 °C. Bound primary Abs were incubated with appropriate secondary Abs for 1 h. The proteins were detected using chemiluminescence reagents (Thermo Scientific). Images were scanned with a UVP imaging system and analyzed using an Image Quant LAS 4000 mini system (GE Healthcare Bio-Sciences AB, Uppsala, Sweden).
Flow cytometry (FCM)
Apoptosis of HAT II cells was assessed using flow cytometry. HAT II cells were left in serum free media for 24 h before exposure to LPS (1 μg/ml) with or without LXA4100nM for 24 h. After treatment with LPS and LXA4, HAT II cells were harvested and suspended in the binding buffer supplied in the Annexin V-FITC/Propidium iodide (PI) Apoptosis Detection Kit, and were then stained with Annexin V-FITC and Propidium iodide (PI) according to the manufacturer’s instruction (BD Biosciences, USA). The cytometric data were analyzed with FlowJo software.
Blinding method
The present study adopted randomized, blinded methods. The randomization list of animals was computer-generated by the statistician using SAS/STAT software.
Statistical analysis
Data are presented as mean ± SD or mean ± SEM. All data were analyzed using one-way ANOVA, followed by a Tukey test for post hoc comparisons. P < 0.05 was considered significant. Statistical analyses were performed using Prism 6.0 software (Graph Pad Software, San Diego, CA).
Results
LXA4 stimulates AT II cell proliferation and reduces AT II cell apoptosis in LPS induced lung injury
As shown in Additional file 1: Figure S1, intratracheal instillation of LPS (10 mg/kg) in mice induced lung injury with characteristic neutrophil accumulation, septal thickening, interstitial fluid accumulation, and alveolar hemorrhage at 24 h (Additional file 1: Figure S1B), 48 h (Additional file 1: Figure S1C) and 72 h (Additional file 1: Figure S1D). Treatment with LXA4 attenuated LPS-induced lung injury (Additional file 1: Figure S1E). The lung injury score was consistent with the histopathological changes (Additional file 1: Figure S1F). The Wet/Dry (W/D) ratio increased after LPS treatment, and LXA4 reversed the W/D ratio induced by LPS at 72 h (Additional file 1: Figure S1G), suggesting that LXA4 can alleviate lung permeability damage induced by LPS. The proliferation and apoptosis of AT II cells in the intratracheal LPS murine model of ALI/ARDS were observed by lung specimen immunofluorescence double staining of SP-C (a type II cell marker) and PCNA, SP-C and TUNEL respectively. LPS inhibited the proliferation of AT II cell (SP-C/PCNA double positive cells) and LXA4 abrogated the inhibition of LPS on AT II cells proliferation at 24 h (Fig. 1a, b). Meanwhile, apoptosis of AT II cells was calculated by the co-dying of SP-C and TUNEL. As shown in Fig. 1c and d, LPS increased AT II cell apoptosis, and LXA4 reduced apoptosis of AT II cell induced by LPS at 24 h.
LXA4 stimulates AT II cell proliferation and reduces AT II cell apoptosis in LPS induced lung injury. C57BL/6 J mice were intra-tracheal given N.S or LPS 10 mg/kg for 24 h, with or without LXA4 1μg intraperitoneal injection per mouse. Immunofluorescence staining of lung specimens was shot by fluorescence microscope and calculated by positive goals compared to DAPI. a-b: co-dying of SP-C and PCNA (× 200, × 400). c-d: co-dying of SP-C and TUNEL (× 200, × 400), scar bar = 50 μm. Data were presented with means ± SD; n = 4; ***P < 0.001, ****P < 0.0001
LXA4 decreases LPS-stimulated caspase-3 activation in lung tissue
Apoptosis is accompanied by caspase-3 cleavage, so cleaved caspase-3 was measured by both immunofluorescence and western blotting in different groups. Our results demonstrated that LPS increased the expression of cleaved caspase-3 in lung tissue, and LXA4 inhibited LPS-stimulated cleaved caspase-3 expression at 24 h in lung tissue (Fig. 2).
LXA4 alleviates apoptosis in LPS-induced lung injury. C57BL/6 J mice were intra-tracheal given N.S or LPS 10 mg/kg for 24 h, with or without LXA4 1μg per mouse intraperitoneal injection. Immunofluorescence staining of lung specimens was shot by fluorescence microscope and calculated by positive goals compared to DAPI. a-b: Immunofluorescence staining of cleaved-caspase-3, scar bar = 50 μm. c-d: WB of cleaved-caspase-3. Data were presented with means ± SD, *P < 0.05, **P < 0.01, ***P < 0.001; n = 3
LXA4 reduces HAT II cells apoptosis and stimulates primary human lung alveolar type II (HAT II) cells proliferation in vitro
As shown in Fig. 1, LXA4 stimulated HAT II cell proliferation and reduced HAT II cell apoptosis in the intratracheal LPS murine model of ALI/ARDS. Next, we investigated whether LXA4 could also stimulate HAT II cell proliferation and reduce HAT II cell apoptosis in vitro. As shown in Fig. 3a and c, LPS increased HAT II cell apoptosis, and treatment with LXA4 reduced apoptosis of HAT II cell induced by LPS at 24 h. LPS inhibited the proliferation of HAT II cells, while LXA4 promoted their proliferation. (Fig. 3c).
LXA4 stimulates HAT II cell proliferation and reduces HAT II cell apoptosis in vitro. HAT II cells were cultured as mentioned in the methods. a and b: apoptosis of HAT II after the stimulation of LPS and LXA4. c: Proliferation of HAT II after the stimulation of LPS and LXA4. Data were presented with means ±SEM. **P < 0.01, ***P < 0.001, **** P < 0.0001, n = 4 for each culture condition, repeated using cells from 4 donors
LXA4 inhibits the epithelial-mesenchymal transition (EMT) in LPS-induced lung injury
To observe the process of EMT in the LPS-induced lung injury model, we performed immunofluorescence staining of the EMT markers including E-cadherin, α-SMA, N- cadherin and vimentin. We found that LPS reduced the expression of epithelial cell markers E-cadherin in a time dependent manner, while LXA4 promoted the expression of E-cadherin in the lung tissue (Fig. 4a, b). In contrast, LPS increased the expression of mesenchymal cell markers including N- cadherin, α-SMA and vimentin in a time dependent manner, but LXA4 down-regulated the expression of mesenchymal cell markers stimulated by LPS (Fig. 4c-h). To determine whether AT II cells undergo EMT process in LPS-induced lung injury, lung specimens SP-C (a type II cell marker) and α-SMA double staining immunofluorescence were observed. We found that SP-C/α-SMA double positive cells were increased after LPS treatment (Fig. 4i, j). However, treatment with LXA4 significantly decreased SP-C/α-SMA double positive cells in the intratracheal LPS murine model of ALI/ARDS (Fig. 4i, j).
LXA4 inhibits the epithelial-mesenchymal transition (EMT) in LPS-induced lung injury. C57BL/6 J mice were intra-tracheal given N.S or LPS 10 mg/kg (for 24 h, 48 h or 72 h), with or without LXA4 1μg per mouse intraperitoneal injection. Immunofluorescence staining of lung specimens was shot by fluorescence microscope and calculated by positive goals compared to DAPI. a-h: Immunofluorescence staining of marker of EMT (× 400): E-cadherin(a-b), N-cadherin(c-d), α-SMA(e-f) and Vimentin(g-h). i and j: co-dying of SP-C and α-SMA. scar bar = 50 μm. All of the data was conducted in triplicate. Data were presented with means ± SD. n = 3. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
TGF-β1 induces EMT in HAT II cells
To investigate if TGF-β1 could induce EMT in HAT II cells, HAT II cells were incubated with TGF-β1 (0 ng/ml, 5 ng/ml, 10 ng/ml, 20 ng/ml) for 48 h or with TGF-β1 10 ng/ml for 0 h, 24 h, 48 h and 72 h. We found that the mRNA levels of epithelial markers, including CDH-1 (Fig. 5a), SP-C (Fig. 5b) and AQP-5 (Fig. 5c) in different TGF-β1 concentration groups, were all reduced by treatment with TGF-β1, and 10 ng/ml TGF-β1 group was lower than other groups. The mRNA levels of mesenchymal markers including CDH-2 (Fig. 5d), snail (Fig. 5e), α-SMA (Fig. 5f), and fibronectin (Fig. 5g), were promoted as the TGF-β1 concentration increased. There was no significant difference in the mRNA levels between treatment with 10 ng/ml and 20 ng/ml TGF-β1. After HAT II cells were treated with TGF-β1 10 ng/ml for 0 h, 24 h, 48 h and 72 h, the mRNA expression of CDH-1 (Fig. 5h), SP-C (Fig. 5i) and AQP-5 (Fig. 5j) were inhibited by TGF-β1 at different time points, and the mRNA expression of CDH-1, AQP-5 at 48 h were lower than at other time points, while the mRNA expression of SP-C reached the lowest level at 72 h. However, the mRNA expression of mesenchymal markers, including CDH-2 (Fig. 5k), Snail (Fig. 5l), α-SMA (Fig. 5m), fibronectin (Fig. 5n) were higher at 72 h than other time points, but there was no significant difference in the mRNA levels between treatment with TGF-β1 for 48 h and 72 h. Based on these results, it is reasonable to establish the vitro EMT model with the concentration of TGF-β1 10 ng/ml for 48 h.
TGF-β1 induces EMT in primary human lung alveolar type II (HAT II) cells. HAT II cells were cultured as mentioned in the methods. a-g: HAT II cells were incubated with TGF-β1 (0 ng/ml, 5 ng/ml, 10 ng/ml, 20 ng/ml) for 48 h. h-n: HAT II cells were incubated with TGF-β1 10 ng/ml for 0 h, 24 h, 48 h and 72 h. The expression of CDH-1, SP-C, AQP-5, CDH-2, snail, α-SMA and fibronectin were assessed by Real-time PCR. n = 4 for each culture condition, repeated using cells from 4 donors. Data were presented with means ± SEM, *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
LXA4 inhibits the EMT induced by TGF-β1 in HAT II cells
To investigate the effect of LXA4 on EMT induced by TGF-β1, Realtime-PCR and western blotting analyses were applied respectively. As shown in Fig. 6a-g, LXA4 promoted the mRNA expression of epithelial cell markers (CDH1, SP-C and AQP-5) in a does-dependent manner, while inhibiting the mRNA expression of mesenchymal cell markers, including CDH2, Snail, fibronectin and α-SMA in a does-dependent manner. Furthermore, the effects of LXA4 (100 nM) on the TGF-β1-induced CDH1 (E-cadherin), α-SMA, CDH2 (N-cadherin) protein expression of HAT II cells were confirmed by western blot (Fig. 6h-k).
LXA4 inhibits TGF-β1 induced EMT in primary HAT II cells. HAT II cells were incubated with or without TGF-β1 10 ng/ml for 48 h with or without LXA4 0.1 nM, 1 nM, 10 nM and 100 nM. a-g: the mRNA expression of CDH-1, SP-C, AQP-5, CDH-2, α-SMA and fibronectin. h-k: the protein expression level of E-cadherin, N-cadherin and α-SMA. n = 4 for each culture condition, repeated using cells from 4 donors. Data were presented with means ±SEM. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
LXA4 inhibits TGF-β1-induced EMT in primary HAT II cells through activation of LXA4 receptor (ALX)
To identify the involvement of ALX in LXA4 blockade of TGF-β1 induced EMT, HAT II cells were pre-treated with ALX ligands including BOC-2 10 μM (the LXA4 receptor antagonist) and BML-111 10 μM (the LXA4 receptor agonist) separately for 30 min. The effect of LXA4 on EMT was abrogated by the preincubation of HAT II cells with BOC-2 (Fig. 7a-d). While BML-111 promoted the effects of LXA4 on TGF-β1-induced EMT in HAT II cells (Fig. 7e-h). These results suggest that the effects of LXA4 on TGF-β1-induced EMT are mediated via activation of ALX.
LXA4 inhibits TGF-β1-induced EMT in primary AT II cells through activation of LXA4 receptor (ALX). HAT II cells were pre-incubated with or without BOC-2 10μΜ or BML-111 10μΜ 30 min before TGF-β1 10 ng/ml for 48 h with or without LXA4 100 nM. a-d: the effect of LXA4 on EMT was promoted by the pre-incubation of AT II cells with BML-111 (the LXA4 receptor agonist). e-h: the effect of LXA4 on EMT was abrogated by the pre-incubation of AT II cells with BOC-2(the LXA4 receptor antagonist). n = 4 for each culture condition, repeated using cells from 4 donors. Data were presented with means ±SEM. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
LXA4 reduces TGF-β1-induced EMT in primary HAT II cells partly through the SMAD and PI3K/AKT signaling pathway
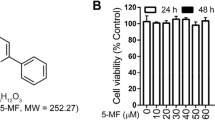
To confirm the involvement of the Smad2/3 and PI3K/Akt pathways in LXA4 blockade of TGF-β1-induced EMT in primary HAT II cells, HAT II cells were pre-treated with 10 μM Sis3 (a specific Smad3 inhibitor) and 10 μM LY294002 (PI3Kinhibitor) for 30 min prior to TGF-β1 and/or LXA4 administration. Sis3 and LY294002 treatment abolished the inhibitory effect of LXA4 on the EMT in HAT II cells (Fig. 8a-h). To further determine the activity of the PI3K/AKT and SMAD signaling pathways in primary HAT II cells stimulated by TGF-β1 after treatment with LXA4, the phosphorylation of AKT and Smad in HAT II cells were measured. The expressions of p-AKT and p-Smad were stimulated by TGF-β1 in primary HAT II cells and significantly downregulated by LXA4 (Fig. 8i-k). The agonist and antagonists had no effect on cell viability (Additional file 1: Figure S2).
LXA4 reduces TGF-β1-induced EMT in HAT II cells partly through the SMAD and PI3K/AKT signaling pathways. HAT II cells were pre-incubated with 10 μM Sis3 (a specific Smad3 inhibitor), and 10 μM LY294002(PI3Kinhibitor) for 30 min prior to TGF-β1 10 ng/ml for 48 h with or without LXA4 100 nM. a-h: Sis3 and LY294002 treatment abolished the inhibition of LXA4 on the EMT in AT II cells. i-k: LXA4 inhibited TGF-β1-induced the phosphorylation of AKT and Smad in primary AT II cells. n = 4 for each culture condition, repeated using cells from 4 donors. Data were presented with means ±SEM. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
Discussion
Our study demonstrated that LXA4 alleviated lung injury via promoting type II alveolar lung epithelial cell proliferation, whilst inhibiting apoptosis and decreasing caspase-3 activation in an intratracheal LPS murine model of ALI/ARDS. In vitro, LXA4 reduced AT II cell apoptosis and promoted AT II cell proliferation induced by LPS. We also showed that LXA4 inhibited EMT in vivo and reduced TGF-β1 induced EMT in human primary type II alveolar epithelial cells. Furthermore, treatment with LXA4 receptor antagonist, Smad2/3 inhibitor and PI3K/AKT inhibitor abolished the inhibitory effect of LXA4 on the EMT in AT II cells, indicating that LXA4 can inhibit TGF-β1-induced EMT in primary AT II cells through the SMAD, PI3K/AKT signaling pathways and activation of LXA4 receptor (ALX).
The epithelial cell is a main target in the development of ALI/ARDS [21]. Injury of the alveolar epithelial cells (AT II cells) are acknowledged as critical hallmark of ARDS [22]. Timely repair of AT II cells is critical for restoration of lung function in ARDS. Inappropriate repair, such as EMT, can lead to disrupted barrier function and promote fibrogenesis [21]. Many studies reported that LXA4 exerts a protective effect on ALI in mice and on the airway epithelial cells [18, 23, 24]. Our previous study also showed that LXA4 alleviated inflammation and pulmonary permeability [18]. In order to investigate the potential mechanism of LXA4 in promoting resolution of ARDS, we previously demonstrated that LXA4 promoted lung epithelial repair and inhibited sFasL induced AT II cell apoptosis in vitro. In the present study we used an animal model of LPS-induced lung injury to confirm the previous results. We found that intratracheal instillation of LPS inhibited the proliferation of AT II cells and increased apoptosis of these cells. However, LXA4 restored the function of the epithelial barriers by reversing the inhibition of LPS on AT II cell proliferation and reducing apoptosis of AT II cells induced by LPS. In addition, LXA4 promoted primary AT II cell proliferation and reduced apoptosis induced by LPS [25, 26].
As a central role in the execution of the apoptotic program, caspase-3 is primarily responsible for the cleavage of poly (ADP-ribose) polymerase (PARP) during apoptosis [27, 28]. In our study, treatment with LPS in mice significantly increased TUNEL-positive AT II cells and cleaved caspase-3 expression in the lung tissue. However, LXA4 reduced LPS-stimulated cleaved caspase-3 expression and TUNEL-positive AT II cells at 24 h in lung tissue, indicating its anti-apoptotic effects in this murine model of lung injury.
Previous evidence in animal models of ARDS showed that pulmonary edema can happen only after the impairment of epithelium function [5, 29, 30]. Injury to the AT II cells activates apoptotic markers such as caspases-3, while some of the AT II cells undergo EMT which includes loss of their epithelial morphology as well as epithelial biomarkers and acquisition of a mesenchymal (fibroblast-like) cell phenotype [30,31,32,33]. Inflammation, which is one of the primary causes of ARDS, also results in EMT [33]. LPS was shown to induce EMT [32], while LXA4 could suppress EMT in proximal tubular epithelial cells, pancreatic cancer cells and hepatocarcinoma cells [34,35,36]. In our study, LPS induced EMT in a time dependent manner. We also demonstrated that LXA4 stimulated the expression of E-cadherin while inhibiting the expressions of mesenchymal cell markers including N-cadherin, vimentin and α-SMA in LPS induced lung injury. Furthermore, we also showed that AT II cells expressed more mesenchymal biomarkers (α-SMA), which was inhibited by treatment with LXA4 in the lung tissue. These data indicate that targeting the anti-EMT actions of LXA4 may be a therapeutic strategy for treating ARDS.
To confirm the result that LXA4 suppressed EMT in lung tissue, we investigated the effect of LXA4 on EMT in vitro. We showed that TGF-β1 induced EMT in primary human lung alveolar type II (HAT II) cells, while LXA4 inhibited TGF-β1 induced EMT in a concentration-dependent manner. In addition, LXA4 exerts its pro-resolving action through ALX (lipoxin receptor) [37]. In the present study, BOC-2 (ALX antagonist) reversed LXA4-suppressed EMT. Interestingly, BML-111(lipoxin receptor agonist), which was used in this study, promoted the effects of LXA4 on TGF-β1-induced EMT in primary human AT II cells. These data imply that LXA4 may act via activation of ALX.
Various studies have demonstrated underlying mechanisms involved in TGF-β1 induced EMT including the Smad signaling pathway and the PI3K/Akt signaling pathway [38, 39]. Our study suggests that inhibition of Smad3 and PI3K abolished the inhibitory effects of LXA4 on EMT in AT II cells, indicating that LXA4 inhibits EMT via the Smad and the PI3K/Akt signaling pathways. Indeed, in our study, LXA4 downregulated the phosphorylation of AKT and Smad induced by TGF-β1 in AT II cells.
Conclusion
In conclusion, we have shown that LXA4 attenuates lung injury via stimulating epithelial cell proliferation, reducing epithelial cell apoptosis and inhibits EMT. In addition, LXA4 suppressed TGF-β1 induced EMT through the SMAD, PI3K/AKT signaling pathways and activation of LXA4 receptor (ALX). Our findings provide the evidence that targeting the pro-proliferaory, anti-apoptotic and anti-EMT actions of LXA4 may be a potential approach in developing an effective strategy for the treatment of ARDS. Further experiments are necessary to understand the basic mechanism underlying the anti-apoptotic effects of LXA4.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALI:
-
Acute lung injury
- AQP-5:
-
Aquaporin V
- ARDS:
-
Acute respiratory distress syndrome
- AT II:
-
Alveolar Type II
- CDH-1:
-
E-cadherin
- CDH-2:
-
N-cadherin
- EMT:
-
Epithelial-Mesenchymal Transition
- HAT II:
-
Human Alveolar Type II
- LPS:
-
Lipopolysaccharides
- LXA4:
-
Lipoxin A4
- PCNA:
-
Proliferating Cell Nuclear Antigen
- SP-C:
-
Surfactant protein C
- TGF-β1 :
-
Transforming growth factor-β1
- TUNEL:
-
Terminal deoxynucleotidyl transferase-mediated dUTP-biotin nick End Labeling
- α-SMA:
-
α-Smooth muscle actin
References
Rezoagli E, Fumagalli R, Bellani G. Definition and epidemiology of acute respiratory distress syndrome. Ann Transl Med. 2017;5:282. https://doi.org/10.21037/atm.2017.06.62.
Matthay MA, Zimmerman GA. Acute lung injury and the acute respiratory distress syndrome: four decades of inquiry into pathogenesis and rational management. Am J Respir Cell Mol Biol. 2005;33:319–27. https://doi.org/10.1165/rcmb.F305.
Matthay MA, Robriquet L, Fang X. Alveolar epithelium: role in lung fluid balance and acute lung injury. Proc Am Thorac Soc. 2005;2:206–13. https://doi.org/10.1513/pats.200501-009AC.
Bachofen M, Weibel ER. Structural alterations of lung parenchyma in the adult respiratory distress syndrome. Clin Chest Med. 1982;3:35–56.
Martin TR, Hagimoto N, Nakamura M, Matute-Bello G. Apoptosis and epithelial injury in the lungs. Proc Am Thorac Soc. 2005;2:214–20. https://doi.org/10.1513/pats.200504-031AC.
Perl M, Lomas-Neira J, Chung CS, Ayala A. Epithelial cell apoptosis and neutrophil recruitment in acute lung injury-a unifying hypothesis? What we have learned from small interfering RNAs. Mol Med. 2008;14:465–75. https://doi.org/10.2119/2008-00011.Perl.
Matthay MA, Zemans RL. The acute respiratory distress syndrome: pathogenesis and treatment. Annu Rev Pathol. 2011;6:147–63. https://doi.org/10.1146/annurev-pathol-011110-130158.
Bartis D, Mise N, Mahida RY, Eickelberg O, Thickett DR. Epithelial-mesenchymal transition in lung development and disease: does it exist and is it important? Thorax. 2014;69:760–5. https://doi.org/10.1136/thoraxjnl-2013-204608.
Gouda MM, Shaikh SB, Bhandary YP. Inflammatory and Fibrinolytic system in acute respiratory distress syndrome. Lung. 2018;196:609–16. https://doi.org/10.1007/s00408-018-0150-6.
Chen Q, et al. Monocyte interaction accelerates HCl-induced lung epithelial remodeling. BMC Pulm Med. 2014;14:135. https://doi.org/10.1186/1471-2466-14-135.
Cabrera-Benitez NE, et al. Mechanical stress induces lung fibrosis by epithelial-mesenchymal transition. Crit Care Med. 2012;40:510–7. https://doi.org/10.1097/CCM.0b013e31822f09d7.
Panneerdoss S, et al. Cross-talk between miR-471-5p and autophagy component proteins regulates LC3-associated phagocytosis (LAP) of apoptotic germ cells. Nat Commun. 2017;8:598. https://doi.org/10.1038/s41467-017-00590-9.
Serhan, C. N., Chiang, N. & Van Dyke, T. E. Resolving inflammation: dual anti-inflammatory and pro-resolution lipid mediators. Nat Rev Immunol 8, 349–361, doi: https://doi.org/10.1038/nri2294 (2008).
Morris T, Stables M, Gilroy DW. New perspectives on aspirin and the endogenous control of acute inflammatory resolution. ScientificWorldJournal. 2006;6:1048–65. https://doi.org/10.1100/tsw.2006.192.
Filep JG, Zouki C, Petasis NA, Hachicha M, Serhan CN. Anti-inflammatory actions of lipoxin a (4) stable analogs are demonstrable in human whole blood: modulation of leukocyte adhesion molecules and inhibition of neutrophil-endothelial interactions. Blood. 1999;94:4132–42.
Reville K, Crean JK, Vivers S, Dransfield I, Godson C. Lipoxin A4 redistributes myosin IIA and Cdc42 in macrophages: implications for phagocytosis of apoptotic leukocytes. J Immunol. 2006;176:1878–88.
Walker J, et al. Lipoxin a4 increases survival by decreasing systemic inflammation and bacterial load in sepsis. Shock. 2011;36:410–6. https://doi.org/10.1097/SHK.0b013e31822798c1.
Jin SW, et al. Posttreatment with aspirin-triggered lipoxin A4 analog attenuates lipopolysaccharide-induced acute lung injury in mice: the role of heme oxygenase-1. Anesth Analg. 2007;104:369–77. https://doi.org/10.1213/01.ane.0000252414.00363.c4.
Wang Q, et al. Lipoxin A (4) activates alveolar epithelial sodium channel, Na,K-ATPase, and increases alveolar fluid clearance. Am J Respir Cell Mol Biol. 2013;48:610–8. https://doi.org/10.1165/rcmb.2012-0274OC.
Zheng S, et al. Lipoxin A4 promotes lung epithelial repair whilst inhibiting fibroblast proliferation. ERJ Open Res. 2016;2. https://doi.org/10.1183/23120541.00079-2015.
Wang X, Adler KB, Erjefalt J, Bai C. Airway epithelial dysfunction in the development of acute lung injury and acute respiratory distress syndrome. Expert Rev Respir Med. 2007;1:149–55. https://doi.org/10.1586/17476348.1.1.149.
Gropper MA, Wiener-Kronish J. The epithelium in acute lung injury/acute respiratory distress syndrome. Curr Opin Crit Care. 2008;14:11–5. https://doi.org/10.1097/MCC.0b013e3282f417a0.
Bonnans C, Fukunaga K, Levy MA, Levy BD. Lipoxin a (4) regulates bronchial epithelial cell responses to acid injury. Am J Pathol. 2006;168:1064–72. https://doi.org/10.2353/ajpath.2006.051056.
Qi W, et al. Lipoxin A4 activates alveolar epithelial sodium channel gamma via the microRNA-21/PTEN/AKT pathway in lipopolysaccharide-induced inflammatory lung injury. Lab Invest. 2015;95:1258–68. https://doi.org/10.1038/labinvest.2015.109.
Kitamura, Y. et al. Fas/FasL-dependent apoptosis of alveolar cells after lipopolysaccharide-induced lung injury in mice. Am J Respir Crit Care Med 163, 762–769, doi:https://doi.org/10.1164/ajrccm.163.3.2003065 (2001).
Xie W, et al. ResolvinD1 reduces apoptosis and inflammation in primary human alveolar epithelial type 2 cells. Lab Invest. 2016;96:526–36. https://doi.org/10.1038/labinvest.2016.31.
Boulares AH, et al. Role of poly (ADP-ribose) polymerase (PARP) cleavage in apoptosis. Caspase 3-resistant PARP mutant increases rates of apoptosis in transfected cells. J Biol Chem. 1999;274:22932–40.
Kuribayashi K, Mayes PA, El-Deiry WS. What are caspases 3 and 7 doing upstream of the mitochondria? Cancer Biol Ther. 2006;5:763–5.
Crosby LM, Waters CM. Epithelial repair mechanisms in the lung. Am J Physiol Lung Cell Mol Physiol. 2010;298:L715–31. https://doi.org/10.1152/ajplung.00361.2009.
Zeisberg M, Neilson EG. Biomarkers for epithelial-mesenchymal transitions. J Clin Invest. 2009;119:1429–37. https://doi.org/10.1172/jci36183.
Kalluri R, Neilson EG. Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest. 2003;112:1776–84. https://doi.org/10.1172/jci20530.
Zhang YQ, et al. Resveratrol ameliorates lipopolysaccharide-induced epithelial mesenchymal transition and pulmonary fibrosis through suppression of oxidative stress and transforming growth factor-beta1 signaling. Clin Nutr. 2015;34:752–60. https://doi.org/10.1016/j.clnu.2014.08.014.
Heise RL, Stober V, Cheluvaraju C, Hollingsworth JW, Garantziotis S. Mechanical stretch induces epithelial-mesenchymal transition in alveolar epithelia via hyaluronan activation of innate immunity. J Biol Chem. 2011;286:17435–44. https://doi.org/10.1074/jbc.M110.137273.
Zong L, et al. Lipoxin A4 reverses mesenchymal phenotypes to attenuate invasion and metastasis via the inhibition of autocrine TGF-beta1 signaling in pancreatic cancer. J Exp Clin Cancer Res. 2017;36:181. https://doi.org/10.1186/s13046-017-0655-5.
Wu SH, Zhang YM, Tao HX, Dong L. Lipoxin a (4) inhibits transition of epithelial to mesenchymal cells in proximal tubules. Am J Nephrol. 2010;32:122–36. https://doi.org/10.1159/000315121.
Xu F, et al. Lipoxin A4 and its analog suppress hepatocarcinoma cell epithelial-mesenchymal transition, migration and metastasis via regulating integrin-linked kinase axis. Prostaglandins Other Lipid Mediat. 2018;137:9–19. https://doi.org/10.1016/j.prostaglandins.2018.05.007.
Pirault J, Back M. Lipoxin and Resolvin receptors transducing the resolution of inflammation in cardiovascular disease. Front Pharmacol. 2018;9:1273. https://doi.org/10.3389/fphar.2018.01273.
Yang J, Dai C, Liu Y. A novel mechanism by which hepatocyte growth factor blocks tubular epithelial to mesenchymal transition. J Am Soc Nephrol. 2005;16:68–78. https://doi.org/10.1681/asn.2003090795.
Bakin AV, Tomlinson AK, Bhowmick NA, Moses HL, Arteaga CL. Phosphatidylinositol 3-kinase function is required for transforming growth factor beta-mediated epithelial to mesenchymal transition and cell migration. J Biol Chem. 2000;275:36803–10. https://doi.org/10.1074/jbc.M005912200.
Acknowledgments
We thank the patients and relatives who agreed to both tissue donation during elective surgery. We thank Peter Santer for helping us revise the manuscript for English language.
Funding
This work was supported by the National Natural Science Foundation of China (grants No: 81401579, 81870065, 81570076). None of the funding sources had any involvement in the study design, in the collection, analysis and interpretation of data, in the writing of the report or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
conceptualization, JY, FGS, SJ and SZ; methodology, JY and ML; software, XC and QW; validation, ML, XC; formal analysis, JY and FGS; investigation, JY; resources, QL; data curation, JY; writing—original draft preparation, JY; writing—review and editing, JY and SZ; visualization, SZ; supervision, SJ; project administration, SJ; funding acquisition, SJ. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Human lung tissue was obtained from peripheral normal lung tissue distal from the tumor in patients undergoing lung cancer resection. All procedures in this study were carried out in accordance with approval from the local research ethics committees at the Second Affiliated Hospital of Wenzhou Medical University (2017–17) from May 2015 to December 2017. All patients gave written informed consent for the use of their tissue and clinical data for research purposes. All animal experiments in this study were performed in accordance with the Guide for the Care and Use of Laboratory Animals of Wenzhou Medical University. The in vivo protocols were approved by the Committee of Experimental Animals of Wenzhou Medical University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Figure S1. LXA4 alleviates inflammation and pulmonary permeability in LPS-induced lung injury. A-E: HE staining of lung. F: injury score of lung. G: wet/dry ratio of lung. Data were presented with means ±SD. ***P<0.001, ****P<0.0001. n=3. Figure S2. The agonist and antagonists had no effect on cell vialibity. There is no significant of the agonist and antagonists on HATII cell vilibity. Data were presented with means ±SD. n=3. (DOCX 605 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yang, Jx., Li, M., Chen, Xo. et al. Lipoxin A4 ameliorates lipopolysaccharide-induced lung injury through stimulating epithelial proliferation, reducing epithelial cell apoptosis and inhibits epithelial–mesenchymal transition. Respir Res 20, 192 (2019). https://doi.org/10.1186/s12931-019-1158-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-019-1158-z